SANTA CRUZ POST ACUTE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Santa Cruz Post Acute has received a Trust Grade of F, indicating significant concerns and overall poor performance compared to other facilities. They rank #901 out of 1155 in California, placing them in the bottom half of nursing homes in the state, and #5 out of 7 in Santa Cruz County, meaning only two local options are worse. The facility's trend is stable, with 21 issues reported in both 2024 and 2025, but the staffing rating is only 2 out of 5 stars, with a concerning turnover rate of 59%, much higher than the state average of 38%. Additionally, the home has incurred $77,549 in fines, which is higher than 82% of California facilities, suggesting ongoing compliance problems. Strengths include excellent quality measures rated 5 out of 5, indicating good outcomes for residents. However, serious incidents have been reported, such as a resident falling and sustaining a laceration after being left unsupervised, and multiple residents not receiving necessary medication management, including a failure to monitor blood pressure before administering critical medications. These findings highlight significant weaknesses in both resident safety and medication oversight.
- Trust Score
- F
- In California
- #901/1155
- Safety Record
- High Risk
- Inspections
- Holding Steady
- Staff Stability ⚠ Watch
- 59% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $77,549 in fines. Lower than most California facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 26 minutes of Registered Nurse (RN) attention daily — below average for California. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 82 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below California average (3.1)
Below average - review inspection findings carefully
13pts above California avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
11 points above California average of 48%
The Ugly 82 deficiencies on record
Jul 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to obtain informed consent for psychotropic medications from the responsible party (RP, a person empowered to make decisions for the resident)...
Read full inspector narrative →
Mar 2025
20 deficiencies
1 IJ (1 affecting multiple)
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0757
(Tag F0757)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure 13 out of 40 sampled residents (Residents 10, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain respect, and dignity to three of 28 sampled ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement their policy and procedure on self-administ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure needs were accommodated for one of 28 sampled ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to complete a comprehensive minimum data set (MDS - a federally manda...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0836
(Tag F0836)
Could have caused harm · This affected 1 resident
Based on observation, interview, and document review, the facility failed to comply with Federal and State laws and regulations when the approval letter for staffing waiver was not posted where visito...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the comprehensive care plans were developed and implemented ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide care in accordance with professional standards...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide appropriate care and services for indwelling catheter (a catheter which is inserted into the bladder [a sac-shaped mu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the proper use of side or bed rails (adjustabl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to provide sufficient nursing staff on a 24-hour basis based on the Staffing Data Report submitted to the Centers for Medicare & Medicaid Serv...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
2. During the medication pass observation on 2/24/25 at 9:17 a.m., Licensed Vocational Nurse C (LVN C), was observed giving medications to Resident 6.
On 2/24/25 at 9:33 a.m., LVN C was also observed...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the provision of pharmaceutical services that ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the Consultant Pharmacist (CP) identified and reported irregularities during the monthly medication regimen review (MR...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure three out of 28 sampled residents (Residents 45, 104, and 107) were free from unnecessary psychotropic medications (drugs that affec...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility had a medication error rate of 12.12% when four medication errors were observed out of 33 opportunities during medication administratio...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, record review, the facility failed to ensure medications were properly stored and labeled in three of three medication carts and in two of three medication rooms. Mult...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure palatability and nutritive value of cooked food...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure food items were stored and prepared in accorda...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5a. During a medication administration observation with Registered Nurse (RN) F on 2/24/25 at 8:43 a.m., she was observed prepar...
Read full inspector narrative →
Dec 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide and/or communicate the appropriate information to the recei...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide approriate and necessary services in accordance with profes...
Read full inspector narrative →
Dec 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure the Activities of Daily Living (ADL -routine tasks/activities such as bathing, dressing and toileting a person performs daily to car...
Read full inspector narrative →
Oct 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide proper supervision for one of three residents (Resident 1) when a nurse aide (nursing assistant) did not have the required certific...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0728
(Tag F0728)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure three of 12 aides (Nursing Assistant A (NA A), Nursing Assistant B (NA B), and Nursing Assistant C (NA C)) completed their state cer...
Read full inspector narrative →
Aug 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to provide appropriate care and services for an indwelling catheter (flexible tube inserted and left in the bladder to drain urine) for one of...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure nurses documented the admission for one of three residents (...
Read full inspector narrative →
Aug 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop a care plan (identifies residents' concerns and outlines th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure care and services were provided in accordance with professio...
Read full inspector narrative →
Jul 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to honor two of three residents' (Residents 2 and 3) req...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure care and services were provided in accordance with professi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow their bed rails (adjustable rigid bars attached to the side of a bed: side rails, safety rails, and grab/assist bars) ...
Read full inspector narrative →
Jul 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to provide a written notice for two of six residents (Resident 1 and 2) prior to a room change. Also, there was no documentation in the medica...
Read full inspector narrative →
Jun 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure supervision and assistance were provided for one of three sa...
Read full inspector narrative →
Jun 2024
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure nurses were trained and demonstrated competenc...
Read full inspector narrative →
Jun 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure care and services were provided in accordance with profession...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure care and services were provided in accordance with professio...
Read full inspector narrative →
Mar 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to meet professional standard of practice when there were missing licensed nurse's signature entries in the treatment administration record (T...
Read full inspector narrative →
Jan 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide safe discharge for one of three sampled residents (Resident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to develop a care plan that reflect the specific care needs for one of three sampled residents (Resident 1) when there was no care plan develo...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide services which meet professional standards for one of three...
Read full inspector narrative →
Nov 2023
6 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure services were provided to meet professional standard of practice for one of two residents (Resident 1) when:
1. There was no documen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure quality of care was provided for two out of two residents (Resident 2 & 3) when the weekly wound evaluations were not ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure acceptable parameters of nutrition and hydration when the me...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the wound doctor write the progress notes at each visit for Resident 2. The wound doctor physician had no documented written notes i...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure resident ' s medical records were complete and readily available for review by official authorized by law for Resident 2 when the wo...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify the resident's responsible party (RP, a person responsible i...
Read full inspector narrative →
Oct 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure care and services were provided in accordance with professio...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and policy review, the facility failed to ensure proper medication storage when an unlocked medication cart with a bottle of acetaminophen (used to treat aches and pai...
Read full inspector narrative →
May 2023
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to maintain the call light was within reach for one of 25 sampled residents (Resident 69). The failure could result to untimely d...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0642
(Tag F0642)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to maintain the accuracy of the resident assessment of one of 25 sampled residents (Resident 113). The failure resulted in ineffective care pl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure services were provided to meet the professiona...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure an eye consultation and/or referral was arrang...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide necessary podiatry services for one of 25 sam...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of nine residents (Resident 273) who had t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure the central venous catheter (CVC, a thin, flex...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure each resident's medication regimen was free from unnecessary medication for two of 25 sampled residents (Residents 62 and 69). Resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of 25 sampled residents (Resident 69) was free from unnecessary psychotropic medications (drugs that affect brain activities ass...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
2. During a kitchen observation on 5/8/23, at 8:20 a.m., accompanied by the Dietary Director (DD), there was one dented big can of golden cream style corn and one dented big can of salsa de queso para...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure compliance with infection control practices when one Laundry Personnel I (LP I) was wearing gloves in the hallway. Thi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident 113 was admitted with diagnoses including chronic kidney disease, and neuromuscular dysfunction of bladder. There wa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the provision for safe use of insulin (medication to lower blood glucose) pens; and controlled medications (those with...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure the consultant pharmacist (CP) identify and report to the facility irregularities related to medication regimen for three of 25 samp...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility had a medication error rate of 10.34% when three medication errors occurred out of 29 opportunities during the medication administratio...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the food served to two of 25 sampled residents (Resident 63 and one anonymous resident) were maintained at the proper ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure the proper disposal of garbage when two of the four receptacles were overfilled so the lids could not be closed. This f...
Read full inspector narrative →
May 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the assistant director of nursing (ADON) failed to document the hospitalist's (a doctor wh...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents are discharged appropriately for two of two sample...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide evidence of documentation regarding the action...
Read full inspector narrative →
Dec 2022
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and clinical record review, the facility failed to ensure one of two sampled residents (Resident 1) had an ap...
Read full inspector narrative →
Nov 2022
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to address hearing deficit issues for one resident (Resid...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to follow their infection prevention and control policy a...
Read full inspector narrative →
Jan 2020
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure peripherally inserted central catheter (PICC, a thin flexible tube was inserted into a vein in the upper arm and guide...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Review of Resident 6's clinical record indicated he was admitted to the facility with diagnoses including acute respiratory failure with hypoxia (absence of enough oxygen in the tissues to sustain bod...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Review of Resident 75's clinical record indicated he was admitted to the facility with diagnoses including diabetes mellitus (group of diseases that result in too much sugar in the blood high blood gl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Review of Resident 25's clinical record indicated she was admitted on [DATE] with diagnoses major depressive disorder and dement...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility had a 12% error rate when three medication errors out of 25 opp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to store medication in accordance with professional stan...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure safe food storage practices when residents' food were not labeled and dated and when the temperature of two of two res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure staff implemented proper infection control pract...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to accommodate resident's needs for one of 26 residents (Resident 61) when staff did not attend to Resident 61's needs promptly. ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s), 2 harm violation(s), $77,549 in fines. Review inspection reports carefully.
- • 82 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $77,549 in fines. Extremely high, among the most fined facilities in California. Major compliance failures.
- • Grade F (13/100). Below average facility with significant concerns.
About This Facility
What is Santa Cruz Post Acute's CMS Rating?
CMS assigns SANTA CRUZ POST ACUTE an overall rating of 2 out of 5 stars, which is considered below average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Santa Cruz Post Acute Staffed?
CMS rates SANTA CRUZ POST ACUTE's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 59%, which is 13 percentage points above the California average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 73%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Santa Cruz Post Acute?
State health inspectors documented 82 deficiencies at SANTA CRUZ POST ACUTE during 2020 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 2 that caused actual resident harm, and 79 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
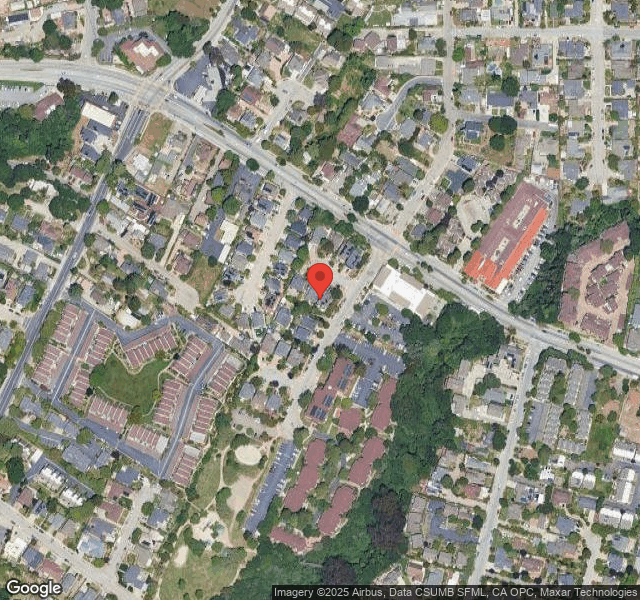
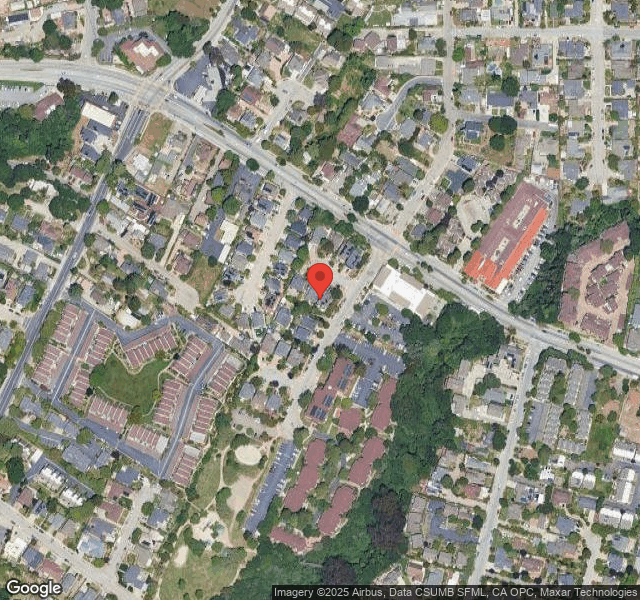
Who Owns and Operates Santa Cruz Post Acute?
SANTA CRUZ POST ACUTE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PACS GROUP, a chain that manages multiple nursing homes. With 149 certified beds and approximately 135 residents (about 91% occupancy), it is a mid-sized facility located in SANTA CRUZ, California.
How Does Santa Cruz Post Acute Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, SANTA CRUZ POST ACUTE's overall rating (2 stars) is below the state average of 3.1, staff turnover (59%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Santa Cruz Post Acute?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the facility's high staff turnover rate, and the below-average staffing rating.
Is Santa Cruz Post Acute Safe?
Based on CMS inspection data, SANTA CRUZ POST ACUTE has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in California. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Santa Cruz Post Acute Stick Around?
Staff turnover at SANTA CRUZ POST ACUTE is high. At 59%, the facility is 13 percentage points above the California average of 46%. Registered Nurse turnover is particularly concerning at 73%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Santa Cruz Post Acute Ever Fined?
SANTA CRUZ POST ACUTE has been fined $77,549 across 2 penalty actions. This is above the California average of $33,854. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Santa Cruz Post Acute on Any Federal Watch List?
SANTA CRUZ POST ACUTE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.