OCEAN POINTE HEALTHCARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Ocean Pointe Healthcare Center in Santa Monica has received a Trust Grade of F, indicating significant concerns about the facility's quality of care. It ranks #867 out of 1155 nursing homes in California, placing it in the bottom half of available options, and #219 out of 369 in Los Angeles County, meaning only a few local facilities are rated worse. While the facility's overall trend is improving, having decreased from 16 issues in 2024 to 13 in 2025, it still has a concerning total of 56 deficiencies, including two critical incidents. Staffing is average with a 40% turnover rate, and RN coverage is also average, but the facility has incurred $55,450 in fines, which is higher than 88% of California facilities, indicating ongoing compliance issues. Specific incidents include a failure to provide an alternate call system, leaving several residents without timely assistance and one resident in significant pain, and missing records related to daily nurse staffing data which raises concerns about transparency and accountability.
- Trust Score
- F
- In California
- #867/1155
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 40% turnover. Near California's 48% average. Typical for the industry.
- Penalties ✓ Good
- $55,450 in fines. Lower than most California facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 31 minutes of Registered Nurse (RN) attention daily — about average for California. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 56 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (40%)
8 points below California average of 48%
Facility shows strength in fire safety.
The Bad
Below California average (3.1)
Below average - review inspection findings carefully
Near California avg (46%)
Typical for the industry
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 56 deficiencies on record
Sept 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 72543(b) Based on observation, interview and record review, the facility failed to maintain medical records for one out of three...
Read full inspector narrative →
Mar 2025
9 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident's written notice of transfer was provided to the resident's responsible party as soon as practicable for one (1) out of t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of two residents (Resident 30) had bilateral floor mats per the physician order and the resident's high risk for f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to label enteral hydration for one of sixteen sampled residents (Resident 162).
These deficient practices had the potential to c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to label enteral hydration for one of sixteen sampled residents (Resident 162).
These deficient practices had the potential to c...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed to:
1) Ensure staffing information on the Direct Hours Patient Day (DHPPD - a list of staff hours of direct daily care) form was completed and ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure safe and sanitary food storage and preparation practices when the facility failed to:
1. Ensure all opened food items...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to ensure the industrial washing machine used to wash the facility linen and residents including clothing was not leaking.
This ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure:
1. The floor in laundry room walkway did not have holes and was not cracked.
2. The door leading to the resident dini...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0912
(Tag F0912)
Minor procedural issue · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure that 19 out of 29 resident rooms (Rooms 1, 2, 3, 4, 5, 7, 8, 9, 10, 11, 12, 15, 16, 17, 18, 19, 20, and 21) met the sq...
Read full inspector narrative →
Jan 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure one of one sampled resident (Resident 1) was properly super...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure safe and orderly discharge from the facility to home for one...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement a comprehensive care plan that met the care/services base...
Read full inspector narrative →
Jun 2024
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide reasonable accommodation of resident needs and preferences ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure a grievance involving one of two sampled reside...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement its policy and procedure for ensuring the reporting of a ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement its abuse policies and procedures to ensure an investigat...
Read full inspector narrative →
Mar 2024
12 deficiencies
1 IJ (1 facility-wide)
CRITICAL
(L)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0919
(Tag F0919)
Someone could have died · This affected most or all residents
⚠️ Facility-wide issue
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide alternate call system for nine of 62 residents from 3/9/202...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to initiate a change of condition (COC) for one of six sampled residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure a safe homelike environment for eight ambulatory residents.
This deficient practice had the potential to result in residents falling i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop a comprehensive care plan for one of five residents (Reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow the physicians order for oxygen supplementatio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to administer pain medication in accordance with physician's orders and care plans for one out of eight sampled residents (Residents 58).
As ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and records review, the facility failed to:
1) Ensure staffing information was posted in a prominent place readily accessible to residents and visitors.
2) Make nurse...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow up and communicate with a physician the consultant pharmacis...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
During an interview on 11/7/23 at 2:18 AM with Maintenance Supervisor (MS). MS stated MS was not aware of any water management program. However, MS stated MS had tested the water temperatures and kept...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure Pneumonia (PNA-infection of one or both lungs) vaccines was ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0912
(Tag F0912)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure that 19 out of 29 resident rooms (Rooms 1, 2, 3, 4, 5, 6, 7 ,8, 9, 10, 11, 12, 15, 16, 17, 18, 19, 20, and 21) met the...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the safety of storing, preparing, distributing, and serving food in accordance with professional standards and its pol...
Read full inspector narrative →
Nov 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, facility failed to implement dish washing cleaning and sanitizing procedures while cleaning cups, plates, lids, and utensils for 64 of 64 Residents.
...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide necessary respiratory care services for two o...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to act upon the licensed pharmacist's recommendation to change the pre...
Read full inspector narrative →
Sept 2023
2 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0678
(Tag F0678)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure Licensed Vocational Nurse 3 (LVN 3), performed cardio pulmona...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure documentation was accuracy for one of three sampled residents (Resident 1), when Resident 1's Treatment Administration Records (TARs...
Read full inspector narrative →
Aug 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0563
(Tag F0563)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure its ' visitation policy was in compliance with the federal regulation to not limit resident visitation hours.
This def...
Read full inspector narrative →
Jul 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide the written Bed-Hold Policy Notice to the resident and her ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Transfer
(Tag F0626)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, observation, and record review, the facility failed to ensure it implemented its' policy regarding Bed-Holds...
Read full inspector narrative →
Apr 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure the assessment entries were accurate for one of six sampled...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure:
1. That Licensed Vocational Nurse 1 (LVN 1) had the specif...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to schedule a Registered Nurse (RN) for at least 8 consecutive hours a day aside from the Director of Nursing for six of the seve...
Read full inspector narrative →
Jan 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed implement an individualized person-centered plan of care...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a resident received appropriate treatment and ...
Read full inspector narrative →
Jul 2021
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to incorporate and respect the goals, preferences, and pe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to revise a care plan for one of one resident (Resident 31) who had a poor oral intake.
This deficient practice had the potentia...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to follow physician orders to deliver oxygen at 1 to 2 liters per min (L/min) for one of three sampled residents (Resident 63).
...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to maintain acceptable parameters of nutritional status for one of one resident (Resident 31) as indicated in Resident 31's care ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure available medications stored are not expired w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure nursing staff followed physician orders and the facility's p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of one sampled resident (Resident 124 )rec...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to implement its policy to ensure weekly Covid-19 (Coronavirus disease, a severe respiratory illness caused by virus and spread from person to...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to:
1. Treated four of 10 sampled residents (Residents 1...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interview, and record review, the facility failed to provide an accident free environment and adequate su...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0800
(Tag F0800)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed implement its policies and procedures to ensure food safety and to meet residents' dietary needs when:
1) Cold foods such as dai...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the safety of storing, preparing, distributing, and serving food in accordance with professional standards and its pol...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. During an observation on 7/19/21 at 8:51 a.m., Resident 6's urine catheter drainage bag was observed touching the floor.
Duri...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0912
(Tag F0912)
Minor procedural issue · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure that 19 out of 29 resident rooms (Rooms 1, 2, 3, 4, 5, 6, 7 ,8, 9, 10, 11, 12, 15, 16, 17, 18, 19, 20, and 21) met the...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 40% turnover. Below California's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 2 life-threatening violation(s), $55,450 in fines, Payment denial on record. Review inspection reports carefully.
- • 56 deficiencies on record, including 2 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $55,450 in fines. Extremely high, among the most fined facilities in California. Major compliance failures.
- • Grade F (16/100). Below average facility with significant concerns.
About This Facility
What is Ocean Pointe Healthcare Center's CMS Rating?
CMS assigns OCEAN POINTE HEALTHCARE CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Ocean Pointe Healthcare Center Staffed?
CMS rates OCEAN POINTE HEALTHCARE CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 40%, compared to the California average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Ocean Pointe Healthcare Center?
State health inspectors documented 56 deficiencies at OCEAN POINTE HEALTHCARE CENTER during 2021 to 2025. These included: 2 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 52 with potential for harm, and 2 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
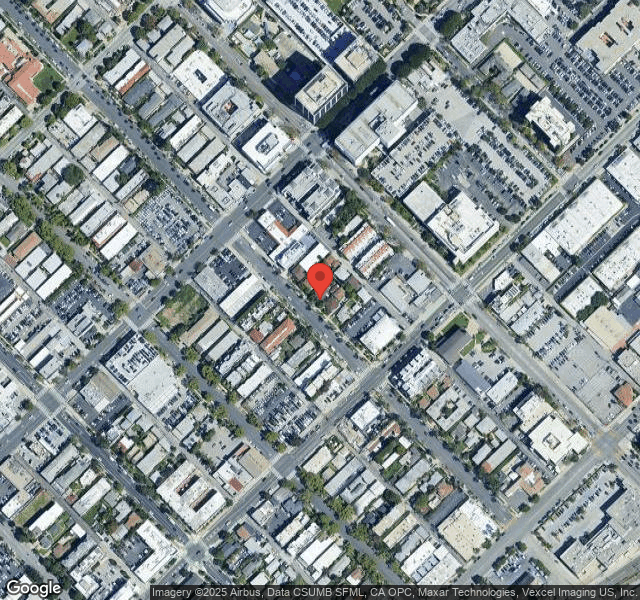
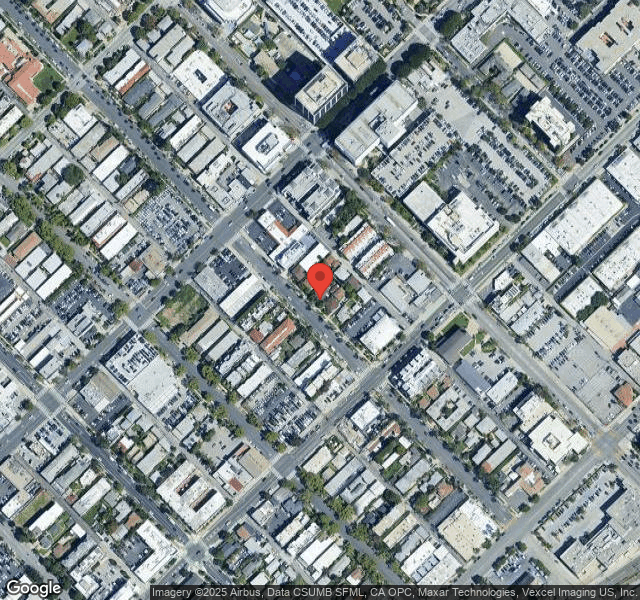
Who Owns and Operates Ocean Pointe Healthcare Center?
OCEAN POINTE HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by ASPEN SKILLED HEALTHCARE, a chain that manages multiple nursing homes. With 72 certified beds and approximately 60 residents (about 83% occupancy), it is a smaller facility located in SANTA MONICA, California.
How Does Ocean Pointe Healthcare Center Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, OCEAN POINTE HEALTHCARE CENTER's overall rating (2 stars) is below the state average of 3.1, staff turnover (40%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Ocean Pointe Healthcare Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Ocean Pointe Healthcare Center Safe?
Based on CMS inspection data, OCEAN POINTE HEALTHCARE CENTER has documented safety concerns. Inspectors have issued 2 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in California. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Ocean Pointe Healthcare Center Stick Around?
OCEAN POINTE HEALTHCARE CENTER has a staff turnover rate of 40%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Ocean Pointe Healthcare Center Ever Fined?
OCEAN POINTE HEALTHCARE CENTER has been fined $55,450 across 1 penalty action. This is above the California average of $33,633. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Ocean Pointe Healthcare Center on Any Federal Watch List?
OCEAN POINTE HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.