ARBOL HEALTHCARE CENTER OF SANTA ROSA




Over 2 years since last inspection. Current conditions may differ from available data.
Arbol Healthcare Center of Santa Rosa has a Trust Grade of C, which means it is average and sits in the middle of the pack among nursing homes. It ranks #738 out of 1,155 facilities in California, placing it in the bottom half, and #13 out of 18 in Sonoma County, indicating that there are only a few local options that perform better. The facility's trend is stable, with 45 concerns reported consistently over the last two years, which suggests ongoing issues that have not improved. Staffing is a relative strength with a rating of 4 out of 5 stars, but the turnover rate is concerning at 54%, significantly higher than the California average of 38%. Notably, the center has not incurred any fines, which is a positive sign, and it boasts better RN coverage than 81% of similar facilities, providing reassurance that registered nurses are present to catch potential issues. However, there are critical weaknesses to consider. Recent inspections revealed that the facility failed to store food safely, putting residents at risk for gastrointestinal diseases, and dietary staff were not trained adequately in food safety practices. Additionally, there was a serious concern regarding the failure to report an incident of alleged resident abuse within the required time frame, which could hinder timely investigations and potentially endanger residents. Overall, while there are strengths in staffing and regulatory compliance, families should weigh these against the concerning findings and the facility's average performance.
- Trust Score
- C
- In California
- #738/1155
- Safety Record
- Low Risk
- Inspections
- Holding Steady
- Staff Stability ⚠ Watch
- 54% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most California facilities.
- Skilled Nurses ✓ Good
- Each resident gets 64 minutes of Registered Nurse (RN) attention daily — more than 97% of California nursing homes. RNs are the most trained staff who catch health problems before they become serious.
- Violations ⚠ Watch
- 45 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, fire safety.
The Bad
Below California average (3.1)
Below average - review inspection findings carefully
Near California avg (46%)
Higher turnover may affect care consistency
The Ugly 45 deficiencies on record
Feb 2025
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure supervision to prevent accidents for one resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure patient care equipment was functioning and maintained under sanitary conditions when oxygen therapy equipment provided...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected multiple residents
Based on interview, and facility record review, the facility failed to have a Registered Nurse (RN) performing the function of the Director of Nursing (DON) on a full-time basis to provide oversight a...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure a facility-wide assessment (a review of a facility's infrastructure, resident population, and services to determine needed resources...
Read full inspector narrative →
Jul 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to develop and implement a person-centered care plan wit...
Read full inspector narrative →
Jun 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to honor (Resident 1) choice for the refusal of end-of-li...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based observation, interview and record review, the facility failed to store, prepare, distribute, and serve food in accordance with professional standards of food service safety when:
1) the facility...
Read full inspector narrative →
Jan 2024
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to report one incident of resident abuse to authorities ...
Read full inspector narrative →
Oct 2023
7 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Resident 20
During an interview on 10/23/23 at 10:58 a.m., Resident 20 stated she would have preferred to administer her own med...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record reviews, the facility failed to provide care and services in accordance with standa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure it had a medication error rate of less than 5%, when three of 30 medications were not given according to the physician'...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to honor the food preferences for two of three residents sampled for food (Residents 1 and 4). These failures resulted in Residen...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on dietary staff observations, dietary staff interviews and dietary document review, the facility failed to ensure staff c...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on kitchen observations, dietary staff interview, and dietary document review, the facility failed to ensure safe dietetic services as evidence by 1) meat not thawed according to the facility's ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record reviews, the facility failed to maintain an effective infection prevention and cont...
Read full inspector narrative →
Jan 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure that the Certified Nursing Assistants (CNAs) comply with the facility ' s Policy & Procedure on dress code to keep the ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that resident received necessary respiratory care and servic...
Read full inspector narrative →
Dec 2021
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure medication self-administration assessment was p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
2. During a clinical record review for Resident 8, the Clinical Notes Reports indicated the facility sent Resident 8 to the hospital on the following dates and times:
- On 7/5/21 at 12:43 a.m.
- On 7...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During a clinical record review for Resident 8, the Clinical Notes Reports indicated the facility sent Resident 8 to the hosp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement a person-centered care plan for two of eight sampled resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to review and revise the Care Plan quarterly for one of 8 sampled residents (Resident 8) when:
1) One nurse was checking gastric residual when...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed provide assessment and treatment for one of 8 sampled residents (Resident 8) when the nurses did not assess Resident 8 before an...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure safe and secured medication administration and ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
3. During an observation on 11/29/21, at 9:06 a.m., Licensed Staff N was observed in the nursing station wearing yellow gown, face shield and N-95 respirator (protective device used in filtration of a...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to ensure residents and staff knew the complaint and grievance process and failed to post complaint and grievance notices in a ma...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected most or all residents
3) During a clinical record review for Resident 8, the hospital's document titled Skilled Nursing Facility Orders the facility received on 10/2/21 indicated a doctor's order for Atropine 1% eye drop (...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure food safety in accordance with standards of practice when 1) there was a lack of accurate labeling/dating of thawing m...
Read full inspector narrative →
Jul 2019
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide visual privacy during a wound dressing change for one of 12 sampled residents (Resident 123), when her privacy curtai...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to submit the results of its investigation of an allegation of abuse to the California Department of Public Health (the Department) within fiv...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to timely notify the Long Term Care Ombudsman (LTC Ombudsman, organiza...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete the baseline care plan within 48 hours of admission for on...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop an activities care plan for one of 12 sampled residents (Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to update the care plans of one to 12 sampled residents (Resident 4) w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide services to prevent falls to one of 12 sampled residents (R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, facility nursing staff failed to document administration of controlled medications and had no system for regularly tracking discontinued controlled ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to maintain complete and accurate medical records for one of 12 sampled residents (Resident 12), when the facility did not consistently and ac...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility nurses failed to identify the residents before administration of medications. This failure could potentially lead to residents receivin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to carry out residents' restorative nursing treatments as ordered for four sampled (Residents 5, 6, 9 and 10) and four un-sampled residents (R...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide interventions to prevent pressure ulcers for one of 12 samp...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to monitor the medication carts and the medication room stock, for outdates, when one expired medication was found in a medicati...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
3) During an observation and concurrent interview on 7/10/19 at 10:40 a.m., Licensed Nurse B changed the dressing on Resident 123's lower leg wound while Resident 123 lay in bed. Licensed Nurse B wash...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure its menus met nutritional adequacy when:
1) the menus lacked a cook's spreadsheet to guide dietary staff in assembling food trays, a...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to store, prepare, distribute and serve food, in accordance with professional standards for food service safety, when:
1) Dietary...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility Quality Assurance and Performance Improvement (QAPI) committee failed to identify quality issues in dietary and pharmacy services. This failure preve...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • No fines on record. Clean compliance history, better than most California facilities.
- • 45 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • Grade C (50/100). Below average facility with significant concerns.
About This Facility
What is Arbol Healthcare Center Of Santa Rosa's CMS Rating?
CMS assigns ARBOL HEALTHCARE CENTER OF SANTA ROSA an overall rating of 2 out of 5 stars, which is considered below average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Arbol Healthcare Center Of Santa Rosa Staffed?
CMS rates ARBOL HEALTHCARE CENTER OF SANTA ROSA's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 54%, compared to the California average of 46%.
What Have Inspectors Found at Arbol Healthcare Center Of Santa Rosa?
State health inspectors documented 45 deficiencies at ARBOL HEALTHCARE CENTER OF SANTA ROSA during 2019 to 2025. These included: 45 with potential for harm.
Who Owns and Operates Arbol Healthcare Center Of Santa Rosa?
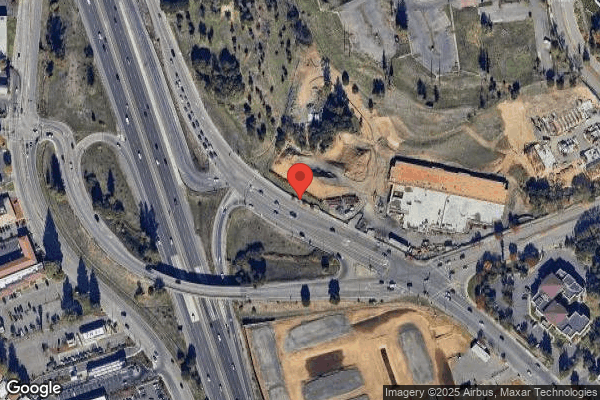
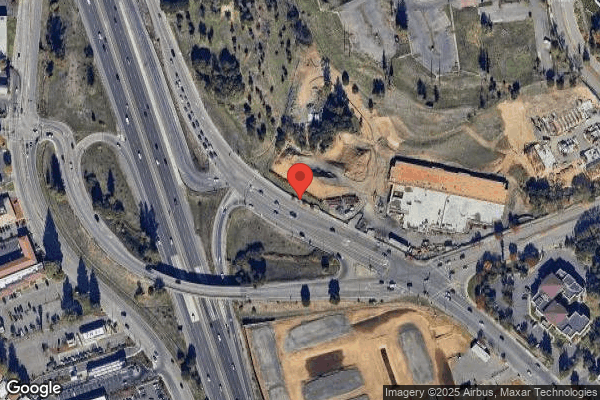
ARBOL HEALTHCARE CENTER OF SANTA ROSA is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 45 certified beds and approximately 25 residents (about 56% occupancy), it is a smaller facility located in SANTA ROSA, California.
How Does Arbol Healthcare Center Of Santa Rosa Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, ARBOL HEALTHCARE CENTER OF SANTA ROSA's overall rating (2 stars) is below the state average of 3.1, staff turnover (54%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Arbol Healthcare Center Of Santa Rosa?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Arbol Healthcare Center Of Santa Rosa Safe?
Based on CMS inspection data, ARBOL HEALTHCARE CENTER OF SANTA ROSA has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Arbol Healthcare Center Of Santa Rosa Stick Around?
ARBOL HEALTHCARE CENTER OF SANTA ROSA has a staff turnover rate of 54%, which is 8 percentage points above the California average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Arbol Healthcare Center Of Santa Rosa Ever Fined?
ARBOL HEALTHCARE CENTER OF SANTA ROSA has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Arbol Healthcare Center Of Santa Rosa on Any Federal Watch List?
ARBOL HEALTHCARE CENTER OF SANTA ROSA is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.