THE GROVE POST-ACUTE CARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
The Grove Post-Acute Care Center has a Trust Grade of D, indicating below-average performance with some concerning issues. It ranks #923 out of 1155 facilities in California, placing it in the bottom half of the state, and #248 out of 369 in Los Angeles County, suggesting limited local options that are better. The facility is currently improving, reducing issues from 27 in 2024 to just 4 in 2025, which is a positive trend. Staffing is a strength, with a turnover rate of 20%, significantly lower than the state average, indicating that staff members are likely to stay and build relationships with residents. However, the facility has encountered serious problems, such as serving improperly prepared food to residents on modified diets, which could pose a choking hazard, and failing to manage waste disposal properly, increasing the risk of infection. While there are some strengths, these significant weaknesses raise concerns for families considering this home for their loved ones.
- Trust Score
- D
- In California
- #923/1155
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ✓ Good
- 20% annual turnover. Excellent stability, 28 points below California's 48% average. Staff who stay learn residents' needs.
- Penalties ✓ Good
- $17,345 in fines. Lower than most California facilities. Relatively clean record.
- Skilled Nurses ○ Average
- RN staffing data not reported for this facility.
- Violations ⚠ Watch
- 81 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Low Staff Turnover (20%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (20%)
28 points below California average of 48%
Facility shows strength in quality measures, staff retention, fire safety.
The Bad
Below California average (3.1)
Below average - review inspection findings carefully
Below median ($33,413)
Minor penalties assessed
The Ugly 81 deficiencies on record
Aug 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to report the allegation of a visitor-to-resident sexual abuse (sexual behavior or a sexual act forced upon a woman, man, or child without th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow professional standards of practice for one of three sampled residents (Resident 1) by failing to ensure licensed nurses and social s...
Read full inspector narrative →
Feb 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to report allegation of staff-to-resident abuse within two hours to the State Survey Agency (SSA- the agency that inspects long-term care faci...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to maintain accurate and complete medical record for one of four sampled residents (Resident 1).
This deficient practices had the potential to...
Read full inspector narrative →
Dec 2024
22 deficiencies
1 IJ
CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0805
(Tag F0805)
Someone could have died · This affected 1 resident
Based on observation, interview, and record review, the facility failed to prepare food in a form designed to meet individual needs (requirements that a person has in order to be well such as food) fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** b. During a review of Resident 39's admission Record, the admission Record indicated the facility admitted Resident 39 on 8/6/20...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to inform residents and their responsible party about their right to formulate an advance directive (a written statement of a pe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the physician was notified that azithromycin (antibiotic-medication used to treat infection) was not available on 12/10/2024, 12/11/...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide a safe and homelike environment to one of one sampled resident (Resident 114) by failing to ensure the resident's wal...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** b. During a review of Resident 39's admission Record, the admission Record indicated the facility admitted Resident 39 on 8/6/20...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide the necessary treatment and services for two ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** b. During a review of Resident 23's admission Record, the admission Record indicated the facility admitted Resident 23 on 1/12/2...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide a Registered Nurse (RN) for eight consecutive hours on 11/1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the resident was free from any significant medication error for one of three sampled residents (Resident 214) by not following the p...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed to ensure the Infection Preventionist (IP) was competent in implementing the facilities infection control program by failing to:
1.
Follow the...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide pharmaceutical services (including procedures...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure kitchen staff were routinely trained and evaluated for competency (measurable pattern of training, skills, experience,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to follow the menu and did not meet nutritional needs of 62 of 63 residents on regular (diet with no restriction) and puree textu...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to prepare food by methods that conserved flavor and appearance for breakfast when:
a.
Cook 1 did not follow the recipe for cof...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure safe and sanitary food storage and food prepar...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0841
(Tag F0841)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to designate a Medical Director (MD) for 12 months of 12 months (12/30/2023 to 12/30/2024) whose responsibilities were outlined in a job descr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2.
During a review of Resident 39's admission Record, the admission Record indicated the facility admitted Resident 39 on 8/6/2...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** c. During a review of Resident 52's admission Record, the admission Record indicated the facility admitted Resident 52 on 6/13/2...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to dispose garbage and refuse properly by:
a.
Not putting a plastic liner in the trash can used in the kitchen.
b.
Not comple...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Assessment Accuracy
(Tag F0641)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to accurately code the Minimum Data Set (MDS-a resident assessment too...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0911
(Tag F0911)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to meet the requirement for no more than four resident p...
Read full inspector narrative →
Jul 2024
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement its infection control policy by failing to:...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility:
1. Failed to provide documented evidence staff were provided education regarding the benefits and potential risks associated with coronavirus disease...
Read full inspector narrative →
Jul 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow the facility's policy and procedure on submitting the 5-day report to the State Survey Agency (SSA) within five working days of the ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure safe provision of pharmaceutical services for one of three sampled residents (Resident 3) by failing to ensure the res...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain one of four means of egress (designated exit door) was free from obstructions.
This deficient practice had the poten...
Read full inspector narrative →
Dec 2023
20 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide care in a manner that promoted dignity and respect for one of one sampled resident (Resident 19) by failing to ensure...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure the resident's responsible party was informed in advance prior to the use of the bed side rails for one of one sampled...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure the call light was within reach for one of eight sampled residents (Resident 108).
This deficient practice had the pote...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0577
(Tag F0577)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to promote the resident rights to examine the results of the most recent survey (a survey to determine compliance with state and...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review facility failed to maintain privacy of confidential information when Licensed Vocational Nurse 2 (LVN 2) left an electronic health record (EHR- a digi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to develop and implement a comprehensive care plan for one of three sampled residents (Resident 46) by:
a. Failing to develop a care plan for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to update a resident's comprehensive care plan after the resident's nephrostomy (a procedure to drain urine from the kidney using a tube) tube...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop and implement a discharge care plan for a resident who was ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to provide the appropriate treatment and services to a resident who has a suprapubic catheter (a type of catheter that is inserte...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0691
(Tag F0691)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to provide the appropriate treatment and services to a resident who has a colostomy (a surgical procedure that brings on end of the large intes...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident who received dialysis (process of removing waste products and excess fluid from the body when the kidneys stop working pr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure one of one sampled resident (Resident 12) was free from unnecessary medication when Licensed Vocational Nurse 3 (LVN 3...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to complete Surveillance Data Collection Forms for one of five residents (Resident 46) in the 9/2023 log.
This deficient practice had the pote...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide care and services in accordance with professional standards of practice that will meet each resident's physical, ment...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure that licensed nursing staff have the specific competency (measurable pattern of knowledge, abilities, behaviors in order to perform ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to provide the services of a registered nurse (RN) for at least eight consecutive hours a day as indicated in the facility's policy.
This defi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure safe storage and handling of medications by fa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to implement their facility assessment (determines the resources necessary to care for residents competently during the day-to-day operations ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement infection prevention and control practices ...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0911
(Tag F0911)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to meet the requirement for no more than four residents ...
Read full inspector narrative →
Oct 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement their COVID-19 (a disease caused by a virus named SARS-Co...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to implement infection control practices for five of seven sampled residents by:
1. Failing to conduct a complete screening of vi...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure one of five residents sampled received the pneumococcal vaccine (a drug that helps the immune system develop immunity from pneumococ...
Read full inspector narrative →
Sept 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to implement their policy and procedure by failing to ensure the Responsible Party (RP) was informed for one of four sampled residents (Reside...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of four sampled residents (Resident 1) was free of unnecessary medication when Resident 1 was given ivermectin (an anti-parasiti...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to conduct skin scraping on one of four sampled resident (Resident 1) when on 9/1/2023 Resident 1 was identified with a rash on their back, ch...
Read full inspector narrative →
Aug 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure that the resident's at risk for fall or injury care plan interventions were revised timely when the resident no longer required the ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure a resident was free from physical restraints (any manual method, physical or mechanical device, material or equipment ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to meet professional standards of quality care for one o...
Read full inspector narrative →
Jun 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure one of three sampled residents (Resident 1) was free of any significant medication errors (administration of medications which was n...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to provide pharmaceutical services (including procedures that assure the accurate acquiring, receiving, dispensing, and administering of all d...
Read full inspector narrative →
Dec 2021
19 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** b. A review of the admission Record indicated Resident 30 was admitted to the facility, on 3/16/2020 and readmitted on [DATE], w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to rightfully inform in advance of the risks and benefits of the proposed plan in medication for one of one resident (Resident 47). Resident 4...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on interview and record review, the Social Services Director (SSD) failed to ensure a grievance (a formal complaint) was completed for a resident to staff complaint for one of one resident (Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the Social Services Director (SSD) failed to ensure a grievance (a formal complaint) was completed for a resident to staff complaint for one of one resident (Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on interview and record review, the Social Services Director (SSD) failed to ensure a grievance (a formal complaint) was completed for a resident to staff complaint for one of one resident (Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure residents received care consistent with profess...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow the physician's order regarding oxygen therapy...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to treat a resident's pain in a timely manner when the licensed nursing staff did not communicate with each other, for one (Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify the physician regarding an absent bruit (sound of blood pass...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the Medication Regimen Review (MRR - review of a resident's ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to adequately monitor for complications that include signs and symptom...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** b. A review of Resident 42's admission Record indicated Resident 42 was admitted to the facility on [DATE], and was most recentl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to observe infection control measures for two out of two sampled residents (Residents 8 and 9) by failing to clean and disinfect...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure care was provided in accordance with professional standards of practice as evidenced by Licensed Vocational Nurse 4 (LVN 4) did not ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** b. A review of Resident 6's admission Record indicated the resident was admitted into the facility on [DATE], and was most recen...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** b. A review of Resident 39's admission Record indicated the resident was admitted to the facility on [DATE] and was readmitted o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to follow the menu as written for residents with a physician's order for a regular texture diet (foods that have a regular textur...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review the facility failed to:
1. Ensure the kitchen's ice machine was free from dark spots on the inside of the ice machine.
2. Ensure the ice machine air ...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0911
(Tag F0911)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to meet the requirement for no more than four residents p...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 20% annual turnover. Excellent stability, 28 points below California's 48% average. Staff who stay learn residents' needs.
- • Multiple safety concerns identified: 1 life-threatening violation(s), Payment denial on record. Review inspection reports carefully.
- • 81 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $17,345 in fines. Above average for California. Some compliance problems on record.
- • Grade D (41/100). Below average facility with significant concerns.
About This Facility
What is The Grove Post-Acute's CMS Rating?
CMS assigns THE GROVE POST-ACUTE CARE CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is The Grove Post-Acute Staffed?
CMS rates THE GROVE POST-ACUTE CARE CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 20%, compared to the California average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at The Grove Post-Acute?
State health inspectors documented 81 deficiencies at THE GROVE POST-ACUTE CARE CENTER during 2021 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 76 with potential for harm, and 4 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
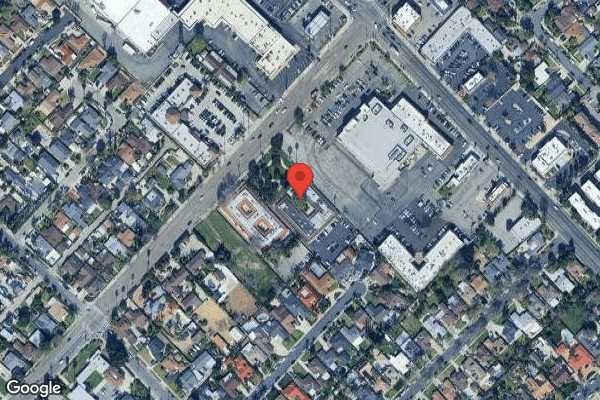
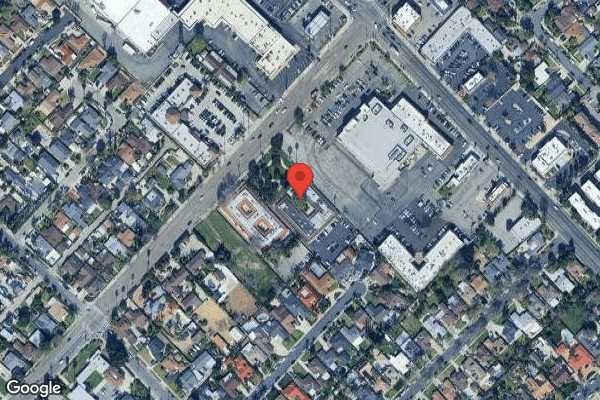
Who Owns and Operates The Grove Post-Acute?
THE GROVE POST-ACUTE CARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 75 certified beds and approximately 61 residents (about 81% occupancy), it is a smaller facility located in SYLMAR, California.
How Does The Grove Post-Acute Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, THE GROVE POST-ACUTE CARE CENTER's overall rating (2 stars) is below the state average of 3.1, staff turnover (20%) is significantly lower than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting The Grove Post-Acute?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is The Grove Post-Acute Safe?
Based on CMS inspection data, THE GROVE POST-ACUTE CARE CENTER has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in California. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at The Grove Post-Acute Stick Around?
Staff at THE GROVE POST-ACUTE CARE CENTER tend to stick around. With a turnover rate of 20%, the facility is 25 percentage points below the California average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly.
Was The Grove Post-Acute Ever Fined?
THE GROVE POST-ACUTE CARE CENTER has been fined $17,345 across 1 penalty action. This is below the California average of $33,252. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is The Grove Post-Acute on Any Federal Watch List?
THE GROVE POST-ACUTE CARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.