VERMONT HEALTHCARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Vermont Healthcare Center in Torrance, California has received a Trust Grade of F, indicating significant concerns about the facility's care standards. It ranks #1147 out of 1155 facilities in California, placing it in the bottom half, and #362 out of 369 in Los Angeles County, meaning there are only a few local options that are better. Unfortunately, the facility is experiencing a worsening trend, increasing from 29 issues in 2024 to 37 in 2025. Staffing is rated at 3 out of 5 stars, which is average, but the turnover rate of 50% is concerning compared to the state average of 38%. The facility has also accrued $120,486 in fines, which is higher than 84% of California facilities, indicating ongoing compliance problems. Specific incidents include failures in resident care, such as a resident with paraplegia not being safely transferred from bed to a shower chair, resulting in a fall risk. Another resident developed a serious skin injury due to not being turned and repositioned as required, and a high-risk resident was not properly monitored to prevent falls, which could lead to serious harm. While there are some strengths in staffing coverage, the overall issues highlight significant weaknesses that families should carefully consider.
- Trust Score
- F
- In California
- #1147/1155
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 50% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $120,486 in fines. Higher than 51% of California facilities. Some compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 35 minutes of Registered Nurse (RN) attention daily — about average for California. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 95 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below California average (3.1)
Significant quality concerns identified by CMS
Near California avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
The Ugly 95 deficiencies on record
Jul 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0627
(Tag F0627)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of three sampled residents (Resident 1), who resided at ...
Read full inspector narrative →
Jul 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to assist one of three residents (Resident 2) to shower at least twice ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure medication was not left on one of three residen...
Read full inspector narrative →
Jul 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement care plan interventions for one of one resident (Resident...
Read full inspector narrative →
May 2025
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure the resident, who had a diagnosis of paraplegia (loss of mo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure the physician for one of three sampled residents (Resident ...
Read full inspector narrative →
Mar 2025
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete a change of condition (CIC/COC- noticeable shift or altera...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to wear proper personal protective equipment ([PPE] spec...
Read full inspector narrative →
Mar 2025
26 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the resident did not develop a deep tissue skin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the failed to ensure a preadmission screening resident review (PASARR) level II was comple...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement a care plan for one of three sampled residents (Resident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure one of four reviewed residents (Resident 218) had a Interdisc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of five sampled residents (Resident 154) w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to assist resident who receive proper assistive devices to maintain hearing abilities for one of three sample residents (Resident 20).
This fa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure one of two sampled residents, Residents 22 intra...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure resident who were receiving hemodialysis (clin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected 1 resident
Based interview, and record review the facility failed to ensure staffing information was accurate and current on 1/13/25,2/12/25, 3/9/25 and 3/10/25.
This deficient practice had the potential to aff...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of three residents (Resident 78) was provi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of three sampled residents (Resident 112) is free of unn...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation interview and record review the facility failed to ensure Resident 10 was provided with lower dentures.
Thi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility's Quality Assessment and Assurance Committee ([QAA] develop and implement appropriate plans of action to correct identified quality deficiencies) fai...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement its protocol for antibiotic stewardship program (coordina...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to maintain a functional call light ( device or button th...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to complete a Change of Condition (COC) and notify physician for two o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide services to five of 11 reviewed residents (Re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to:
1.Ensure there was sufficient Restorative Nursing Ai...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure that medication error rate was less than five ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the intravenous (IV, into the vein) antibiotic (medicines that fight bacterial infections) medications had labels in a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, and interview the facility failed to ensure the ice machine had an air gap for back flow (the unwanted reverse flow of contaminated water) prevention.
This failure had the potent...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility did not provide accurate documentation for five of 11 reviewed ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. During a review of Resident 134's Minimum Data Set ([MDS] a federally mandated resident assessment tool), dated 12/11/2024, t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure laundry washers were maintained in operational condition for 160 of 160 residents by failing to ensure the washer temp...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility:
1.Failed to ensure morning medication administrations were done on time in the subacute unit (SAU, a nursing unit that provides a leve...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure two of three reviewed residents were free of...
Read full inspector narrative →
Feb 2025
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure the resident, who was a high risk for falls and injuries, di...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure accurate picture of the resident ' s status on the Minimum D...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to observe infection control measures on one of three sam...
Read full inspector narrative →
Oct 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure medical records were complete, legible, organized, and were r...
Read full inspector narrative →
Sept 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review the facility failed to ensure one of three sampled residents (Resident 3) had tracheostomy...
Read full inspector narrative →
Aug 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to notify the responsible party of change of condition, when it was d...
Read full inspector narrative →
Jul 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Transfer
(Tag F0626)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to re-admit one of three sampled residents (Resident 1),...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to implement Enhanced Standard Precautions (ESP), precaut...
Read full inspector narrative →
May 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure free from abuse by facility staff, for one of three sampled ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to document, for one of three sampled resident's (Resident 1), records accurately and completely when Resident 1 had a change of condition.
T...
Read full inspector narrative →
Apr 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to protect one of three sampled residents (Resident 1), right to be fr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure an allegation of abuse were reported to the state agency (De...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure Licensed Vocational Nurse (LVN) 1 had training on preventing ...
Read full inspector narrative →
Mar 2024
17 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Incontinence Care
(Tag F0690)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure the resident, who had a history of urinary tract infection (U...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of five sampled residents (Resident 30) had a completed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of six sampled residents (Resident 62) was...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to ensure the licensed nurses completed one of 25 sampled residents (Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to accurately assess and follow through with the Preadmission Screenin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** During observation, interview, and record review the facility failed to ensure one of 31 sampled residents (Resident 137) receiv...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** During observation, interview, and record review the facility failed to provide personal care and implement fall precaution inte...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide an effective pain management on one of six sa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of three sampled residents (Resident 109) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0790
(Tag F0790)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to follow up on necessary dental services for one of fiv...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide care in a manner that maintained or enhanced a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide activities of daily living ( activities relat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the emergency kit ([E-kit], a small quantity of medications kit that can be dispensed when pharmacy services are not a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure that its medication error rate was less than 5...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure refrigerator temperature readings were in a correct range of 36 to 46 degrees Fahrenheit (°F- unit of temperature) ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected most or all residents
During observation, interview, and record review the facility failed to ensure Dietary Aide (DA) 1 had the appropriate training on how to operate the dishwasher machine.
This deficient practice had th...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to implement and maintain infection control measures by:
...
Read full inspector narrative →
Jan 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure the resident, who was a high risk for falls, di...
Read full inspector narrative →
Jan 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to initiate a care plan for fall risk for one of three sampled reside...
Read full inspector narrative →
Oct 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Transfer
(Tag F0626)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to re-admit one of two sampled residents (Resident 1), when Resident 1...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** nterview, and record review, the facility failed to:
A. Prevent Resident 2 from being slap on his right thigh by Resident 1 who ...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide appropriate treatment and services to maintai...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure one of two sampled resident's (Resident 2) drug records for ...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure electrical wheelchair was charged for one of t...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure one Certified Nursing Assistant (CNA) demonstra...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure one of three sampled residents (Residents 2)'s...
Read full inspector narrative →
Jun 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to observe infection control measures for two of three s...
Read full inspector narrative →
May 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement an individualized person-centered plan of c...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure supervision was provided to prevent elopement (...
Read full inspector narrative →
Apr 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to report an allegation of emotional and psychological abuse to the St...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to conduct an investigation and provide the investigation within five ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure one of three sampled residents (Resident 1) was free from m...
Read full inspector narrative →
Apr 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to notify and consult the physician when Resident 1 had nausea, abdomi...
Read full inspector narrative →
Mar 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to ensure an Advanced Health Care Directive ([AHCD] a written stateme...
Read full inspector narrative →
Dec 2022
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the resident, who was smoking on the patio, was...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Intakes: CA00811382, CA00811713
Based on interview and record review the facility failed to ensure Resident 1 was transferred to...
Read full inspector narrative →
Feb 2022
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide incontinent (loss of voluntary control over u...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to communicate to five of 22 sampled residents (Resident 17, 34, 93,...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to notify physician when the resident continued to refuse...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide the necessary care and services to attain or ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure respiratory care was consistent with profession...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to follow its policy and ensure eight of 22 sampled residents (Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review facility failed to ensure one of 22 sampled residents (Resident 50) was provid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
facility failed to put date open on house stock medication
FACILITY
Medication Storage and Labeling
Based on observation, interview, and record review, the facility failed to label two out of 2 medica...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to promptly provide requested denture adhesive for 11 mon...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Social Worker
(Tag F0850)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to employ a qualified social worker on a full-time basis that met the ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** C. During a review of Resident 106 admission record. The admission record indicated, Resident 106 was admitted to the facility o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility's Quality Assessment and Assurance (QAA) and Quality Assurance Performance Improvement (QAPI) committee failed to:
1. Employ a qualified social worke...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 6 harm violation(s), $120,486 in fines, Payment denial on record. Review inspection reports carefully.
- • 95 deficiencies on record, including 6 serious (caused harm) violations. Ask about corrective actions taken.
- • $120,486 in fines. Extremely high, among the most fined facilities in California. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Vermont Healthcare Center's CMS Rating?
CMS assigns VERMONT HEALTHCARE CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within California, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Vermont Healthcare Center Staffed?
CMS rates VERMONT HEALTHCARE CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 50%, compared to the California average of 46%.
What Have Inspectors Found at Vermont Healthcare Center?
State health inspectors documented 95 deficiencies at VERMONT HEALTHCARE CENTER during 2022 to 2025. These included: 6 that caused actual resident harm and 89 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Vermont Healthcare Center?
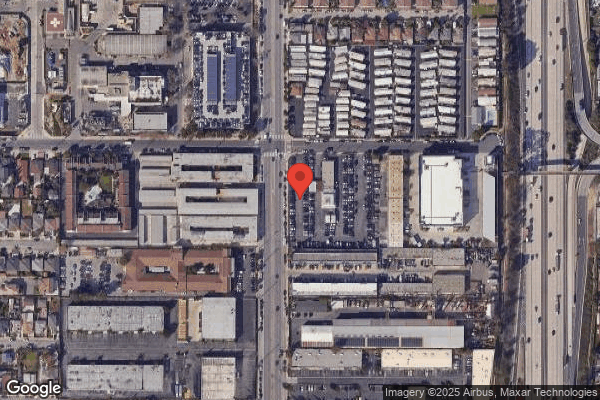
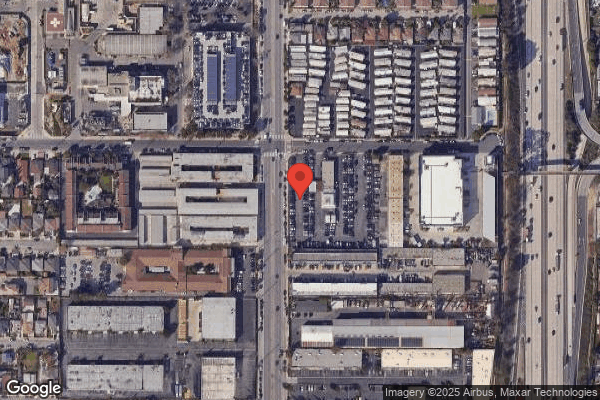
VERMONT HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 200 certified beds and approximately 164 residents (about 82% occupancy), it is a large facility located in TORRANCE, California.
How Does Vermont Healthcare Center Compare to Other California Nursing Homes?
Compared to the 100 nursing homes in California, VERMONT HEALTHCARE CENTER's overall rating (1 stars) is below the state average of 3.1, staff turnover (50%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Vermont Healthcare Center?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Vermont Healthcare Center Safe?
Based on CMS inspection data, VERMONT HEALTHCARE CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in California. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Vermont Healthcare Center Stick Around?
VERMONT HEALTHCARE CENTER has a staff turnover rate of 50%, which is about average for California nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Vermont Healthcare Center Ever Fined?
VERMONT HEALTHCARE CENTER has been fined $120,486 across 4 penalty actions. This is 3.5x the California average of $34,284. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Vermont Healthcare Center on Any Federal Watch List?
VERMONT HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.