CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record reviews, review of facility documentation, and interviews for 1 of 6 residents at risk for...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record reviews, review of facility documentation, and interviews for 1 of 6 residents at risk for elopement (Resident # 8), the facility failed to implement interventions for a resident identified at risk for elopement. Resident #8 was able to exit the facility without staff knowledge and was found 0.6 miles away from the facility by law enforcement. This failure resulted in a finding of Immediate Jeopardy (IJ). The finding includes:
Resident #8's diagnoses included paranoid schizophrenia, dementia, depression, anxiety disorder and psychosis.
The clinical record identified Person # 3 as Resident # 8's conservator.
The quarterly Minimum Data Set (MDS) assessment, dated 2/23/2024, indicated Resident #8 as moderately cognitively impaired and noted no wandering behaviors had occurred at the time of the assessment.
The Resident Care Plan (RCP) dated 3/14/2024 for at risk of leaving the facility with a desire to go home, noted tendency to cut off wander guard. Interventions included: the application of a wander guard bracelet, picture identification and description of Resident #8 to all departments and staff located near exits (including the reception desk) to re-direct the resident if seen near an exit, encourage the resident to come with staff and assist Resident #8 with finding his/her own room, bathroom and nursing unit as needed.
On 5/9/2024 the facility transferred Resident # 8 to the hospital at 5:59 PM for a psychiatric evaluation due to behavioral changes. Prior to the transfer at approximately 5:30 PM Resident # 8's wander guard was removed by staff.
An elopement and wandering evaluation, completed and dated 5/30/2024 (readmission) at 8:21 PM, indicated Resident #8 was at risk for wandering and elopement.
The readmission nursing assessment, dated 5/30/2024 at 8:39 PM, failed to reflect the nursing staff implemented measures to address Resident #8's risk for elopement.
A Brief Interview for Mental Status (BIMS) assessment, completed 5/31/2024 at 11:32 AM, indicated Resident #8 was severely cognitively impaired.
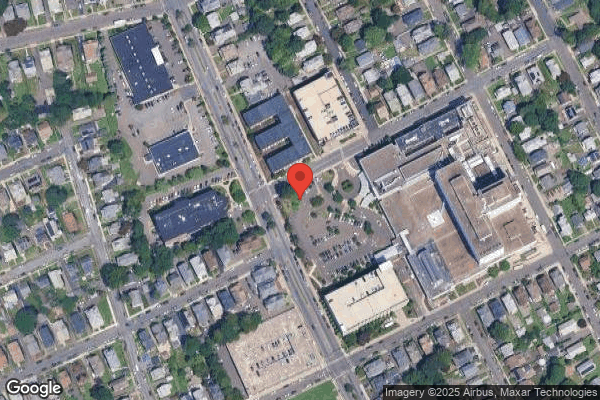
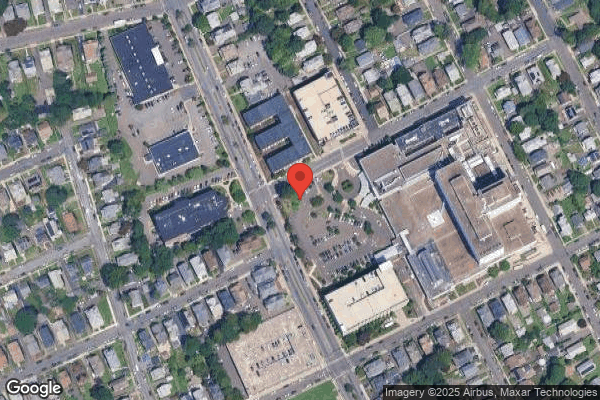
The Emergency Medical System (EMS) Run sheet, dated 6/16/2024 at 5:06 PM, indicated the EMS team was called to respond at 5:01 PM and arrived at 5:06 PM to find Resident #8 on a side street in the same city (0.6 miles away from the facility, across a 4-lane divided busy street, outside temperature was 73 degrees and no precipitation) with a bystander. The EMS form indicated Resident #8 was crying and stated s/he could not go on and did not want to live anymore. The EMS form further indicated Resident # 8 was assisted to a stretcher and transported to the closest hospital arriving at the acute care facility at 5:19 PM.
A nursing progress note, dated 6/16/2024 at 11:49 PM, indicated at about 7:30 PM the writer was alerted by the charge nurse Resident #8 was not found in his/her room. The note indicated at the same time a phone call was received from an acute care facility indicating Resident #8 was at the hospital. The note further indicated the Director of Nursing Services (DNS), Administrator, Advanced Practice Registered Nurse (APRN) were notified, and a message was left for the responsible party to call the facility for an update on Resident #8's status.
Observation on 6/17/2024 at 9:59 AM identified Resident #8's bedroom was located at the end of the hallway near the elevators that have a coded keypad to access usage.
A review of the facility investigation, dated 6/16/24, included a handwritten document with Dietary Aide #2's name, no date/time and no signature, the statement indicated Dietary Aide #2 was on the elevator after delivering the last meal truck to the fourth floor. The elevator stopped on the third floor and a resident unknown to the Dietary Aide #2 got on the elevator and the elevator stopped at the first floor. Dietary Aide #2 indicated s/he did not know where the resident on the elevator went when the elevator stopped on the first floor.
The facility investigation statement dated 6/16/2024 (no time) written by Nurse Aide (NA) #3 indicated Resident #8 was seen walking around in the hall. At 7:00 PM when s/he went to Resident #8's room to provide care the resident was not there at which time NA # 3 reported to the charge nurse the resident was not present.
The facility investigation dated 6/16/2024 (no time), with Licensed Practical Nurse (LPN #13) indicated the nurse aide assigned to Resident #8 reported to him/her at 7:10 PM s/he was unable to locate Resident #8 who was not in his/her room or bathroom. LPN #13 indicated looking for the resident everywhere. LPN #13 further indicated after speaking with the Receptionist #1, a call came to the unit from the hospital that identified Resident #8 was there.
On 6/17/2024 at 10:55 AM the Administrator indicated the facility was currently investigating a Reportable Event involving Resident #8 who eloped (left unattended and without staff knowledge) from the facility on Sunday 6/16/2024. The location where Resident #8 was found, and exact time was unknown to the administrator at that time. The Administrator indicated Resident #8 went down the elevator with Dietary Aide # 2 and then exited the building out the front entrance. Although Receptionist #1 was on duty, and a book containing pictures and descriptions of residents at risk of eloping (including Resident # 8) was present at the desk.
Receptionist # 1 was unaware Resident # 8 had exited the building. The Administrator indicated the police found Resident #8 on 6/16/24 and brought the resident to an acute care facility. This resulted in a finding of Immediate Jeopardy (IJ).
On 6/17/2024 an interview and record review with the DNS at 11:20 AM indicated it is facility policy to page a Dr. Hunt (emergency paging system to locate a missing person) over the intercom system in the event a resident was missing. The DNS indicated staff did not follow facility policy Dr. Hunt at the time Resident # 8 was identified missing. Review of the physician's orders, Medication Administration Record (MAR) and Treatment Administration Record (TAR) with the DNS from 5/30/2024(re-admission date) through 6/16/2024 failed to reflect a physician's orders for re-application of Resident # 8's wander guard to monitor the resident's location per facility policy for a resident at risk for elopement. The DNS was unable to provide evidence that a wander guard bracelet was applied to Resident # 8 between 5/30/2024 through 6/16/2024 or any other interventions to monitor Resident # 8's location in the facility.
Interview with Receptionist #1 on 6/17/2024 at 4:35 PM indicated Resident #8 must have been with a visitor and exited the building when s/he pressed the button to unlock the front entrance door for the visitor to leave. Receptionist # 1 also indicated the incident occurred on Father's Day which was a busy day because s/he was watching the computer monitor looking forward outside the window where the transportation vehicles pick up and drop off residents and watching for visitors wanting to enter and exit the facility. Receptionist #1 further indicated s/he pressed the button to unlock the front entrance door not realizing a resident at risk was with the visitor. Receptionist # 1 further indicated s/he was aware of the elopement risk book and location. However, the day of the incident s/he did not see a wander guard on anyone and did not hear an alarm go off when s/he let the visitor exit.
Interview on 6/18/2024 with the Director of Nursing Services (DNS) and Administrator at 1:30 PM indicated the staff noted Resident #8 on the unit at the beginning of the shift (3:00PM) and actively walking on the unit around 3:00 PM-4:00 PM. The DNS and Administrator further indicated through staff interviews they were able to identify that Resident #8 was on the elevator with Dietary Aide #2 around 4:30 PM to 4:45 PM before meals arrived onto the unit about 5:00 PM. The Administrator indicated s/he viewed the video surveillance on 6/17/2024 to determine the time Resident #8 was on the elevator with Dietary Aide #2 and the surveillance video showed Resident #8 exiting the front entrance of the building at 4:37 PM.
Interview with the DNS and the Administrator on 6/18/2024 at 1:35 PM indicated at time of Resident # 8's readmission on [DATE] the facility had 8 wander guard bracelets available for use and currently the same 8 bracelets are available for use now. The DNS indicated when a resident is admitted /readmitted an elopement evaluation is completed. If found at risk for elopement the nurse who completed the evaluation is responsible for notifying the supervisor that a wander guard is needed for the resident. The wander guard bracelets are locked in the supervisor's office so the supervisor would need to provide the bracelet to the nurse for application to the resident. Resident #8 was evaluated and found at risk for elopement on 5/30/2024, the charge nurse should have followed the facility policy, updated the supervisor regarding the outcome of the evaluation, obtained physician orders to apply a wander guard bracelet and notified responsible party.
The hospital's Initial Psychiatric Evaluation, dated 6/20/2024 at 9:37 AM, indicated Resident #8 was found on the street after eloping in an impulsive and disorganized manner from the skilled nursing facility. The evaluation further indicated Resident #8 was found on the street disheveled and tearful and brought to the Emergency Department for an evaluation. Resident # 8 was assessed and verbalized at the hospital s/he wanted to self-harm without a clear plan at which time Resident # 8 was admitted to the acute care facility under a Physician's Emergency Certificate (PEC).
Interview with Licensed Practical Nurse (LPN #14), on 6/20/24 at 9:45 AM, indicated s/he was working on 5/30/2024 when Resident #8 was readmitted . LPN #14 further indicated s/he collected data for the completion of the elopement evaluation on 5/30/2024 but s/he did not inform the supervisor Resident #8 was at risk for elopement. LPN # 14 also indicated the license staff is responsible for applying wander guard bracelet to residents. LPN #14 could not explain why s/he did not notify the supervisor Resident # 8 required a wander guard bracelet on 5/30/24.
On 6/20/2024 at 10:21 AM interview with Registered Nurse (RN #6) who was the RN supervisor on 5/30/2024 when Resident #8 was readmitted to the facility. RN #6 indicated the evaluations (including elopement risk) are completed by the charge nurses and indicated the admitting nursing supervisor is responsible for reviewing the evaluations and if a resident is at risk put safety precautions in place per the policy.
On 6/20/2024 at 11:20 AM interview and facility document review with the DNS indicated the 24-hour supervisor paper report for 5/30/2024 through 6/16/2024 did not reference Resident #8 was at risk for elopement or the need for a wander guard bracelet.
Interview with RN #6 on 6/20/24 at 11:20 with DNS further indicated s/he did not receive any report regarding Resident #8 from the off going supervisor.
An interview on 6/20/2024 at 1:05 PM with Nurse Aide (NA #3) assigned to Resident #8 indicated s/he last saw Resident #8 around 5:00 PM or just before the incident. Resident # 8 had not made any attempts to leave the unit that evening. NA#3 indicated s/he noticed Resident #8 was missing at around 7:00 PM when s/he went to Resident # 8's room to provide PM care and was told by the charge nurse to look for the resident.
Interview with Licensed Practical Nurse (LPN) #13 on 6/24/2024 at 8:58 AM indicated s/he did not call Dr. Hunt before looking downstairs first and talking to Receptionist #1. LPN # 13 further indicated once s/he was back on the unit s/he received a call from the hospital informing her/him Resident #8 was at the hospital.
On 6/25/2024 at 8:58 PM an interview with LPN #13 s/he on 6/16/2024 worked from 7:00 AM through 11: 00 PM as the charge nurse caring for Resident #8. LPN #13 indicated s/he saw Resident #8 walking in the hall on the unit at 3:00 PM when s/he arrived on duty and recalls a nurse aide indicated Resident #8 had been crying. LPN #13 administered Resident #8 her/his 4:00 PM medications and the resident was in her/his room at that time. Later Resident #8 came to LPN #13 in the hall during medication pass and complained of a headache at which time s/he LPN # 13 provided medication to relieve the headache. At 7:00 PM the nurse aide reported Resident #8 was missing at which time s/he stopped the medication pass and began to look for Resident # 8.
Attempts to interview Dietary Aide #2 during the survey were unsuccessful.
The facility policy titled Elopement consists of screening all residents for risk of elopement, implement preventive strategies for those identified at risk, institute measures for resident identification at the time of admission, and conduct missing resident procedures as warranted. The policy defines elopement as the inability of a resident who is not capable of protecting him or herself from harm to successfully leave the facility unsupervised and unnoticed and who may enter harm's way.
The Administrator was presented with the Immediate Jeopardy Template on June 16, 2024, at 5:20 PM for F 689 Free of Accident Hazards/supervision /devices.
The facility submitted the following IJ removal plan on June 17 and 18, 2024:
1. The facility conducted an in-house audit of all residents at risk for elopement on 6/17/24 and 6/18/24.
2. All staff have been in serviced on the facility elopement and wander guard policy, Dr. Hunt policy, Medical Doctor and family notification and Leave of Absence policy and indicated all policy remains current.
3. All staff have been educated if a resident on admission and readmission triggers for at risk for elopement to place a wander guard on the resident. Staff have been educated to obtain a physician's order for the wander guard, to conduct checks per facility policy.
4. An Interdisciplinary meeting was held to review all residents at risk for elopement and current residents with wander guards.
5. RN supervisor and charge nurse will check all wander guards for placements, to ensure evaluations are completed, physician's orders for wander guard and care plans when a resident is noted at risk for elopement upon admission and readmission.
6. Wander guard book check for pictures on all units
7. The Receptionist will report and review all residents at risk for elopement at mealtime and at shift change.
8. Dr. Hunt Drill conducted 6/17/24 on the 3:00 PM to 11:00 PM shift
9. Audit tool created for all residents with wander guards for tracking and placement. The facility will perform evaluation on admission, readmission, random audits will be conducted weekly time 4 and monthly times 3. The DNS and designee.
a. On 6/17/2024 an interview and record review with the DNS at 11:20 AM indicated staff did not follow procedure for paging a Dr. Hunt at the time Resident # 8 was identified missing on 6/16/24.
On 6/20/2024 at 10:21 AM interview with RN #6 indicated she did not hear a page for Dr. Hunt to indicate a resident was missing.
An interview on 6/20/2024 at 1:05 PM with NA # 3 indicated s/he did not hear a Dr. Hunt paged.
Interview on 6/20/2024 at 6:06 PM with supervisor, RN #7 who worked 7:00 AM -7:00 PM on 6/16/2024 indicated s/he did not hear a page for Dr. Hunt initiated while she was on duty.
On 6/25/2024 at 8:58 PM an interview via phone with. LPN #13 identified no Dr. Hunt was paged when the resident was noted missing.
b. A review of the facility removal plan for the Immediate Jeopardy dated 6/18/24 identified RN # 9 the 3-11 PM supervisor on 6/19/24 at 3 :25 PM placing the transmitter near the wander guard device without pressing the button to activate the device to validate functioning per manufacture directions. Interview with RN # 9 identified s/he had been educated recently on the facility policy and procedure for transmitter use and thought she was doing it correct. Interview with the DNS and the Administrator at the time of the incident identified they would conduct an in-house education with all RN supervisors again to ensure they are aware of how to use the transmitter to test for wander guard functioning every shift. This resulted in the facility not having the removal of the Immediate Jeopardy.
c. Observations on 6/20/24 on the 3-11 PM at 4:45 PM to 5:00 PM of the receptionist desk where the location of residents at risk for elopement picture book is located failed to identify Resident # 88 picture in the book per facility removal plan for Immediate Jeopardy. Interview with the Administrator and DNS on 6/20/2024 identified that they have several residents who wander guard location is on the wheelchair and not the resident's persons such as: Residents # 17, # 30, # 55, # 75 and # 97 wander guards are located on the resident's wheelchair. The Administrator also indicated that Resident # 88 refused to have his/her picture taken. The Administrator further indicated s/he did not inform the resident's conservator and the physician of the resident's refusal to have his/her picture taken for at risk for elopement. After inquiry, the Administrator indicated s/he would follow up with the conservator this evening and the physician. The DNS and Administrator also indicated they would follow up with Residents #17, # 30, # 55, # 75 and # 97 location of wander guard by having a discussion in an interdisciplinary meeting to ensure the facility is appropriately monitoring and supervising resident at risk for elopement. However, the state agency could not remove the facility Immediate Jeopardy based on the removal plan was not implemented.
2. Interview with the DNS and the Administrator on 6/18/2024 at 1:35PM identified the function of the wander guard bracelets for all residents are checked on the night shift by the nursing supervisor per physician's orders and the facility obtained a transmitter from a sister facility to initiate the checks and a log to track functioning of the wander guard because there was not one in facility prior to the 6/16/2024 incident of Resident #8 elopement. The Administrator indicated the transmitter is used to check the function of the wander guard bracelets for all residents during the night shift. However, the transmitter had been broken since the middle of April 2024.
An interview with the Administrator on 6/18/20254 at 2:00PM indicated the delay in obtaining another transmitter was due to administrative staff member resigning without notice. She/he became sidetracked and did not order the transmitter to check the function of the wander guard bracelets. The Administrator re-ordered the transmitter on 6/17/2024, after surveyor inquiry and provided an invoice (146 days later.
Interview with LPN #14 on 6/20/24 at 9:45 AM indicated working 11-7 AM shift at the facility identified s/he was not made aware the transmitter to check the function of the residents wander guard bracelets was broken.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, and staff interviews, for 1 of 2 residents observed for accidents for (Resident #9...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, and staff interviews, for 1 of 2 residents observed for accidents for (Resident #99), the facility failed to ensure a resident was assessed for self-medication administration. The findings include:
Resident #99's diagnoses included diabetes mellitus, arthritis, and depression.
The nursing evaluations for self-administration of medications dated 12/22/2023 and 2/27/2024 indicated Resident # 99 did not desire to self-administer medications.
The MDS assessment dated [DATE] identified Resident #99 was cognitively intact exhibiting no behaviors of rejecting care. The MDS further identified the resident as independent with transferring and requiring setup assistance for eating.
A care plan dated 6/8/2024 identified Resident #99 had a deficit in performing Activities of Daily Living (ADL) due to generalized weakness. Interventions included: providing assistance when needed and keeping the call bell and other needed items within reach. The care plan did not identify the resident who was able to self-administer medications.
On 6/13/2024 at 10:07 AM, observation of Resident #99 identified two medication cups containing pills next to the resident's breakfast tray on the tray table. One medication cup contained two white oblong tablets, three round white tablets, one orange capsule, two small green tablets, and one green oblong tablet. The second medication cup contained one yellow oblong tablet, six round white tablets of various sizes, and one white half-tablet. An interview with Resident #99 indicated that s/he had requested the medications to be left in his/her room while s/he ate breakfast. Resident #99 also indicated s/he separated the medications into two cups; one cup contained the medications they were going to take, and the second cup contained the medications Resident # 99 did not want to take that morning.
On 6/13/2024 at 10:20 AM, an interview with Licensed Practical Nurse ( LPN) #10 identified that during the morning medication pass, the resident requested his/her medication be left at the bedside so Resident # 99 could see the medications and had agreed to call the nurse when s/he was ready to swallow the medications. LPN#10 indicated s/he left the medications with the resident because it was the resident's preference. However, LPN#10 indicated he did not know Resident # 99 had been evaluated for self-administration of medication. LPN #4 further identified that when a resident can self-administer medication, there would be an order and a care plan.
On 6/17/2024 at 3:37 PM a chart review and interview with the Director of Nursing Services ( DNS) identified Resident #99 had not been evaluated for self-administration of medication. Additionally, the DNS indicated a resident would first be evaluated to self -administer medication if the resident wanted to have his/her pills at the bedside.
The facility policy for oral medication administration indicated that the nurse administering medication should stay with the resident until the resident has swallowed the medication.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review and staff interviews for 1 of 3 residents reviewed for pain for (Resident #100), the facility fa...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review and staff interviews for 1 of 3 residents reviewed for pain for (Resident #100), the facility failed to ensure the physician was notified of a resident new and ongoing pain after a fall. The findings include:
Resident #100 was admitted on [DATE] with a diagnosis that included dementia, repeated falls, and osteoporosis.
A quarterly MDS assessment dated [DATE] identified Resident #100 was severely cognitively impaired and required extensive assistance for bed mobility. Additionally, the MDS indicated the resident could not verbalize the presence of pain but had vocal complaints and protective body movements or postures as indicators of pain. The MDS further indicated the resident received hospice care and exhibited daily indicators of pain or possible pain.
A physician's order dated 6/6/2022 directed to assess the resident's pain every hour and medicate if needed per order for pain, and to follow up with hospice/MD if the pain is uncontrolled with the regimen.
A physician's order dated 6/14/2022 directed to administer 5 milligrams (mg) of Morphine every 4 hours scheduled for pain. Additionally, physician orders dated 6/14/2022 directed to administer 5 MG of Morphine every hour as needed for moderate pain and 10 mg of morphine every hour as needed for severe pain.
A nursing progress note by LPN #12 dated and signed on 6/15/2022 at 4:02 PM indicated Resident # 100 appeared to be holding his/her left leg and exhibited symptoms of pain at the beginning of the shift (7:00 AM to 3:00 PM shift). The nursing progress note further indicated that a left hip x-ray taken during the shift 7-3 PM shift identified a fracture, and the resident was taken to the hospital on 6/15/2024 at 2:24 PM.
A review of the Medication Administration Record (MAR) from 6/1/2022 through 6/15/2022 identified Resident #100 was evaluated for pain every hour, and the resident's pain was consistently at zero from 6/1/2022 through 6/15/2022. On 6/15/2022, Resident #100 was evaluated as having a pain level of 5 (moderate pain) on 6/15/2022 at the following times: 3:00 AM, 4:00 AM, 5:00 AM, 6:00 AM, and 7:00 AM, the MAR indicated the resident received a scheduled dose of Morphine at 4:00 AM.
A further review of nursing progress notes did not identify an assessment by a registered nurse addressing the new continued pain. Additionally, the nursing progress notes do not indicate that a provider was contacted when the resident first exhibited moderate pain at 3:00 AM (one hour after the resident's unwitnessed fall) or at 4:00 AM when the resident was noted to have difficulty sleeping and having facial expressions of pain. The nursing progress notes did not indicate that the APRN was notified of the resident's new ongoing pain post-fall until 6:30 AM.
A nursing progress note by the nursing supervisor Registered Nurse (RN#4) dated and signed on 8/15/2022 at 2:25 AM identified Resident #100 had an unwitnessed fall on 8/15/2022 at 1:45 AM. The nursing note indicated the resident had facial grimaces with no complaint of pain post fall and that Advanced Practice Registered Nurse (APRN #3) had been updated.
A nursing progress note by LPN #11 dated and signed 8/15/2022 at 6:48 AM identified at 4:00 AM Resident #100 was having difficulty sleeping and exhibiting facial expressions of pain. Additionally, the nursing note indicated at 6:30 AM the resident was awake with continued expressions of pain. The nursing note further indicates LPN #11 made attempts to call the hospice service with no return call back.
A further review of nursing progress notes did not identify an assessment by a registered nurse addressing the new continued pain. Additionally, the nursing progress notes do not indicate physician or APRN was contacted when the resident first exhibited moderate pain at 3:00 AM (one hour after the resident's unwitnessed fall) or at 4:00 AM when the resident was noted to have difficulty sleeping and having facial expressions of pain. The nursing progress notes did not indicate that the APRN was notified of the resident's new ongoing pain post-fall until 6:30 AM.
In an interview on 6/18/2024 at 1:39 PM, LPN# 11 indicated she did not recall details of the incident and the only thing she remembered was Resident # 100 had fallen and had received an x-ray.
Attempts to contact RN #4 were unsuccessful.
Attempts to contact APRN #3 were unsuccessful.
On 6/18/2024 at 1:56 PM an interview with APRN #1 indicated he did not know if a physician was notified during the night shift when the resident was experiencing pain. Additionally, APRN #1 indicated that his rationale for ordering an x-ray in the day shift on 6/15/2022 was due to the resident's fall and continued complaints of pain.
On 6/20/2024 at 11:20 AM, an interview with the DNS indicated there should have been an intervention addressing Resident #100's ongoing pain and staff should have investigated why the resident was having increased pain, especially considering the resident had a recent fall.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the clinical record, facility documentation, facility policy and interviews for 1 of 1 sampled resident (Resi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the clinical record, facility documentation, facility policy and interviews for 1 of 1 sampled resident (Resident #189) reviewed for abuse, the facility failed to ensure resident was free from verbal abuse from staff. The findings include:
Resident #189's diagnoses included adjustment disorder, type 2 diabetes mellitus and hypotension.
The quarterly Minimum Data Set (MDS) assessment dated [DATE] identified the resident as cognitive intact and required supervision for eating, limited assistance with bed mobility and transfers. MDS additionally indicated Resident 189 presented with feeling of hopelessness and feeling down/depressed.
The care plan dated 5/19/22 identified Resident #189, has signs of history of depression. Interventions included: to encourage verbalization of feelings, provide emotional support as needed and for psychiatric consult.
The nursing progress note dated 6/23/22 at 9:33 PM identified a report was received that a resident was being verbally abused by the charge. The note further identified an investigation was initiated and the police were notified.
The Reportable Event dated 6/23/22 indicated Licensed Practical Nurse (LPN #6) called Resident #189 an prick and asshole.
Interview with psychiatric consultant supervisor on 6/18/24 at 11:35AM regarding the incident reported on 6/23/22 identified the agency no longer has a record of the incident. She indicated the staff who witnessed the incidents is no longer employed with the company and whatever information the agency had about the incident was given to the nursing home.
Interview with the Director of Nursing Services (DNS) on 6/18/24 at 12:35 PM who was not in her/his current position at the time of the incident, the facilities procedures direct the staff be removed from the resident's care, an investigation started, which include interviewing all persons involved, alerting the Administrator, notifying the police and state agency. The DNS also indicated the perpetrator would be placed on administrative leave until further notice.
Interview with Administrator on 6/18/24 at 12:45 PM identified the incident was reported by psychiatric consultant staff. She reported the incident occurred during a 7-3 PM shift and expressed statements were taken from staff and residents regarding the allegations, the staff was removed from the resident's care pending investigation. LPN # 6 is no longer employed by the facility secondary to substantiated verbal abuse.
Attempts to interview the psychiatric consultant were unsuccessful.
Attempts to interview LPN #6 were unsuccessful.
Review of the Abuse Prohibition policy dated September 2020 with update 2024 indicated, the facility has the responsibility to ensure that each resident has the right to be free from abuse.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on, review of the clinical record, facility documentation, facility policy and interviews for the 1 of 1 sampled resident ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on, review of the clinical record, facility documentation, facility policy and interviews for the 1 of 1 sampled resident (Resident #189) reviewed for abuse, the facility failed to report and allegation of verbal abuse to an outside state agency timely. The findings include:
Resident #189's diagnoses included adjustment disorder, type 2 diabetes mellitus and hypotension.
The quarterly Minimum Data Set (MDS) assessment dated [DATE] identified the resident as cognitive intact and required supervision for eating, limited assistance with bed mobility and transfers. MDS additionally indicated Resident 189 presented with feeling of hopelessness and feeling down/depressed.
The care plan dated 5/19/22 identified Resident #189, has signs of history of depression. Interventions included: to encourage verbalization of feelings, provide emotional support as needed and for psychiatric consult.
The nursing progress note dated 6/23/22 at 9:33 PM identified a report was received that a resident was being verbally abused by the charge. The note further identified an investigation was initiated and the police were notified.
The Reportable Event dated 6/23/22 indicated Licensed Practical Nurse (LPN #6) called Resident #189 an prick and asshole.
Interview with Administrator on 6/20/24 at 11:01 AM indicated I don't believe it was reported to other state agency outside Department of Public Health.
Attempts to contact the other state agency were unsuccessful.
Review of the Abuse Prohibition policy dated September 2020 with update 2024 indicated, if resident abuse has been confirmed a copy of the mandated reporter Form for Long-term care Facilities should be sent to the Connecticut Department of Social Service.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record reviews, facility documentation, facility policy and interviews for 1 of 6 residents reviewed for elope...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record reviews, facility documentation, facility policy and interviews for 1 of 6 residents reviewed for elopement ( Resident #8), the facility failed to revised the resident's plan care timely regarding the need for wander guard device and for 1 2 of sampled residents, (Resident #88) reviewed for hospice, the facility failed to ensure the resident care plan was revised to reflect a change in code status for a resident receiving end of life care. The findings included:
1. Resident #8's diagnoses included paranoid schizophrenia, dementia, depression, anxiety disorder and psychosis.
The clinical record identified Person # 3 as Resident # 8's conservator.
The quarterly Minimum Data Set (MDS) assessment, dated [DATE], indicated Resident #8 as moderately cognitively impaired and noted no wandering behaviors had occurred at the time of the assessment.
The Resident Care Plan (RCP) dated [DATE] for at risk of leaving the facility with a desire to go home, noted tendency to cut off wander guard. Interventions included: the application of a wander guard bracelet, picture identification and description of Resident #8 to all departments and staff located near exits (including the reception desk) to re-direct the resident if seen near an exit, encourage the resident to come with staff and assist Resident #8 with finding his/her own room, bathroom and nursing unit as needed.
On [DATE] the facility transferred Resident # 8 to the hospital at 5:59 PM for a psychiatric evaluation due to behavioral changes. Prior to the transfer at approximately 5:30 PM Resident # 8's wander guard was removed by staff.
An elopement and wandering evaluation, completed and dated [DATE] (readmission) at 8:21 PM, indicated Resident #8 was at risk for wandering and elopement.
The readmission nursing assessment, dated [DATE] at 8:39 PM, failed to reflect the nursing staff implemented measures to address Resident #8's risk for elopement.
A Brief Interview for Mental Status (BIMS) assessment, completed [DATE] at 11:32 AM, indicated Resident #8 was severely cognitively impaired.
The Emergency Medical System (EMS) Run sheet, dated [DATE] at 5:06 PM, indicated the EMS team was called to respond at 5:01 PM and arrived at 5:06 PM to find Resident #8 on a side street in the same city (0.6 miles away from the facility, across a 4-lane divided busy street, outside temperature was 73 degrees and no precipitation) with a bystander. The EMS form indicated Resident #8 was crying and stated s/he could not go on and did not want to live anymore. The EMS form further indicated Resident # 8 was assisted to a stretcher and transported to the closest hospital arriving at the acute care facility at 5:19 PM.
A nursing progress note, dated [DATE] at 11:49 PM, indicated at about 7:30 PM the writer was alerted by the charge nurse Resident #8 was not found in his/her room. The note indicated at the same time a phone call was received from an acute care facility indicating Resident #8 was at the hospital. The note further indicated the Director of Nursing Services (DNS), Administrator, Advanced Practice Registered Nurse (APRN) were notified, and a message was left for the responsible party to call the facility for an update on Resident #8's status.
Observation on [DATE] at 9:59 AM identified Resident #8's bedroom was located at the end of the hallway near the elevators that have a coded keypad to access usage.
A review of the facility investigation, dated [DATE], included a handwritten document with Dietary Aide #2's name, no date/time and no signature, the statement indicated Dietary Aide #2 was on the elevator after delivering the last meal truck to the fourth floor. The elevator stopped on the third floor and a resident unknown to the Dietary Aide #2 got on the elevator and the elevator stopped at the first floor. Dietary Aide #2 indicated s/he did not know where the resident on the elevator went when the elevator stopped on the first floor.
A review of the clinical record from [DATE] through [DATE] failed to reflect that the facility had revised Resident # 8's plan of care to address the need for a wander guard per elopement assessment and per facility practice.
Interview with Licensed Practical Nurse (LPN #14), on [DATE] at 9:45 AM, indicated s/he was working on [DATE] when Resident #8 was readmitted . LPN #14 further indicated s/he collected data for the completion of the elopement evaluation on [DATE] but s/he did not inform the supervisor Resident #8 was at risk for elopement. LPN # 14 also indicated the license staff is responsible for applying wander guard bracelet to residents. LPN #14 could not explain why s/he did not notify the supervisor Resident # 8 required a wander guard bracelet on [DATE].
On [DATE] at 10:21 AM interview with Registered Nurse (RN #6) who was the RN supervisor on [DATE] when Resident #8 was readmitted to the facility. RN #6 indicated the evaluations (including elopement risk) are completed by the charge nurses and indicated the admitting nursing supervisor is responsible for reviewing the evaluations and if a resident is at risk put safety precautions in place per the policy and updating the plan of care.
2. Resident #88's diagnoses included dementia and failure to thrive.
The admission clinical record identified Resident #88 was not responsible for self.
The physician's orders dated [DATE] directed Resident #88 start receiving hospice services and Do Not Resuscitate, DNR (no life saving measures).
The Resident Care Plan (RCP) dated [DATE] identified Resident #88's Advanced Directives which directed DNR/DNI (do not intubate or provide an artificial airway to assist with breaths).
The Advanced Directive Code Status dated [DATE] identified Resident #88 would have all resuscitation efforts performed (in the event s/he required life saving measures).
A social worker progress note dated [DATE] at 3:20 PM identified a meeting was held with the Interdisciplinary Team and responsible party. Resident #88 was admitted into hospice. Advanced Directive were reviewed, and the responsible party was considering changing the code status to Full Code/ CPR (cardiopulmonary resuscitation or life saving measures). Hospice would be contacted to follow up with the responsible party to discuss code status and plan of care.
A nursing progress note dated [DATE] at 12:05 PM identified Advanced Directives were discussed with Resident #88 who expressed wishes for DNR/ DNI (do not intubate). The responsible party made the final decision for a full code and Resident #88's clinical record was updated.
The physician's orders dated [DATE] directed Resident #88 as Full Code (implement life saving measures if necessitated).
The Resident Care Plan was not revised to reflect the change in Resident #88's code status.
An interview and clinical record review with Social Worker (SW #1) with the Corporate Social Worker in attendance on [DATE] at 12:34 PM identified the Interdisciplinary Team (IDT) was responsible for overseeing a resident receiving hospice services. The responsible party had considered a Full Code status, so SW #1 referred them to hospice social services for discussion. SW #1 identified she did not follow up on the resident's code status any time between [DATE] to present but noted the code status was changed to Full Code on [DATE].
An interview with the Corporate Social Worker on [DATE] at 12:34 PM identified that social services were involved in the hospice referral process and care planning of services and the IDT managed ongoing care. S/he did not know if hospice spoke with the responsible party regarding the resident's code status. However, s/he would expect the care plan to match the code status.
A review of the facility policy for care planning identified the care plan was developed by the IDT for each resident and includes measurable objectives and timelines to accommodate preferences, special medical, nursing, and psychological needs. The care plan is evaluated and revised as needed or at least quarterly.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on clinical record reviews, facility documentation, facility policy and interviews for 1 of 3 sampled residents (Resident...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on clinical record reviews, facility documentation, facility policy and interviews for 1 of 3 sampled residents (Resident #6) reviewed for nutrition, the facility failed to evaluate the medical needs of a resident identified with significant weight loss in a timely manner and for 1 of 3 sampled residents (Resident #82) reviewed for dental services, the facility failed to ensure a resident was assessed for safe food consumption while awaiting dental services for a broken denture and for 1 of 1 resident ( Resident # 84) reviewed for utilization of ACE wrap, the facility failed to apply the ACE wrap as prescribed and for 1 of 3 sampled residents, (Resident #88) reviewed for hospice, the facility failed to ensure a change in code status was communicated to a community specialty service for a resident receiving end of life care and for 1 of 3 residents for ( Resident # 126) who utilized oxygen, the facility failed to obtain a physician's order for the oxygen. The findings include:
1. Resident #6 's diagnoses included dementia, anemia, and hypertension.
The annual Minimum Data Set, MDS assessment dated [DATE] identified Resident #6 required one person assist with bed mobility and supervised assist with eating.
The Resident Care Plan dated 1/5/24 identified Resident #6 had the potential for impaired nutrition related to impaired cognition and advanced age. Interventions directed to assist with meals as needed, monitor intake and complete nutritional assessments as needed.
The Nutritional assessment dated [DATE] identified Resident #6's current weight was 136.7 lbs, noted impaired cognition, advanced age, variable intake while on a mechanically altered diet. Laboratory results reflect adequate hydration and slightly depleted protein stores with extra protein provided in supplements. Resident #6's Body Mass Index or BMI (measures body fat) was 24.2 (normal 18.5 to 24.9) and within her/his desired weight range. There were no new recommendations.
The Weight record dated 4/16/24 identified a documented weight of 113lbs. reflecting a 23.7 lb. or 17.34% weight loss from the previous month with no documented re-weight.
An Advanced Practice Registered Nurse, APRN progress note dated 4/24/24, eight days following the significant weight discrepancy identified since last review, weights were trending down to 110.4 lbs. from 137.5 lbs. in March 2024. Per record review intake was 25-50% of meals with set-up assist with self-feeding. Resident #6 was identified with moderate protein calorie malnutrition as evidenced by BMI of 19.55, loss of body fat and muscle mass, labile weight and appetite which was anticipated with advancing disease. The plan included increasing supplements to 240 cc, starting Remeron 7.5. mg to help with appetite, monitor weight weekly and encourage small snacks in between meals.
An internal dietitian to nursing communication form dated 4/25/34, nine days after the identified discrepancy, identified on 3/1/24, a weight loss greater than 10% loss in 180 days. New ancillary orders included adding Power Cereal at breakfast, diet was downgraded to mechanical soft diet and a dental consult was submitted.
A Nutritional Progress note dated 5/9/24 identified a weight of 109 lbs reflecting a 20.7%, 28.5 lb weight loss from the previous month. Power Cereal was added at breakfast.
The physician's orders dated 5/2/24 directed a level II dysphagia mechanically altered diet) moist and soft-textured foods that are easy to chew). The physician's orders dated 5/10/24 directed Power Cereal at breakfast for weight loss.
An interview with APRN #2 during the survey identified she previously provided services to the facility and had evaluated Resident #6 for weight loss. APRN #2 identified that although she may have been notified at an earlier time regarding Resident #6's significant weight loss, she would typically wait to put in any new orders until she was completed a monthly review for a resident long standing dementia with anticipated weight loss as Resident #6.
An interview with Medical Doctor, MD #2 (primary physician) on 6/20/24 at 11:00 AM identified that although no harm resulted in the delay, he would expect residents to receive a medical evaluation as soon as the weight discrepancy was known.
A review of the facility policy for Food First/Nutrition/Weight dated 8/2015 with update 2024 directed that weights are documented in the clinical record and a significant weight loss/gain of 5% in 30 days or 10% on 6 months the interdisciplinary team, dietitian, physician, and family are notified. The weight loss is reviewed by the dietary team and responsible party and interventions implemented as appropriate and monitored weekly.
2. Resident #82 's diagnoses included dementia, anorexia, and dysphagia.
The quarterly Minimum Data Set assessment dated [DATE] identified Resident #82 as severely cognitively impaired and independent with activities of daily living skills.
A quarterly Nursing assessment dated [DATE] identified Resident #82 exhibited no chewing or swallowing difficulties and had upper dentures that had no broken areas and were worn regularly.
The physician's orders dated 6/8/24 directed a regular diet with thin liquids.
The Resident Care Plan dated 6/9/23 identified Resident #82 used partial dentures. Interventions directed to monitor/document/report any signs of oral/dental problems needing attention.
A social service progress note dated 6/9/23 identified the responsible party had questions regarding dentures and indicated the resident be referred to the dentist for an evaluation of the lower dentures.
An electronic correspondence (email) to the Director of Nursing Services (DNS) dated 6/9/24 at 1:17 PM identified Resident #82's responsible party was requesting broken dentures be evaluated with no response.
A review of the clinical record did not include a documented assessment for safe food consumption while waiting for a dental evaluation.
An interview and clinical record review with the Director of Rehabilitation on 6/21/24 at 3:27 PM identified Resident #82 was not receiving and specialized rehabilitation services during the time the broken denture was reported and had no documented therapy notes Resident #82 was referred for an evaluation of safe food consumption during that time. The Director of Rehabilitation identified nursing was able to assess for any difficulties with chewing or swallowing and would notify rehabilitation services for any signs exhibited to determine if further services were required.
An interview with Speech Therapist, SLP #1 on 6/21/24 at 3:42 PM identified just prior to 6/9/24, Resident #82 was receiving a regular diet with thin liquids. SLP #1 identified she had not provided services to Resident #82 following the documented broken denture on 6/9/24. SLP #1 further identified that although there were some residents who could tolerate a regular diet with broken or missing dentures, nursing staff could assess for any difficulties in chewing and swallowing and refer to therapy if any abnormalities were identified.
An interview with the Director of Nursing Services (DNS) on 6/21/24 at 4:02 PM identified there was no documentation that Resident #82 was assessed for safe food consumption following the report of broken dentures on 6/9/24. The DNS further identified Resident #82 should have been evaluated at the time the damaged denture was reported to determine if s/he could eat and drink adequately.
A review of the facility policy for Dental Services/Dentures dated 4/2015 updated 2024 directed dental services will be provided to each resident, as needed, by a qualified dentist as part of the facility's oral health program. Staff will assist in obtaining routine and emergency dental care. For lost or stolen dentures, the facility must promptly, within three days refer the resident with lost or damaged dentures for dental services. If the referral does not occur within three days the facility must provide documentation of what was done so the resident can still eat and drink adequately while waiting for services.
3. Resident #84's diagnosis included Congestive Heart Failure (CHF), cardiomyopathy, and end stage renal disease.
A physician's order dated 4/1/24 identified the resident as on a fluid restriction of 1000 ml daily.
The quarterly Minimum Data Set assessment dated [DATE] identified Resident #84 as severely cognitively impaired and required maximum assistance for personal hygiene and dependent for showering and toileting.
The Resident Care Plan dated 5/23/24 identified the resident had Congestive Heart Failure. Interventions included monitoring weights as ordered and a fluid restriction of 1000 ml daily.
A nurse's note dated 6/9/24 at 6:40 PM written by LPN # 15 identified Resident # 84 returned to facility at 12 :00 PM today following brief Emergency Department (ED) visit for elevated blood pressures. BP- 174/66 (Normal Range 120/80), P- 67, T-97.5, RR-18, O2 sat- 98% on 2L NC.
Observation on 6/12/24 at 12:13 PM identified Resident # 84 was on oxygen at 2.5 liters per minute via nasal cannula.
In an interview and observation with LPN #3 on 6/18/24 at 9:43 AM identified Resident #84 is supposed to be on oxygen, however s/he cannot locate the physician's order. LPN #3 found a discontinued order for oxygen on 3/11/24. Observation made with LPN #3 confirmed that Resident #84 was wearing nasal cannula, O2 at 2.5L/min. O2 saturation was at 99% on room air.
Interview with APRN #1 on 6/18/24 at 09:54 AM identified Resident #84 should be on oxygen. APRN # 1 indicated s/he did not discontinue the oxygen on 3/11/24. After surveyor inquiry, APRN #1 entered an oxygen physician's order.
Review of the Oxygen Administration Nasal Cannula Policy dated 4/15 with update 2024, directed in part, to deliver low flow oxygen per the physician's order.
Although requested, a facility policy for physician orders was not provided.
4. Resident #88's diagnoses included dementia and failure to thrive.
The admission clinical record identified Resident #88 was not responsible for self.
The physician's orders dated 4/16/24 directed Resident #88 start receiving hospice services and Do Not Resuscitate, DNR (no life saving measures).
The Resident Care Plan (RCP) dated 4/16/24 identified Resident #88's Advanced Directives which directed DNR/DNI (do not intubate or provide an artificial airway to assist with breaths).
The Advanced Directive Code Status dated 4/17/24 identified Resident #88 would have all resuscitation efforts performed (in the event s/he required life saving measures).
A social worker progress note dated 4/18/2024 at 3:20 PM identified a meeting was held with the Interdisciplinary Team and responsible party. Resident #88 was admitted into hospice. Advanced Directive were reviewed, and the responsible party was considering changing the code status to Full Code/ CPR (cardiopulmonary resuscitation or life saving measures). Hospice would be contacted to follow up with the responsible party to discuss code status and plan of care.
A nursing progress note dated 5/15/2024 at 12:05 PM identified Advanced Directives were discussed with Resident #88 who expressed wishes for DNR/ DNI (do not intubate). The responsible party made the final decision for a full code and Resident #88's clinical record was updated.
The physician's orders dated 5/15/24 directed Resident #88 as Full Code (implement life saving measures if necessitated).
The Full Code/ CPR (cardiopulmonary resuscitation or life saving measures). Hospice would be contacted to follow up with the responsible party to discuss code status and plan of care.
The clinical record did not include documented communication to hospice of Resident #88's change to full code status.
An interview with the Director of Nursing on 6/17/24 at 12:20 PM identified the Full Code status should have been communicated by facility staff to hospice.
An interview and clinical record review with Social Worker, SW #1 with the Corporate Social Worker on 6/17/24 at 12:34 PM identified the Interdisciplinary Team (IDT) was responsible for overseeing a resident receiving hospice services. SW #1 further identified that hospice should be communicating changes to the facility and follow up. SW #1 identified she referred Resident #88 to hospice services at the responsible party's request on admission. The responsible party had considered a Full Code status, so SW #1 referred family to hospice social services for a discussion. SW #1 identified she did not follow up on the code status any time between 4/17/24 to present but noted the code status was changed to Full Code on 5/15/24. SW #1 identified she did not communicate the change to hospice.
An interview with the Corporate Social Worker on 6/17/24 at 12:34 PM identified social services were involved in the hospice referral process and the IDT for ongoing care. SW #1 would expect social services to follow up on any issues.
An interview Person #1 6/20/24 at 11:40 AM identified s/he was the Director of Nursing Services (DNS) # 2 for community hospice and was currently providing services for Resident #88. Person #1 identified Resident #88 originally had orders in place for DNR. Person #1 was not informed of Resident #88's change in code status until this week after surveyor inquiry.
A review of the facility policy for Hospice Services directed the facility communicated with hospice any changes in condition regarding resident treatment and provide any related documentation.
5. Resident # 126's diagnosis included heart failure, hypertension, and edema.
The admission Minimum Data Set assessment dated [DATE] identified Resident #126 as cognitively intact and required set up assistance with personal hygiene, oral hygiene, and maximum assistance with showering.
The Resident Care Plan dated 5/15/24 identified the resident had lower extremity edema. Interventions included weighing resident as ordered, and to observe for complications of edema.
A physician's order dated 6/7/24 directed to apply ACE wraps to bilateral lower extremities. Apply in the morning and remove in the evening.
The Treatment Administration Record for June 2024 indicated to apply ACE wraps to bilateral lower extremities. Apply in the morning and remove in the evening beginning 6/8/24.
Observation on 6/12/24 at 12:00 PM and 6/17/24 at 1:00 PM identified Resident # 126 without the benefit of the ACE wraps on her/his lower extremities.
In an interview and observation with LPN #2 on 6/17/24 at 1:00 PM, Resident # 126 did not have ACE wraps on. LPN #2 stated the resident was getting Lasix (diuretic) for her/his edema, and s/he was not aware of any other treatments. This surveyor asked if she knew there was an order written on 6/7/24 for ACE wraps. LPN #2 identified there was a physician's orders and could not explain why Resident # 126's ACE was not applied and would follow up.
LPN # 2 stated Resident # 126's ACE wrap was not applied in the morning as resident woke up at 11:25 AM and went to therapy and indicated s/he would apply them now.
Although requested, a facility policy for physician orders was not provided.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, facility documentation, facility policy and interviews for 1 of 3 sampled residents (Resident #...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, facility documentation, facility policy and interviews for 1 of 3 sampled residents (Resident #6) reviewed for nutrition, the facility failed to ensure a resident weight was obtained according to policy and failed to evaluate the resident's nutritional needs following significant weight loss in a timely manner. The findings include:
Resident #6's diagnoses included dementia, anemia, and hypertension.
The annual Minimum Data Set (MDS) assessment dated [DATE] identified Resident #6 required one person assist with bed mobility and supervised assist with eating.
The Resident Care Plan dated 1/5/24 identified Resident #6 had the potential for impaired nutrition related to impaired cognition and advanced age. Interventions directed to assist with meals as needed, monitor intake and complete nutritional assessments as needed.
The Nutritional assessment dated [DATE] identified Resident #6's current weight was 136.7 lbs., had impaired cognition, advanced age, variable intake on a mechanically altered diet. Laboratory results reflect adequate hydration and slightly depleted protein stores with extra protein provided in supplements. Resident #6's Body Mass index or BMI (measures body fat) was 24.2 (normal 18.5 to 24.9) and within her/his desired weight range. There were no new recommendations.
a. The Weight record dated 4/16/24 identified a documented weight of 113 lbs. reflecting a 23.7 lb. or 17.34% weight loss from the previous month with no documented re-weight.
An interview with Licensed Practical Nurse, (LPN) #8 on 6/18/24 at 10:45 AM identified weights is compared with the previous weight to identify changes and any discrepancies recorded in the Advanced Practice Registered Nurse (APRN) book or reported to the nursing supervisor. S/he further indicated a re-weight would be requested if needed. LPN #8 identified although s/he documented the significant weight discrepancy on 4/16/24, s/he was unable to recall what actions s/he took to address the weight loss or discrepancy. LPN # 8 indicated s/he would have likely notified the nursing supervisor and documented the discrepancy in the APRN communication book. LPN # 8 also indicated s/he would not have notified the dietitian directly.
An interview and review of the communication dashboard (an internal communication system) with the DNS on 6/18/24 and 1:06 PM identified there was no request for re-weight following the 4/16/24 significant weight discrepancy. The DNS further identified for any weight discrepancy; the resident should be re-weighed immediately. Once a true weight discrepancy was identified, a dietary consult would be initiated and the APRN should be notified.
A review of the facility policy for Food First/Nutrition/Weight dated 8/2015 with update 2024 directed a weight loss/gain of 5lbs. or more on a resident weighing 100lbs or more, requires a reweigh for verification using the same scale and with a licensed nurse. Weights are documented in the clinical record and a significant weight loss/gain of 5% in 30 days or 10% on 6 months the interdisciplinary team, dietitian, physician, and family are notified. The weight loss is reviewed by the dietary team and the responsible party is notified and interventions implemented as appropriate. The interventions are monitored weekly.
b. The Weight record dated 4/16/24 identified a documented weight of 113 lbs. reflecting a 23.7lb or 17.34% weight loss from the previous month with no documented re-weight.
An internal dietitian to nursing communication form dated 4/25/34, 9 days after the identified discrepancy, identified on 3/1/24, a weight loss greater than 10% loss in 180days. New ancillary orders included adding Power Cereal at breakfast, diet was downgraded to mechanical soft diet and a dental consult was submitted.
A nutritional progress note dated 5/9/24 identified a weight of 109 lbs. reflecting a 20.7%, 28.5 lb weight loss from the previous month. Power Cereal was added at breakfast.
The physician's orders dated 5/2/24 directed a level II dysphagia mechanically altered diet) moist and soft-textured foods that are easy to chew). The physician's orders dated 5/10/24 directed Power Cereal at breakfast for weight loss.
An interview with Medical Doctor, MD #2 (primary physician) on 6/18/24 10:59 AM identified he would expect the dietitian to be notified within a few days of identifying the weight discrepancy.
An interview with the Administrator on 6/18/24 at 11:07 AM identified weights were discussed daily in morning report and weekly during Risk Management meetings. The charge nurses should be reporting weight discrepancies to the nursing supervisor who was expected to notify the dietitian immediately. The dietitian was not at the facility daily but could be notified by phone or remotely.
An interview with the Director of Nursing Services (DNS) on 6/18/24 at 1:06 PM identified s/he would expect the nutritionist to address a resident's nutritional needs immediately after a significant weight loss.
An interview with the Dietitian on 6/20/24 at 10:26 AM identified she provided dietary services one day a week for the facility. Weights and vital signs were reviewed during the weekly visits and an assessment completed for any resident with significant changes. The Dietitian further identified occasionally nursing staff did report weight changes, but Resident #6's weight discrepancy was not reported in this case, there was no documented reweigh and Resident #6 did not 'trigger' in the electronic clinical record that there was a significant change. The Dietitian identified she utilized a communication tool to inform the nurse of her recommendations for Resident #6. However, it is a long process to address matters timely when recommendations are placed in the medical communication book and reviewed before the physician/APRN signs the orders. The Dietitian also identified the provision of dietary services only one day a week contributed to the not addressing timely nutritional needs and indicated the facility has employed a dietary technician to assist now which was not previously in place.
Attempts to interview the Nursing Supervisor assigned 4/16/24 were unsuccessful.
A review of the facility policy for Food First/Nutrition/Weight dated 8/2015 with update 2024 directed a weight loss/gain of 5lbs. or more on a resident weighing 100lbs or more, requires a reweigh for verification using the same scale and with a licensed nurse. Weights are documented in the clinical record and a significant weight loss/gain of 5% in 30 days or 10% on 6 months the interdisciplinary team, dietitian, physician, and family are notified. The weight loss is reviewed by the dietary team and the responsible party is notified and interventions implemented as appropriate. The interventions are monitored weekly.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, review of clinical records, facility documentation, facility policy and interviews for 3 of 4 residents (...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, review of clinical records, facility documentation, facility policy and interviews for 3 of 4 residents (Residents # 69, #84, and # 126) reviewed for oxygen, the facility failed to change and label the residents oxygen tubing weekly per facility policy and practice. The findings included:
1. Resident #69 's diagnoses included Acute on Chronic Congestive Heart Failure, pneumonia, Acute and Chronic Respiratory Failure.
A physician's order dated 6/4/24 directed to administer oxygen at 2 liters per minute via nasal cannula.
The Resident Care Plan dated 6/5/24 identified the resident has Congestive Heart Failure. Interventions included providing oxygen as ordered.
The admission Minimum Data Set assessment dated [DATE] identified Resident #69 as cognitively intact and required moderate assistance with toileting, personal hygiene, and maximum assistance with showering.
Observations on 6/12/24 at 12:57 PM, identified Oxygen tubing was not dated.
The Treatment Administration Record dated June 2024 directed to change oxygen tubing every Sunday night shift starting June 23, 2024. After surveyor inquiry about oxygen tubing date.
2. Resident #84's diagnosis included Congestive Heart Failure, cardiomyopathy, and end stage renal disease.
A physician's order dated 4/1/24 identified the resident as on a fluid restriction of 1000 ml daily.
The quarterly Minimum Data Set assessment dated [DATE] identified Resident #84 as severely cognitively impaired and required maximum assistance for personal hygiene and dependent for showering and toileting.
The Resident Care Plan dated 5/23/24 identified the resident had Congestive Heart Failure. Interventions included monitoring weights as ordered and a fluid restriction of 1000 ml daily.
Observation on 6/12/24 at 12:13 PM identified the resident's oxygen tubing without a date.
3. Resident # 126's diagnosis included Heart Failure, hypertension, and edema.
The admission Minimum Data Set assessment dated [DATE] identified Resident #126 as cognitively intact and required set up assistance with personal hygiene, oral hygiene, and maximum assistance with showering.
The Resident Care Plan dated 5/15/24 identified the resident had lower extremity edema. Interventions included weighing resident as ordered, and to observe for complications of edema.
A physician's order dated 5/30/24 directed oxygen via nasal cannula at 2 liters per minute.
The Treatment Administration Record for June 2024 identified the resident's oxygen tubing should be changed every Sunday beginning 6/2/24. However, based on clinical record review and observation there was no evidence that the tubing was changed on 6/9/24.
Observation on 6/12/24 at 12:35 PM identified Resident # 126's oxygen tubing without a date.
In an interview and observation with LPN #1 on 6/12/24 at 1:00 PM identified oxygen tubing should be changed every Sunday, and LPN #1 was unable to locate the date on the oxygen tubing for Residents #'s 69, # 84 and # 126.
Interview with LPN #2 on 6/17/24 at 10:30 AM identified oxygen tubing should be changed weekly and documented on the Treatment Administration Record.
Review of the Oxygen Administration Nasal Cannula policy dated April 2015 updated 2024 directed, in part, replace and date cannula and tubing weekly or when visibly soiled or damaged.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, review of facility policy and staff interviews for 1 of 3 residents observed for pain (Resident...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, review of facility policy and staff interviews for 1 of 3 residents observed for pain (Resident #100), the facility failed to ensure a resident was medicated appropriately for symptoms of pain. The findings include:
Resident #100 was admitted on [DATE] with a diagnosis that included dementia, repeated falls, and osteoporosis.
A quarterly MDS assessment dated [DATE] identified Resident #100 was severely cognitively impaired and required extensive assistance for bed mobility. Additionally, the MDS indicated the resident could not verbalize the presence of pain but had vocal complaints and protective body movements or postures as indicators of pain. The MDS further indicated the resident received hospice care and exhibited daily indicators of pain or possible pain.
A physician's order dated 6/6/2022 directed to assess the resident's pain every hour and medicate if needed per order for pain, and to follow up with hospice/MD if the pain is uncontrolled with the regimen.
A physician's order dated 6/14/2022 directed to administer 5 milligrams (mg) of Morphine every 4 hours scheduled for pain. Additionally, physician orders dated 6/14/2022 directed to administer 5 MG of Morphine every hour as needed for moderate pain and 10 mg of morphine every hour as needed for severe pain.
A nursing progress note by LPN #12 dated and signed on 6/15/2022 at 4:02 PM indicated Resident # 100 appeared to be holding his/her left leg and exhibited symptoms of pain at the beginning of the shift (7:00 AM to 3:00 PM shift). The nursing progress note further indicated that a left hip x-ray taken during the shift 7-3 PM shift identified a fracture, and the resident was taken to the hospital on 6/15/2024 at 2:24 PM.
A review of the Medication Administration Record (MAR) from 6/1/2022 through 6/15/2022 identified Resident #100 was evaluated for pain every hour, and the resident's pain was consistently at zero from 6/1/2022 through 6/15/2022. On 6/15/2022, Resident #100 was evaluated as having a pain level of 5 (moderate pain) on 6/15/2022 at the following times: 3:00 AM, 4:00 AM, 5:00 AM, 6:00 AM, and 7:00 AM, the MAR indicated the resident received a scheduled dose of Morphine at 4:00 AM.
A nursing progress note by LPN #11 dated and signed 8/15/2022 at 6:48 AM identified at 4:00 AM Resident #100 was having difficulty sleeping and exhibiting facial expressions of pain. Additionally, the nursing note indicated at 6:30 AM the resident was awake with continued expressions of pain. The nursing note further indicates LPN #11 made attempts to call the hospice service with no return call back.
In an interview on 6/18/2024 at 1:39 PM, LPN# 11 indicated she did not recall details of the incident and the only thing she remembered was Resident # 100 had fallen and had received an x-ray.
Attempts to contact RN #4 were unsuccessful.
On 6/20/2024 at 11:20 AM, an interview with the DNS indicated there should have been an intervention addressing Resident #100's ongoing pain and staff should have investigated why the resident was having increased pain, especially considering the resident had a recent fall. The DNS also indicated the resident could have been medicated for pain per physician's orders for prescribed pain management.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, facility documentation, facility policy and interviews for 1 of 3 sampled residents (Resident #...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, facility documentation, facility policy and interviews for 1 of 3 sampled residents (Resident #82) reviewed for dental services, the facility failed to ensure dental services was provided following a responsible party request for an evaluation for broken dentures. The findings include:
Resident #82's diagnoses included dementia, anorexia, and dysphagia.
The quarterly Minimum Data Set assessment dated [DATE] identified Resident #82 as severely cognitively impaired and independent with activities of daily living skills.
The Resident Care Plan dated 6/9/23 identified Resident #82 used partial dentures. Interventions directed to monitor/document/report any signs of oral/dental problems needing attention.
A social service progress note dated 6/9/23 identified the responsible party had questions regarding the resident's dentures and Resident # 82 was referred to the dentist for evaluation of his/her lower dentures.
The dental consults dated 2/8/23 and 9/11/23 identified broken or missing dentures with no recommendations for replacement or repair.
The dental consults dated 9/11/23, 12/5/2023 and 2/8/24 noted Resident #82 was seen for routine dental prophylaxis without any documented request to evaluate for lower dentures.
An electronic correspondence (email) to the DNS dated 6/9/24 at 1:17 PM identified Resident #82's responsible party requested that Resident # 82's broken dentures be evaluated with no response.
An interview and clinical record review with Social Worker (SW #1) on 6/18/24 at 11:45 AM identified Resident #82's broken dentures were discussed in a care plan meeting. An email was sent to the Director of Nursing Services to address and there was no response.
An interview with the DNS on 6/18/24 at 12:02 PM identified she would expect any requests for specialty services to be acted on and the dental consult reflect the specific request for evaluation/replacement of broken dentures.
An interview with Medical Records Associate on 6/18/24 at 12:07 PM identified she was responsible for the scheduling of specialty services in the community. The Medical Records Associate further identified she had not received any specialty (dental) requests of any kind on behalf of Resident #82 for an evaluation or replacement of h/her dentures.
A review of the facility policy for Dental Services/Dentures dated 4/2015 with update 2024 directed dental services will be provided to each resident, as needed, by a qualified dentist as part of the facility's oral health program. Staff will assist in obtaining routine and emergency dental care. For lost or stolen dentures, the facility must promptly, within three days refer the resident with lost or damaged dentures for dental services. If the referral does not occur within three days the facility must provide documentation of what was done so the resident can still eat and drink adequately while waiting for services.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, and policy review and staff interviews for 1 of 2 residents reviewed for pressure ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, and policy review and staff interviews for 1 of 2 residents reviewed for pressure ulcers (Resident #57), the facility failed to ensure staff followed the appropriate infection control practices while performing a dressing change. The findings include:
Resident #57 was admitted on [DATE]. The resident's diagnoses included dementia, weakness, and a history of Extended Spectrum Beta Lactamase (ESBL) resistance.
The MDS assessment dated [DATE] indicated Resident #57 had severe cognitive impairment. The resident required extensive assistance with bed mobility and was dependent on transferring and toilet use. Additionally, the MDS indicated Resident #57 had an unhealed stage 3 pressure ulcer.
A care plan dated 5/23/2024 identified Resident #57 was incontinent of bowel and bladder and had a history of infection with ESBL (a resistant micro-organism). Interventions included maintaining precautions.
A wound specialist progress note dated 6/12/24 identified Resident #57 had a stage 3 pressure ulcer injury to the coccyx area measuring 6 centimeters (cm) long, 6 cm wide, and 3.2 cm deep, with moderate amount of serosanguineous drainage. The recommended treatment directed cleansing the wound with ¼ strength Dakin's solution for 15 minutes, then applying a Hydrofera blue dressing and to cover the area with a foam dressing.
On 6/17/2024 at 10:50 AM, observation of wound care for Resident #57 by LPN #5 and NA #2 identified a sign next to the resident's room door with instruction for staff to wear gloves and a gown when providing personal care or changing a dressing. LPN #5 gathered supplies, then performed hand hygiene with alcohol-based hand sanitizer and donned gloves without the benefit of donning a gown. NA #2 performed hand hygiene with an alcohol-based hand sanitizer and donned gloves. NA#2 then proceeded to turn Resident # 57 towards the resident's left side. LPN #5 proceeded to remove the old dressing and cleansed the wound bed with a spray called DermaKlenz ( wound cleanser). LPN #5 removed the soiled gloves and donned a new pair of clean gloves. LPN#5 did not perform hand hygiene in between changing gloves. LPN #5 then proceeded to pack the wound with gauze soaked in Dakin's solution. The resident was repositioned by LPN#5 and NA #2, who then left the room and allowed the resident to rest for 15 minutes. Upon exiting the room, LPN #5 and NA #2 removed their soiled gloves and performed hand hygiene with an alcohol-based hand sanitizer. At 11:10 AM, LPN # 5 and NA #2 returned to complete the dressing change. LPN #5 and NA #2 performed hand hygiene and donned clean gloves prior to entering the resident's room. LPN #5 and NA#2 did not don gowns. NA #2 then proceeded to turn the resident towards the resident's left side. LPN #5 removed the Dakin's-soaked gauze packing. LPN #5 removed the soiled gloves and donned a new pair of clean gloves. LPN#5 did not perform hand hygiene in between changing gloves. LPN #5 then proceeded to pack the wound with a Hydrofera blue dressing and covered the area with a foam dressing.
On 6/17/2024 at 12:37 PM an interview with LPN #5 indicated she was aware Resident # 57 was on enhanced barrier precautions and staff were required to wear gowns and gloves when performing dressing changes or providing care. LPN #5 indicated not wearing the isolation gown was an oversight. Additionally, LPN #5 indicated s/he was not aware performing hand hygiene in between glove changes was part of hand hygiene compliance.
On 6/17/2024 at 3:31 PM, an interview with the DNS identified s/he expected a signage to be posted for a resident requiring enhanced barrier precautions and for staff to follow the instructions on the appropriate personal protective equipment to use. The DNS indicated staff should wear a gown when providing wound care as part of enhanced barrier precautions.
A review of the facility policy for hand hygiene notes in part hand hygiene with an alcohol-based hand sanitizer should be performed after removing gloves. The facility policy for enhanced barrier precautions indicated the use of gowns and gloves are required when performing high-contact resident care activities, including toileting, providing hygiene, and wound care.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record reviews, facility documentation, policy review and interviews for 2 of 3 residents (Residents #286, #28...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record reviews, facility documentation, policy review and interviews for 2 of 3 residents (Residents #286, #288) observed for Cardiopulmonary Resuscitation (CPR), the facility failed to maintain a copy of licensed staff CPR certification card per facility practice and failed to complete the Code Blue transcription log per facility practice and policy. The findings included:
1. Resident #286 's diagnoses included pneumonia, Chronic Obstructive Pulmonary Disease (COPD) and asthma.
The admission Minimum Data Set assessment dated [DATE] identified Resident #286 was cognitively intact and required maximum assistance for showering and toileting and set up assistance for oral hygiene.
The Resident Care Plan dated [DATE] identified Resident #286 had pneumonia. Interventions included administering antibiotics as ordered, encouraging fluids, monitoring pulse oximetry, and providing oxygen as ordered.
A physician's order dated [DATE] directed to administer oxygen at 1 liter per minute via nasal cannula and as needed for shortness of breath, administer Cefuroxime Axetil (antibiotic) 500 mg twice daily for pneumonia and noted the resident was a full code.
A nurse's note dated [DATE] at 7:01 AM written by RN # 1, identified a charge nurse, LPN #4, informed RN#1 Resident # 286 was unresponsive. On assessment, resident confirmed with no pulse, no heartbeat, no respiration, pupils fixed and non-reactive. Full code status confirmed, and CPR initiated, 911 called.
2. Resident #287's diagnosis included type 2 diabetes with Neuropathy, vascular dementia, and heart failure.
The quarterly Minimum Data Set assessment dated [DATE] identified Resident #287 as moderately cognitively impaired and independent with toileting, showering and oral hygiene.
A physician's order dated [DATE], directed to provide CPR.
A nurse's note dated [DATE] at 5:27 AM written by LPN #13 identified Resident # 287 was observed in bed and appeared without breathing. Resident # 287 was not responsive with no blood pressure, no respiration, and no pulse. Code was initiated, LPN #13 started CPR and called 911.
The Resident Care Plan dated [DATE] identified Resident #287 as a full code and wished to receive CPR. Interventions included reviewing code status quarterly with resident and/or resident's decision maker.
Review of the facility CPR certification binder for LPN# 4 dated [DATE] identified the certification expired 1/2022. No evidence was provided to identify that LPN # 4's CPR certification was renewed in 2022.
Review of CPR certification binder for NA #1 and LPN #13 did not include any CPR certifications.
Interview with NA #1 on [DATE] at 11:41 AM identified s/he (NA #1) did not remember if s/he was certified at the time of the code she stated, I think I was, but I cannot find my card.
In an interview with Administrator, Regional Nurse, and DNS on [DATE] at 1:37 PM identified that they discard the CPR certifications once an employee has been terminated. LPN #4 and NA #1 are no longer employed by the facility. Further interview identified that all CPR certifications are kept in a binder used to track renewal dates. The Administrator stated LPN #13 was going attend the [DATE] class to get certified in CPR. LPN # 4 was hired in [DATE] and did not give the facility any documentation indicating s/he was CPR certified.
Interview with LPN #4 on [DATE] at 11:40 AM identified s/he cannot find her/his 2022 CPR certification, LPN # 4 started at a new facility and was not sure if they did the training when she got there. LPN # 4 stated that s/he has a card for February of 2023.
Review of the Cardiopulmonary Resuscitation (CPR) policy dated 10/16 directed, in part, written verification for the completion of CPR training for each health care professional and all other trained personnel will be maintained in the employee file.
3a. Resident #286 's diagnoses included pneumonia, Chronic Obstructive Pulmonary Disease, and asthma.
The admission Minimum Data Set assessment dated [DATE] identified Resident #286 was cognitively intact and required maximum assistance for showering and toileting and set up assistance for oral hygiene.
The Resident Care Plan dated [DATE] identified Resident #286 had pneumonia. Interventions included administering antibiotics as ordered, encouraging fluids, monitoring pulse oximetry, and providing oxygen as ordered.
A physician's order dated [DATE] directed to administer oxygen at 1 liter per minute via nasal cannula and as needed for shortness of breath, administer Cefuroxime Axetil 500 mg twice daily for pneumonia, resident was a full code.
A nurse's note dated [DATE] at 7:01 AM written by RN # 1, identified the charge nurse (LPN #4), informed her/her Resident # 286 was unresponsive. On assessment, resident confirmed with no pulse, no heartbeat, no respiration, pupils fixed and non-reactive. Full code status confirmed, and CPR initiated, 911 called.
Review of the facility clinical documentation identified that a Code Blue log was not located Resident # 286's file per facility practice.
b. Resident #288's diagnosis included End Stage Renal Disease, heart failure, and type 2 diabetes mellitus.
A physician's order dated [DATE] directed the resident to be a full code and to receive CPR.
The Resident Care plan dated [DATE] identified Resident #288 as a full code wishing to receive CPR. Interventions included reviewing advanced directives quarterly with resident and/or resident's decision maker.
The admission Minimum Data Set assessment dated [DATE] identified Resident #288 as cognitively intact and required partial assistance with toileting and showering and was independent with oral hygiene.
A nurses note dated [DATE] at 11:04 AM written by RN #5 identified Code Blue called secondary to resident found unresponsive. Resident # 288 was lying flat in bed on assessment with CPR being administered by facility staff and Emergency Medical Technician (EMT) were on scene to pick resident up for specialized treatment.
Review of the clinical documentation identified of the Code Blue log failed to identify the log in the resident's medical file.
Interview on [DATE] at 10:00 AM with LPN #5 identified a Code Blue log should be completed for every code. Blank forms are located on a clip board on the crash cart.
In an Interview with Administrator and Regional Nurse and DNS on [DATE] at 1:37 PM, the Code Blue Log should be in the resident's clinical record.
Review of the Cardiopulmonary Resuscitation (CPR) policy dated 10/16 given to surveyor as policy in place at time of the CPR directed, in part, that documentation in the resident's chart is to include the course of events leading up to and including CPR.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0678
(Tag F0678)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, facility documentation, facility policy and interviews for 1 of 3 residents (Resident #286) obs...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, facility documentation, facility policy and interviews for 1 of 3 residents (Resident #286) observed for CPR, the facility failed to ensure an employee who administered CPR was appropriately trained as per facility practice and policy. The findings include:
Resident #286 's diagnoses included pneumonia, Chronic Obstructive Pulmonary Disease (COPD) and asthma.
The admission Minimum Data Set assessment dated [DATE] identified Resident #286 was cognitively intact and required maximum assistance for showering and toileting and set up assistance for oral hygiene.
The Resident Care Plan dated [DATE] identified Resident #286 had pneumonia. Interventions included administering antibiotics as ordered, encouraging fluids, monitoring pulse oximetry, and providing oxygen as ordered.
A physician's order dated [DATE] directed to administer oxygen at 1 liter per minute via nasal cannula and as needed for shortness of breath, administer Cefuroxime Axetil (antibiotic) 500 mg twice daily for pneumonia and noted the resident was a full code.
A nurse's note dated [DATE] at 7:01 AM written by RN # 1, identified a charge nurse, LPN #4, informed RN#1 Resident # 286 was unresponsive. On assessment, resident confirmed with no pulse, no heartbeat, no respiration, pupils fixed and non-reactive. Full code status confirmed, and CPR initiated, 911 called.
Interview with LPN #4 on [DATE] at 1:50 PM identified s/he went into room and started CPR. The Nurse Aide (NA # 1) took over CPR and s/he (LPN# 4) went to call the supervisor.
A telephone interview on [DATE] at 11:41 AM with NA #1 identified s/he was checking Resident # 286 every 15 minutes as the resident was very sick. NA #1 could not remember what time it was when s/he went to check on the resident and Resident # 286 was not breathing. NA #1 called the nurse (LPN #4) to tell LPN #4 to start CPR. LPN #4 told her/him (NA #1) to call the supervisor so that a code can be called at which time NA #1 told LPN # 4 s/he did not know how to do that, so NA#1 took over CPR, LPN #4 called the supervisor who came up with the cart. NA #1 did not remember if she was CPR certified at the time of the code; she stated I think I was, but I cannot find my card. I knew what to do, I watched the nurse. When asked if she knew what the facility policy is about nurse aides doing CPR, she replied Yes, we are not supposed to. But I did not know how to call a code, so the LPN needed to do that, so I took over for her/him. LPN # 4 came right back and started doing CPR again.
Interview with Administrator, Regional Nurse, and DNS on [DATE] at 1:37 PM identified RNs, LPNs and/or any person with a valid CPR certification can perform CPR as per facility policy. However, the facility does not allow NAs to perform CPR and they do not train them to become certified. The Administrator also indicated that NA #1 was not trained and certified to perform CPR at the time of the code for Resident #286.
Review of the Cardiopulmonary Resuscitation (CPR) policy dated 10/16 given to surveyor for policy at time of code directed, in part, CPR will be done by the trained registered or licensed practical nurse or any other personnel who have completed CPR training.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the facility Sufficient and Competent Nurse Staffing, facility documentation and interview, the facility fail...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the facility Sufficient and Competent Nurse Staffing, facility documentation and interview, the facility failed to ensure competencies were conducted for Nurse Aides and Licensed Nurses to ensure staff was competent to provide care for and meet the needs of all residents. The findings include.
An interview and review of facility documentation on 6/20/24 at 9:15 AM with the Administrator indicated mandatory in-service training was completed for all staff for the year of 2022.
However, a review of the facility mandatory in servicing identified the facility was unable to provide any competencies for Nurse Aides or licensed nurses for the years of 2022 to present.
An interview and review of facility documentation on 6/20/2024 at 2:00 PM with the Administrator found mandatory in servicing completed for all staff during the year of 2023 but was unable to provide any competencies for Nurse Aides or Licensed nurses for the years of 2022 to present. The Administrator indicated although ongoing advertising for the position of Staff Development Coordinator, the facility has not been able to fill the position since March 2023. The Administrator further indicated s/he has been conducting interviews for RN position and a RN is scheduled to start next week. S/he also indicated the monthly and annual in-servicing has continued with the assistance of the nursing supervisor and the Infection Preventionist. The Administrator indicated s/he will ensure that all staff complete in-servicing and training.
The Facility assessment dated [DATE] indicated mandatory staff training/education and competencies are conducted at orientation and at least once a year and as needed.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations of the kitchen, review of facility documentation, review of policy and interviews, the facility failed to consistently document in the PH (check for the appropriate amount of san...
Read full inspector narrative →
Based on observations of the kitchen, review of facility documentation, review of policy and interviews, the facility failed to consistently document in the PH (check for the appropriate amount of sanitizer) log for the three-bay sink manual sanitizer. The findings include:
On 6/12/2024 at 11:55 AM, a tour of the kitchen with the Dietary Director identified Dietary Aide #1 manually washing pots in the kitchen's three-bay sink. Further observations identified there was a pot submerged in a pink-tinged liquid in the three-bay sink's left-most bay. The Dietary Director indicated pots and pans do not go through the dishwasher and are sanitized in the three-bay sink.
An interview with Dietary aide #1 in the presence of the Dietary Director identified s/he was unable to explain or demonstrate the procedure for checking if the sanitizing bay contained the appropriate amount of sanitizer. After prompting from the Dietary Director, Dietary Aide #1 was able to demonstrate how s/he would check the concentration of the sanitizer. However, at the time of the observation Dietary Aide #1 had difficulty in interpreting the results of the pH test strip. When the surveyor questioned the Dietary Aide about the difficulty in reading the pH test strip, the Dietary Director indicated Dietary Aide #1 had a vision problem the week prior and was having difficulty reading the test strip's result.
Dietary Aide #1 indicated s/he checked the concentration of the sanitizer prior to starting washing dishes. Dietary Aide #1 was able to identify where s/he would log the pH of the manual sanitizer.
A review of the daily temperature logs with the Dietary Director from 6/1/2024 through 6/12/2024 identified PH testing of the manual sanitizer was not documented on 6/3/2024 for breakfast, lunch, or dinner. PH testing documentation was missing for dinner for 6/4, 6/5, 6/6, 6/8/2024. The Dietary Director indicated there would have been pots to sanitize after dinner on the above days. Furthermore, PH testing documentation was missing for breakfast, lunch, and dinner on 6/9 and 6/10/2024. The Dietary Director indicated s/he did not know why PH testing would not be documented on the log and the reason maybe that staff might be forgetting to write down their results.
A review of facility policy for PH testing in manual ware washing notes PH testing is to ensure that sanitizing levels are adequate to effectively remove harmful bacteria on food contact surfaces. Additionally, the policy indicated that staff would perform tests with PH strips and record the result in the temperature log.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected most or all residents
Based on review of facility documentation Sufficient and Competent Nurse staffing and interviews, the facility failed to ensure all nurse aides were monitored to ensure they received at least 12 hours...
Read full inspector narrative →
Based on review of facility documentation Sufficient and Competent Nurse staffing and interviews, the facility failed to ensure all nurse aides were monitored to ensure they received at least 12 hours of annual in-service training. The findings include.
Interview and review of facility document with the Administrator on 6/20/2024 at 2:50PM identified in-servicing for all staff were conducted and many in-servicing sheets were lacked the duration of time of training and who conducted the in-service. The Administrator was unable to locate any tracking/ monitoring for the nurse aides to ensure each received at least 12 hours of annual training.
An interview and review of facility documentation on 6/20/2024 at 2:00 PM with the Administrator indicated that although ongoing advertising for the position of staff development coordinator was in place, the facility had not been able to fill the position Staff Development position since March 2023.
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0946
(Tag F0946)
Minor procedural issue · This affected most or all residents
Based on review of facility documents and interviews during extended survey, the facility failed to ensure effective communication of standards, policies and procedures of its Compliance and Ethics pr...
Read full inspector narrative →
Based on review of facility documents and interviews during extended survey, the facility failed to ensure effective communication of standards, policies and procedures of its Compliance and Ethics program to its entire staff. The findings include.
On 6/26/2024 at 2:45 PM an interview and facility document review with the Administrator who was unable to locate initial or annual in-service training that included communication of the Corporate Compliance program for all staff. The Administrator indicated annual in-service training would begin in 2024. The Administrator verified the facility's governing body operates five or more buildings.
On 6/26/2024 at 2:50 PM an interview and facility employee files with the Human Resources Director identified 4 out of 6 employee staff files were missing the Compliance Certificate Statement, kept in the employee's personnel file at the time of hire that indicated the employee received, in part, Corporate Compliance training.