EVERGREEN POST ACUTE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Evergreen Post Acute in Smyrna, Delaware, has received a Trust Grade of F, indicating significant concerns about the quality of care provided. It ranks #32 out of 43 nursing homes in Delaware, placing it in the bottom half of facilities in the state and #7 out of 7 in Kent County, meaning it is the least favorable option locally. While the facility is showing improvement in the number of issues reported-going from 27 in 2024 to 25 in 2025-there are still serious concerns, including $109,425 in fines, which is higher than 75% of Delaware nursing homes. Staffing has a rating of 3 out of 5, which is average, but the turnover rate is concerning at 48%. Additionally, there are significant incidents documented, including a failure to administer CPR to a resident who required it, leading to a tragic death, and a serious medication error that hospitalized a resident due to incorrect medication dosages. Overall, while there are some areas of strength, the facility's weaknesses raise significant concerns for families considering care for their loved ones.
- Trust Score
- F
- In Delaware
- #32/43
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 48% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $109,425 in fines. Lower than most Delaware facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 31 minutes of Registered Nurse (RN) attention daily — about average for Delaware. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 74 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Delaware average (3.3)
Below average - review inspection findings carefully
Near Delaware avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 74 deficiencies on record
Apr 2025
23 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0760
(Tag F0760)
A resident was harmed · This affected 1 resident
Based on record review and interview, it was determined that for one (R644) out of eleven residents, the facility failed to ensure that R644 was free of medication error. On 9/13/24, R644 was inadvert...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and interview, it was determined that for one (R14) out of forty-three (43) residents in the investigative sample, the facility failed to ensure R14 was treated with respect and d...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for one (R641) out of the seven residents reviewed for advanced directives, the facility failed to ensure that R641's' representative was i...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for one (R188) out of four residents reviewed for Beneficiary Notification Review, the facility failed to ensure the resident was informed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on a random observation and interview, it was determined that for four (R37, R69, R72, and R133) residents, the facility failed to protect personal privacy. Findings include:
4/10/25 11:08 AM - ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0603
(Tag F0603)
Could have caused harm · This affected 1 resident
Based on record review and interviews, for one (R112) out of five sampled for abuse, it was determined that R112 was not free from involuntary seclusion. Findings include:
Cross refer F684 and F880.
...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for one (R79) out of five residents reviewed for hospitalizations, the facility failed to notify R79's responsible party in writing of the ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for one (R136) out of forty-three sampled residents, the facility failed to complete a comprehensive assessment after R136 had a significan...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on record review and interviews, it was determined for two (R40 and R50) out of forty-three sampled residents, the facility failed to ensure the MDS was accurate. Findings include:
1. Review of ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record reviewed and interview it was determined that for one (R196) out of forty-three residents sampled, the facility failed to ensure the person centered care plan included necessary interv...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined that for one (R188) out of three residents reviewed for discharge the facility failed implement a discharge planning process that prepared the re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on interview, observation and record reviews it was determined that for one (R132) out of one resident reviewed for communication the facility failed to provide assistive devices to support comm...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
2. Review of R73's clinical record revealed:
1/2/20 - R73 was admitted to the facility.
1/4/20 - A care plan documented that R73 required assitance with all ADL's with the following interventions: as...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined that for two (R112 and R644) out of forty three residents reviewed in the investigative sample, the facility failed to ensure received treatment ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, it was determined that for one (R35) out of 11 resiedents reviewed for accidents the facility failed to implement a care planned fall intervention. F...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0808
(Tag F0808)
Could have caused harm · This affected 1 resident
Based on observation and interview, it was determined that for one (R3) out of ten residents sampled for dining, the facility failed to provide the therapeutic diet that was prescribed by the physicia...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, it was determined that for two (R18 & R33) out of five residents reviewed for antibiotic u...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, it was determined that for two (R33 and R96) out of twelve residents reviewed for pneumoco...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, it was determined that for two out of three resident units the facility failed to provide a ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
3. Review of R119's clinical record revealed:
5/13/24 - R119 was admitted to the facility.
5/20/24 - An admission MDS was completed.
5/22/24 - The admission Resident Care Conference Attendance Sheet ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and interview it was determined that the facility failed to ensure food was stored, prepared, and served in manner that prevents food borne illness to the residents. Findings incl...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4/8/25 6:16 AM - A random observation revealed a clear plastic trash bag with dirty briefs and gloves was sitting on the floor i...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0761
(Tag F0761)
Minor procedural issue · This affected multiple residents
Based on observation and interview it was determined that for three out of three medication carts observed the facility failed to ensure that opened medications were labeled with an open date. Finding...
Read full inspector narrative →
Jan 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview, record review and a review of other facility documentation, it was determined that for one (R1) out of three sampled residents reviewed abuse, the facility failed to report an alle...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview, record review and review of other facility documentation, it was determined that for one (R1) out of three sampled residents for investigating an allegation of abuse, the facility ...
Read full inspector narrative →
May 2024
27 deficiencies
4 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
REVISED POST IDR
Based on observation, interviews and record review it was determined that for one (R110) out of two residents reviewed for pressure ulcers, the facility failed to provide care and ser...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on record review, observations and interviews, it was determined that for one (R106) out of three residents reviewed for accidents, the facility failed to ensure that R106 received adequate supe...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Incontinence Care
(Tag F0690)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observations and interviews, it was determined that for one (R106) out of five residents reviewed for bo...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
Based on interview and record review, it was determined that for one (R399) out of one resident reviewed for hydration, the facility failed to ensure that R399 was offered adequate fluid intake to pre...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, it was determined that the facility failed to promote R18's dignity by keeping R18's urinary collection bag in a privacy bag. Findings include:
Revi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record review, it was determined that for one (R65) out of one sampled resident reviewed for choices and preferences, the facility failed to accommodate R65's pre...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined that for three (R18, R65 and R116 ) out of six residents reviewed for Advance Directives, the facility failed to offer an opportunity to formula...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on record review and interviews, it was determined that for one (R80) out of two reviewed for Personal Property, the facility failed to maintain evidence demonstrating the result of R80's grieva...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for one (R294) out of one sampled resident reviewed for reporting of alleged violations, it was determined that the facility failed to iden...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview, record review, and review of other facility documentation, as indicated, it was determined that for one (R294) out of one sampled resident for investigate/correct alleged violation...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on record review and interviews, it was determined for four (R2, R46, R98 and R106) out of thirty residents in the investigative sample, the facility failed to ensure the MDS was accurate. Findi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
2. Review of R28's clinical record revealed:
4/2/21 - R28 was admitted to the facility with diagnoses, including but not limited to, stroke affecting the right dominant side and aphasia (a language di...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined that for one (R47) out of six residents sampled for PASARR review, the facility failed to provide evidence that a Delaware State PASARR was obta...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for two (R40 and R106) out of three residents reviewed for bowel and bladder, the facility failed to develop a person centered care plan to...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, it was determined that for one (R3) out of four residents reviewed for Medication Adminis...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interviews, it was determined that for four (R18, R54, R65, and R79) out of six residents reviewed for ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
3. Review of R397's clinical record revealed:
10/26/23 - R397 was admitted to the facility with diagnoses including type II diabetes and morbid obesity due to excess calories.
10/27/23 12:30 PM - A ph...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for one (R297) out of four residents reviewed for respiratory care the facility failed to properly administer oxygen. Findings include:
Rev...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. 7/5/18 - R3 was admitted to the facility with the following diagnoses, including but not limited to, multiple sclerosis.
2/14...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review and interviews, it was determined that for one (R3) out of four residents reviewed for Medication Administration, the facility failed to ensure that R3's monthly medication revi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
3. Review of R47's clinical record revealed:
12/15/15 - R47 was admitted to the facility.
1/11/16 - A care plan was initiated for R47's use of anticoagulant therapy with an intervention of observing a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and interview it was determined the facility failed to receive and document narcotic medications per professional standards of care. Findings include:
Review of R65's clinical rec...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0773
(Tag F0773)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined, for one (R79) out of one resident sampled for laboratory services, the facility failed to promptly notify the ordering medical practitioner of ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review and review of other facility documentation it was determined that the facility failed to ensur...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Based on record review and interview, it was determined that for five (R2, R32, R55, R88 and R120) out of five sampled residents for care plan timing and revision, the facility failed to have input fr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to establish and maintain an infection prevention and control program designed to provide a safe and sanitary environment. Findings include:
1. ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview, it was determined that the facility failed to ensure food was stored, prepared, and served in a manner that prevents food borne illness to the residents. Findings i...
Read full inspector narrative →
Apr 2023
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on interview and observation of one out of two units toured, it was determined that the facility failed to provide a clean and homelike environment. Findings include:
4/6/23 1:37 PM - An observa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for one (R49) out of three residents reviewed for hospitalization, the facility failed to ensure the Ombudsman was notified of the resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, it was determined that for one (R98) out of five sampled residents for ADL's (activities of daily living), the facility failed to provide oral hygie...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview, record review and review of other documentation, it was determined that for one (R128) out of one resident reviewed for skin conditions, the facility failed to initiate timely trea...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined that for one (R15) out of one resident reviewed for dialysis, the facility failed to monitor the residents dialysis catheter. Findings include:
...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on review of facility documentation and interview, it was determined that for six (E8, E9, E10, E11, E12 and E21) out of six employee evaluations reviewed, the facility failed to ensure that per...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation and interview, it was determined that the facility failed to ensure that it was free of a medication error rate of 5% or greater. Medication pass observations identified three (3)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and staff interview, it was determined that the facility failed to ensure that one (R116) out of eight (8) ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0790
(Tag F0790)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, it was determined that for one (R98) out of two sampled residents for dental services, the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for one (R7) out of five residents reviewed for unnecessary medication administration, the facility failed to properly identify the appropr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined that the facility failed to provide one (R98) out five sampled residents for immunizations, an informed consent for four administered doses of t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and interview, it was determined that the facility failed to ensure that all staff employ hygienic practices, ensure the safe storage of food and beverages, and ensure food storag...
Read full inspector narrative →
Jan 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, staff interview, review of other facility documentation, and EMS records as indicated, it was determined...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews, interviews and review of facility documentation, it was determined that for one (R1) out of three (3) s...
Read full inspector narrative →
Dec 2022
2 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0678
(Tag F0678)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, record review and review of other documentation as indicated, it was determined that for one (R1) out of thr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, it was determined that for one (R1) out of three residents reviewed for a change in condit...
Read full inspector narrative →
Nov 2022
6 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
2. Review of R8's clinical record revealed:
2/25/22 - R8 was admitted to the facility.
3/1/22 - An admission MDS assessment documented that R8 was severely cognitively impaired, dependent on staff f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for one (R7) out of three residents sampled for activities of daily living, the facility failed to ensure that a resident who was unable to...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, it was determined that for one (R3) out of three residents sampled for range of motion (ROM), the facility failed to ensure consistent treatment and ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for one (R1) out of three residents reviewed for medication errors, the facility failed to administer R1's antibiotic as ordered when R1 wa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that for one (R8) out of ten residents reviewed, the facility failed to ensure the accuracy of medical records. Findings include:
Cross refer F...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
Based on record review, interview, and review of other documentation, it was determined that for three (R1, R4 and R8) out of three residents sampled for falls, the facility failed to complete post fa...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s), 5 harm violation(s), $109,425 in fines. Review inspection reports carefully.
- • 74 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $109,425 in fines. Extremely high, among the most fined facilities in Delaware. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Evergreen Post Acute's CMS Rating?
CMS assigns EVERGREEN POST ACUTE an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Delaware, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Evergreen Post Acute Staffed?
CMS rates EVERGREEN POST ACUTE's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 48%, compared to the Delaware average of 46%. RN turnover specifically is 64%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Evergreen Post Acute?
State health inspectors documented 74 deficiencies at EVERGREEN POST ACUTE during 2022 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 5 that caused actual resident harm, 67 with potential for harm, and 1 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Evergreen Post Acute?
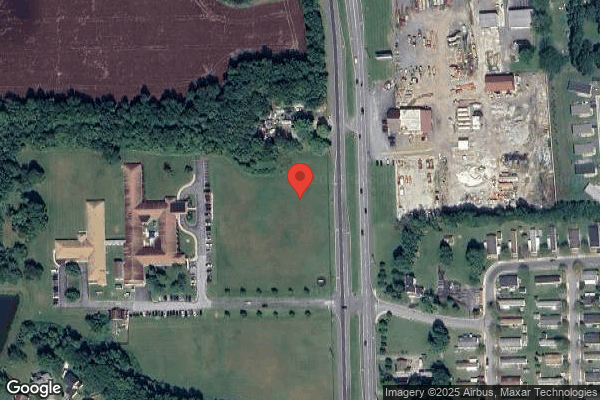
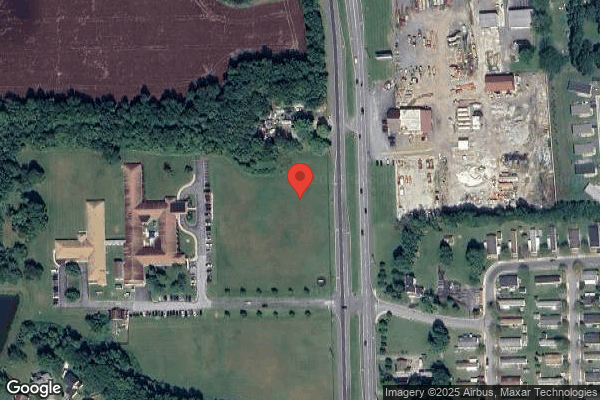
EVERGREEN POST ACUTE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PRESTIGE HEALTHCARE ADMINISTRATIVE SERVICES, a chain that manages multiple nursing homes. With 151 certified beds and approximately 130 residents (about 86% occupancy), it is a mid-sized facility located in SMYRNA, Delaware.
How Does Evergreen Post Acute Compare to Other Delaware Nursing Homes?
Compared to the 100 nursing homes in Delaware, EVERGREEN POST ACUTE's overall rating (2 stars) is below the state average of 3.3, staff turnover (48%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Evergreen Post Acute?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Evergreen Post Acute Safe?
Based on CMS inspection data, EVERGREEN POST ACUTE has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Delaware. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Evergreen Post Acute Stick Around?
EVERGREEN POST ACUTE has a staff turnover rate of 48%, which is about average for Delaware nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Evergreen Post Acute Ever Fined?
EVERGREEN POST ACUTE has been fined $109,425 across 3 penalty actions. This is 3.2x the Delaware average of $34,173. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Evergreen Post Acute on Any Federal Watch List?
EVERGREEN POST ACUTE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.