CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to protect the residents' right to be free from neglec...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to protect the residents' right to be free from neglect to ensure two residents (#10, #12) out of 11 residents at risk, with known neurocognitive disorders and/or dementia and a history of wandering and exit seeking, was provided supervision and services to prevent elopement. The facility neglected to maintain an exit door alarm system in proper operation or implement alternate methods to prevent elopements since 08/02/2023.
The facility nursing staff neglected to ensure the safety of Resident #10, from approximately 12:40 p.m. until 1:37 p.m. or approximately 57 minutes on 09/02/2023. Resident #10 exited the front door unobserved by staff. She traveled down a steep drive, across a street to an apartment building parking lot which was approximately 600 feet away. She was discovered and returned to the facility by a male resident of the apartment complex.
The facility nursing staff neglected to ensure the safety of Resident #12. Resident #12 was able to exit the facility unsupervised on 08/28/2023. Resident #12 was able to tailgate out the front entrance of the facility. The resident was discovered outside by staff and brought back into the facility.
The facility was aware the door alarming system was not operating properly since 08/02/2023, and despite this knowledge the facility neglected to put interventions in place to prevent the elopements of Resident #10 and Resident #12.
This neglect created a situation that resulted in the likelihood for serious injury and or death to Resident #10 and Resident #12 and resulted in the determination of Immediate Jeopardy on 08/02/2023. The findings of Immediate Jeopardy were determined to be removed on 10/06/2023 and the severity and scope was reduced to a D after verification of removal of Immediate Jeopardy.
Findings included:
During a phone interview on 10/06/2023 at 9:21 a.m. a customer service representative from the [contracted technology company] stated, On 09/05/2023, they had issues with the [wandering alarm system] reception. It was not picking up the transmissions all the time. On 08/02/2023 we initially talked to them about the issue. We did some trouble shooting steps over the phone but was unable to solve the issue. We sent them a service agreement form (Authorization Form) for signature. We did not get the form back. We have to have a signature on an Authorization Form before we send anyone out. On 09/02/2023, the Maintenance Director called back about the same issue. Again, one of the techs tried to troubleshoot over the phone but was unable to. We resent the form that day, 09/02/2023, and received it back the same day. We dispatched it for 09/05/2023. On 09/05/2023 the tech arrived, he checked the main entrance, and adjusted the antennas. He adjusted the wire termination for a timer and bypass button. After the test it was working fine. He tested all the other doors. The termination wires on the keypads adjust the schedule of opening and closing of the door. He checked the wiring only it did not have to be replaced or repaired.
Resident #10 was admitted on [DATE] and readmitted on [DATE]. Record review showed diagnoses included but were not limited to neurocognitive disorder with Lewy bodies; brief psychotic disorder; adjustment disorder with anxiety; generalized anxiety disorder; unspecified lack of coordination; Diabetes; muscle weakness (generalized); other abnormalities of gait and mobility; difficulty in walking, not elsewhere classified; major depressive disorder, recurrent moderate; and essential hypertension. Record review of the annual, Minimum Data Set (MDS), dated [DATE], showed in Section C: Cognitive Function, a Brief Interview Mental Status (BIMS) score of 04, indicating severe cognitive impairment; Section G: Functional Status showed the resident required extensive assistance of two for bed mobility, extensive assistance of one for toileting, limited assistance of two for transfers, and she was independent on and off the unit. Section E: Behaviors showed wandering behavior were not exhibited.
Review of the Physician Orders Summary for September 2023 showed the following:
Actively Exit Seeking Record Intervention Code (s): 1. N/A, 2. Engage in conversation, 3. Redirect to alternative location in facility, 4. Call family/friend 5. Activity, 6. Give snacks/food, 7. Give fluids, 8. Toileting (every shift) as of 07/22/2022.
Actively Exit Seeking Record Outcome Code: 1. N/A, 2. Improved, 3. Worsening, 4. Unchanged, if worsening / unchanged, notify supervisor (every shift) as of 07/22/2022.
Behavior Monitoring -Active Exit Seeking Record the Number of Occurrences every shift, (0 if did not occur) as of 07/22/2022. Psychiatric Consult for Evaluation and follow as needed as of 01/09/2023.
Wanderguard (wandering device)- check function every night shift for wandering device use as of 07/22/2022.
Wandering device - Check placement to LLE (Left lower extremity) every shift for wandering device use as of 07/22/2022.
Wandering device to LLE due to: Elopement Risk as of 03/10/2023 and expires 10/08/2023.
Depakote Oral Tablet Delayed Release 125 mg (milligram) every 12 hours for anxiety as of 07/30/2023 and was increased to 250 mg every 12 hours for mood disorder as of 09/05/2023.
Memantine HCL 10 mg every 12 hours for dementia as of 08/03/2020.
Mirtazapine 7.5 mg in the morning for depression as of 02/01/2023.
UA with C and S (urine analysis with Culture and Sensitivity) on 09/06/2023.
Cipro 500 mg every 12 hours for UTI (Urinary Tract Infection) for 7 days as of 09/10/2023.
Review of the September 2023 Behaviors Record showed the following:
Actively Exit Seeking Record Intervention Code (s): 1. N/A, 2. Engage in conversation, 3. Redirect to alternative location in facility, 4. Call family/friend 5. Activity, 6. Give snacks/food, 7. Give fluids, 8. Toileting (every shift) as of 07/22/2022. On 09/02/23 N/A for day shift was documented.
Actively Exit Seeking Record Outcome Code: 1. N/A, w. Improved, 3. Worsening, 4. Unchanged, if worsening / unchanged, notify supervisor (every shift) as of 07/22/2022 on 09/02/23 N/A for day shift.
Behavior Monitoring -Active Exit Seeking Record the Number of Occurrences every shift, (0 if did not occur) as of 07/22/2022. On 09/02/2023 0 was documented.
Review of the September 2023 Treatment Administration Record (TAR) showed the following:
Wandering device - check function every night shift for wandering device use as of 07/22/2022. On 09/01/2023 it was documented as checked by nursing.
Wandering device - Check placement to LLE (Left lower extremity) every shift for wandering device use as of 07/22/2022. On 09/02/2023 it was documented as checked on the day shift.
Review of Resident #10's progress notes showed no documentation regarding an elopement on 09/02/2023.
Review of the nursing progress notes dated 09/05/2023 at 2:48 p.m. showed the following:
Psychiatric Nurse Practitioner on site for visit with resident. New orders were given to increase her Depakote from 125 mg PO [by mouth] BID [twice a day] to 250 mg PO BID. Entered into PCC [Point Click Care or electronic medical record].
Review of Resident #10's Elopement Risk Evaluation, dated 07/02/2023 showed the following:
1. Is resident ambulatory and / or able to self-propel wheelchair? Yes.
2. Presence of any of the following risk factors indicates the resident is a risk for elopement.
2b. Resident displays behaviors indicting desire to leave the facility, i.e., packing belongings, tailgating, searching for exits from facility or searching for someone/something from past life events, verbalizing desire to go home/elsewhere.
2d. Resident's family/responsible party expressed concerns resident may attempt to leave.
3. Resident is 1. At risk for elopement.
Review of Resident #10's Elopement Risk Evaluation. dated 09/02/2023 showed the following:
1. Is resident ambulatory and / or able to self-propel wheelchair? Yes.
2. Presence of any of the following risk factors indicates the resident is a risk for elopement.
2b. Resident displays behaviors indicting desire to leave the facility, i.e., packing belongings, tailgating, searching for exits from facility or searching for someone/something from past life events, verbalizing desire to go home/elsewhere.
3. Resident is 1. At risk for elopement.
During an interview on 10/05/2023 at 12:30 p.m. with the Advanced Practice Registered Nurse (APRN) she stated Resident #10 had a little bit of confusion, and thought she was going home, and she went out to the park. That was not her normal. She did a urinalysis (UA) and culture and sensitivity (C/S) and placed her on antibiotics. She was back to normal. Her Depakote was increased on 09/05/2023. Her urinalysis was on 09/06/2023 and results on 09/09/2023. Cipro was started on 09/10/2023 for 10 days. The facility told her when she came into the facility the resident had eloped, they did not call her. They called the psychiatric nurse because it was exit-seeking.
Record review of the UA and C/S, dated 09/06/2023, showed over 100,000 Escherichia Coli microorganisms in the urine.
Review of the care plans showed as of 08/18/2022 Resident #10 was at risk for elopement / exit seeking activity, exit seeking, aimless wandering due to cognition, has the potential to approach exit doors.
A goal initiated on 08/18/2022 showed the resident will not leave facility unattended through the review date of 10/15/2023.
The interventions included but were not limited to the following:
On 08/18/2022, checking for proper functioning of the audible alarm system daily and prn (as needed).
On 08/18/2022, check functioning of wandering device every night.
Revised on 05/25/2023, check placement of wandering device every shift - LLE.
On 08/18/2022, Discuss with resident / family the risk of elopement and wandering.
On 07/27/2023, Encourage resident to participate in activities and redirect resident when exit seeking.
Revised on 5/25/2023, Every 1-hour safety checks monitor resident due to identified elopement risk.
On 08/18/2022, Indicate risk in Care Profile and Kardex, Place demographics in Risk Binders.
On 08/18/2022, Monitor resident for tailgating when visitors are in the building.
On 08/18/2022, Monitor resident for active exit seeking behavior each shift.
On 08/18/2022, Use audible monitoring system to alert staff of exit seeking behaviors.
On 08/18/2022, Use diversional activities when exit-seeking behavior is occurring (i.e., offer food, activities, one-on-one company).
An observation and interview were conducted on 10/02/2023 at 10:15 a.m., Resident #10 was lying in bed, awake. Her wandering device was observed on her RUE (Right Upper Extremity). The head of the bed was elevated. She stated, I went on a walk last week, to the mall, went by myself because no one could take me. I went up a hill.
During an interview and observation on 10/02/2023 at 1:15 p.m. Staff B, LPN (Licensed Practical Nurse) was asked to locate Resident #10's wandering device. Staff B was unable to find the wandering device on Resident #10's LLE. She stated, It is supposed to be there (lifting up the resident's pants legs). Staff B went into the bathroom to look at the resident's wheelchair and it was not present. Staff B was observed locating the wandering device on her RUE. She stated, It's on her RUE. Staff B, LPN attempted to remove the wandering device, and stated it could not be taken off even with effort.
An observation was conducted on 10/04/2023 at 10:35 a.m. Resident #10 was dressed and groomed for the day and seated in her wheelchair. She was located in the dining room looking out the dining room door. She was alone. She demonstrated she was able to move herself in her wheelchair with her feet. The wandering device was observed on her RUE.
During an interview on 10/03/2023 at 8:57 a.m. the DON was asked for a timeline.
A timeline provided on 10/03/2023 at 11:20 a.m. revealing the following:
09/02/23, approximately 12:40 p.m. resident observed exiting dining room after lunch.
09/02/23, approximately 12:45 p.m. nurse reports seeing resident wheel herself down hall.
09/02/23, approximately 1:37 p.m., resident returned to facility by neighbor, Staff F, receptionist was alerted by sounding of the alarm.
09/02/23, approximately 1:38 p.m., resident assessed by social services, floor nurse to have no injuries.
09/02/23, approximately 1:50 p.m., head count initiated on facility residents with no other issues noted.
09/02/23, approximately 2:00 p.m., Social Service Director (SSD) placed on door monitoring.
09/02/23, approximately 2:35 p.m., DON arrived at the facility to assess the event, and complete head to toe assessment on Resident #10. The resident was placed on 1:1 supervision.
09/02/23 approximately 3:15 p.m., NHA, Maintenance Director arrived to assess doors.
Review of the [contracted technology company] On-Site Service Charge Authorization Form dated 08/02/2023 showed, Customer Described Problem: Maintenance Director called in requesting a Service Call to have a tech work on the Main Entrance's ANT (antenna) range as some residents have been able to escape without setting off the alarm. On the lower half of the form, it showed, My signature on this agreement certifies that I am an authorized agent for the facility listed above. It was signed as authorized by the NHA on 09/01/2023.
Review of the [contracted electric company] Invoice dated 08/23/23 showed:
The following charges are for electrical work performed as listed:
Inspected the lobby door.
Opened the panel and tested power.
Found the panel power was testing for 17 volts AC (alternating current) and 0 volts DC (direct current).
Replaced the power supply for 12 volt, applied power to panel.
Tested receivers and found the receiver on antenna 4 was not functioning.
Replaced the receiver from maintenance stock and placed antenna for circuits on antenna 1 terminal.
Ranged all three receivers.
Receivers picked up transmitter and door annunciates while the transmitter is in range and door is ajar.
Found three outdated transmitters before testing with a in date transmitter.
Administration was not in the building.
Maintenance came in for a brief period of time to check how wandering device range test was going then departed.
Labor one tech 4.5 hours weekend labor
Review of the Service Call Job Form, dated 09/05/23, [contracted technology company] showed under description Maintenance Director called in requesting a Service Call to have a tech work on the Main Entrance's antennae range as some residents have been able to escape without setting off the alarm. Documentation showed On site met Maintenance Director and NHA. Checked and tested the main entry 9450 T70 with 3 duo link antennae. Adjusted the door antenna and adjusted wiring terminations for timer and bypass button / IEIKeypad. System working as designed. While on site, checked and tested all remaining Code Alert door systems for working order. System ok.
Review of the electronic maintenance system dated 08/28/2023 through 09/01/2023 showed the following: Residents Monitoring Systems: Check operation of door monitors and patient wandering system performed by Maintenance Director revealed all doors including the Main Entrance Pass. On 09/02/2023 a handwritten form showed all doors including the Main Entrance Pass and was completed by the Maintenance Director. Documentation at the bottom of the 09/02/2023 form showed, Spoke with [contracted technology company] tech about adjusting T10 (antenna). We got it dialed in good. Therapy patio longer than usual on door alarm.
During an interview on 10/02/2023 at 1:00 p.m. the Maintenance Director was observed checking the following exit doors: Therapy Hall, [NAME] Hall, Magnolia Hall, Smoking Area, Delta Hall, and Park Hall, Laundry door and Dining Room. All alarmed doors were in working order. He stated the alarmed doors had a 15-second delay alarm. He stated he checks the door alarms daily. He stated the front door was unlocked from about 7 a.m. to 5 p.m. but it won't open if a resident has a wandering device on. When asked what happened on 09/02/2023, he stated I do not know.
During an observation on 10/02/2023 at 1:40 p.m. the dining room door screeching alarm went off twice. On investigation, the activity assistant was taking residents out for air and guitar playing. No other staff members responded to the alarms. The activity assistant set it off again and again and no one responded, this included the kitchen staff.
During an observation on 10/02/23 at 1:50 p.m. the Maintenance Director tested a wandering device at the front door. The door did alarm during the test. He stated the door will not open if a wandering device comes near the door. If the door was open it would alarm. He again said he did not know what went wrong (09/02/2023). He stated, I just called the company, and they adjusted the antennas.
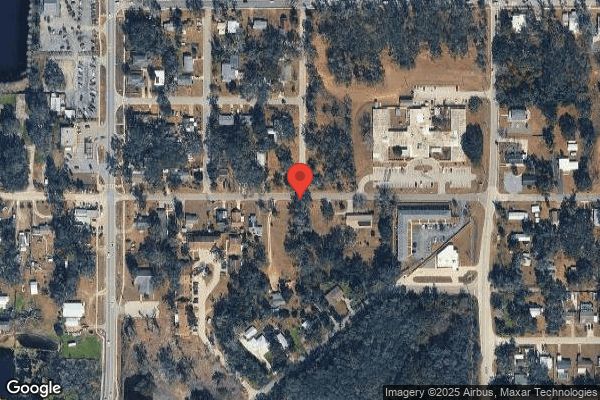
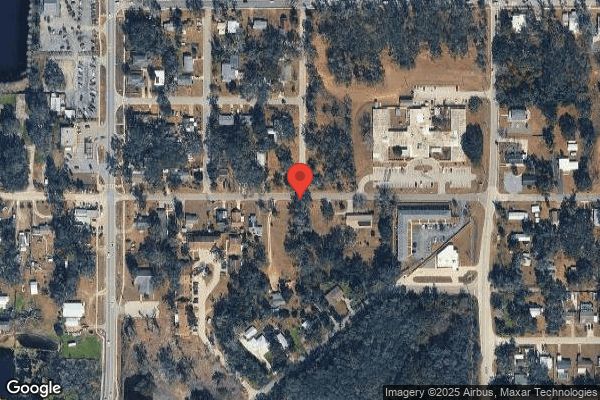
On 10/02/23 at 2:55 p.m. Resident #10's elopement route was observed with the DON and the Regional Nursing Home Administrator (RNHA). This included walking down a steeply sloped driveway and crossing a 2-lane street with a speed limit of 30 miles per hour. There was an occasional car observed going down the street. Resident #10 entered the grounds of an apartment complex. She was found by a gentleman at the back of the apartment complex parking lot. The DON stated she and the NHA went door-to-door in the apartment complex and found the gentleman who brought Resident #10 back. He informed them where he found her in the parking lot. He told the DON and the NHA the resident had told him she wanted to get to the playground, which is part of the apartment complex where she was found. He told them she was calm and was just sitting in her wheelchair. He said he tried to change her mind about going to the playground. (Photographic evidence obtained).
During an interview on 10/02/2023 at 3:12 p.m. the Maintenance Director was asked about the statement on the On-Site Charge Authorization Form. He stated, I just was trying to get them (contracted technology company) to come for the antennas. He stated, It was the only thing I can think of. He verified a work order had been placed 30 days prior to the elopement. He stated he did check the main door, on 09/02/2023, when they came in, post elopement, he documented it was working.
During an interview on 10/02/2023 at 3:30 p.m. the Regional Nursing Home Administrator (RNHA) and the DON stated they verified there were two forms from the contracted technology company, Form 1 was On-site Service Charge Authorization Form, dated 08/02/2023 (a month before elopement), stating Maintenance Director called in requesting a Service Call to have a tech work on the Main Entrance's antennae range as some residents have been able to escape without setting off the alarm. It was signed by the NHA on 09/01/23 (a day before the elopement). The NHA was unavailable for an interview during the dates of the survey. Form 2 was Service Call Job Form, dated 09/05/2023. The RNHA stated when he was told about the elopement and the door problems, he told them to put someone on the door and get someone out to fix it as soon as possible (ASAP). The DON stated the NHA had chewed the contracted technology company out (for not responding timely). The RNHA stated the Maintenance Director told him they had receipts from another company, and the Maintenance Director was looking for the receipts.
The RNHA and Maintenance Director produced an invoice from a (contracted electric company). They stated they came out on 08/23/23. The RNHA stated they then called the manufacturer [contracted technology company] because the antennas were still not working properly. The RNHA, the Maintenance Director and the DON stated they could not get the contracted technology company to come out, so they called the contracted electric company to come out. The RNHA stated the main door was not alarming the way it should, so he told the facility to get the manufacturer (contracted technology company). The DON stated the door was supposed to be functioning but was not alarming. The contracted electric company installed new antennas. The contracted technology company came in and did not add any equipment but adjusted the antennas. The Maintenance Director stated he did not know if the antenna was adjusted by the contracted electric company, but it had to be readjusted.
During an interview with the DON on 10/03/2023 at 8:57 a.m. the DON stated she did a head-to-toe assessment on the resident, with no abnormal findings. The resident was fine. The resident told the DON she was going to work. The DON called the management team in. The DON stated no one saw her, she was able to leave the dining room on her own. The DON verified for approximately 57 minutes it was unknown where the resident was located. The DON stated Staff M, CNA was assigned to care for Resident #10 that day. The DON stated she interviewed Staff M and she saw the resident in the dining room at about 11:30 a.m. on 09/02/2023. The DON stated staffing was good on 09/02/2023, it was meeting the 2.0 minimum. The DON stated the documentation of the event (elopement) was part of the resident's risk notes. Those notes are not found in the resident's electronic medical records. The DON verified there was no documentation in the electronic medical record of the incident. She verified there was only a post evaluation which did not state she eloped. There was no documentation that the attending physician and / or responsible party had been notified. It was documented in the risk report. She stated they had psych (psychiatric services) in to see the resident. They had the attending physician in to see the resident. The DON verified the Psych note on 09/05/2023 showed She elopes and has outdoor privileges. Patient is now on 1:1 observation for safety measures and does not remember. DON stated, she does not have outdoor privileges. The DON stated she would ask medical records if there were any other notes that had not been uploaded. A Post Incident was in the chart. The DON stated, We had an IDT (Interdisciplinary Team) meeting and reviewed the care plan and made sure everything was there. We have an IDT meeting every morning and review all incidents that happen. The note for the IDT meeting was documented in the risk notes by the DON. They did not document the IDT meeting in the electronic medical chart. She stated they reviewed the care plans. They reassessed her elopement risk, performed labs, did a UA and C/S on 09/06/2023. On 09/05/23 they changed the Depakote order. The resident did have a UTI and was treated with antibiotics. She stated the care plan was updated with 1:1 supervision on 09/02/23.
During an interview on 10/03/2023 at 3:01 p.m. the DON stated, She (Resident #10) does not get up as much as she did. She had a UTI. She was used to seeing her up and about. The UTI kind of took her down a little bit. The Depakote may be making her sleepier. I will talk to psych the Advanced Practice Registered Nurse Practitioner (APRN). You have to approach her 'Resident #10 it is time to get up', vs. 'Do you want to get up?'. The DON stated she did not know of any other residents going out. The door was not sounding. She stated, I was used to hearing an alarm when a resident with a wandering device on got near the door. Maintenance told her Some residents have been able to escape without setting off the alarm, was stated (on the Service Form) due to it being so hard to get the company (contracted technology company) out. The DON stated the Maintenance Director and NHA were working it out (the door issue on 08/02/2023). She stated she did not know if the resident was tailgating or not. It (door locking and alarming) would sometimes not capture from the wandering device going out but would always capture on coming in. The DON stated no one was sitting at the main door until 09/02/2023. The DON stated if they knew it (the door) wasn't working, they would have put a staff member on the exit door 24/7 to ensure no one left the building who wasn't supposed to. Before the main door was only being monitored by the receptionist. She stated, She was not aware there was anything wrong with the door. The DON stated, It wasn't always consistently picking them up, but they were picked up and staff intervened.
During an interview on 10/03/2023 at 4:10 p.m. the Maintenance Director stated, The sound announced but it did not announce like it was supposed to be. The door was functioning like it was supposed to but not the sound. I don't know, it was a while ago. He stated, Am positive it was announcing in the past, it has a speaker in it. I know they have to report if someone escapes. If there is an issue, I have to take care of it. I have to do my part. We have had residents escape before and it was reported to you guys. If a resident got out, you guys know about it. The NHA was aware there was a problem. I handed the On-Site Service Charge Authorization Form to the administrator at the time (08/02/2023). I do not know who it was (that eloped). I explained what was going on and [contracted electric company] did a complete check. We had an antenna in the building, and [contracted electric company] replaced it. He did fix the sound, don't know what was going on, but he fixed it. I may have been on the phone with the company (contracted technology company) on 09/02/2023, trying to get them out here. They (contracted technology company) adjusted the two antennas to their full potential range. They are in a half circle. I tested the doors when everyone came in on Saturday, 09/02/2023. It (the testing) was handwritten that I checked all the doors on 09/02/2023. I can't remember that part, if the NHA checked her (the resident's) wandering device and was it was working part time.
During an interview on 10/03/23 at 4:35 p.m. SSD, which was present on the day of the elopement, stated on 09/02/23 she did not know when Resident #10 got out or how. The SSD had gone up front to relieve the receptionist for lunch. Staff F, receptionist, came back from lunch and she stated she came back to her office. Some guy said Resident #10 was across the street. Staff F took her to the nurses' station. Resident #10 then came to my door. She was not sweating; skin was cool to the touch. Resident #10 went down the hall, stated She was going to see her friend. The man (who brought her back) was gone. When she got out the door it was not working. She stated she sat at the main door from about 2 p.m. until 6 p.m. She did not know if the door made a noise or not, but it was supposed to lock down, for residents with a wandering device. It (the door) would lock when they got close to the door, but she did not know about the alarms. Resident #10 would get up and go, she was able to self-propel herself.
During an interview on 10/04/23 at 9:02 a.m. Staff M, CNA, who was present on the day of the elopement, stated she was Resident #10's aide that day. She was in the dining room that day. She got her up in the morning and went to the bathroom. The resident wandered. She saw her after lunch. She was walking down the hall and the nurse said she was outside. It was around lunch. She saw her after dining wandering.
During an interview over the phone on 10/04/2023 at 12:58 p.m. Staff L, LPN, who was present on the day of the elopement, stated the resident was up and down the hallways in her wheelchair. She had Just seen her 1 minute before that happened. She could have Only been out of the building for 2 or 3 minutes. She thought she went out behind someone. There was no way she got out of the parking lot, she had to be on the patio and brought her back in. There was no way she would have gotten down the driveway in her wheelchair. Stated she did not see how she got in the parking lot. She stated she had just seen her 5 minutes before they called, she was out the door. They tested the wandering device. The wandering device on the way back in, it went off. She was assessed, looked over, nothing was wrong. The aides Put her back to bed. They called a Code Gray and we had to make sure all the residents were accounted for. We looked her over, she had no bruises or skin tears. Staff L said she did not know the door was not working. We have a lot of residents who go out to the patio (outside the front door). Resident #10 was the only one she knew of who got out. The receptionist was right there at the door.
During an interview on 10/04/2023 at 1:25 p.m. Staff I, CNA, who was present on the day of the elopement, stated she worked that day but did not have the resident assigned to her. She saw her in the day room in the morning watching TV (before lunch). Staff M, CNA took her to the dining room. Staff I stated, She got out and some guy brought her back in. The alarm did not go off. No Code Gray was called. We looked for all the residents. Stated no other resident has gotten out that she was aware of and had not heard that the door was not working.
During an interview on 10/04/23 at 8:55 a.m. Staff G, LPN, who was present on the day of the elopement, stated we had somebody in the front (office). She stated she went up front to make a copy or something. Somebody (SSD) had to go to the bathroom and was gone for 2 - 3 minutes. She was watching the front. She did not remember seeing Resident #10. They (person in the bathroom, SSD) came back and she went back to the floor. A Code Gray was not called that day. We were told to count heads.
During an interview on 10/04/2023 at 3:43 p.m. Staff F, receptionist, who was present on the day of the elopement, stated she went to lunch (on 9/2/2023) around 11:30 or 11:45 a.m. and returned around 12:15 p.m. When she got back, the SSD was in the office, the SSD returned to her office. She had gone to the copier and heard the door alarm go off. A gentleman was pushing Resident #10 back in the door, she didn't remember the time. She went up to the door and was turning off the alarm and tried to talk to him. It was hard to hear him due to the alarm sounding. He said he found her and was bringing her back. She took Resident #10 to the nurses' station on the [NAME] Wing where she was from and alerted the nurse. She alerted Staff L and Staff J. She then stated she informed the SSD, and the SSD notified the DON. She went back up front to her desk to watch the door. She stated if someone was coming in and a resident with a wandering device was going out, the door sometimes canceled the alarm out. There had been problems with the doors in the past, they told her they were fixed. It was about 4-6 months ago, and they were fixed within 24 hours. That was the only time she knew the door was malfunctioning. She stated she was at lunch and not aware Resident #10 was out of the building. She was not aware of any other residents getting out. She stated, It was hard to be vigilant with only one person in the office on the weekends.
During an interview on 10/04/23 at 12:00 p.m. Staff J, restorative CNA stated she was doing the dining room that day. Resident #10 left the dining room. That was the last time she saw her. She did see her going up and down the hallways. She left the dining room around 12:00 p.m.to 12:30 p.m.
During an interview on 10/04/2023 at 3:11 p.m. Staff N, Admissions Coordinator stated if a resident with a wandering device was near the door there was no alarm, but the door would stay closed. If a resident with a wandering device went in or out through the open
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure two residents (#10, #12) out of 11 residents...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure two residents (#10, #12) out of 11 residents at risk, with known neurocognitive disorders and / or dementia and a history of wandering and exit seeking, was provided supervision and services to prevent elopement. The facility failed to maintain an exit door alarm system in proper operation to prevent elopements since 08/02/2023.
The facility nursing staff failed to ensure the safety of Resident #10, from approximately 12:40 p.m. until 1:37 p.m. or approximately 57 minutes on 09/02/2023. Resident #10 exited the front door unobserved by staff. She traveled down a steep drive, across a street to an apartment building parking lot which was approximately 600 feet away. She was discovered and returned to the facility by a male resident of the apartment complex.
The facility nursing staff failed to ensure the safety of Resident #12. Resident #12 was able to exit the facility unsupervised on 08/28/2023. Resident #12 was able to tailgate out the front entrance of the facility. The resident was discovered outside by staff and brought back into the facility.
This failure created a situation that resulted in the likelihood for serious injury and or death to Resident #10 and resulted in the determination of Immediate Jeopardy on 08/02/2023. The findings of Immediate Jeopardy were determined to be removed on 10/06/2023 and the severity and scope was reduced to a D after verification of removal of Immediate Jeopardy.
Findings included:
During a phone interview on 10/06/2023 at 9:21 a.m. a customer service representative from the [contracted technology company] stated, On 09/05/2023, they had issues with the [wandering alarm system] reception. It was not picking up the transmissions all the time. On 08/02/2023 we initially talked to them about the issue. We did some trouble shooting steps over the phone but was unable to solve the issue. We sent them a service agreement form (Authorization Form) for signature. We did not get the form back. We have to have a signature on an Authorization Form before we send anyone out. On 09/02/2023, the Maintenance Director called back about the same issue. Again, one of the techs tried to troubleshoot over the phone but was unable to. We resent the form that day, 09/02/2023, and received it back the same day. We dispatched it for 09/05/2023. On 09/05/2023 the tech arrived, he checked the main entrance, and adjusted the antennas. He adjusted the wire termination for a timer and bypass button. After the test it was working fine. He tested all the other doors. The termination wires on the keypads adjust the schedule of opening and closing of the door. He checked the wiring only it did not have to be replaced or repaired.
Resident #10 was admitted on [DATE] and readmitted on [DATE]. Record review showed diagnoses included but were not limited to neurocognitive disorder with Lewy bodies; brief psychotic disorder; adjustment disorder with anxiety; generalized anxiety disorder; unspecified lack of coordination; Diabetes; muscle weakness (generalized); other abnormalities of gait and mobility; difficulty in walking, not elsewhere classified; major depressive disorder, recurrent moderate; and essential hypertension. Record review of the annual, Minimum Data Set (MDS), dated [DATE], showed in Section C: Cognitive Function, a Brief Interview Mental Status (BIMS) score of 04, indicating severe cognitive impairment; Section G: Functional Status showed the resident required extensive assistance of two for bed mobility, extensive assistance of one for toileting, limited assistance of two for transfers, and she was independent on and off the unit. Section E: Behaviors showed wandering behavior were not exhibited.
Review of the Physician Orders Summary for September 2023 showed the following:
Actively Exit Seeking Record Intervention Code (s): 1. N/A, 2. Engage in conversation, 3. Redirect to alternative location in facility, 4. Call family/friend 5. Activity, 6. Give snacks/food, 7. Give fluids, 8. Toileting (every shift) as of 07/22/2022.
Actively Exit Seeking Record Outcome Code: 1. N/A, 2. Improved, 3. Worsening, 4. Unchanged, if worsening / unchanged, notify supervisor (every shift) as of 07/22/2022.
Behavior Monitoring -Active Exit Seeking Record the Number of Occurrences every shift, (0 if did not occur) as of 07/22/2022. Psychiatric Consult for Evaluation and follow as needed as of 01/09/2023.
Wanderguard (wandering device)- check function every night shift for wandering device use as of 07/22/2022.
Wandering device - Check placement to LLE (Left lower extremity) every shift for wandering device use as of 07/22/2022.
Wandering device to LLE due to: Elopement Risk as of 03/10/2023 and expires 10/08/2023.
Depakote Oral Tablet Delayed Release 125 mg (milligram) every 12 hours for anxiety as of 07/30/2023 and was increased to 250 mg every 12 hours for mood disorder as of 09/05/2023.
Memantine HCL 10 mg every 12 hours for dementia as of 08/03/2020.
Mirtazapine 7.5 mg in the morning for depression as of 02/01/2023.
UA with C and S (urine analysis with Culture and Sensitivity) on 09/06/2023.
Cipro 500 mg every 12 hours for UTI (Urinary Tract Infection) for 7 days as of 09/10/2023.
Review of the September 2023 Behaviors Record showed the following:
Actively Exit Seeking Record Intervention Code (s): 1. N/A, 2. Engage in conversation, 3. Redirect to alternative location in facility, 4. Call family/friend 5. Activity, 6. Give snacks/food, 7. Give fluids, 8. Toileting (every shift) as of 07/22/2022. On 09/02/23 N/A for day shift was documented.
Actively Exit Seeking Record Outcome Code: 1. N/A, w. Improved, 3. Worsening, 4. Unchanged, if worsening / unchanged, notify supervisor (every shift) as of 07/22/2022 on 09/02/23 N/A for day shift.
Behavior Monitoring -Active Exit Seeking Record the Number of Occurrences every shift, (0 if did not occur) as of 07/22/2022. On 09/02/2023 0 was documented.
Review of the September 2023 Treatment Administration Record (TAR) showed the following:
Wandering device - check function every night shift for wandering device use as of 07/22/2022. On 09/01/2023 it was documented as checked by nursing.
Wandering device - Check placement to LLE (Left lower extremity) every shift for wandering device use as of 07/22/2022. On 09/02/2023 it was documented as checked on the day shift.
Review of Resident #10's progress notes showed no documentation regarding an elopement on 09/02/2023.
Review of the nursing progress notes dated 09/05/2023 at 2:48 p.m. showed the following:
Psychiatric Nurse Practitioner on site for visit with resident. New orders were given to increase her Depakote from 125 mg PO [by mouth] BID [twice a day] to 250 mg PO BID. Entered into PCC [Point Click Care or electronic medical record].
Review of Resident #10's Elopement Risk Evaluation, dated 07/02/2023 showed the following:
1. Is resident ambulatory and / or able to self-propel wheelchair? Yes.
2. Presence of any of the following risk factors indicates the resident is a risk for elopement.
2b. Resident displays behaviors indicting desire to leave the facility, i.e., packing belongings, tailgating, searching for exits from facility or searching for someone/something from past life events, verbalizing desire to go home/elsewhere.
2d. Resident's family/responsible party expressed concerns resident may attempt to leave.
3. Resident is 1. At risk for elopement.
Review of Resident #10's Elopement Risk Evaluation. dated 09/02/2023 showed the following:
1. Is resident ambulatory and / or able to self-propel wheelchair? Yes.
2. Presence of any of the following risk factors indicates the resident is a risk for elopement.
2b. Resident displays behaviors indicting desire to leave the facility, i.e., packing belongings, tailgating, searching for exits from facility or searching for someone/something from past life events, verbalizing desire to go home/elsewhere.
3. Resident is 1. At risk for elopement.
During an interview on 10/05/2023 at 12:30 p.m. with the Advanced Practice Registered Nurse (APRN) she stated Resident #10 had a little bit of confusion, and thought she was going home, and she went out to the park. That was not her normal. She did a urinalysis (UA) and culture and sensitivity (C/S) and placed her on antibiotics. She was back to normal. Her Depakote was increased on 09/05/2023. Her urinalysis was on 09/06/2023 and results on 09/09/2023. Cipro was started on 09/10/2023 for 10 days. The facility told her when she came into the facility the resident had eloped, they did not call her. They called the psychiatric nurse because it was exit-seeking.
Record review of the UA and C/S, dated 09/06/2023, showed over 100,000 Escherichia Coli microorganisms in the urine.
Review of the care plans showed as of 08/18/2022 Resident #10 was at risk for elopement / exit seeking activity, exit seeking, aimless wandering due to cognition, has the potential to approach exit doors.
A goal initiated on 08/18/2022 showed the resident will not leave facility unattended through the review date of 10/15/2023.
The interventions included but were not limited to the following:
On 08/18/2022, checking for proper functioning of the audible alarm system daily and prn (as needed).
On 08/18/2022, check functioning of wandering device every night.
Revised on 05/25/2023, check placement of wandering device every shift - LLE.
On 08/18/2022, Discuss with resident / family the risk of elopement and wandering.
On 07/27/2023, Encourage resident to participate in activities and redirect resident when exit seeking.
Revised on 5/25/2023, Every 1-hour safety checks monitor resident due to identified elopement risk.
On 08/18/2022, Indicate risk in Care Profile and Kardex, Place demographics in Risk Binders.
On 08/18/2022, Monitor resident for tailgating when visitors are in the building.
On 08/18/2022, Monitor resident for active exit seeking behavior each shift.
On 08/18/2022, Use audible monitoring system to alert staff of exit seeking behaviors.
On 08/18/2022, Use diversional activities when exit-seeking behavior is occurring (i.e., offer food, activities, one-on-one company).
An observation and interview were conducted on 10/02/2023 at 10:15 a.m., Resident #10 was lying in bed, awake. Her wandering device was observed on her RUE (Right Upper Extremity). The head of the bed was elevated. She stated, I went on a walk last week, to the mall, went by myself because no one could take me. I went up a hill.
During an interview and observation on 10/02/2023 at 1:15 p.m. Staff B, LPN (Licensed Practical Nurse) was asked to locate Resident #10's wandering device. Staff B was unable to find the wandering device on Resident #10's LLE. She stated, It is supposed to be there (lifting up the resident's pants legs). Staff B went into the bathroom to look at the resident's wheelchair and it was not present. Staff B was observed locating the wandering device on her RUE. She stated, It's on her RUE. Staff B, LPN attempted to remove the wandering device, and stated it could not be taken off even with effort.
An observation was conducted on 10/04/2023 at 10:35 a.m. Resident #10 was dressed and groomed for the day and seated in her wheelchair. She was located in the dining room looking out the dining room door. She was alone. She demonstrated she was able to move herself in her wheelchair with her feet. The wandering device was observed on her RUE.
During an interview on 10/03/2023 at 8:57 a.m. the DON was asked for a timeline.
A timeline provided on 10/03/2023 at 11:20 a.m. revealing the following:
09/02/23, approximately 12:40 p.m. resident observed exiting dining room after lunch.
09/02/23, approximately 12:45 p.m. nurse reports seeing resident wheel herself down hall.
09/02/23, approximately 1:37 p.m., resident returned to facility by neighbor, Staff F, receptionist was alerted by sounding of the alarm.
09/02/23, approximately 1:38 p.m., resident assessed by social services, floor nurse to have no injuries.
09/02/23, approximately 1:50 p.m., head count initiated on facility residents with no other issues noted.
09/02/23, approximately 2:00 p.m., Social Service Director placed on door monitoring.
09/02/23, approximately 2:35 p.m., DON arrived at the facility to assess the event, and complete head to toe assessment on Resident #10. The resident was placed on 1:1 supervision.
09/02/23 approximately 3:15 p.m., NHA, Maintenance Director arrived to assess doors.
Review of the [contracted technology company] On-Site Service Charge Authorization Form dated 08/02/2023 showed, Customer Described Problem: Maintenance Director called in requesting a Service Call to have a tech work on the Main Entrance's ANT (antenna) range as some residents have been able to escape without setting off the alarm. On the lower half of the form, it showed, My signature on this agreement certifies that I am an authorized agent for the facility listed above. It was signed as authorized by the NHA on 09/01/2023.
Review of the [contracted electric company] Invoice dated 08/23/23 showed:
The following charges are for electrical work performed as listed:
Inspected the lobby door.
Opened the panel and tested power.
Found the panel power was testing for 17 volts AC (alternating current) and 0 volts DC (direct current).
Replaced the power supply for 12 volt, applied power to panel.
Tested receivers and found the receiver on antenna 4 was not functioning.
Replaced the receiver from maintenance stock and placed antenna for circuits on antenna 1 terminal.
Ranged all three receivers.
Receivers picked up transmitter and door annunciates while the transmitter is in range and door is ajar.
Found three outdated transmitters before testing with a in date transmitter.
Administration was not in the building.
Maintenance came in for a brief period of time to check how wandering device range test was going then departed.
Labor one tech 4.5 hours weekend labor
Review of the Service Call Job Form, dated 09/05/23, [contracted technology company] showed under description Maintenance Director called in requesting a Service Call to have a tech work on the Main Entrance's antennae range as some residents have been able to escape without setting off the alarm. Documentation showed On site met Maintenance Director and NHA. Checked and tested the main entry 9450 T70 with 3 duo link antennae. Adjusted the door antenna and adjusted wiring terminations for timer and bypass button / IEIKeypad. System working as designed. While on site, checked and tested all remaining Code Alert door systems for working order. System ok.
Review of the electronic maintenance system dated 08/28/2023 through 09/01/2023 showed the following: Residents Monitoring Systems: Check operation of door monitors and patient wandering system performed by Maintenance Director revealed all doors including the Main Entrance Pass. On 09/02/2023 a handwritten form showed all doors including the Main Entrance Pass and was completed by the Maintenance Director. Documentation at the bottom of the 09/02/2023 form showed, Spoke with [contracted technology company] tech about adjusting T10 (antenna). We got it dialed in good. Therapy patio longer than usual on door alarm.
During an interview on 10/02/2023 at 1:00 p.m. the Maintenance Director was observed checking the following exit doors: Therapy Hall, [NAME] Hall, Magnolia Hall, Smoking Area, Delta Hall, and Park Hall, Laundry door and Dining Room. All alarmed doors were in working order. He stated the alarmed doors had a 15-second delay alarm. He stated he checks the door alarms daily. He stated the front door was unlocked from about 7 a.m. to 5 p.m. but it won't open if a resident has a wandering device on. When asked what happened on 09/02/2023, he stated I do not know.
During an observation on 10/02/2023 at 1:40 p.m. the dining room door screeching alarm went off twice. On investigation, the activity assistant was taking residents out for air and guitar playing. No other staff members responded to the alarms. The activity assistant set it off again and again and no one responded, this included the kitchen staff.
During an observation on 10/02/23 at 1:50 p.m. the Maintenance Director tested a wandering device at the front door. The door did alarm during the test. He stated the door will not open if a wandering device comes near the door. If the door was open it would alarm. He again said he did not know what went wrong (09/02/2023). He stated, I just called the company, and they adjusted the antennas.
On 10/02/23 at 2:55 p.m. Resident #10's elopement route was observed with the DON and the Regional Nursing Home Administrator (RNHA). This included walking down a steeply sloped driveway and crossing a 2-lane street with a speed limit of 30 miles per hour. There was an occasional car observed going down the street. Resident #10 entered the grounds of an apartment complex. She was found by a gentleman at the back of the apartment complex parking lot. The DON stated she and the NHA went door-to-door in the apartment complex and found the gentleman who brought Resident #10 back. He informed them where he found her in the parking lot. He told the DON and the NHA the resident had told him she wanted to get to the playground, which is part of the apartment complex where she was found. He told them she was calm and was just sitting in her wheelchair. He said he tried to change her mind about going to the playground. (Photographic evidence obtained).
During an interview on 10/02/2023 at 3:12 p.m. the Maintenance Director was asked about the statement on the On-Site Charge Authorization Form. He stated, I just was trying to get them (contracted technology company) to come for the antennas. He stated, It was the only thing I can think of. He verified a work order had been placed 30 days prior to the elopement. He stated he did check the main door, on 09/02/2023, when they came in, post elopement, he documented it was working.
During an interview on 10/02/2023 at 3:30 p.m. the Regional Nursing Home Administrator (RNHA) and the DON stated they verified there were two forms from the contracted technology company, Form 1 was On-site Service Charge Authorization Form, dated 08/02/2023 (a month before elopement), stating Maintenance Director called in requesting a Service Call to have a tech work on the Main Entrance's antennae range as some residents have been able to escape without setting off the alarm. It was signed by the NHA on 09/01/23 (a day before the elopement). The NHA was unavailable for an interview during the dates of the survey.
Form 2 was Service Call Job Form, dated 09/05/2023, and stated Maintenance Director called in requesting a Service Call to have a tech work on the Main Entrance's antennae range as some residents have been able to escape without setting off the alarm. The Service Notes showed On site met Maintenance Director and the NHA. Checked and tested the main entry 9450 T70 with 3 duo link antennae. Adjusted the door antenna and adjusted wiring terminations for timer and bypass button / IEIKeypad. System working as designed. While on site, checked and tested all remaining Code Alert door systems for working order. System ok.
The RNHA stated when he was told about the elopement and the door problems, he told them to put someone on the door and get someone out to fix it as soon as possible (ASAP). The DON stated the NHA had chewed the contracted technology company out (for not responding timely). The RNHA stated the Maintenance Director told him they had receipts from another company, and the Maintenance Director was looking for the receipts.
The RNHA and Maintenance Director produced an invoice from a (contracted electric company). They stated they came out on 08/23/23. The RNHA stated they then called the manufacturer [contracted technology company] because the antennas were still not working properly. The RNHA, the Maintenance Director and the DON stated they could not get the contracted technology company to come out, so they called the contracted electric company to come out. The RNHA stated the main door was not alarming the way it should, so he told the facility to get the manufacturer (contracted technology company). The DON stated the door was supposed to be functioning but was not alarming. The contracted electric company installed new antennas. The contracted technology company came in and did not add any equipment but adjusted the antennas. The Maintenance Director stated he did not know if the antenna was adjusted by the contracted electric company, but it had to be readjusted.
During an interview with the DON on 10/03/2023 at 8:57 a.m. the resident told the DON she was going to work. The DON called the management team in. The DON stated no one saw her, she was able to leave the dining room on her own. The DON verified for approximately 57 minutes it was unknown where the resident was located. The DON stated Staff M, CNA was assigned to care for Resident #10 that day. The DON stated she interviewed Staff M and she saw the resident in the dining room at about 11:30 a.m. on 09/02/2023. The DON stated staffing was good on 09/02/2023, it was meeting the 2.0 minimum. The DON stated the documentation of the event (elopement) was part of the resident's risk notes. Those notes are not found in the resident's electronic medical records. The DON verified there was no documentation in the electronic medical record of the incident. She verified there was only a post evaluation which did not state she eloped. There was no documentation that the attending physician and / or responsible party had been notified. It was documented in the risk report. She stated they had psych (psychiatric services) in to see the resident. They had the attending physician in to see the resident. The DON verified the Psych note on 09/05/2023 showed She elopes and has outdoor privileges. Patient is now on 1:1 observation for safety measures and does not remember. DON stated, she does not have outdoor privileges. The DON stated she would ask medical records if there were any other notes that had not been uploaded. A Post Incident was in the chart. The DON stated, We had an IDT (Interdisciplinary Team) meeting and reviewed the care plan and made sure everything was there. We have an IDT meeting every morning and review all incidents that happen. The note for the IDT meeting was documented in the risk notes by the DON. They did not document the IDT meeting in the electronic medical chart. She stated they reviewed the care plans. They reassessed her elopement risk, performed labs, did a UA and C/S on 09/06/2023. On 09/05/23 they changed the Depakote order. The resident did have a UTI and was treated with antibiotics. She stated the care plan was updated with 1:1 supervision on 09/02/23.
During an interview on 10/03/2023 at 3:01 p.m. the DON stated, She (Resident #10) does not get up as much as she did. She had a UTI. She was used to seeing her up and about. The UTI kind of took her down a little bit. The Depakote may be making her sleepier. I will talk to psych the Advanced Practice Registered Nurse Practitioner (APRN). You have to approach her 'Resident #10 it is time to get up', vs. 'Do you want to get up?'. The DON stated she did not know of any other residents going out. The door was not sounding. She stated, I was used to hearing an alarm when a resident with a wandering device on got near the door. Maintenance told her Some residents have been able to escape without setting off the alarm, was stated (on the Service Form) due to it being so hard to get the company (contracted technology company) out. The DON stated the Maintenance Director and NHA were working it out (the door issue on 08/02/2023). She stated she did not know if the resident was tailgating or not. It (door locking and alarming) would sometimes not capture from the wandering device going out but would always capture on coming in. The DON stated no one was sitting at the main door until 09/02/2023. The DON stated if they knew it (the door) wasn't working, they would have put a staff member on the exit door 24/7 to ensure no one left the building who wasn't supposed to. Before the main door was only being monitored by the receptionist. She stated, She was not aware there was anything wrong with the door. The DON stated, It wasn't always consistently picking them up, but they were picked up and staff intervened.
During an interview on 10/03/2023 at 4:10 p.m. the Maintenance Director stated, The sound announced but it did not announce like it was supposed to be. The door was functioning like it was supposed to but not the sound. I don't know, it was a while ago. He stated, Am positive it was announcing in the past, it has a speaker in it. I know they have to report if someone escapes. If there is an issue, I have to take care of it. I have to do my part. We have had residents escape before and it was reported to you guys. If a resident got out, you guys know about it. The NHA was aware there was a problem. I handed the On-Site Service Charge Authorization Form to the administrator at the time (08/02/2023). I do not know who it was (that eloped). I explained what was going on and [contracted electric company] did a complete check. We had an antenna in the building, and [contracted electric company] replaced it. He did fix the sound, don't know what was going on, but he fixed it. I may have been on the phone with the company (contracted technology company) on 09/02/2023, trying to get them out here. They (contracted technology company) adjusted the two antennas to their full potential range. They are in a half circle. I tested the doors when everyone came in on Saturday, 09/02/2023. It (the testing) was handwritten that I checked all the doors on 09/02/2023. I can't remember that part, if the NHA checked her (the resident's) wandering device and was it was working part time.
During an interview on 10/03/23 at 4:35 p.m. SSD, which was present on the day of the elopement, stated on 09/02/23 she did not know when Resident #10 got out or how. The SSD had gone up front to relieve the receptionist for lunch. Staff F, receptionist, came back from lunch and she stated she came back to her office. Some guy said Resident #10 was across the street. Staff F took her to the nurses' station. Resident #10 then came to my door. She was not sweating; skin was cool to the touch. Resident #10 went down the hall, stated She was going to see her friend. The man (who brought her back) was gone. When she got out the door it was not working. She stated she sat at the main door from about 2 p.m. until 6 p.m. She did not know if the door made a noise or not, but it was supposed to lock down, for residents with a wandering device. It (the door) would lock when they got close to the door, but she did not know about the alarms. Resident #10 would get up and go, she was able to self-propel herself.
During an interview on 10/04/23 at 9:02 a.m. Staff M, CNA, who was present on the day of the elopement, stated she was Resident #10's aide that day. She was in the dining room that day. She got her up in the morning and went to the bathroom. The resident wandered. She saw her after lunch. She was walking down the hall and the nurse said she was outside. It was around lunch. She saw her after dining wandering.
During an interview over the phone on 10/04/2023 at 12:58 p.m. Staff L, LPN, who was present on the day of the elopement, stated the resident was up and down the hallways in her wheelchair. She had Just seen her 1 minute before that happened. She could have Only been out of the building for 2 or 3 minutes. She thought she went out behind someone. There was no way she got out of the parking lot, she had to be on the patio and brought her back in. There was no way she would have gotten down the driveway in her wheelchair. Stated she did not see how she got in the parking lot. She stated she had just seen her 5 minutes before they called, she was out the door. They tested the wandering device. The wandering device on the way back in, it went off. She was assessed, looked over, nothing was wrong. The aides Put her back to bed. They called a Code Gray and we had to make sure all the residents were accounted for. We looked her over, she had no bruises or skin tears. Staff L said she did not know the door was not working. We have a lot of residents who go out to the patio (outside the front door). Resident #10 was the only one she knew of who got out. The receptionist was right there at the door.
During an interview on 10/04/2023 at 1:25 p.m. Staff I, CNA, who was present on the day of the elopement, stated she worked that day but did not have the resident assigned to her. She saw her in the day room in the morning watching TV (before lunch). Staff M, CNA took her to the dining room. Staff I stated, She got out and some guy brought her back in. The alarm did not go off. No Code Gray was called. We looked for all the residents. Stated no other resident has gotten out that she was aware of and had not heard that the door was not working.
During an interview on 10/04/23 at 8:55 a.m. Staff G, LPN, who was present on the day of the elopement, stated we had somebody in the front (office). She stated she went up front to make a copy or something. Somebody (SSD) had to go to the bathroom and was gone for 2 - 3 minutes. She was watching the front. She did not remember seeing Resident #10. They (person in the bathroom, SSD) came back and she went back to the floor. A Code Gray was not called that day. We were told to count heads.
During an interview on 10/04/2023 at 3:43 p.m. Staff F, receptionist, who was present on the day of the elopement, stated she went to lunch (on 9/2/2023) around 11:30 or 11:45 a.m. and returned around 12:15 p.m. When she got back, the SSD was in the office, the SSD returned to her office. She had gone to the copier and heard the door alarm go off. A gentleman was pushing Resident #10 back in the door, she didn't remember the time. She went up to the door and was turning off the alarm and tried to talk to him. It was hard to hear him due to the alarm sounding. He said he found her and was bringing her back. She took Resident #10 to the nurses' station on the [NAME] Wing where she was from and alerted the nurse. She alerted Staff L and Staff J. She then stated she informed the SSD, and the SSD notified the DON. She went back up front to her desk to watch the door. She stated if someone was coming in and a resident with a wandering device was going out, the door sometimes canceled the alarm out. There had been problems with the doors in the past, they told her they were fixed. It was about 4-6 months ago, and they were fixed within 24 hours. That was the only time she knew the door was malfunctioning. She stated she was at lunch and not aware Resident #10 was out of the building. She was not aware of any other residents getting out. She stated, It was hard to be vigilant with only one person in the office on the weekends.
During an interview on 10/04/23 at 12:00 p.m. Staff J, restorative CNA stated she was doing the dining room that day. Resident #10 left the dining room. That was the last time she saw her. She did see her going up and down the hallways. She left the dining room around 12 to 12:30 p.m.
During an interview on 10/04/2023 at 3:11 p.m. Staff N, Admissions Coordinator stated if a resident with a wandering device was near the door
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure the Patient-Centered Care Plan was followed ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure the Patient-Centered Care Plan was followed for one resident (#10) out of 16 residents sampled.
Findings included:
Resident #10 was admitted on [DATE] and readmitted on [DATE]. Record review showed diagnoses included but were not limited to neurocognitive disorder with Lewy bodies; brief psychotic disorder; adjustment disorder with anxiety; generalized anxiety disorder; unspecified lack of coordination; Diabetes; muscle weakness (generalized); other abnormalities of gait and mobility; difficulty in walking, not elsewhere classified; major depressive disorder, recurrent moderate; and essential hypertension. Record review of the annual, Minimum Data Set (MDS), dated [DATE], showed in Section C: Cognitive Function, a Brief Interview Mental Status (BIMS) score of 04, indicating severe cognitive impairment; Section G: Functional Status showed the resident required extensive assistance of two for bed mobility, extensive assistance of one for toileting, limited assistance of two for transfers, and she was independent on and off the unit. Section E: Behaviors showed wandering behavior were not exhibited.
Review of the Physician Orders Summary for September 2023 showed the following:
Actively Exit Seeking Record Intervention Code (s): 1. N/A, 2. Engage in conversation, 3. Redirect to alternative location in facility, 4. Call family/friend 5. Activity, 6. Give snacks/food, 7. Give fluids, 8. Toileting (every shift) as of 07/22/2022.
Actively Exit Seeking Record Outcome Code: 1. N/A, 2. Improved, 3. Worsening, 4. Unchanged, if worsening / unchanged, notify supervisor (every shift) as of 07/22/2022.
Behavior Monitoring -Active Exit Seeking Record the Number of Occurrences every shift, (0 if did not occur) as of 07/22/2022. Psychiatric Consult for Evaluation and follow as needed as of 01/09/2023.
Wanderguard (wandering device)- check function every night shift for wandering device use as of 07/22/2022.
Wandering device - Check placement to LLE (Left lower extremity) every shift for wandering device use as of 07/22/2022.
Wandering device to LLE due to: Elopement Risk as of 03/10/2023 and expires 10/08/2023.
Depakote Oral Tablet Delayed Release 125 mg (milligram) every 12 hours for anxiety as of 07/30/2023 and was increased to 250 mg every 12 hours for mood disorder as of 09/05/2023.
Memantine HCL 10 mg every 12 hours for dementia as of 08/03/2020.
Mirtazapine 7.5 mg in the morning for depression as of 02/01/2023.
UA with C and S (urine analysis with Culture and Sensitivity) on 09/06/2023.
Cipro 500 mg every 12 hours for UTI (Urinary Tract Infection) for 7 days as of 09/10/2023.
Review of the September 2023 Behaviors Record showed the following:
Actively Exit Seeking Record Intervention Code (s): 1. N/A, 2. Engage in conversation, 3. Redirect to alternative location in facility, 4. Call family/friend 5. Activity, 6. Give snacks/food, 7. Give fluids, 8. Toileting (every shift) as of 07/22/2022. On 09/02/23 N/A for day shift was documented.
Actively Exit Seeking Record Outcome Code: 1. N/A, w. Improved, 3. Worsening, 4. Unchanged, if worsening / unchanged, notify supervisor (every shift) as of 07/22/2022 on 09/02/23 N/A for day shift.
Behavior Monitoring -Active Exit Seeking Record the Number of Occurrences every shift, (0 if did not occur) as of 07/22/2022. On 09/02/2023 0 was documented.
Review of the September 2023 Treatment Administration Record (TAR) showed the following:
Wandering device - check function every night shift for wandering device use as of 07/22/2022. On 09/01/2023 it was documented as checked by nursing.
Wandering device - Check placement to LLE (Left lower extremity) every shift for wandering device use as of 07/22/2022. On 09/02/2023 it was documented as checked on the day shift.
Review of the care plans showed as of 08/18/2022 Resident #10 was at risk for elopement / exit seeking activity, exit seeking, aimless wandering due to cognition, has the potential to approach exit doors.
A goal initiated on 08/18/2022 showed the resident will not leave facility unattended through the review date of 10/15/2023.
The interventions included but were not limited to the following:
On 08/18/2022, checking for proper functioning of the audible alarm system daily and prn (as needed).
On 08/18/2022, check functioning of wandering device every night.
Revised on 05/25/2023, check placement of wandering device every shift - LLE.
On 08/18/2022, Discuss with resident / family the risk of elopement and wandering.
On 07/27/2023, Encourage resident to participate in activities and redirect resident when exit seeking.
Revised on 5/25/2023, Every 1-hour safety checks monitor resident due to identified elopement risk.
On 08/18/2022, Indicate risk in Care Profile and [NAME], Place demographics in Risk Binders.
On 08/18/2022, Monitor resident for tailgating when visitors are in the building.
On 08/18/2022, Monitor resident for active exit seeking behavior each shift.
On 08/18/2022, Use audible monitoring system to alert staff of exit seeking behaviors.
On 08/18/2022, Use diversional activities when exit-seeking behavior is occurring (i.e., offer food, activities, one-on-one company).
Review of Resident #10's Elopement Risk Evaluation, dated 07/02/2023 showed the following:
1. Is resident ambulatory and / or able to self-propel wheelchair? Yes.
2. Presence of any of the following risk factors indicates the resident is a risk for elopement.
2b. Resident displays behaviors indicting desire to leave the facility, i.e., packing belongings, tailgating, searching for exits from facility or searching for someone/something from past life events, verbalizing desire to go home/elsewhere.
2d. Resident's family/responsible party expressed concerns resident may attempt to leave.
3. Resident is 1. At risk for elopement.
Review of Resident #10's Elopement Risk Evaluation. dated 09/02/2023 showed the following:
1. Is resident ambulatory and / or able to self-propel wheelchair? Yes.
2. Presence of any of the following risk factors indicates the resident is a risk for elopement.
2b. Resident displays behaviors indicting desire to leave the facility, i.e., packing belongings, tailgating, searching for exits from facility or searching for someone/something from past life events, verbalizing desire to go home/elsewhere.
3. Resident is 1. At risk for elopement.
An observation and interview was conducted on 10/02/2023 at 10:15 a.m. The resident was awake lying-in bed. Her wandering device was observed on her RUE (Right Upper Extremity). The head of the bed was elevated. She stated, I went on a walk last week, to the mall, went by myself because no one could take me. I went up a hill.
During an interview and observation on 10/02/2023 at 1:15 p.m. Staff B, LPN (Licensed Practical Nurse) was asked to locate Resident #10's wandering device. Staff B was unable to find the wandering device on Resident #10's LLE. She stated, It is supposed to be there (lifting up the resident's pants legs). Staff B went into the bathroom to look at the resident's wheelchair and it was not present. Staff B was observed locating the wandering device on her RUE. She stated, It's on her RUE. Staff B, LPN attempted to remove the wandering device, and stated it could not be taken off even with effort.
Observation on 10/04/2023 at 10:35 a.m., the resident was dressed and groomed for the day and in her wheelchair. She was located in the dining room looking out the dining room door. She was alone. She demonstrated she was able to move herself in her wheelchair with her feet. The wandering device was observed on her RUE.
During an interview on 10/03/2023 at 8:57 a.m. the DON was asked for a timeline.
A timeline was provided on 10/03/2023 at 11:20 a.m. revealing the following:
09/02/23, approximately 12:40 p.m. resident observed exiting dining room after lunch.
09/02/23, approximately 12:45 p.m. nurse reports seeing resident wheel herself down hall.
09/02/23, approximately 1:37 p.m., resident returned to facility by neighbor, Staff F, receptionist was alerted by sounding of the alarm.
09/02/23, approximately 1:38 p.m., resident assessed by social services, floor nurse with no injuries.
09/02/23, approximately 2:35 p.m., DON arrived at the facility to assess the event. And complete head to toe assessment on Resident #10. The resident was placed on 1:1 supervision.
On 10/02/23 at 2:55 p.m. Resident #10's elopement route was observed with the DON and the Regional Nursing Home Administrator (RNHA). This included walking down a steeply sloped driveway and crossing a 2-lane street with a speed limit of 30 miles per hour. There was an occasional car observed going down the street. Resident #10 entered the grounds of an apartment complex. She was found by a gentleman at the back of the apartment complex parking lot. He informed them where he found her in the parking lot. He told the DON and the NHA the resident had told him she wanted to get to the playground, which is part of the apartment complex where she was found. He told them she was calm and was just sitting in her wheelchair. (Photographic evidence obtained).
During an interview with the DON on 10/03/2023 at 8:57 a.m. the DON verified the Psych note on 09/05/2023 showed She elopes and has outdoor privileges. Patient is now on 1:1 observation for safety measures and does not remember. DON stated, she does not have outdoor privileges. The DON stated she would ask medical records if there were any other notes that had not been uploaded The DON stated, We had an IDT (Interdisciplinary Team) meeting and reviewed the care plan and made sure everything was there. We have an IDT meeting every morning and review all incidents that happen. She stated they reviewed the care plans. They reassessed her elopement risk, performed labs, did a UA and C/S on 09/06/2023. On 09/05/23 they changed the Depakote order. The resident did have a UTI and was treated with antibiotics. She stated the care plan was updated with 1:1 supervision on 09/02/23.
During an interview on 10/04/2023 at 10:51 a.m. the DON, the RNHA and the Nurse Consultant stated they did ask the staff why the wandering device was placed on the upper right extremity when the physician order was for the left lower extremity. The DON reported she changed out the wandering device on the resident after she eloped and put it on the resident's right ankle. When we commented that it was on the resident's right arm, the DON said yes the NHA had asked that they change the site. The NHA explained to the DON that it would be at a better level to signal the door alarm if it was on her arm, not her leg. The DON stated she did not know if the wandering device would not set off the alarm if it was on her LLE.
During an interview on 10/05/2023 at 9:15 a.m. with Staff O RN, MDS Coordinator and Staff P, RN, MDS Coordinator stated they do not do the section E (behaviors), it was done by the SSD. Staff O reviewed the Resident Assessment Instrument (RAI) manual regarding wandering, and it showed if a resident was wandering from one area to another it was considered wandering. It was not necessarily attached to exit seeking. She stated they are supposed to talk to the staff regarding behaviors.
During an interview on 10/05/2023 at 9:17 a.m. SSD stated she determines if a resident was a wanderer or not. She stated she gets the information from the nurses and on site. She did not feel Resident #10 was a wanderer because she was not exit seeking. She reviewed the RAI manual. She stated she does not remember from July 2023 if Resident #10 wandered or not.
Record review of the facility's policy titled, Comprehensive Care Plans, revised 09/18/2023 showed the following: Policy: it is the policy of this facility to develop and implement a comprehensive person-centered care plan for each resident, consistent with resident rights, that includes measurable objectives and timeframes to meet a resident's medical, nursing, and mental and psychosocial needs that are identified in the resident's comprehensive assessment. 3. The comprehensive care plan will describe, at a minimum, the following: a. the services that are to be furnished to attain or maintain the resident's highest practicable physical, mental, and psychosocial well-being. F. resident specific interventions that reflect the resident's needs and preferences and align with the resident's cultural identity, as indicated. 6. The comprehensive care plan will include measurable objectives and timeframes to meet the resident's needs as identified in the resident's comprehensive assessment. The objectives will be utilized to monitor the resident's progress. Alternative interventions will be documented, as needed.
Review of the facility's policy titled, Elopements and Wandering Residents, revised 07/12/2012 showed the following:
Policy: this facility ensures that residents who exhibit wandering behavior and / or are at risk for elopement receive adequate supervision to prevent accidents and receive care in accordance with their person-centered plan of care addressing the unique factors contributing to wandering or elopement risk.
4. Monitoring and Managing Residents for Elopement or Unsafe Wandering:
a. Residents will be assessed for risk for elopement and unsafe wandering upon admission and throughout their stay by the interdisciplinary care plan team.
B. the interdisciplinary team will evaluate the unique factors contributing to risk in order to develop a person-centered care plan.
C. interventions to increase staff awareness of the resident's risk, modify the resident's behavior, or to minimize risks associated with hazards will be added to the resident's care plan and communicated to appropriate staff.
D. adequate supervision will be provided to help prevent accidents or elopements.
E. charge nurses and unit managers will monitor the implementation of interventions, response to interventions, and document accordingly.
F. the effectiveness of interventions will be evaluated, and changes will be made as needed. Any changes or new interventions will be communicated to relevant staff.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based interviews and record review, the facility failed to ensure one resident (# 11) received an antibiotic ordered for a urina...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based interviews and record review, the facility failed to ensure one resident (# 11) received an antibiotic ordered for a urinary tract infection out of 17 residents sampled during the survey.
Findings included:
Resident #11 was admitted to the facility on [DATE] with diagnoses that included metabolic encephalopathy, chronic kidney disease and dementia.
A review of the nurses' progress notes revealed the resident was exhibiting aggressive behaviors toward the staff.
On 09/08/23 at 4:05 p.m., the nurse documented, Resident has refused all medications since overnight shift, attempted multiple times to encourage with no success.
On 09/13/23 at 11:55 a.m. the nurse documented, Resident having behavior issues. resident noncompliant with care plan. attempting to walk with no assistance. biting and refusing care from staff. Doctor notified. On 09/13/23 the nurse documented, Resident attempting to ambulate without assist. Aide attempted to assist resident. Resident bit into aide's arm. Resident continued to throw items that she is able to obtain - e.g. towels, wash cloths, crumpled up paper, book. Resident heard yelling 'give em hell' repeatedly. Resident also began to call aide names while providing care. Resident observed ambulating without assistance and as aide attempted to assist the resident, she grabbed the aide's neck and scratched his neck. Doctor and Nurse Practitioner (NP) notified of behavior and new orders obtained.
The new orders included the following:
Obtain urine for a urinalysis on 09/16/2023.
A review of the lab results, dated 09/19/2023, revealed the urinalysis showed TNTC (too numerous to count) WBC (white blood cells) with the organism >100,000 CFU/ML Klebsiella Pneumoniae (ESBL).
An order was written to administer Ertapenem Sodium injection 1 gm intramuscularly in the evening every 5 days for ESBL until 09/23/2023, with the start date of 09/19/2023.
A review of the Medication Administration Record (MAR), dated September 2023 revealed the following:
09/19/23 at 1700 (5:00 p.m.). The entry was marked with the nurses initials and the number '2'. The chart code on the MAR revealed that the '2' meant the drug had been refused. There were no other entries on the MAR for the medication and for the rest of the month.
A review of the physician's orders and the nurses notes did not reveal the order had been discontinued or changed and the nurse's notes did not include the physician or NP had been notified that the medication was not being administered.
On 10/05/23 at 9:00 a.m. the DON reported the facility's Infection Log did not include Resident #11 as having a urinary tract infection and order for the antibiotic. She reported she had informed the NP the resident had not received the medication. The DON reported the NP was told the resident seemed to be back to her baseline and the NP told her to hold off on giving the antibiotic or trying to obtain another sample of urine to test. The DON reported at the time nurses should have documented the resident refused the first dose of the medication and they should have continued to try to give the resident the injection. The DON reported the resident was refusing all of her medications that day which was probably why the nurse didn't attempt to give the injection.
A review of the MAR for 09/20/2023 revealed the resident was accepting some of her medications: the resident took her medications as ordered through out the day including: Magnesium, Melatonin, Multi-vitamin, Depakote, Potassium, Statin, and Lorazepam.
On 10/05/2023, an interview was conducted with the NP at 12:40 p.m. She reported she was familiar with the resident and was aware the urine sample had been obtained and sent in for analysis with the results identifying an organism and the antibiotic indicated for the organism was ordered. She reported she was told the order wasn't clear and confirmed no one reached out to clarify the order. She reported she was aware the resident refused the injection the first day and the nurses didn't seem to have tried again. She reported because the resident didn't seem to be exhibiting symptoms she would not order a new analysis or order the injection at this time.
On 10/05/2023 at 1:45 p.m. the NP reported she had assessed the resident and found she wasn't at her baseline and she had changed since she saw her last week. She reported she had ordered another urinalysis and would wait for the results to determine the medication to order.
The NP note, dated 10/05/2023, revealed the following: Today when I was rounding, staff informed me she is not eating or drinking and in bed. The note included, Patient has altered mental status. The NP completed a physical assessment of the resident and documented, Patient awake with verbal stimuli, refuses to eat or drink for me, when I try to assess she tries to punch me with both hands made into fists but soft, unable to connect, stops after exam. The Plan included a complete blood count, complete metabolic profile, urinalysis, and culture and sensitivity. Failure to thrive meets McGreer requirements for UA and C&S . Will treat if positive - last UA results from 09/19, over 16 days old, need to recollect to check C&S to see which antibiotic is sensitive.
The UA C&S results, returned on 10/10/2023, showed >100,000 CFU/ML Klebsiella Pneumoniae, ESBL, which was the same organism reported on 09/19/2023.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review the facility failed to ensure the medical records included completed docume...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review the facility failed to ensure the medical records included completed documentation for one resident (#10) out of 16 residents sampled.
Findings included:
Resident #10 was admitted on [DATE] and readmitted on [DATE]. Record review showed diagnoses included but were not limited to neurocognitive disorder with Lewy bodies; brief psychotic disorder; adjustment disorder with anxiety; generalized anxiety disorder; unspecified lack of coordination; Diabetes; muscle weakness (generalized); other abnormalities of gait and mobility; difficulty in walking, not elsewhere classified; major depressive disorder, recurrent moderate; and essential hypertension. Record review of the annual, Minimum Data Set (MDS), dated [DATE], showed in Section C: Cognitive Function, a Brief Interview Mental Status (BIMS) score of 04, indicating severe cognitive impairment; Section G: Functional Status the resident required extensive assistance of two for bed mobility, extensive assistance of one for toileting, limited assistance of two for transfers, and she was independent on and off the unit. Section E: Behaviors showed wandering behavior was not exhibited.
Review of physician orders summary for September 2023 showed the following:
Actively Exit Seeking Record Intervention Code (s): 1. N/A, 2. Engage in conversation, 3. Redirect to alternative location in facility, 4. Call family/friend 5. Activity, 6. Give snacks/food, 7. Give fluids, 8. Toileting (every shift) as of 07/22/2022.
Actively Exit Seeking Record Outcome Code: 1. N/A, 2. Improved, 3. Worsening, 4. Unchanged, if worsening / unchanged, notify supervisor (every shift) as of 07/22/2022.
Behavior Monitoring -Active Exit Seeking Record the Number of Occurrences every shift, (0 if did not occur) as of 07/22/2022. Psychiatric Consult for Evaluation and follow as needed as of 01/09/2023.
Wanderguard (Wandering device) - check function every night shift for wandering device use as of 07/22/2022.
Wandering device - Check placement to LLE (Left lower extremity) every shift for wandering device use as of 07/22/2022.
Wandering device to LLE due to: Elopement Risk as of 03/10/2023 and expires 10/08/2023.
Depakote Oral Tablet Delayed Release 125 mg (milligram) every 12 hours for anxiety as of 07/30/2023 and was increased to 250 mg every 12 hours for mood disorder as of 09/05/2023.
Memantine HCL 10 mg every 12 hours for dementia as of 08/03/2020.
Mirtazapine 7.5 mg in the morning for depression as of 02/01/2023.
UA with C and S (urine analysis with Culture and Sensitivity) on 09/06/2023.
Cipro 500 mg every 12 hours for UTI (Urinary Tract Infection) for 7 days as of 09/10/2023.
Review of the September 2023 Behaviors Record showed the following:
Actively Exit Seeking Record Intervention Code (s): 1. N/A, 2. Engage in conversation, 3. Redirect to alternative location in facility, 4. Call family/friend 5. Activity, 6. Give snacks/food, 7. Give fluids, 8. Toileting (every shift) as of 07/22/2022 on 09/02/23 N/A for day shift.
Actively Exit Seeking Record Outcome Code: 1. N/A, w. Improved, 3. Worsening, 4. Unchanged, if worsening / unchanged, notify supervisor (every shift) as of 07/22/2022 on 09/02/23 N/A for day shift. Behavior Monitoring -Active Exit Seeking Record the Number of Occurrences every shift, (0 if did not occur) as of 07/22/2022 on 09/02/2023 0.
Review of the September 2023 Treatment Administration Record (TAR) showed the following: Wandering device - check function every night shift for wandering device use as of 07/22/2022 on 09/01/2023 showed it had been checked.
Wandering device - Check placement to LLE (Left lower extremity) every shift for wandering device use as of 07/22/2022 showed it had been checked 09/02/2023 on day shift.
Review of the care plans showed as of 08/18/2022 the Resident #10 was at risk for elopement / exit seeking activity, exit seeking, aimless wandering due to cognition, has the potential to approach exit doors.
Goal initiated on 08/18/2022 showed the resident will not leave facility unattended through the review date of 10/15/2023.
Interventions included but not limited to the following:
On 08/18/2022, checking for proper functioning of the audible alarm system daily and prn (as needed
On 08/18/2022, check functioning of wandering device every night.
Revised on 05/25/2023, check placement of wandering device every shift - LLE.
On 08/18/2022, Discuss with resident / family the risk of elopement and wandering.
On 07/27/2023, Encourage resident to participate in activities and redirect resident when exit seeking.
Revised on 5/25/2023, Every 1-hour safety checks monitor resident due to identified elopement risk.
On 08/18/2022, Indicate risk in Care Profile and [NAME], Place demographics in Risk Binders.
On 08/18/2022, Monitor resident for tailgating when visitors are in the building.
On 08/18/2022, Monitor resident for active exit seeking behavior each shift.
On 08/18/2022, Use audible monitoring system to alert staff of exit seeking behaviors.
On 08/18/2022, Use diversional activities when exit-seeking behavior is occurring (i.e., offer food, activities, one-on-one company).
An observation on 10/02/2023 at 9:40 a.m., revealed Resident #10 lying in bed asleep with the side rails up. She was dressed and groomed for the day. The wheelchair was at the bedside. The overbed table was at the bedside.
An observation and interview was conducted on 10/02/2023 at 10:15 a.m. The resident was awake lying-in bed. Her wandering device was observed on her RUE (Right Upper Extremity). The head of the bed was elevated. She stated, I went on a walk last week, to the mall, went by myself because no one could take me. I went up a hill.
During an interview and observation on 10/02/2023 at 1:15 p.m. Staff B, LPN (Licensed Practical Nurse) was asked to locate Resident #10's wandering device. Staff B was unable to find the wandering device on Resident #10's LLE. She stated, It is supposed to be there (lifting up the resident's pants legs). Staff B went into the bathroom to look at the resident's wheelchair and it was not present. Staff B was observed locating the wandering device on her RUE. She stated, It's on her RUE. Staff B, LPN attempted to remove the wandering device, and stated it could not be taken off even with effort.
Observation on 10/04/2023 at 10:35 a.m., the resident was dressed and groomed for the day and in her wheelchair. She was located in the dining room looking out the dining room door. She was alone. She demonstrated she was able to move herself in her wheelchair with her feet. The wandering device was observed on her RUE.
Review of Safety-1:1 Supervision of Front Door, dated 09/02/2023 began at 2:00 p.m. and was performed on 09/04/2023 and 09/05/2023. The documentation for 09/03/2023 was not provided. The documentation was performed by facility staff.
Review of the Safety Check Log - 30 minutes were performed on 09/112023, 09/12/2923, 09/13/2023, 09/14/2023 was missing, 09/15/2023, 09/16/2023, 09/17/2023, and 09/18/2023 was documented by the CNA staff.
During interview with the Director of Nursing (DON) on 10/03/2023 at 8:57 a.m. she stated the documentation of the event (elopement) was part of the resident's risk notes. Those notes are not found in the resident's electronic medical records. The DON verified there was no documentation in the electronic medical record of the incident. She verified there was only a post evaluation which does not state she eloped. There was no documentation that the attending physician and / or responsible party had been notified. It was documented in the risk report. A Post Incident was in the chart. The DON stated, We had an IDT (Interdisciplinary Team) meeting and reviewed the care plan and made sure everything was there. We have an IDT meeting every morning and review all incidents that happen. The note for the IDT meeting was documented in the risk notes by the DON. They did not document the IDT meeting in the electronic medical chart. She stated they reviewed the care plans. She stated the care plan was updated with 1:1 supervision on 09/02/23.
During an interview on 10/05/2023 at 9:15 a.m. with Staff O RN, MDS Coordinator and Staff P, RN, MDS Coordinator stated they do not do the section E (behaviors), it was done by the SSD. Staff O reviewed the Resident Assessment Instrument (RAI) manual regarding wandering, and it showed if a resident was wandering from one area to another it was considered wandering. It was not necessarily attached to exit seeking. They are supposed to talk to the staff regarding behaviors.
During an interview on 10/05/2023 at 9:17 a.m. SSD stated she determines if a resident was a wanderer or not. She stated she gets the information from the nurses and on site. She did not feel Resident #10 was a wanderer because she was not exit- seeking. She reviewed the RAI manual. She stated she does not remember from July 2023 if Resident #10 wandered or not.
Review of the facility's policy, Elopements and Wandering Residents, revised 07/12/2012 showed Policy: this facility ensures that residents who exhibit wandering behavior and / or are at risk for elopement receive adequate supervision to prevent accidents and receive care in accordance with their person-centered plan of care addressing the unique factors contributing to wandering or elopement risk.
Definitions: Wandering is random or repetitive locomotion that may be goal directed or non-goal directed or aimless. Elopement occurs when a resident leaves the premises or a safe area without authorization and / or any necessary supervision to do so.
6. Procedure Post-Elopement
a. a nurse will perform a physical assessment, document, and report findings to physician.
B. any new physician orders will be implemented and communicated to the family/authorized representative.
C. a social service designee will re-assess the resident and make any referrals for counseling or psychological/psychiatric consults.
E. staff may be educated on the reasons for elopement and possible strategies for avoiding such behavior.
G. documentation in the medical record will include findings from nursing and social service assessments, physician/family notification, care plan discussions, and consultant notes as applicable. I
Review of the facility's policy, Incidents and Accidents, revised on 08/2023 showed Policy: it is the policy of this facility for staff to utilize ______________________(left blank by the facility) to report, investigate, and review any accidents or incidents that occur or allegedly occur, on facility property and may involve or allegedly involve a resident.
Compliance Guidelines:
13. Documentation should include the date, time, nature of the incident, location, initial findings, immediate interventions, notifications, and orders obtained or follow-up interventions.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review it was determined the facility failed to provide Quality Assessment and Ass...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review it was determined the facility failed to provide Quality Assessment and Assurance (QAA) practices that demonstrated identification, monitoring, and implementation of an effective Action Plan regarding assessing and ensuring two residents (#10 and #12) out of 11 sampled residents with wandering and exit-seeking behaviors was provided supervision and services to prevent elopement.
Findings included:
Review of the facility's policy entitled, QAPI Change Process, revised on 07/12/2023, showed the following:
Policy: the facility has established and utilizes a systematic approach to performance improvement activities to ensure changes are effective and improvements are sustained.
Policy Explanation and Compliance Guidelines:
1. The facility has in operation a Quality Assessment and Assurance (QAA) Committee that is responsible for coordinating and evaluating activities under the facility's QAPI program.
2. The QAA Committee utilizes a systematic approach to performance improvement, including analysis of data, corrective action, and performance tracking.
3. Data Analysis-
a. The facility draws data from multiple sources, including input from all staff, residents, families, and others as appropriate. This data is reported to the QAA Committee.
b. The QAA committee analyzes the data in order to identify or better understand a problem.
c. Once a potential problem is identified, the committee utilizes a systematic approach to help identify the root cause of the problem.
d. As corrective actions are taken, the committee continues to collect and analyze data to determine the effectiveness of any changes.
4. Corrective Action-
a. Once the root cause of a problem is identified, the QAA committee oversees the development of an appropriate corrective action. An appropriate corrective action is one that addresses the underlying cause of the issue comprehensively, at a systems level.
b. Corrective action plans include:
i. a definition of the problem / which includes determining contributing causes of the problem;
ii. Measurable goals;
iii. Step-by-step interventions to correct the problem and achieve established goals; and
iv. A description of how the QAA committee will monitor to ensure changes yield the expected results.
c. Example corrective actions may include but are not limited to:
i. introducing new equipment or products that specifically address the identified problem.
Iv. Providing education and verifying competency following the education.
Vi. Observing staff members and providing feedback on their performance of new practices.
Vii. Convening a Performance Improvement Project (PIP) to improve a systematic problem or improve quality in absence of a problem.
d. the QAA committee uses the Plan, DO, Study, Act (PDSA) cycle of improvement for testing any changes within a PIP.
I Plan: developing a plan related to the change that will be tested.
Ii. Do: carrying out the plan. Iii. Study: observing and analyzing data collected, learning from any consequences.
Iv. Act: making a decision regarding the change, such as to adopt, modify, or abandon the change and start over.
e. Multiple PDSA cycles may be implemented until the desired performance goals have been met.
During an interview on 10/03/2023 at 8:57 a.m. the Regional Nursing Home Administration (RNHA) and the DON stated they had performed a Quality Assurance and Performance Improvement (QAPI) / PIP (Performance Improvement Plan). They were unable to find any documentation regarding the QAPI / PIP. The DON stated she would check in the Nursing Home Administrator (NHA) office for it. She stated she knew they had an Ad hoc (means for this).
During an interview on 10/03/2023 at 11:00 a.m. the DON and the RNHA provided minutes for a QAPI meeting dated 09/21/2023. The sign-in sheet showed the Medical Director attended the meeting. The minutes showed, Sentinel Event wandering event from 09/02/23 involving resident (#10). The RNHA and the DON stated they had a QAPI call on 09/05/2023 because the RNHA was on the phone for it. They stated they were unable at this time to find paperwork related to QAPI / PIP.
Review of the QAPI Meeting Signature Sheet, dated 09/21/2023, showed 11 members present, one being the Medical Director. The sign-in sheet did not show that either the Nursing Home Administrator (NHA) or the Director of Nursing (DON) attended. Only reference to Elopement was, the minutes showed, Sentinel Events wandering event from 09/02/23 involving resident (#10).
During a phone interview on 10/05/2023 at 1:20 p.m. the Medical Director, who was also Resident #10's attending physician stated the Advanced Practice Registered Nurse (APRN) was following her. The resident was restless, and they did some medication changes. He stated he did not remember anything about a QAPI meeting. He stated he attends all of them and signs the sign-in sheet. He stated he did not participate in a Plan for elopement that he could think of.
During a phone interview on 10/06/2023 at 9:21 a.m. a customer service representative from the [contracted technology company] stated, On 09/05/2023, they had issues with the [wandering alarm system] reception. It was not picking up the transmissions all the time. On 08/02/2023 we initially talked to them about the issue. We did some trouble shooting steps over the phone but was unable to solve the issue. We sent them a service agreement form (Authorization Form) for signature. We did not get the form back. We have to have a signature on an Authorization Form before we send anyone out. On 09/02/2023, the Maintenance Director called back about the same issue. Again, one of the techs tried to troubleshoot over the phone but was unable to. We resent the form that day, 09/02/2023, and received it back the same day. We dispatched it for 09/05/2023. On 09/05/2023 the tech arrived, he checked the main entrance, and adjusted the antennas. He adjusted the wire termination for a timer and bypass button. After the test it was working fine. He tested all the other doors. The termination wires on the keypads adjust the schedule of opening and closing of the door. He checked the wiring only it did not have to be replaced or repaired.
Resident #10 was admitted on [DATE] and readmitted on [DATE]. Record review of the annual, Minimum Data Set (MDS), dated [DATE], showed in Section C: Cognitive Function, a Brief Interview Mental Status (BIMS) score of 04, indicating severe cognitive impairment; Section G: Functional Status showed the resident required extensive assistance of two for bed mobility, extensive assistance of one for toileting, limited assistance of two for transfers, and she was independent on and off the unit. Section E: Behaviors showed wandering behavior were not exhibited.
Review of the Physician Orders Summary for September 2023 showed the following:
Actively Exit Seeking Record Intervention Code (s): 1. N/A, 2. Engage in conversation, 3. Redirect to alternative location in facility, 4. Call family/friend 5. Activity, 6. Give snacks/food, 7. Give fluids, 8. Toileting (every shift) as of 07/22/2022.
Actively Exit Seeking Record Outcome Code: 1. N/A, 2. Improved, 3. Worsening, 4. Unchanged, if worsening / unchanged, notify supervisor (every shift) as of 07/22/2022.
Behavior Monitoring -Active Exit Seeking Record the Number of Occurrences every shift, (0 if did not occur) as of 07/22/2022. Psychiatric Consult for Evaluation and follow as needed as of 01/09/2023.
Wanderguard (wandering device)- check function every night shift for wandering device use as of 07/22/2022.
Wandering device - Check placement to LLE (Left lower extremity) every shift for wandering device use as of 07/22/2022.
Wandering device to LLE due to: Elopement Risk as of 03/10/2023 and expires 10/08/2023.
Depakote Oral Tablet Delayed Release 125 mg (milligram) every 12 hours for anxiety as of 07/30/2023 and was increased to 250 mg every 12 hours for mood disorder as of 09/05/2023.
Memantine HCL 10 mg every 12 hours for dementia as of 08/03/2020.
Mirtazapine 7.5 mg in the morning for depression as of 02/01/2023.
UA with C and S (urine analysis with Culture and Sensitivity) on 09/06/2023.
Cipro 500 mg every 12 hours for UTI (Urinary Tract Infection) for 7 days as of 09/10/2023.
Review of the September 2023 Behaviors Record showed the following:
Actively Exit Seeking Record Intervention Code (s): 1. N/A, 2. Engage in conversation, 3. Redirect to alternative location in facility, 4. Call family/friend 5. Activity, 6. Give snacks/food, 7. Give fluids, 8. Toileting (every shift) as of 07/22/2022. On 09/02/23 N/A for day shift was documented.
Actively Exit Seeking Record Outcome Code: 1. N/A, w. Improved, 3. Worsening, 4. Unchanged, if worsening / unchanged, notify supervisor (every shift) as of 07/22/2022 on 09/02/23 N/A for day shift.
Behavior Monitoring -Active Exit Seeking Record the Number of Occurrences every shift, (0 if did not occur) as of 07/22/2022. On 09/02/2023 0 was documented.
Review of the September 2023 Treatment Administration Record (TAR) showed the following:
Wandering device - check function every night shift for wandering device use as of 07/22/2022. On 09/01/2023 it was documented as checked by nursing.
Wandering device - Check placement to LLE (Left lower extremity) every shift for wandering device use as of 07/22/2022. On 09/02/2023 it was documented as checked on the day shift.
Review of Resident #10's progress notes showed no documentation regarding an elopement on 09/02/2023.
Review of the nursing progress notes dated 09/05/2023 at 2:48 p.m. showed the following:
Psychiatric Nurse Practitioner on site for visit with resident. New orders were given to increase her Depakote from 125 mg PO [by mouth] BID [twice a day] to 250 mg PO BID. Entered into PCC [Point Click Care or electronic medical record].
Review of Resident #10's Elopement Risk Evaluation, dated 07/02/2023 showed the following:
1. Is resident ambulatory and / or able to self-propel wheelchair? Yes.
2. Presence of any of the following risk factors indicates the resident is a risk for elopement.
2b. Resident displays behaviors indicting desire to leave the facility, i.e., packing belongings, tailgating, searching for exits from facility or searching for someone/something from past life events, verbalizing desire to go home/elsewhere.
2d. Resident's family/responsible party expressed concerns resident may attempt to leave.
3. Resident is 1. At risk for elopement.
Review of Resident #10's Elopement Risk Evaluation. dated 09/02/2023 showed the following:
1. Is resident ambulatory and / or able to self-propel wheelchair? Yes.
2. Presence of any of the following risk factors indicates the resident is a risk for elopement.
2b. Resident displays behaviors indicting desire to leave the facility, i.e., packing belongings, tailgating, searching for exits from facility or searching for someone/something from past life events, verbalizing desire to go home/elsewhere.
3. Resident is 1. At risk for elopement.
During an interview on 10/05/2023 at 12:30 p.m. with the Advanced Practice Registered Nurse (APRN) she stated Resident #10 had a little bit of confusion, and thought she was going home, and she went out to the park. That was not her normal. She did a urinalysis (UA) and culture and sensitivity (C/S) and placed her on antibiotics. She was back to normal. Her Depakote was increased on 09/05/2023. Her urinalysis was on 09/06/2023 and results on 09/09/2023. Cipro was started on 09/10/2023 for 10 days. The facility told her when she came into the facility the resident had eloped, they did not call her. They called the psychiatric nurse because it was exit-seeking.
Review of the care plans showed as of 08/18/2022 Resident #10 was at risk for elopement / exit seeking activity, exit seeking, aimless wandering due to cognition, has the potential to approach exit doors.
A goal initiated on 08/18/2022 showed the resident will not leave facility unattended through the review date of 10/15/2023.
The interventions included but were not limited to the following:
On 08/18/2022, checking for proper functioning of the audible alarm system daily and prn (as needed).
On 08/18/2022, check functioning of wandering device every night.
Revised on 05/25/2023, check placement of wandering device every shift - LLE.
On 08/18/2022, Discuss with resident / family the risk of elopement and wandering.
On 07/27/2023, Encourage resident to participate in activities and redirect resident when exit seeking.
Revised on 5/25/2023, Every 1-hour safety checks monitor resident due to identified elopement risk.
On 08/18/2022, Indicate risk in Care Profile and Kardex, Place demographics in Risk Binders.
On 08/18/2022, Monitor resident for tailgating when visitors are in the building.
On 08/18/2022, Monitor resident for active exit seeking behavior each shift.
On 08/18/2022, Use audible monitoring system to alert staff of exit seeking behaviors.
On 08/18/2022, Use diversional activities when exit-seeking behavior is occurring (i.e., offer food, activities, one-on-one company).
An observation and interview were conducted on 10/02/2023 at 10:15 a.m., Resident #10 was lying in bed, awake. Her wandering device was observed on her RUE (Right Upper Extremity). The head of the bed was elevated. She stated, I went on a walk last week, to the mall, went by myself because no one could take me. I went up a hill.
During an interview and observation on 10/02/2023 at 1:15 p.m. Staff B, LPN (Licensed Practical Nurse) was asked to locate Resident #10's wandering device. Staff B was unable to find the wandering device on Resident #10's LLE. She stated, It is supposed to be there (lifting up the resident's pants legs). Staff B went into the bathroom to look at the resident's wheelchair and it was not present. Staff B was observed locating the wandering device on her RUE. She stated, It's on her RUE. Staff B, LPN attempted to remove the wandering device, and stated it could not be taken off even with effort.
An observation was conducted on 10/04/2023 at 10:35 a.m. Resident #10 was dressed and groomed for the day and seated in her wheelchair. She was located in the dining room looking out the dining room door. She was alone. She demonstrated she was able to move herself in her wheelchair with her feet. The wandering device was observed on her RUE.
Review of the [contracted technology company] On-Site Service Charge Authorization Form dated 08/02/2023 showed, Customer Described Problem: Maintenance Director called in requesting a Service Call to have a tech work on the Main Entrance's ANT (antenna) range as some residents have been able to escape without setting off the alarm. On the lower half of the form, it showed, My signature on this agreement certifies that I am an authorized agent for the facility listed above. It was signed as authorized by the NHA on 09/01/2023.
Review of the [contracted electric company] Invoice dated 08/23/23 showed:
The following charges are for electrical work performed as listed:
Inspected the lobby door.
Opened the panel and tested power.
Found the panel power was testing for 17 volts AC (alternating current) and 0 volts DC (direct current).
Replaced the power supply for 12 volt, applied power to panel.
Tested receivers and found the receiver on antenna 4 was not functioning.
Replaced the receiver from maintenance stock and placed antenna for circuits on antenna 1 terminal.
Ranged all three receivers.
Receivers picked up transmitter and door annunciates while the transmitter is in range and door is ajar.
Found three outdated transmitters before testing with a in date transmitter.
Administration was not in the building.
Maintenance came in for a brief period of time to check how wandering device range test was going then departed.
Labor one tech 4.5 hours weekend labor
Review of the Service Call Job Form, dated 09/05/23, [contracted technology company] showed under description Maintenance Director called in requesting a Service Call to have a tech work on the Main Entrance's antennae range as some residents have been able to escape without setting off the alarm. Documentation showed On site met Maintenance Director and NHA. Checked and tested the main entry 9450 T70 with 3 duo link antennae. Adjusted the door antenna and adjusted wiring terminations for timer and bypass button / IEIKeypad. System working as designed. While on site, checked and tested all remaining Code Alert door systems for working order. System ok.
Review of the electronic maintenance system dated 08/28/2023 through 09/01/2023 showed the following: Residents Monitoring Systems: Check operation of door monitors and patient wandering system performed by Maintenance Director revealed all doors including the Main Entrance Pass. On 09/02/2023 a handwritten form showed all doors including the Main Entrance Pass and was completed by the Maintenance Director. Documentation at the bottom of the 09/02/2023 form showed, Spoke with [contracted technology company] tech about adjusting T10 (antenna). We got it dialed in good. Therapy patio longer than usual on door alarm.
During an interview on 10/02/2023 at 1:00 p.m. the Maintenance Director was observed checking the following exit doors: Therapy Hall, [NAME] Hall, Magnolia Hall, Smoking Area, Delta Hall, and Park Hall, Laundry door and Dining Room. All alarmed doors were in working order. He stated the alarmed doors had a 15-second delay alarm. He stated he checks the door alarms daily. He stated the front door was unlocked from about 7 a.m. to 5 p.m. but it won't open if a resident has a wandering device on. When asked what happened on 09/02/2023, he stated I do not know.
During an observation on 10/02/2023 at 1:40 p.m. the dining room door screeching alarm went off twice. On investigation, the activity assistant was taking residents out for air and guitar playing. No other staff members responded to the alarms. The activity assistant set it off again and again and no one responded, this included the kitchen staff.
During an observation on 10/02/23 at 1:50 p.m. the Maintenance Director tested a wandering device at the front door. The door did alarm during the test. He stated the door will not open if a wandering device comes near the door. If the door was open it would alarm. He again said he did not know what went wrong (09/02/2023). He stated, I just called the company, and they adjusted the antennas. He stated again he did not know what went wrong (on 09/02/2023).
On 10/02/23 at 2:55 p.m. Resident #10's elopement route was observed with the DON and the Regional Nursing Home Administrator (RNHA). This included walking down a steeply sloped driveway and crossing a 2-lane street with a speed limit of 30 miles per hour. There was an occasional car observed going down the street. Resident #10 entered the grounds of an apartment complex. She was found by a gentleman at the back of the apartment complex parking lot. The DON stated she and the NHA went door-to-door in the apartment complex and found the gentleman who brought Resident #10 back. He informed them where he found her in the parking lot. He told the DON and the NHA the resident had told him she wanted to get to the playground, which is part of the apartment complex where she was found. He told them she was calm and was just sitting in her wheelchair. He said he tried to change her mind about going to the playground. (Photographic evidence obtained).
During an interview on 10/02/2023 at 3:12 p.m. the Maintenance Director was asked about the statement on the On-Site Charge Authorization Form. He stated, I just was trying to get them (contracted technology company) to come for the antennas. He stated, It was the only thing I can think of. He verified a work order had been placed 30 days prior to the elopement. He stated he did check the main door, on 09/02/2023, when they came in, post elopement, he documented it was working.
During an interview on 10/02/2023 at 3:30 p.m. the Regional Nursing Home Administrator (RNHA) and the DON stated they verified there were two forms from the contracted technology company, Form 1 was On-site Service Charge Authorization Form, dated 08/02/2023 (a month before elopement), stating Maintenance Director called in requesting a Service Call to have a tech work on the Main Entrance's antennae range as some residents have been able to escape without setting off the alarm. It was signed by the NHA on 09/01/23 (a day before the elopement). The NHA was unavailable for an interview during the dates of the survey.
Form 2 was Service Call Job Form, dated 09/05/2023, and stated Maintenance Director called in requesting a Service Call to have a tech work on the Main Entrance's antennae range as some residents have been able to escape without setting off the alarm. The Service Notes showed On site met Maintenance Director and the NHA. Checked and tested the main entry 9450 T70 with 3 duo link antennae. Adjusted the door antenna and adjusted wiring terminations for timer and bypass button / IEIKeypad. System working as designed. While on site, checked and tested all remaining Code Alert door systems for working order. System ok.
The RNHA stated when he was told about the elopement and the door problems, he told them to put someone on the door and get someone out to fix it as soon as possible (ASAP). The DON stated the NHA had chewed the contracted technology company out (for not responding timely). The RNHA stated the Maintenance Director told him they had receipts from another company, and the Maintenance Director was looking for the receipts.
The RNHA and Maintenance Director produced an invoice from a (contracted electric company). They stated they came out on 08/23/23. The RNHA stated they then called the manufacturer [contracted technology company] because the antennas were still not working properly. The RNHA, the Maintenance Director and the DON stated they could not get the contracted technology company to come out, so they called the contracted electric company to come out. The RNHA stated the main door was not alarming the way it should, so he told the facility to get the manufacturer (contracted technology company). The DON stated the door was supposed to be functioning but was not alarming. The contracted electric company installed new antennas. The contracted technology company came in and did not add any equipment but adjusted the antennas. The Maintenance Director stated he did not know if the antenna was adjusted by the contracted electric company, but it had to be readjusted.
During an interview with the DON on 10/03/2023 at 8:57 a.m. a timeline of the elopement was reviewed. The DON stated at around 12:45 to 1:00 p.m. Staff L, LPN saw the resident coming out of the dining room. She had finished with lunch at 12:40 p.m. and she was on the [NAME] Wing at that time. Staff J, CNA, the aide assigned to the dining room on 9/2/23, said dining was over at 12:40 p.m. The DON stated at approximately 1:37 p.m. the resident was brought to the facility by a gentleman, the receptionist was at the copier. Staff F, receptionist, was alerted due to the wandering device alarm going off when the resident came into the main door. Staff F got the resident and came to the SSD who was the Manager on Duty. The SSD then notified the DON at 1:42 p.m. The DON stated she gave the direction to do a head count to ensure everyone was there. She was enroute, and here at 2:35 p.m. The SSD was at the front door. The DON stated she did a head-to-toe assessment on the resident, with no abnormal findings. The resident was fine. The resident told the DON she was going to work. The DON called the management team in. The DON stated no one saw her, she was able to leave the dining room on her own. The DON verified for approximately 57 minutes it was unknown where the resident was located. The DON stated Staff M, CNA was assigned to care for Resident #10 that day. The DON stated she interviewed Staff M and she saw the resident in the dining room at about 11:30 a.m. on 09/02/2023. The DON stated staffing was good on 09/02/2023, it was meeting the 2.0 minimum. The DON stated the documentation of the event (elopement) was part of the resident's risk notes. Those notes are not found in the resident's electronic medical records. The DON verified there was no documentation in the electronic medical record of the incident. She verified there was only a post evaluation which did not state she eloped. There was no documentation that the attending physician and / or responsible party had been notified. It was documented in the risk report. She stated they had psych (psychiatric services) in to see the resident. They had the attending physician in to see the resident. The DON verified the Psych note on 09/05/2023 showed She elopes and has outdoor privileges. Patient is now on 1:1 observation for safety measures and does not remember. DON stated, she does not have outdoor privileges. The DON stated she would ask medical records if there were any other notes that had not been uploaded. A Post Incident was in the chart. The DON stated, We had an IDT (Interdisciplinary Team) meeting and reviewed the care plan and made sure everything was there. We have an IDT meeting every morning and review all incidents that happen. The note for the IDT meeting was documented in the risk notes by the DON. They did not document the IDT meeting in the electronic medical chart. She stated they reviewed the care plans. They reassessed her elopement risk, performed labs, did a UA and C/S on 09/06/2023. On 09/05/23 they changed the Depakote order. The resident did have a UTI and was treated with antibiotics. She stated the care plan was updated with 1:1 supervision on 09/02/23.
During an interview on 10/03/2023 at 3:01 p.m. the DON stated, She (Resident #10) does not get up as much as she did. She had a UTI. She was used to seeing her up and about. The UTI kind of took her down a little bit. The Depakote may be making her sleepier. I will talk to psych the Advanced Practice Registered Nurse Practitioner (APRN). You have to approach her 'Resident #10 it is time to get up', vs. 'Do you want to get up?'. The DON stated she did not know of any other residents going out. The door was not sounding. She stated, I was used to hearing an alarm when a resident with a wandering device on got near the door. Maintenance told her Some residents have been able to escape without setting off the alarm, was stated (on the Service Form) due to it being so hard to get the company (contracted technology company) out. The DON stated the Maintenance Director and NHA were working it out (the door issue on 08/02/2023). She stated she did not know if the resident was tailgating or not. It (door locking and alarming) would sometimes not capture from the wandering device going out but would always capture on coming in. The DON stated no one was sitting at the main door until 09/02/2023. The DON stated if they knew it (the door) wasn't working, they would have put a staff member on the exit door 24/7 to ensure no one left the building who wasn't supposed to. Before the main door was only being monitored by the receptionist. She stated, She was not aware there was anything wrong with the door. The DON stated, It wasn't always consistently picking them up, but they were picked up and staff intervened.
During an interview on 10/03/2023 at 4:10 p.m. the Maintenance Director stated, The sound announced but it did not announce like it was supposed to be. The door was functioning like it was supposed to but not the sound. I don't know, it was a while ago. He stated, Am positive it was announcing in the past, it has a speaker in it. I know they have to report if someone escapes. If there is an issue, I have to take care of it. I have to do my part. We have had residents escape before and it was reported to you guys. If a resident got out, you guys know about it. The NHA was aware there was a problem. I handed the On-Site Service Charge Authorization Form to the administrator at the time (08/02/2023). I do not know who it was (that eloped). I explained what was going on and [contracted electric company] did a complete check. We had an antenna in the building, and [contracted electric company] replaced it. He did fix the sound, don't know what was going on, but he fixed it. I may have been on the phone with the company (contracted technology company) on 09/02/2023, trying to get them out here. They (contracted technology company) adjusted the two antennas to their full potential range. They are in a half circle. I tested the doors when everyone came in on Saturday, 09/02/2023. It (the testing) was handwritten that I checked all the doors on 09/02/2023. I can't remember that part, if the NHA checked her (the resident's) wandering device and was it was working part time.
During an interview on 10/03/23 at 4:35 p.m. SSD, which was present on the day of the elopement, stated on 09/02/23 she did not know when Resident #10 got out or how. The SSD had gone up front to relieve the receptionist for lunch. Staff F, receptionist, came back from lunch and she stated she came back to her office. Some guy said Resident #10 was across the street. Staff F took her to the nurses' station. Resident #10 then came to my door. She was not sweating; skin was cool to the touch. Resident #10 went down the hall, stated She was going to see her friend. When she got out the door it was not working. She stated she sat at the main door from about 2 p.m. until 6 p.m. She did not know if the door made a noise or not, but it was supposed to lock down, for residents with a wandering device. It (the door) would lock when they got close to the door, but she did not know about the alarms. Resident #10 would get up and go, she was able to self-propel herself.
During an interview on 10/04/23 at 9:02 a.m. Staff M, CNA, who was present on the day of the elopement, stated she was Resident #10's aide that day. She was in the dining room that day. She got her up in the morning and went to the bathroom. The resident wandered. She saw her after lunch. She was walking down the hall and the nurse said she was outside. It was around lunch. She saw her after dining wandering.
During an interview over the phone on 10/04/2023 at 12:58 p.m. Staff L, LPN, who was present on the day of the elopement, stated the resident was up and down the hallways in her wheelchair. She had Just seen her 1 minute before that happened. She could have Only been out of the building for 2 or 3 minutes. She thought she went out behind someone. There was no way she got out of the parking lot, she had to be on the patio and brought her back in. There was no way she would have gotten down the driveway in her wheelchair. Stated she did not see how she got in the parking lot. She stated she had just seen her 5 minutes before they called, she was out the door. They tested the wandering device. The wandering device on the way back in, it went off. She was assessed, looked over, nothing was wrong. The aides Put her back to bed. They called a Code Gray and we had to make sure all the residents were accounted for. We looked her over, she had no bruises or skin tears. Staff L said she did not know the door was not working. We have a lot of residents who go out to the patio (outside the front door). Resident #10 was the only one she knew of who got out. The receptio[TRUNCATED]
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record review, the facility failed to ensure all grievances were tracked through to their conclusion for 1) voiced concerns by residents from the Resident Counci...
Read full inspector narrative →
Based on observations, interviews, and record review, the facility failed to ensure all grievances were tracked through to their conclusion for 1) voiced concerns by residents from the Resident Council and the Food Committee Council meetings between April 2023 and September 2023, and 2) voiced concerns from three residents (#11, #14, and #17) related to their specific diet out of seventeen residents sampled during survey.
Findings included:
A review was conducted of the Resident Council Meeting Minutes, from April 2023 through September 2023 after speaking with the Resident Council President (Resident #14). An interview was conducted with the Resident Council President (RCP) on 10/03/2023 at 8:50 a.m. The RCP reported the Activities Director (AD) ran the meetings and the RCP was not provided with the minutes from the prior meetings. She reported she did not remember the AD reporting on old business and the status of resolving concerns. The RCP reported the dietary department had not updated likes and dislikes for her and she was aware that new residents are not interviewed about their likes and dislikes and they receive what is on the planned menu. She reported her other concern was the Laundry Department as she rarely gets her own clothing back, even though her name is in all of her clothing.
The Resident Council met on 04/27/2023 and minutes were documented on the Resident Council Minutes form which provided guidance for concerns voiced, such as Old Business and New Business. The guidance provided on the form for Old Business was List unresolved old business from last meeting's minutes, status of the concern and identify person responsible. Move unresolved issues to New Business. Three concerns were documented as Old Business which were noted to be the same concerns documented under New Business as: need denture; need braille for the blind; and name tag employees. There was no documentation of the status of the concerns listed. The section to document new business included actions taken, person responsible, and outcome. Only the person or department responsible was documented.
The Resident Council met on 05/23/2023, the Resident Council Minutes form only included the date, time, meeting location, facilitator and the two officers who were in attendance (President and Secretary). No Meeting Minutes review or Old Business Review was documented. The second page for New Business was not provided. Typed pages with multiple concerns voiced at the meeting included: issues with insulin, missing food from the pantry, slamming doors at night, staff not answering the call lights at 4:00 a.m., staff were cruel about a resident's oxygen use, the television channels were not available, clothing was missing, the smoking patio needed cleaning supplies, it takes too long to answer door alarms and staff don't know the code to turn them off, and visitors enter through the front door on the weekends and set the alarms off. The minutes from May 2023 did not refer to the three voiced concerns from the prior month.
The Resident Council met on 06/27/2023 and the Resident Council Minutes form documented Old Business. Three issues were documented: [NAME] side shower needs a make over; the alarm on the weekend, no one's the code to turn off (sic); and two residents need dental care. The shower concern had not been mentioned in either April 2023 or May 2023; the alarm concern had been brought up in May 2023, and the need for denture care had been mentioned in April 2023 but it was not clear whether it was the same issue. The form did not document an update or person responsible for the three issues documented under Old Business. Three concerns were listed under New Business: renovate west shower with maintenance responsible; dental with social services responsible; and the van not working with maintenance responsible. All three concerns were marked 'not resolved'. Hand written notes from the meeting were reviewed and included a request that the Administrator attend the meetings. The kitchen was noted for having improved big time, but with the concern voiced there were too many canned peaches and pineapple on the menu and no fresh fruit. The west side shower was described as needing to be renovated as it was found to be moldy, and without a mirror, shelf or waste basket.
The Resident Council met on 07/25/2023 and the documented minutes were typed out, rather than added to the form. There was no reference to the old or new business discussed in the June 2023 meeting and whether those issues were resolved. The concern of television channels not available was voiced again with the new concern that the wifi was not good. New concerns were voiced that the aides were not available during the lunch and dinner meal as they were in the dining room, the aides weren't working as a team, the wait for care on the 11-7 shift was long, the call lights were not working or they weren't answered in a timely manner, and missing clothing was a concern.
The Resident Council met on 08/31/2023 and the form did not document old business that was unresolved or new business. The Administrator attended the meeting and reported there would be more help passing meal trays out so the food would be warmer and ready to eat, not cold. Concerns voiced included: four residents on reno (renal) diets that needed their diets and they needed a packed meal to take with them when they went to dialysis, the aides always on their phones, needing fresh water in the smoking area, the kitchen staff needing the code to put the water out on the smoking patio, and the service (from the aides and nurses) was very slow on the weekends. There was no reference to the new or old business voiced in the July 2023 meeting.
An interview was conducted with Resident #13 on 10/04/2023 at 12:45 p.m. The resident stated she had physician orders for a renal diet and she did not receive a packed lunch or snack to take with when she went to dialysis and missed a meal at the facility. She reported when she goes to dialysis, which is three times a week, sometimes they give her a peanut butter and jelly sandwich with crackers but not in a cooler bag. She said it was hit or miss if she would receive the sandwich and crackers.
On 10/03/2023 at 1:00 p.m., Resident # 17 was observed in his room eating his lunch. He reported that he leaves the facility for his dialysis at 4:00 a.m. or 5:00 a.m. three times a week and has never received any food or snacks to take with him to provide for the breakfast that he misses.
The Resident Council met on 09/26/2023. The minutes were typed out without the form in use to document the status of the old and new business. The President took the opportunity to read to the attending residents their rights, specifically about getting up or going to bed when the resident prefers and not when the aides want the resident to go to bed. The President commented that the aides got rude about it, giving the example of a named aide who was rude when she was told the resident was waiting a long time to receive care. The residents voiced that there were still too many agency staff in the building with one resident voicing that their catheter bag was not emptied all night long and the bag was very full. The residents voiced the door alarms were disturbing at night and nobody seemed to know the code to turn them off. Again, the residents voiced the employees needed to team up to care for the residents. It was voiced the agency staff don't need their paper signed if they were not going to do the job. One resident voiced that he had to wait 30 minutes for his medication because his nurse was playing on her phone. The television remained a problem with being out on the weekends and channels were still missing. Another resident voiced he woke up an aide who was sleeping and the aide got mad. The residents suggested appointing someone in the laundry department to look for lost clothing and to check in other residents' closets for the lost clothing. One resident reported her call light was out all weekend and even though they gave her a little bell to ring, they couldn't hear it. She reported that she rang the bell at 2 a.m. and the nurse, rather than helping her, said she would tell her aide and she wasn't assisted until 4 am. There was no reference to voiced concerns from the August 2023 meeting or from concerns that were addressed such as, the extra staff to pass trays so the meals remained hot, or the need for the residents on renal diets to receive the correct foods. Service from the nurses and aides continued to be a concern related to timeliness, availability and maintaining a pleasant attitude.
Minutes from the Food Committee were reviewed. On 06/08/23 the Food Committee met and a concern was voiced that the residents wanted more condiments served with their meals. There was no reference in the following meetings as to whether the residents noted more condiments provided, but observation of resident meals on 10/04/2023 at lunch revealed a biscuit was served with the beef stew and even though the planned menu and resident specific diet slips indicated margarine would be provided with the biscuit - it was not. On 10/04/23 pancakes were served at breakfast and residents were not served maple syrup.
On 08/28/2023 the Food Committee minutes included the request for english muffins to be buttered in the kitchen. On 10/05/2023, Resident # 17 had received an english muffin at breakfast. It was noted to be dry, without having been buttered in the kitchen. Margarine packets were not observed on the resident's meal tray.
An interview was conducted with the Activities Director (AD) on 10/02/2023 at 12:45 p.m. The AD was asked what her process for addressing concerns voiced by residents at Resident Council was. She reported after the meeting, she would verbally tell department heads about the concerns voiced by the residents. She stated she did not receive the resolutions to the grievance voiced at the meetings or the status of the actions on the concern. She confirmed she didn't review old business with the residents at their next meeting. She stated she had not thought about doing that. She reported she didn't have a reason for why sometimes she used the Resident Council Minutes form and sometimes she did not.
An interview was conducted with the Director of Nursing (DON) on 10/03/2023 at 11:00 a.m. She reported the AD is responsible to share with the relevant department heads any concern voiced at the resident council meeting.
An interview was conducted with the Administrator on 10/03/2023 at 11:10 a.m. The Administrator reported the facility management staff discussed concerns voiced through the grievance process and during resident council meetings at the facility's monthly Quality meeting. The Administrator was told of the interview conducted with the AD and how the AD reported she verbally shared with department heads voiced grievances but did not expect or did not receive information back on the status of the voiced grievances. The Administrator reported the process of resolving resident grievances needed to be reviewed and tightened up.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to ensure residents were free from unnecessary medications by 1) not...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to ensure residents were free from unnecessary medications by 1) not ensuring proper behavioral and side effect monitoring for psychotropic medications for four residents (#2, #5, #6, and #14) of four residents sampled and, 2) not ensuring use of as needed (PRN) psychotropic medications were limited to 14 days for one resident (#5) of four residents sampled.
Findings included:
A review of the medical record revealed Resident #2 was admitted to the facility on [DATE] with diagnoses of insomnia and wedge compression fracture of the first lumbar vertebra. Resident #2 was discharged from the facility on 5/29/2023.
A review of Resident #2's physician's orders revealed the following orders:
- An order, dated 5/18/2023 for Zolpidem Tartrate 10 milligrams (mg) by mouth (PO) as needed at bedtime for insomnia. The order was discontinued on 5/18/2023 and restarted on 5/19/2023 with an order duration limited to 14 days.
- An order, dated 5/19/2023 for sedative/hypnotic medication behavioral monitoring for sleeplessness. Document Y if the resident has behaviors and N if the resident does not have behaviors. If Y document in the progress notes (PNs) every shift. The order was duplicated on 5/22/2023 to include the additional instructions for insomnia.
- An order, dated 5/19/2023 for side effect observation: 1-Dystonia, torticollis (stiffness of neck); 2-Anticholinergic symptoms: dry mouth/blurred vision, constipation/urinary retention; 3-Hypotension; 4-Sedation/drowsiness; 5-Increased falls/dizziness; 6-Cardiac abnormalities (tachycardia, bradycardia, irregular heart rate (HR); 7-Anxiety/agitation; 8-Blurred vision; 9-Sweating/rashes; 10-Headache; 11-Urinary retention/hesitancy; 12-Weakness; 13-Hangover effect; 14-Pseudoparkinsonism; 15-Insomnia; 16-New onset confusion, every shift for medication side effect monitoring.
- An order, dated 5/19/2023 for side effect observation: 17-Akathisia-Restlessness/pacing/inability to sit still/anxiousness/sleep disturbances; 18-Tardive dyskinesia-lip smacking/chewing/abnormal tongue movement/spasmodic movement of arms/legs-rocking/swaying; 19-Sore throat; 20-Seizures; 21-Photosensitivity; 22-Suicidal ideations; 23-Hepatic or renal abnormalities; 24-Ataxia; 25-Nausea/vomiting; 26-Diarrhea; 27-Abdominal discomfort; 28-Discolored urine; 29-Black tarry stools; 30-Bruising; 31-Nose bleeds, every shift for medication side effect monitoring.
A review of Resident #2's behavior monitoring record for May 2023 revealed the following:
- Review of documentation for the order dated 5/19/2023 for sedative/hypnotic medication behavioral monitoring for sleeplessness every shift did not reveal documentation on the Day (7 AM to 3 PM) shift on 5/21, 5/22, 5/24, and 5/28/2023, on the Evening (3 PM to 11 PM) shift on 5/26 and 5/27/2023, or on the Night (11 PM to 7 AM) shift on 5/20/2023.
- Review of documentation for the order dated 5/22/2023 for sedative/hypnotic medication behavioral monitoring for sleeplessness every shift for insomnia did not reveal documentation on the Day shift on 5/24, and 5/28/2023 or on the Evening shift on 5/26 and 5/27/2023.
- Review of documentation for the orders dated 5/19/2023 for side effect observation every shift for medication side effect monitoring did not reveal documentation on the Day shift on 5/21, 5/22, 5/24, and 5/28/2023, on the Evening shift on 5/26 and 5/27/2023, or the Night shift on 5/20/2023.
A review of Resident #5's medical record revealed Resident #5 was admitted to the facility on [DATE] with diagnoses of brief psychotic disorder, major depressive disorder, and anxiety disorder.
A review of Resident #5's physician's orders revealed the following orders:
- An order, dated 9/28/2023 for Haldol 1 mg PO every 4 hours as needed for agitation. The order did not include a duration of use and did not have an end date.
- An order, dated 9/13/2023 for Ativan 0.5 mg PO every 4 hours as needed for anxiety. The order did not include a duration of use and did not have an end date.
- An order, dated 9/8/2023 for Ativan 0.5 mg PO every 12 hours for anxiety.
- An order, dated 7/26/2023 for Mirtazapine 15 mg PO at bedtime for depression.
- An order, dated 6/8/2023 for antianxiety medication behavioral monitoring for restlessness. Document Y if the resident has behaviors and N if the resident does not have behaviors. If Y document in the PNs every shift.
- An order, dated 6/8/2023 for antidepressant medication behavioral monitoring for sadness, tearfulness, and/or self-isolation. Document Y if the resident has behaviors and N if the resident does not have behaviors. If Y document in the PNs every shift.
- An order, dated 6/8/2023 for side effect observation: 1-Dystonia, torticollis (stiffness of neck); 2-Anticholinergic symptoms: dry mouth/blurred vision, constipation/urinary retention; 3-Hypotension; 4-Sedation/drowsiness; 5-Increased falls/dizziness; 6-Cardiac abnormalities (tachycardia, bradycardia, irregular heart rate (HR); 7-Anxiety/agitation; 8-Blurred vision; 9-Sweating/rashes; 10-Headache; 11-Urinary retention/hesitancy; 12-Weakness; 13-Hangover effect; 14-Pseudoparkinsonism; 15-Insomnia; 16-New onset confusion, every shift for medication side effect monitoring.
- An order, dated 6/8/2023 for side effect observation: 17-Akathisia-Restlessness/pacing/inability to sit still/anxiousness/sleep disturbances; 18-Tardive dyskinesia-lip smacking/chewing/abnormal tongue movement/spasmodic movement of arms/legs-rocking/swaying; 19-Sore throat; 20-Seizures; 21-Photosensitivity; 22-Suicidal ideations; 23-Hepatic or renal abnormalities; 24-Ataxia; 25-Nausea/vomiting; 26-Diarrhea; 27-Abdominal discomfort; 28-Discolored urine; 29-Black tarry stools; 30-Bruising; 31-Nose bleeds, every shift for medication side effect monitoring.
Resident #5's physician's orders did not reveal orders related to antipsychotic medication behavioral monitoring.
A review of Resident #5's behavior monitoring record for September 2023 revealed the following:
- Review of documentation for the order dated 6/8/2023 for antianxiety medication behavioral monitoring for restlessness every shift did not reveal documentation on the Day shift on 9/4, 9/5, 9/6, 9/7, 9/13, 9/15, 9/20, 9/26, and 9/27/2023, on the Evening shift on 9/2, 9/4, 9/7, 9/13, 9/14, 9/15, 9/18, 9/20, 9/24, 9/26, 9/27, and 9/28/2023, or the Night shift on 9/23, 9/24, 9/26, and 9/27/2023.
- Review of documentation for the order dated 6/8/2023 for antidepressant medication behavioral monitoring for sadness, tearfulness, and/or self-isolation every shift did not reveal documentation on the Day shift on 9/4, 9/5, 9/6, 9/7, 9/13, 9/15, 9/20, 9/26, and 9/27/2023, on the Evening shift on 9/2, 9/4, 9/7, 9/13, 9/14, 9/15, 9/18, 9/20, 9/24, 9/26, 9/27, and 9/28/2023, or the Night shift on 9/23, 9/24, 9/26, and 9/27/2023.
- Review of documentation for the orders dated 6/8/2023 for side effect observation every shift did not reveal documentation on the Day shift on 9/4, 9/5, 9/6, 9/7, 9/13, 9/15, 9/20, 9/26, and 9/27/2023, on the Evening shift on 9/2, 9/4, 9/7, 9/13, 9/14, 9/15, 9/18, 9/20, 9/24, 9/26, 9/27, and 9/28/2023, or the Night shift on 9/23, 9/24, 9/26, and 9/27/2023.
A review of Resident #5's behavior monitoring record for August 2023 revealed the following:
- Review of documentation for the order dated 6/8/2023 for antianxiety medication behavioral monitoring for restlessness every shift did not reveal documentation on the Day shift on 8/7, 8/17, 8/21, 8/24, 8/26, 8/27, 8/30, and 8/31/2023, on the Evening shift on 8/5, 8/7, 8/9, 8/10, 8/13, 8/17, 8/20, 8/21, 8/23, 8/24, 8/25, 8/27, 8/29, 8/30, and 8/31/2023, or on the Night shift on 8/6, 8/10, and 8/26/2023.
- Review of documentation for the order dated 6/8/2023 for antidepressant medication behavioral monitoring for sadness, tearfulness, and/or self-isolation every shift did not reveal documentation on the Day shift on 8/7, 8/17, 8/21, 8/24, 8/26, 8/27, 8/30, and 8/31/2023, on the Evening shift on 8/5, 8/7, 8/9, 8/10, 8/13, 8/17, 8/20, 8/21, 8/23, 8/24, 8/25, 8/27, 8/29, 8/30, and 8/31/2023, or on the Night shift on 8/6, 8/10, and 8/26/2023.
- Review of documentation for the orders dated 6/8/2023 for side effect observation every shift did not reveal documentation on the Day shift on 8/7, 8/17, 8/21, 8/24, 8/26, 8/27, 8/30, and 8/31/2023, on the Evening shift on 8/5, 8/7, 8/9, 8/10, 8/13, 8/17, 8/20, 8/21, 8/23, 8/24, 8/25, 8/27, 8/29, 8/30, and 8/31/2023, or on the Night shift on 8/6, 8/10, and 8/26/2023.
A review of Resident #6's medical record revealed Resident #6 was admitted to the facility on [DATE] with a diagnosis of anxiety disorder.
A review of Resident #6's physician's orders revealed the following orders:
- An order, dated 6/10/2023 for Alprazolam 0.5 mg PO at bedtime for anxiety.
- An order, dated 6/10/2023 for antianxiety medication behavioral monitoring for restlessness. Document Y if the resident has behaviors and N if the resident does not have behaviors. If Y document in the PNs every shift.
- An order, dated 1/25/2023 for side effect observation: 1-Dystonia, torticollis (stiffness of neck); 2-Anticholinergic symptoms: dry mouth/blurred vision, constipation/urinary retention; 3-Hypotension; 4-Sedation/drowsiness; 5-Increased falls/dizziness; 6-Cardiac abnormalities (tachycardia, bradycardia, irregular heart rate (HR); 7-Anxiety/agitation; 8-Blurred vision; 9-Sweating/rashes; 10-Headache; 11-Urinary retention/hesitancy; 12-Weakness; 13-Hangover effect; 14-Pseudoparkinsonism; 15-Insomnia; 16-New onset confusion, every shift for medication side effect monitoring.
- An order, dated 1/25/2023 for side effect observation: 17-Akathisia-Restlessness/pacing/inability to sit still/anxiousness/sleep disturbances; 18-Tardive dyskinesia-lip smacking/chewing/abnormal tongue movement/spasmodic movement of arms/legs-rocking/swaying; 19-Sore throat; 20-Seizures; 21-Photosensitivity; 22-Suicidal ideations; 23-Hepatic or renal abnormalities; 24-Ataxia; 25-Nausea/vomiting; 26-Diarrhea; 27-Abdominal discomfort; 28-Discolored urine; 29-Black tarry stools; 30-Bruising; 31-Nose bleeds, every shift for medication side effect monitoring.
A review of Resident #6's behavior monitoring record for September 2023 revealed the following:
- Review of documentation for the order dated 6/10/2023 for antianxiety medication behavioral monitoring for restlessness every shift did not reveal documentation on the Day shift on 9/9, 9/10, 9/15, and 9/22/2023, on the Evening shift on 9/2, 9/3, 9/4, 9/6, 9/7, 9/15, 9/16, 9/18, 9/19, 9/20, 9/21, 9/22, 9/23, 9/25, 9/26, 9/27, and 9/28/2023, or on the Night shift on 9/3 and 9/26/2023.
A review of Resident #6's behavior monitoring record for August 2023 revealed the following:
- Review of documentation for the order dated 6/10/2023 for antianxiety medication behavioral monitoring for restlessness every shift did not reveal documentation on the Day shift on 8/3, 8/13, and 8/18/2023, on the Evening shift on 8/1, 8/2, 8/3, 8/6, 8/7, 8/8, 8/9, 8/10, 8/11, 8/12, 8/13, 8/16, 8/17, 8/19, 8/20, 8/21, 8/22, 8/23, 8/24, 8/25, 8/28, 8/29, and 8/31/2023, or on the Night shift on 8/7, 8/8, 8/11, 8/12, 8/13, 8/14, and 8/29/2023.
A review of Resident #6's treatment administration record (TAR) for August 2023 revealed the following:
- Review of documentation for the orders dated 1/25/2023 for side effect observation every shift did not reveal documentation on the Evening shift on 8/9/2023 or on the Night shift on 8/29/2023.
A review of Resident #14's medical record revealed Resident #14 was admitted to the facility on [DATE] with diagnoses of major depressive disorder and generalized anxiety disorder.
A review of Resident #14's physician's orders revealed the following orders:
- An order, dated 5/31/2023 for Citalopram 15 mg PO once daily for depression.
- An order, dated 7/31/2023 for antidepressant medication behavioral monitoring for sadness, tearfulness, and/or self-isolation. Document Y if the resident has behaviors and N if the resident does not have behaviors. If Y document in the PNs every shift.
- An order, dated 7/31/2023 for side effect observation: 1-Dystonia, torticollis (stiffness of neck); 2-Anticholinergic symptoms: dry mouth/blurred vision, constipation/urinary retention; 3-Hypotension; 4-Sedation/drowsiness; 5-Increased falls/dizziness; 6-Cardiac abnormalities (tachycardia, bradycardia, irregular heart rate (HR); 7-Anxiety/agitation; 8-Blurred vision; 9-Sweating/rashes; 10-Headache; 11-Urinary retention/hesitancy; 12-Weakness; 13-Hangover effect; 14-Pseudoparkinsonism; 15-Insomnia; 16-New onset confusion, every shift for medication side effect monitoring.
- An order, dated 7/31/2023 for side effect observation: 17-Akathisia-Restlessness/pacing/inability to sit still/anxiousness/sleep disturbances; 18-Tardive dyskinesia-lip smacking/chewing/abnormal tongue movement/spasmodic movement of arms/legs-rocking/swaying; 19-Sore throat; 20-Seizures; 21-Photosensitivity; 22-Suicidal ideations; 23-Hepatic or renal abnormalities; 24-Ataxia; 25-Nausea/vomiting; 26-Diarrhea; 27-Abdominal discomfort; 28-Discolored urine; 29-Black tarry stools; 30-Bruising; 31-Nose bleeds, every shift for medication side effect monitoring.
A review of Resident #14's behavior monitoring record for September 2023 revealed the following:
- Review of documentation for the order dated 7/31/2023 for antidepressant medication behavioral monitoring for sadness, tearfulness, and/or self-isolation every shift did not reveal documentation on the Day shift on 9/16/2023 or on the Night shift on 9/24 and 9/27/2023.
- Review of documentation for the orders dated 7/31/2023 for side effect observation every shift did not reveal documentation on the Day shift on 9/16/2023 or on the Night shift on 9/24 and 9/27/2023.
A review of Resident #14's behavior monitoring record for August 2023 revealed the following:
- Review of documentation for the order dated 7/31/2023 for antidepressant medication behavioral monitoring for sadness, tearfulness, and/or self-isolation every shift did not reveal documentation on the Day shift on 8/5 and 8/29/2023, on the Evening shift on 9/13/2023, or on the Night shift on 8/6/2023.
- Review of documentation for the order dated 7/31/2023 for side effect observation every shift did not reveal documentation on the Day shift on 8/5 and 8/29/2023, on the Evening shift on 9/13/2023, or on the Night shift on 8/6/2023.
An interview was conducted on 10/3/2023 at 10:48 AM with Staff A, Licensed Practical Nurse (LPN), who was Resident #6's assigned nurse for the Day shift. Staff A, LPN stated residents who were prescribed psychotropic medications had orders in place to monitor for behaviors and side effects related to that medication, completed every shift. Staff A, LPN reviewed Resident #6's behavioral monitoring record and addressed the missing documentation related to Resident #6's behavioral and side effect monitoring for antianxiety medication use. Staff A, LPN stated the documentation might not have been completed because Resident #6 did not have any behaviors or side effects on that shift or the residents may not have been in the facility during that shift. Staff A, LPN stated if a resident was not present in the facility there would be documentation to show the resident was not present at the time and the documentation should be completed each shift as ordered.
An interview was conducted on 10/3/2023 at 11:35 AM with Staff B, LPN, who was Resident #14's assigned nurse for the Day shift. Staff B, LPN stated residents who receive psychotropic medications have orders in place to document and behavioral or side effects related to that medication and the documentation should be completed every shift. Staff B, LPN reviewed Resident #14's medications and stated side effect and behavioral monitoring should be completed for Resident #14's use of Citalopram because it is an antidepressant. Staff B, LPN reviewed Resident #14's behavioral monitoring record and stated the record should not contain any blanks or missing documentation and the documentation should be completed every shift as ordered.
An interview was conducted on 10/3/2023 at 1:18 PM with Staff C, LPN, who was Resident #5's assigned nurse for the Day shift. Staff C, LPN stated resident's who are administered psychotropic medications are monitored for side effects and behaviors related to that medication every shift. Staff C, LPN stated the order appears during medication administration to complete every shift. Staff C, LPN reviewed Resident #5's behavioral monitoring record and addressed the missing documentation for Resident #5's behavioral and side effect monitoring. Staff C, LPN stated the side effect and behavioral monitoring related to psychotropic medication use should be completed as ordered and should not have any missing entries.
An interview was conducted on 10/3/2023 at 2:13 PM with Staff D, LPN Unit Manager (UM). Staff D, LPN UM stated any resident receiving psychotropic medications should have batch orders put in for monitoring of side effects and behaviors. Staff D, LPN UM stated medication classes that would be monitored for side effects and behaviors would include antipsychotics, antidepressants, and antianxiety medications. Staff D, LPN UM stated the floor nurses should be completing their documentation during their shift and before they leave the facility and that she verifies the charting is completed by observing the report in the electronic medical record. Staff D, LPN UM reviewed documentation for Resident #6's use of Alprazolam and verified the missing documentation related to behavioral and side effect monitoring. Staff D, LPN UM stated the floor nurses may have missed the documentation because they were not pulling up the behavior tab in the electronic medical record, which is different from the medication or treatment administration records. Staff D, LPN UM stated the documentation should be completed as ordered and the residents behavior monitoring record should not be missing any documentation.
An interview was conducted on 10/3/2023 at 2:55 PM with Staff B, LPN and Staff C, LPN related to timeframes of as needed (PRN) psychotropic medication use. Staff B, LPN stated they were not instructed to and do not review resident orders to ensure PRN psychotropic medications were limited to 14 days. Staff C, LPN reviewed Resident #5's physician's orders and addressed Resident #5's PRN orders for Haldol and Ativan did not have a limited duration and stated she was not aware the medication order needed to be limited to 14 days.
An interview was conducted on 10/3/2023 at 3:26 PM with Staff E, Registered Nurse (RN) UM. Staff E, RN UM stated she verifies documentation is completed during the Day shift by checking the administration records and ensuring all of the documentation in the various tabs have been completed. Staff E, RN UM stated behavioral and side effect monitoring orders for use of psychotropic medications were previously located in a different section of the chart but is now in a different location. Staff E, RN UM stated any resident prescribed psychotropic medications should have orders in place for monitoring of behaviors and side effects and documentation is completed every shift by the resident's nurse. Staff E, RM UM stated psychotropic medications that are administered on a PRN basis should only be prescribed for 14 days. Staff E, RM UM reviewed Resident #5's physician's orders and address the PRN order for Haldol and Ativan did not have an end date.
An interview was conducted on 10/3/2023 at 4:50 PM with the facility's Director of Nursing (DON). The DON stated she was aware Resident #5 had physician's orders for PRN psychotropic medications which were not limited to 14 days. The DON stated Resident #5 was under hospice care and the provider did not want a stop date on the PRN medication. The DON was not able to state if the facility policy included exceptions based on whether or not a resident was under hospice care. The DON stated behavioral monitoring orders would be implemented based on the type of psychotropic medication the resident was receiving and the orders for side effect monitoring was a catch all for any medication that needed to be monitored for any type of side effect. The DON stated behavioral and side effect monitoring should be completed every shift and the nurse management team should be reviewing the documentation to ensure it is completed as ordered. The DON stated some nurses have not been completing the behavioral and side effect documentation because the documentation was moved to a different tab in the electronic medical record and nurses were not seeing it.
A review of the facility policy titled Use of Psychotropic Medication, last revised in May of 2023, revealed the following:
Policy residents are not given psychotropic drugs unless the medication is necessary to treat a specific condition, as diagnosed and documented in the clinical record, and the medication is beneficial to the resident, as demonstrated by monitoring and documentation of the resident's response to the medication(s).
Policy Explanation and Compliance Guidelines:
- A psychotropic drug is any drug that affects brain activities associated with mental processes and behavior. Psychotropic drugs include, but are not limited to the following categories: antipsychotics, antidepressants, anti-anxiety, and hypnotics.
- PRN orders for all psychotropic drugs shall be used only when the medication is necessary to treat a diagnosed specific condition that is documented in the clinical record, and for a limited duration (i.e. 14 days).
- The effects of the psychotropic medications on a resident's physical, mental, and psychosocial well-being will be evaluated on an ongoing basis, such as in accordance with nurse assessments and medication monitoring parameters consistent with clinical standards of practice, manufacturer's specifications, and the resident's comprehensive plan of care.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review the facility 1) failed to ensure the planned menu was followed for three of...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review the facility 1) failed to ensure the planned menu was followed for three of three observed meals during lunch, 2) failed to ensure residents received an alternate meal when they were absent from the facility for three residents (#11, #14, and #17) out of seventeen sampled, and 3) failed to ensure residents were provided their preferences at meals for four residents (#11, #17, #13, and #6) of seventeen residents sampled during survey.
Findings included:
Resident #11 was admitted to the facility on [DATE] with diagnoses that included Metabolic Encephalopathy, unspecified protein-calorie malnutrition, Chronic Kidney Disease, and Dementia. At admission the physician ordered a Mechanical Soft, Renal diet. A review of the Minimum Data Set (MDS) admission Assessment, dated 07/24/2023, revealed the resident's Brief Interview for Mental Status (BIMS) was coded as a 99, indicating the resident was cognitively not able to complete the interview.
On 10/02/2023 at 1:00 p.m., Resident #11 was observed in her room, sitting on her bed. She had received her lunch which was a large serving of baked ziti with cheese, a serving of whole green beans, a chocolate chip cookie, an 8 ounce carton of whole milk, and an 8 ounce cup of a drink. She had eaten most of the ziti with cheese, all of the cookie, and was drinking her milk. She had eaten none of the green beans or the garlic bread. The resident's diet slip indicated she was on a Mechanical Soft Renal diet. A review of the planned lunch menu for 10/02/2023 revealed the residents on the renal diet should have received a salisbury steak with buttered egg noodles and brown gravy, green beans, garlic bread, 4 ounces of whole milk and creamy rice pudding for dessert.
An interview with the Dietary Manager (DM) and Staff Q, [NAME] was conducted on 10/02/2023 at 1:00 p.m. They stated the canned rice pudding that was planned for dessert had not been delivered by the food service company so the cookie had to be substituted. Neither the DM nor the cook could recall that Resident #11 was on a renal diet and they didn't know whether she had received the salisbury steak rather than the ziti with cheese.
On 10/03/2023 at 12:30 p.m., Resident #14 was observed to be in her room, sitting on her bed. She had been served her lunch which included ground breaded chicken with gravy, macaroni and cheese, spinach, and vanilla pudding for dessert. She had been served an 8 ounce cup of an orange drink and an 8 ounce container of whole milk. A review of the diet slip which accompanied the meal tray revealed the resident had a physician's order for a Mechanical Soft, Renal Diet. A review of the planned menu for the mechanical soft renal diet included ground baked chicken, buttered elbow macaroni, buttered spinach, fruited citrus gelatin and 4 ounces of whole milk.
An interview was conducted with the Staff Q, [NAME] on 10/03/2023 at 1:10 p.m. Staff Q stated he had not prepared the plain buttered elbow macaroni for the residents who had physician ordered renal diets as there were just a few of those residents, and he just served them the macaroni and cheese instead. He stated he had not prepared plain baked chicken for the renal diet residents either. At that same time, the Dietary Manager (DM) was asked about the substituted dessert of the pudding instead of the fruited gelatin. The DM stated no one had made the gelatin the day before so they served the pudding (a canned product) instead.
Resident # 17 was admitted to the facility on [DATE] with diagnoses that included end stage renal disease with dialysis. A review of the MDS quarterly assessment, dated 08/29/2023, revealed the BIMS score as 14, indicating intact cognition.
On 10/03/2023 at 1:00 p.m., Resident # 17 was observed in his room eating his lunch. He reported he leaves the facility for his dialysis at 4:00 a.m. or 5:00 a.m. three times a week and has never received any food or snacks to take with him to provide for the breakfast that he misses. He reported he usually gets back just in time for lunch. During the interview, the resident was eating chicken and he said it was good. When asked about the side dish, he reported it was macaroni and cheese. When the menu was read out to him, indicating buttered noodles, he reported that no, his macaroni was more than just buttered, there was a mild cheese flavor. The resident confirmed that the chicken he had received was breaded, not a plain baked piece of chicken. The resident had received no milk on his lunch tray, but had received two 4 ounce vanilla pudding cups, rather than the planned dessert of fruited gelatin.
On 10/05/2023 during breakfast, Resident #17 was observed in his room, but his breakfast tray could be seen sitting on his over bed table. The resident had left for dialysis before the breakfast tray was served. The breakfast tray was observed to be complete and none of the food items or condiments had been touched. The resident had received scrambled eggs, an unbuttered english muffin split into halves with no butter on the tray for the muffin. He had received 8 ounces of whole milk and 4 ounces of orange juice. The diet slip accompanying the meal indicated for a regular renal diet, the resident should have been served 4 ounces of an apple juice blend, 1 margarine cup, and 4 ounces of whole milk, as well as the eggs and english muffin.
An MDS admission assessment, dated 08/20/2023, for Resident #13 documented a BIMS score of 15, indicating intact cognition.
On 10/04/2023 at 12:45 p.m. Resident #13 was observed having finished her lunch and was sitting on the side of her bed. She reported the food isn't very good, and she showed me she had eaten about half of the beef stew, none of the cauliflower, and less than half of the biscuit. She reported the facility did not follow the renal diet. The planned menu was a 6 ounce serving of beef stew with a 4 ounce serving of buttered cauliflower, a biscuit with margarine, 8 ounces of whole milk, and orange sherbet for dessert. The planned renal diet was 6 ounces of beef tips in gravy with buttered cauliflower, a dinner roll, orange sherbet and 4 ounces of milk. Resident #13 had received the beef stew- with potatoes and carrots, not the single menu item of beef tips, a biscuit with no margarine, 8 ounces of whole milk and rainbow sherbet. She reported when she goes to dialysis sometimes they give her a peanut butter and jelly sandwich with crackers maybe, but not in a cooler bag. She said that it was hit or miss that she would receive the sandwich and crackers.
The MDS quarterly assessment, dated 07/17/2023, for Resident #6 documented a BIMS score of 14, indicating intact cognition.
An interview was conducted with Resident # 6 on 10/02/2023 at 3:30 p.m. She reported the Dietary Department does not follow the diet slips where they list residents' likes and dislikes. She reported she always gets food items she dislikes which means she then has to send her aide back to the kitchen to get what she had initially asked for. She reported she thought her hall was the last to be served and often the kitchen will run out of what ever they had planned to serve. She said one night the planned menu was a kielbasa sausage on a hoagie roll. She said by the time she was served, they must have run out of the kielbasa as she received a hot dog on a hot dog bun with no condiments. She said her aide went back to the kitchen to ask for a cheeseburger and the aide came back with the message from the Cook, Staff R, that there were no cheeseburgers and she would have to eat the hot dog or eat nothing.
On 10/05/23 at 9:00 a.m. an interview was conducted with the Dietary Manager (DM) about the residents who had physician ordered renal diets. He stated there were two residents who were on renal diets. (During the survey there were three residents who had physician ordered renal diets - Resident # 11, #13, and #17.) The DM stated peanut butter and jelly sandwiches, juices, and snacks such as crackers, cookies, and puddings are stocked in the pantries on the resident wings and nurses or aides are supposed to pack a meal for the resident prior to the resident leaving for the dialysis session. The DM stated he attends the Food Committee Meetings, but had not been discussing how the last voiced concerns were being addressed.
On 10/05/2023 at 9:20 a.m. an interview was conducted with Staff B, LPN. Staff B stated the dietary department packs up a lunch with snacks and drinks, for dialysis residents, in an insulated bag with a cooling pack and either leaves it in the refrigerator for residents who miss breakfast, or deliver it later for residents who miss lunch.
On 10/05/2023 at 9:30 a.m. an interview was conducted with Staff D, Unit Manager. She stated the dietary department leaves a packed lunch in the pantry refrigerator for the dialysis resident.
A list of snacks available in the pantry was reviewed and it was noted that no sandwiches were on the list for residents to take to dialysis. Snacks included potato chips, cheez-its, oatmeal creme pie cookies, peanut butter crackers, and chocolate or vanilla pudding.
A review of Resident Council Minutes from 08/31/2023 revealed a concern that four residents on the reno (renal) diet needed their diets and they needed a packed meal to take with them when they went to dialysis. The Resident Council meeting minutes from the meeting held on 09/26/2023 did not refer to the status of the voiced concern for the residents who were not receiving their renal diets.
A review of Food Committee minutes from 06/08/2023 revealed a concern was voiced that the residents wanted more condiments served with their meals. There was no reference in the following meetings as to whether the residents noted more condiments provided.
Observation of resident meals on 10/04/2023 at lunch revealed a biscuit was served with the beef stew and even though the planned menu and resident specific diet slips indicated margarine would be provided with the biscuit it was not. On 10/04/2023 pancakes were served at breakfast and residents were not served maple or any other flavor of syrup.
On 08/28/2023 the Food Committee minutes included the request for english muffins to be buttered in the kitchen. On 10/05/23, Resident #17 received an english muffin. It was noted to be dry, without having been buttered in the kitchen. Margarine packets were not observed on the resident meal trays.