CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, Incident and Accident (I&A) report review, resident, family, and staff interview, it was determined the ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, Incident and Accident (I&A) report review, resident, family, and staff interview, it was determined the facility failed to ensure residents received the level of supervision necessary to prevent residents with diminished cognitive ability from elopement from the facility and to prevent falls. This was true for 2 of 6 residents (#6 and #12) reviewed for supervision and accidents. The facility's failure to implement and maintain supervision measures to prevent elopement placed Resident #12 in immediate jeopardy of serious harm, impairment, or death. The facility's failure to ensure Resident #6 received the level of supervision necessary to prevent falls placed him at risk of bone fractures and/or other serious injuries when he sustained repeated falls over a 3 month period. Findings include:
1. Resident #12 was admitted to the facility 11/12/20, with multiple diagnoses including dementia and depression.
Idaho Preadmission screening and resident review (PASARR), dated 11/12/20, documented Resident #12 had a history of a suicide attempt and suicidal talk and ideas. It stated she received mental health services on 12/9/19, and had a suicide attempt or gesture on 3/16/20.
Resident #12's quarterly MDS assessment, dated 5/3/21, documented she was severely cognitively impaired and walked with a walker.
A nursing progress note, dated 12/21/20 at 5:42 PM, documented Resident #12 had exited the building at 5:00 PM and walked over to the assisted living building, located on the same property. The note documented Resident #12 did not have injuries. The note documented Resident #12's family member and the physician were notified, and an order was received to place a wander guard bracelet on Resident #12's wrist.
The wander guard was placed on Resident #12 and her TAR documented staff were to check the site (wrist) and function of her wander guard every shift, beginning on 12/21/20.
Resident #12's care plan for elopement risk documented the following interventions:
* Distract Resident #12 from wandering, initiated on 12/22/20.
* Identify the pattern of Resident #12's wandering, initiated on 12/22/20.
* Provide structured activities, initiated on 12/22/20.
* Apply wander guard to wrist and check every shift and as needed to ensure it was in place and monitor for proper functioning, initiated on 12/23/20.
* Offer to walk with Resident #12 when she becomes restless, initiated on 12/23/20.
A social services progress note, dated 12/24/20 at 10:43 AM, documented a care conference was held with Resident #12's family to discuss her wandering. The note documented if Resident #12 continued to wander they may need to look for a dementia unit for her. The note documented her family agreed.
A nursing note, dated 3/24/21 at 3:20 PM, documented Resident #12 attempted to exit from the front door and her wander guard alarm sounded. The note documented Resident #12 was confused and was able to be redirected.
A nursing progress note, dated 4/7/21 at 3:38 PM, documented Resident #12 had left the facility with family for an outing and her wander guard did not alarm. The note documented the wander guard was going to be assessed upon Resident #12's return.
A nursing progress note, dated 4/8/21 at 1:21 PM, documented Resident #12 was .wandering around more today . and her wander guard was not working. The note documented management was aware Resident #12's wander guard was not working and were attempting to locate .a new band for her new wander guard.
Progress notes documented Resident #12 was not wearing her wander guard bracelet on 4/9/21 at 10:17 AM and 4/11/21 at 2:38 PM, 2:39 PM, and 2:56 PM. Resident #12's wander guard was not functioning and/or worn for 4 days.
A nursing progress note, dated 4/11/21 at 6:21 PM, documented Resident #12 was up and roaming around facility more than before. The note documented Resident #12 did not have her wander guard on and the oncoming nurse was notified.
Progress notes documented Resident #12 was not wearing her wander guard bracelet on 4/12/21 at 2:10 AM and 12:54 PM.
A social services progress note, dated 4/20/21 at 5:58 PM, documented staff reported to the Social Services Director Resident #12 was displaying increased behavior of eloping/wandering and increased signs and symptoms of depression. The note documented behavior monitoring was in place and the Social Service Director was going to speak with Resident #12 the following day. The next note by the Social Services Director was on 4/30/21, 10 days later, which documented she had left a message with Resident #12's family member to set up a care conference.
A nursing progress note, dated 4/25/21 at 6:02 PM, documented Resident #12 made several attempts to leave the building, stating she needed to go home. The note documented she was redirected by staff.
A nursing progress note, dated 4/27/21 at 7:41 PM, documented Resident #12 made several attempts to leave the building, stating she needed to go home. The note documented she was redirected by staff.
A nursing progress note, dated 4/29/21 at 11:25 AM, documented Resident #12 had gathered some personal belongings and was attempting to leave the building. The note documented she was redirected by staff.
A nursing progress note, dated 4/29/21 at 2:17 PM, documented a call was received from Resident #12's husband and he stated Resident #12 was at their house. The note documented her husband stated Resident #12 was wearing the wander guard. The note documented staff had reported Resident #12 was attempting to exit the facility at approximately 10:30 AM and she was with a staff one-on-one until .she calmed down. The note documented Resident #12 was last seen by a nurse at approximately 11:30 AM. The note also documented Resident #12's husband stated he planned to bring her back to the facility after he visited with her.
An I&A report, dated 5/4/21, documented Resident #12 left the faciity on 4/29/21 without staff knowledge. The I&A report documented the facility became aware Resident #12 had left when her husband called the facility at 2:17 PM. Resident #12's husband reported she was at his home and her wander guard was in place on her wrist. The report documented the root cause of the elopement was due to Resident #12's poor safety awareness, confusion, and that she missed her family. The report documented the plan was to replace her wander guard bracelet and they ordered a transmitter to check the function of the wander guard device. The report also documented staff were to .complete routine visual checks on residents. Staff education provided.
It was unclear in the documentation from the facility the amount of time Resident #12 was away from the facility and without supervision.
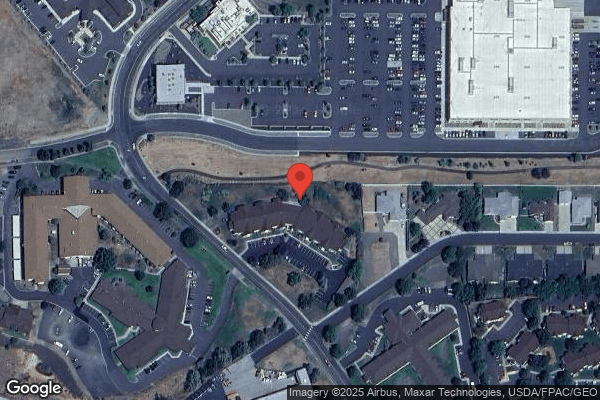
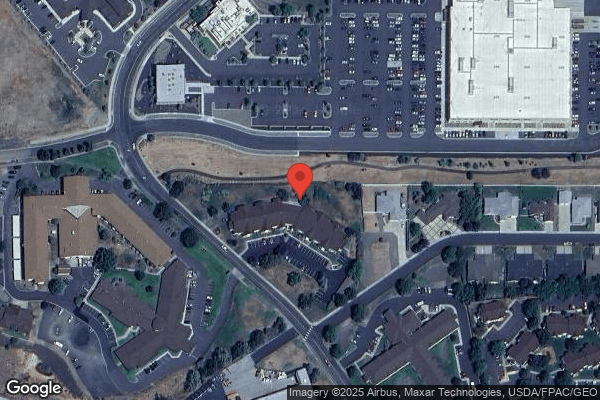
On 7/23/21 at 11:45 AM, Resident #12's family member stated when Resident #12 left the facility her alarm was not working. She stated Resident #12 walked to a business complex near 21st Street and stated it was at least 1 to 2 miles from the facility. Resident #12's family member stated a couple picked her up in that area and dropped her off at her husband's house. The family member stated Resident #12's husband called the facility and notified them she was gone.
The TAR for May 2021 documented Resident #12 was to be observed hourly and to document in a progress note what she was doing, any behaviors, and any interventions, beginning on 4/29/21 at 5:00 PM.
Nursing progress notes from 4/29/21 at 6:21 PM to 4/30/21 at 6:03 AM, included hourly documentation of Resident #12. There was no hourly documentation in the progress notes from 6:03 AM to 7:03 PM on 4/30/21 (13 hours). Hourly documentation in the progress notes resumed on 4/30/21 at 7:03 PM and continued through 5/4/21 at 6:18 PM. After that time, the documentation was not every hour on a consistent basis.
A nursing progress note, dated 5/7/21 at 1:28 PM, documented Resident #12 attempted to exit the facility but was redirected.
A nursing progress note, dated 5/18/21 at 6:56 PM, documented Resident #12 attempted to exit the facility to go home at dinner but was redirected.
The TAR for June 2021 documented Resident #12 was to be observed hourly and to document in a progress note what she was doing, any behaviors, and any interventions. The TAR also directed staff to check on Resident #12 once a shift.
A nursing progress note, dated 6/30/21 at 5:44 PM, documented Resident #12 had increased exit seeking behavior and she was convinced she needed to go home. The note documented Resident #12 became agitated with staff .redirecting her to alternative options like her mail and going to her room.
A nursing progress note, dated 7/1/21 at 9:02 PM, documented Resident #12 exited the facility after dinner and was redirected by staff back into the facility.
A nursing progress note, dated 7/16/21 at 1:10 PM, documented Resident #12 was walking down the hallway toward the exit door. Resident #12 did not respond when the nurse called her name, and she exited the building. The MDS nurse followed Resident#12 and asked her what she was doing. Resident #12 stated she was going .to jump of [sic] the cliff.
The facility was situated on a hill with an approximate 50-foot drop 10 yards from the hallway exit door Resident #12 opened to leave the facility. There was no fencing around the drop, and the hillside had medium sized rocks along the exposed side.
The clinical alerts listing report, documented on 7/16/21 at 3:07 PM, stated Resident #12 was put on alert charting and documented staff were to monitor Resident #12 for wandering and encouraged line-of-sight monitoring by staff when she was not with her family or sleeping. There was no documentation that line-of-sight observation was implemented or occurred.
On 7/23/21 at 9:50 AM, Resident #12 stated she felt sad every day, throughout the day, for several months. When asked if anyone had asked her how she was feeling or if she was feeling sad, she stated only her husband had asked.
On 7/23/21 at 3:14 PM, CNA #1 was interviewed regarding line-of-sight monitoring. CNA #1 stated the staff must always have an eye on the resident, and they must always be within staff's visual field. CNA #1 stated you cannot do line-of-sight observations while walking up and down the hallway and periodically looking into the room at the resident. When asked if any residents were on line-of-sight monitoring in the facility, CNA #1 stated no.
On 7/23/21 at 3:20 PM, CNA #2 was interviewed regarding line-of-sight monitoring. CNA #2 stated that line-of-sight monitoring was like one-on-one monitoring. When asked if walking in the hallway and looking into a room to check a resident would be line-of-sight monitoring CNA #2 stated no. When asked if any residents in the facility were on line-of-sight monitoring, CNA #2 stated she did not know.
On 7/22/21 at 5:38 PM, DDCO documented on the surveyor document request form the facility's change of condition policy was standard of practice and the facility did not have a line-of-sight procedure or policy.
On 7/23/21 at 10:00 AM, LPN #1 was asked to describe what was being monitored on Resident #12's alert charting. LPN #1 stated she was new, and she did not know.
On 7/23/21 at 10:15 AM, RN #1 stated the facility has five exits and the wander guard only alarmed on the hallway the resident exits out of. She stated staff on the other halls would not hear the wander guard alarm alert.
On 7/23/21 at 2:43 PM, the physician stated during a phone call he was not notified of Resident #12's elopement on 7/16/21.
On 7/23/21 at 5:42 PM, the DON stated line-of-sight supervision was when staff encouraged residents to stay within a specific area, so the nurse can always see them.
On 7/23/21 at 6:05 PM, the DON, with the RCN present, was asked about Resident #12's risk for elopement. The RCN interrupted the DON's answer and stated, She has an alarm, and staff were alerted, that is my answer.
This failed practice placed Resident #12 at risk for serious harm, impairment, or death.
On 7/23/21 at 7:58 PM, the Administrator, DON, and RCN were verbally informed and provided written notification of the Immediate Jeopardy determination at F689.
The Immediate Jeopardy was not removed prior to the survey exit on 7/24/21.
2. The facility's policy for Fall Evaluation (Morse Scale) and Management, updated March 2018, documented the following:
* A licensed nurse was to complete the Morse Scale fall evaluation on admission. If the total Morse scale score was greater than 45, the resident was considered as having a high potential for falls.
* A licensed nurse completed re-evaluations with each fall and significant change in condition.
* After the resident has been evaluated and cared for and appropriate notifications have been made, the licensed nurse (LN) would evaluate the resident's neurological status and monitor the resident for seventy-two hours after unwitnessed fall or falls that involved the resident's head striking a surface. The LN would update the Morse Scale, complete orthostatic vital signs, a progress note, a brief summary of the fall, the nursing evaluation, actions taken, who was notified, and the resident's condition. The LN would review and update the care plan with newly identified interventions as needed.
This policy was not followed.
Resident #6 was admitted to the facility on [DATE], with multiple diagnoses, including monoplegia (paralysis that impacts one limb) of the left leg, dementia, and anxiety disorder.
The admission Morse Fall scale assessment dated [DATE], documented Resident #6 was at high risk for falls.
Resident #6's care plan for fall risk, initiated on 4/15/21, documented staff were to anticipate and meet his needs, ensure his call light was within reach and encourage him to use it, ensure he was wearing appropriate footwear when ambulating, keep him in line-of-sight with frequent checks, and anticipate his toileting needs. The care plan did not specify what was meant by line-of-sight and frequent checks.
An admission MDS assessment. dated 4/21/21, documented Resident #6 was cognitively intact and required extensive assistance of one to two staff members for all daily care. He used a wheelchair for locomotion and had a history of falls prior to admission and in the facility.
A quarterly MDS assessment, dated 7/9/21, documented Resident #6's mental status had declined from cognitively intact to severely cognitive impaired.
A progress note, dated 4/13/21 at 1:42 PM, documented Resident #6, At this time resident has nearly fallen six times if not more. Therapy has been assisting as much as they can in monitoring him as he is requiring constant supervision and reminding for his safety.
Resident #6 had eleven falls in three months from 4/17/21 to 7/17/21, 9 unwitnessed falls and 2 witnessed falls. Resident #6 sustained injuries from 3 of the falls, 6/20/21, 7/3/21, and 7/17/21. Examples include:
a. An I&A report, dated 4/17/21 at 10:30 AM, and a nurse progress note dated 4/17/21 at 1:12 PM, documented Resident #6 had an unwitnessed fall. He was found seated between his wheelchair and bed. Resident #6 was confused, oriented to self only. He had a 4 cm by 2 cm skin tear on the back of his right arm. Resident #6 was not able to give a description of what happened.
Resident #6's care plan for fall risk was revised on 4/19/21, and the following interventions were added:
* Vital signs per center policy. Take blood pressure lying /sitting/ standing one time in the first 24 hours. Initiated on 4/19/21.
* Provide activities that promote exercise and strength building when possible. Provide one on one activity if bed bound. Initiated on 4/19/21.
* Offer to lay down or rest in recliner between meals. Initiated on 4/19/21.
The I&A report included an IDT review note, dated 4/22/21, which documented the root cause of the fall was Resident #6's poor safety awareness and impulsive behavior as he appeared to have fallen trying to transfer to bed. The IDT note documented the intervention developed to decrease his risk of falls was to offer assistance to bed or a recliner between meals.
b. An I&A report, dated 4/20/21 at 10:39 AM, and a nurse progress note dated 4/20/21 at 10:49 AM, documented Resident #6 had an unwitnessed fall. He was found on the floor beside his bed. His wheelchair was next to the head of the bed and the brakes were not locked on his wheelchair.
The I&A report included an IDT review note, dated 4/23/21, which documented the root cause of the fall was Resident #6's poor safety awareness and impulsive behavior. New interventions were to apply an anti-roll back device to his wheelchair and continue with the previous interventions for his fall risk care plan.
Resident #6's fall risk care plan was revised to include a new intervention for Antirollback [sic] to be added to W/C [wheelchair] when available, initiated on 4/26/21.
c. An I&A report, dated 5/3/21 at 2:15 PM, and a nurse progress note dated 5/2/21 at 2:02 PM, documented Resident #6 had an unwitnessed fall. He was found on the floor with his buttocks facing the wheelchair and his bed. His wheelchair brakes were locked. Resident #6 said, I think I bumped the side of my head.
The I&A report included an IDT fall review note, dated 5/8/21, which documented the root cause of the fall was Resident #6's poor safety awareness, overestimating his own abilities, and weakness. The intervention to decrease Resident #6's falls was to check orthostatic blood pressure (a condition in which your blood quickly drops when you stand up from a sitting or lying position which may cause dizziness and fainting) for 3 days and to check his blood pressure and heart rate 4 times a day for 3 days to monitor for trends.
Resident #6's fall risk care plan was revised, on 5/3/21, to include the following new interventions:
* When the resident gets restless, offer food and fluids. Offer bathroom. Check to see if resident has any pain. Offer diversional activities.
* Follows the 4 R's:
- Relieve-ask about pain during the visit. Is anything needed to relieve pain?
- Reposition.
- Restroom, assist the resident to the restroom if needed.
- Reach, verify resident's items are within reach.
Resident #6's care plan was also revised to include a new intervention for drug regimen review related to the fall on 5/2/21, initiated on 5/7/21.
d. An I&A report, dated 5/15/21 at 3:00 PM, and a nurse progress note dated 5/15/21 at 4:39 PM, documented Resident #6 had an unwitnessed fall. He was found on the floor next to his bed with his back against the side of the bed, next to his wheelchair. Resident #6 was unable to describe what happened and was confused. Resident #6 had socks on with no shoes.
The I&A report included an IDT fall review note, dated 5/19/21, which documented the cause of the fall was related to Resident #6 removing his shoes and having poor safety awareness. The intervention to decrease Resident #6's fall risk was for non-skid socks to be worn while out of bed.
Resident #6's fall risk care plan was revised to include the new intervention for non-skid socks to be worn with his shoes when he was out of bed, initiated on 5/19/21.
e. An I&A report, dated 5/24/21 at 10:51 PM, and a nurse progress note dated 5/24/21 at 11:24 PM, documented Resident #6 had a witnessed fall of sliding off the bed.
The I&A report included an IDT fall review note, dated 5/25/21, which documented the fall occurred related to Resident #6's impulsive behavior and lack of safety awareness. A diagnosis of overreactive bladder was added as a contributing factor.
Resident #6's fall risk care plan was revised to include the new intervention for a 72-hour one-on-one (1:1) time study, initiated on 5/25/21. The care plan did not specify what was meant by a 1:1 time study.
f. An I&A report, dated 5/30/21 at 1:13 PM, and a nurse progress note dated 5/30/21 at 1:21 PM, documented Resident #6 had an unwitnessed fall. He was sitting on the floor by the end of his bed, approximately two feet in front of his wheelchair. He said, I was going to take that plate and this cup out of my room.
The I&A report included an IDT fall review note, dated 6/3/21, which documented the fall occurred related to Resident #6's attempt to self-transfer and his poor safety awareness. The new intervention was for 1:1 staffing to further track his behaviors and try to identify patterns or fall triggers.
Resident #6's fall risk care plan was revised to include the new intervention of pick up dishes after resident finishes meals and pick up clutter, initiated on 6/3/21.
g. An I&A report, dated 6/7/21 at 12:20 PM, and a nurse progress note dated 6/7/21 at 12:29 PM, documented Resident #6 had an unwitnessed fall. He was lying on the floor by the staff bathroom without his wheelchair.
The I&A report included an IDT fall review note, dated 6/10/21, which documented the root cause of the fall was Resident #6's poor safety awareness and impulsive behavior. The intervention to decrease Resident #6's falls was to conduct an incontinence evaluation to assess if toileting would benefit him and decrease his impulsive behavior.
Resident #6's fall risk care plan did not include new interventions.
h. An I&A report, dated 6/18/21, and a nurse progress note dated 6/17/21 at 2:42 AM, documented Resident #6 had an unwitnessed fall. He was found sitting on the floor in his bathroom and he was confused.
The I&A report included an IDT fall review note, dated 6/18/21, which documented the root cause of Resident #6's fall was lack of awareness regarding safety limitations. The plan to decrease Resident #6's risk for falling was ongoing education, frequent checks, and staff would keep him in eyesight at all times.
Resident #6's fall risk care plan was revised to include new interventions, as follows:
* Do not leave the resident alone in the bathroom, initiated on 6/17/21.
* For no apparent acute injury, determine and address causative factors of the fall, initiated on 6/18/21.
i. An I&A report, dated 6/20/21 at 5:58 PM, and a nurse progress note dated 6/20/21 at 6:36 PM, documented Resident #6 had an unwitnessed fall. He was found lying next to his shoes on the floor in his bathroom with a 4 cm cut to the side of his head. Resident #6 continued to attempt self-transfers several times before being redirected to his evening meal. The family requested the resident be sent to the emergency room (ER) for evaluation.
A progress note, dated 6/20/21 at 6:59 PM, documented Resident #6's family declined to send him to the ER after talking with paramedics who stated the ER would not do anything for Resident #6. The note documented the wound on Resident #6's head was a cut that was no longer bleeding.
The I&A report included an IDT fall review note, dated 6/22/21, which documented the root cause of the fall was Resident #6 was unaware of safety limitations. The intervention to prevent Resident #6's falling was to request a care conference related to the need for placement in a private facility with less stimulation, continue 1:1 resident in staff eyesight until accommodations are met related to safety. The review note also documented ongoing education was to continue with Resident #6 related to weakness and the need for one person to assist him with all transfers.
Resident #6's fall risk care plan had a revised intervention to keep him in-line of sight as able, continue frequent checks, and anticipate toileting needs, initiated on 4/15/21 and revised on 6/22/21.
j. An I&A report, dated 7/4/21 at 10:45 AM, and a nurse progress note dated 7/3/21 at 10:46 AM, documented Resident #6 had a witnessed fall. He had attempted to reach the newspaper on the nursing station counter and lost his balance. He was noted to have two cuts, one on his right temple area and the other on his right cheek, a small skin tear to his right wrist, and some bruising to both of his arms.
A progress note, dated 7/3/21 at 11:10 AM, documented Resident #6 was sent to the hospital for an evaluation.
The I&A report included an IDT fall review note, dated 7/4/21, which documented the facility would continue to monitor Resident #6, keeping him within vision of staff and continue with discharge planning.
Resident #6's care plan did not include new interventions.
Resident # 6's record included an In-service Education Summary, dated 7/3/21, which documented the topic and content was Resident #6 was to be in line-of-sight at all times. A nurse or CNA needed to be with him at all times for his safety. Staff were to encourage Resident #6 to relax and rest in a recliner in the day room, so he remained in line-of-sight of staff at all times.
k. An I&A report, dated 7/18/21 at 12:49 AM, and a nurse progress note dated 7/17/21 at 13:28 AM, documented Resident #6 had a witnessed fall. It documented Resident #6 was sitting in his wheelchair by the nurse's station, attempted to pick up a bag of crackers off the floor, and fell out of his wheelchair. He landed on the floor and hit his right temple, shoulder, and hip. His laceration on his right temple from the prior fall incident on 7/3/21 reopened and grew to 4 cm by 0.2 cm.
The I&A report included an IDT fall review note, dated 7/19/21, which documented the root cause of the fall was Resident #6 was unaware of safety limitations, was confused, and education was not effective because of his memory and confusion. The plan to prevent Resident #6's falls was to continue to ask family for assistance throughout the day and encourage resident to participate in daily activities.
Resident #6's care plan for fall risk was revised on 7/19/21. There were no new interventions documented on his care plan but two interventions, initiated on 5/25/21 and 6/3/21, were revised. The two interventions were a 72 hour 1:1 time study and to keep him in line-of-sight, continue frequent checks, and anticipate his toileting needs.
The care plan did not specify what was meant by line-of-sight, frequent checks, and what the time study involved.
On 7/23/21 at 5:35 PM, the DON stated Resident #6 had multiple falls because he had no safety awareness. The intervention was keep him in line-of-sight at all times and Staff to encourage him to participate in activities. When asked how staff knew who was responsible for keeping Resident #6 in line-of-sight at all times, the DON said they had a staff in-service and alert charting to remind everyone.
The facility did not provide the staff supervision necessary to protect Resident #6 from repeated falls.
Based on observation, record review, family interview, and staff interview, it was determined the facility failed to ensure adequate supervision was provided to meet resident needs to prevent elopement and falls. This was true for 2 of 6 residents (#6 and #12) reviewed for supervision and accidents. The facility's failure to implement and maintain supervision measures to prevent elopement placed Resident #12, and other residents who were at risk for elopement, in immediate jeopardy of serious harm, impairment, or death. Findings include:
1. Resident #12 was admitted to the facility 11/12/20, with multiple diagnoses including dementia and depression.
Resident #12's quarterly MDS assessment, dated 5/3/21, documented she was severely cognitively impaired and walked with a walker.
A nursing progress note, dated 12/21/20 at 5:42 PM, documented Resident #12 had exited the building at 5:00 PM and walked over to the assisted living building, on the same property. The note documented Resident #12 did not have injuries. The note documented Resident #12's family member and the physician were notified, and an order was received to place a wander guard bracelet on Resident #12's wrist, which it was.
The TAR for Resident #12 documented to check the site and the function of her wander guard every shift, beginning on 12/21/20.
Resident #12's care plan for elopement risk documented the following interventions:
*Distract Resident from wandering, initiated on 12/22/20.
*Identify the pattern of Resident #12's wandering, initiated on 12/22/20.
*Provide structured activities, initiated on 12/22/20.
*Apply wander guard to wrist and check every shirt and as needed to ensure it was in place and monitor for proper functioning, initiated on 12/23/20.
*Offer to walk with resident when she becomes restless, initiated on 12/23/20.
A social services progress note, dated 12/24/20 at 10:43 AM, documented a care conference was held with Resident #12's family to discuss her wandering. The note documented if Resident #12 continued to wander they may need to look for a dementia unit for her. The note documented her family agreed.
A nursing note, dated 3/24/21 at 3:20 PM, documented Resident #12 attempted to exit from the front door and her wander guard alarm sounded. The note documented Resident #12 was confused and was able to be redirected.
A nursing progress note, dated 4/7/21 at 3:38 PM, documented Resident #12 had left the facility with family for an outing and her wander guard did not alarm. The note documented the wander guard was going to be assessed upon Resident #12's return.
A nursing progress note, dated 4/8/21 at 1:21 PM, documented Resident #12 was .wandering around more today . and her wander guard was not working. The note documented management was aware Resident #12's wander guard was not working and were attempting to locate .a new band for her new wander guard.
Progress notes documented Resident #12 was not wearing her wander guard bracelet on 4/9/21 at 10:17 AM and 4/11/21 at 2:38 PM, 2:39 PM, and 2:56 PM. Resident #12's wander guard was not functioning and/or worn for 4 days.
A nursing progress note, dated 4/11/21 at 6:21 PM, documented Resident #12 was up and roaming around facility more than before. The note documented Resident #12 did not have her wander guard on and the oncoming nurse was notified.
Progress notes documented Resident #12 was not wearing her wander guard bracelet on 4/12/21 at 2:10 AM and 12:54 PM.
A social services progress note, dated 4/20/21 at 5:58 PM, documented staff reported to the Social Services Director Resident #12 was displaying increased behavior of eloping/wandering and increased signs and symptoms of depression. The note documented behavior monitoring was in place and the Social Service Director was going to speak with Resident #12 the following day. The next note by the Social Services Director was on 4/30/21, 10 days later, which documented she had left a message with Resident #12's family member to set up a care conference.
A nursing progress note, dated 4/25/21 at 6:02 PM, documented Resident #12 made several attempts to leave the building stating she needed to go home. The note documented she was redirected by staff.
A nursing progress note, dated 4/27/21 at 7:41 PM, documented Resident #12 made several attempts to leave the building stating she needed to go home. The note documented she was redirected by staff.
A nursing progress note, dated 4/29/21 at 11:25 AM, documented Resident #12 had gathered some personal belongings and was attempting to leave the building. The note documented she was redirected by staff.
A nursing progress note, dated 4/29/21 at 2:17 PM, documented a call was received from Resident #12's husband and he stated she was at their house. The note documented her husband stated Resident #12 was wearing the wander guard. The note documented staff had reported Resident #12 was attempting to exit the facility at approximately 10:30 AM and she was with a staff one-on-one until .[TRUNCATED]
CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0740
(Tag F0740)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review, staff interview, and resident interview, it was determined the facility failed to ensure ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review, staff interview, and resident interview, it was determined the facility failed to ensure a resident was provided with behavioral health care services to maintain her highest practicable physical, mental, and psychosocial well-being consistent with her needs. This was true for 1 of 4 residents (Resident #12) reviewed for behavioral health. The health and safety of all residents residing in the facility were placed in immediate jeopardy when a) Resident #12 was at risk of suicide and ongoing elopement due to inadequate behavioral health services and b) the other 43 residents residing in the facility were at risk of experiencing isolation and compromised physical and psychosocial well-being related to a lack of preventing, relieving, and/or accommodating a resident's psychological distress. Findings include:
Resident #12 was admitted to the facility on [DATE] with multiple diagnoses, including dementia and depression.
The facility's policy for behavior management, updated 1/19, documented new or increased behaviors were communicated to the IDT team. It documented the IDT team reviewed the resident's record, behavior monitoring flow sheet, and evaluated the effectiveness of the current plan. The IDT team would note the effectiveness of interventions in the medical record and if further evaluation was needed, new interventions would be implemented.
This policy was not followed.
On 5/3/21, Resident #12's quarterly Minimum Data Set (MDS) assessment documented Resident #12 was severely cognitively impaired and walked with a walker.
The Idaho Preadmission screening and resident review (PASARR), dated 11/12/20, documented Resident #12 had a history of a suicide attempt and suicidal talk and ideas. It stated she received mental health services on 12/9/19 and had a suicide attempt or gesture on 3/16/20.
On 7/15/20, a neuropsychological evaluation documented Resident #12 was hospitalized in a psychiatric facility in January 2000 due to increased depression, anxiety and suicidal ideation. The discharge recommendation from her psychologist regarding treatment and follow-up care documented Resident #12 should have regular supervision throughout the day and should not be left alone for extended periods of time. It documented Resident #12 should be seen for a psychiatric follow-up evaluation to monitor further cognitive decline and update treatment/supervision recommendations as needed.
Resident #12's care plan initiated on 12/22/20 documented no interventions for suicidal risk monitoring, elopement, or behavioral health services.
On 6/29/21 at 12:21 PM, a progress note documented an appointment request was filled out for Resident #12 to see a mental health provider. There was no documentation in Resident #12 record that she was seen by a mental health provider after the appointment request was filled out.
On 7/16/21 at 1:10 PM, a progress note documented Resident #12 was walking down the oak hallway toward the oak hallway exit door. She did not respond when the nurse called her name, and she exited the building. The MDS nurse followed the resident and asked her what she was doing. Resident #12 stated she was going to jump off the cliff.
The facility was situated on a hill with an approximate 50-foot drop 10 yards from the oak hallway exit door. There is no fencing around the drop, and the hillside has medium sized rocks along the exposed side.
On 7/16/21 at 3:09 PM, Resident #12 was put on alert charting which documented staff were to monitor Resident #12 for wandering and encourage line-of-sight monitoring by staff when she was not with her family or sleeping. Resident#12's alert charting also directed staff to monitor her for depression and self-harm acts. There was no documentation in Resident #12's record the physician was notified related to her statement she was going to jump off the cliff.
Resident #12's record did not include behavioral monitor flowsheets for suicidal behaviors, triggers, interventions, or outcome. Resident #12's depression behavioral monitor flowsheets documented no for any depressive symptoms for May-July 2021.
On 7/23/21 at 3:14 PM, CNA #1 was interviewed regarding what line-of-sight care. He/she stated that you must always have an eye on the patient, and they must always be within your visual field. He/she stated you cannot do line-of-sight observations while walking up and down the hallway and periodically looking into the room at the resident. When asked if any residents were on line-of-sight care in the facility, he/she stated no.
On 7/23/21 at 3:20 PM, CNA #2 was interviewed regarding line-of-sight care. He/she stated that line of sight care was like 1-on-1 services. When asked if walking in the hallway and looking into a room to check a resident would be line-of-sight care he/she stated no. When asked if any residents in the facility were on line-of-sight care he/she stated he/she didn't know.
On 7/22/21 at 5:38 PM, the lead Divisional Director of Clinical Operations (DDCO) was asked for the suicide precaution policy. On the surveyor document request form, she documented the facility did not have one and wrote call 911 beside the request. She documented the facility change of condition policy was standard of practice and the facility had no line -of -sight procedure or policy.
On 7/23/21 at 9:50 AM, Resident #12 stated she felt sad every day, throughout the day, for several months. When asked if she had been offered psychiatric services she stated No, but I hope they will because it would help. When asked if anyone had asked her how she was feeling or if she was feeling sad, she stated only her husband had asked.
On 7/23/21 at 10:00 AM, LPN #1 was asked to describe what was being monitored on Resident #12's alert charting. LPN #1 stated she was new, and she did not know but she would print it and find out.
On 7/23/21 at 2:43 PM, the physician stated in a phone call with a surveyor he was not notified of Resident #12's suicidal elopement or her statement of her intent to jump off the cliff on 7/16/21.
On 7/23/21 at 5:50 PM, the Regional Clinical Nurse (RCN) was asked if she was aware Resident #12 recently had suicidal thoughts, she stated what is documented in the chart is she wanted to jump off a cliff. When asked if she was aware Resident #12 had a suicide attempt and it was documented on the PASRR I, she stated she could not find it. When a copy of the PASSAR I was given to her with the highlighted information regarding Resident #12's suicidal history, she stated So, I'm looking and I'm not seeing it. I can't find the form you have.
On 7/23/21 at 6:05 PM, the DON stated when residents have suicidal thoughts, staff would monitor that resident, or they would send them to the emergency department. She stated she based suicidal evaluation and interventions on risk, and she would assess a resident's risk related to elopement and suicide or send the resident to the ER for evaluation. When asked what Resident #12's risk was for suicidality and elopement, the RCN interrupted the DON's answer and stated, She has an alarm, and staff were alerted, that is my answer.
The facility did not provide Resident #12 necessary behavioral health care and services and placed Resident #12 at risk for serious harm, impairment, or death.
On 7/23/21 at 7:58 PM, the Administrator, DON, and RCN were notified verbally and in writing of the Immediate Jeopardy to residents' health and safety.
The IJ was unable to be removed by the survey team prior to the end of survey on 7/24/21.
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
ADL Care
(Tag F0677)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, resident representative interview, and resident and staff interview, it was determined the facility fail...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, resident representative interview, and resident and staff interview, it was determined the facility failed to ensure residents were provided with bathing and oral care consistent with their needs. This was true for 6 of 12 residents (#3, #12, #20, #32, #37, and #39) reviewed for ADLs. This failure caused psychosocial harm to Resident #39 when she experienced embarrassment her showers were not given and created the potential for other residents to experience embarrassment, isolation, decreased sense of self-worth, skin impairment, and compromised physical and psychosocial well-being. Findings include:
1. Residents did not receive showers and/or baths following their care plan. Examples include:
a. Resident #39 was admitted to the facility on [DATE], with multiple diagnoses including
urinary tract infection and the need for assistance with personal care.
The admission MDS assessment, dated 6/28/21, documented Resident #39 was cognitively intact and she required extensive assistance of one staff member for bathing.
The facility's shower schedule documented Resident #39's shower day was each Monday and Thursday.
Resident #39's Bathing/Bed Bath documentation report for June 2021 and July 2021, documented the following:
* Resident #39 received a shower on 7/1/21, 6 days after her admission on [DATE].
* Resident #39 received a shower on 7/8/21, 7 days after her last shower.
* Resident #39 received a shower on 7/15/21, 7 days after her last shower.
Resident #39's record documented 3 showers from the time of her admission on [DATE] to her discharge on [DATE], a total of 25 days.
On 7/19/21 at 4:36 PM, Resident #39 said she had been at the facility 3 weeks and was discharging tomorrow. Resident #39 stated I have been here 3 weeks and received 2 showers, 1 shower was offered by the staff and the other was requested by her. Resident #39 said I felt embarrassed because I was not smelling good. I told the staff 'Lord, I really need a shower!' Resident #39 said she told staff about 2 to 3 times a week she needed a shower and staff pretended not to hear her. Resident #39 stated the lack of showers affected her life and It made me feel bad.
Resident #39's showers were not provided per her preference.
b. Resident #37 was admitted on [DATE], with diagnoses which included multiple sclerosis (a potentially disabling disease of the brain and spinal cord) and quadriplegia (paralysis of both arms and legs).
An admission MDS assessment, dated 12/22/20, documented Resident #37 required the assistance of 2 or more staff for bathing and was totally dependent on staff for all ADLs.
Resident #37's care plan, dated 12/15/20, documented he would be bathed 3 times a week on night shift on Monday, Wednesday, and Friday. The care plan also documented Resident #37 preferred bathing in the morning but was willing to be bathed at night, and currently was to have only bed baths, revised 5/3/21.
Resident #37's Bathing/Bed bath documentation reports for June 2021 and July 2021 documented the following:
* Resident #37 received a bed bath on 6/2/21 his next documented bed bath was on 6/22/21, 20 days later. Resident #37 received 2 bed baths from 6/1/21 to 6/30/21, 30 days.
* Resident #37 received a bed bath on 7/8/21, 12 days after his last bed bath on 6/30/21.
* Resident #37 received a bed bath on 7/15/21, 7 days after his previous bath on 7/8/21.
On 7/23/21 at 6:13 PM, the RCN reviewed Resident #37's record and said she saw that Resident #37 did not get bed baths as care planned. The RCN stated if a resident refused, the shower aides should offer a shower again at a more convenient time.
Resident #37's bed baths were not provided per his care plan.
c. Resident #12 was admitted to the facility on [DATE], with multiple diagnoses including dementia and depression.
A quarterly MDS assessment, dated 5/3/21, documented Resident #12 was severely cognitively impaired, used a walker, and she required supervision and limited assistance of one staff member for all daily care.
Resident #12's care plan, initiated on 11/12/20, documented she would be bathed 2 to 3 times a week. The care plan documented Resident #12 was to be provided showers per the shower schedule.
The facility's shower schedule documented Resident #12's shower days were on Wednesday and Saturday.
Resident #12's Bathing/Bed Bath documentation reports for May 2021, June 2021, and July 2021, documented the following:
* Resident #12 did not have a shower from 5/1/21 to 5/10/21, 9 days.
* Resident #12 received a shower on 5/13/21 and her next shower was on 5/18/21, 5 days later. There was no documentation she refused showers during the 5 days.
* Resident #12 received a shower on 5/26/21, 8 days after her last shower. The report documented Resident #12 refused showers on 5/21/21 and 5/25/21. There was no documentation she was re-approached and offered a shower after her refusals.
* Resident #12 received a shower on 6/8/21, 7 days after her last shower.
* Resident #12 received a shower on 6/22/21, 14 days after her last shower. The report documented she refused a shower on 6/18/21, 10 days after her last shower. There was no documentation she was re-approached and offered a shower after her refusals.
* Resident #12 received a shower on 7/20/21, 27 days after her last shower. The report documented she refused a shower on 6/29/21, 7 days after her last shower. There was no documentation she was re-approached and offered a shower after her refusal and over the next 20 days.
Resident #12's showers were not provided per her care plan.
d. Resident #3 was readmitted to the facility on [DATE], with diagnoses including bipolar disorder with psychotic features (a mental disorder that causes unusual shifts in mood, energy, activity levels, concentration, and the ability to carry out day-to-day tasks), diabetes mellitus, and high blood pressure.
Resident #3's care plan documented she required extensive assistance of 1 staff with showering.
Resident #3's Bathing/Bed Bath documentation reports for May 2021, June 2021, and July 2021, documented the following:
* Resident #3 received a shower on 5/14/21, 10 days after her last shower.
* Resident #3 received a shower on 5/25/21, 11 days after her last shower on 5/14/21.
* Resident #3 received a shower on 6/11/21, 10 days after her last shower on 6/1/21.
* Resident #3 received a shower on 6/22/21, 6 days after her last shower on 6/16/21.
* Resident #3 received a shower 7/13/21, 6 days after her last shower on 7/7/21.
* Resident #3 received a shower on 7/20/21, 6 days after her last shower on 7/13/21.
Resident #3's Bathing/Bed Bath reports for May 2021, June 2021, and July 2021 documented she refused a shower once on 6/25/21. There was no further documentation of refusals and/or that she was re-approached for showers.
e. Resident #20 was admitted to the facility on [DATE] and readmitted on [DATE], with diagnoses which included diabetes mellitus, dementia, and depression.
Resident #20's care plan, dated 9/4/20, documented he required extensive assistance of 1 staff with showering, and showers were to be completed per the facility's showering schedule and as needed.
Resident #20's Bathing/Bed Bath reports for May 2021, June 2021, and July 2021, documented the following:
* Resident #20 received a shower on 5/11/21 for May 2021. The report documented he refused a shower on 5/12/21, 5/18/21, and 5/27/21. No additional showers were documented as offered or completed from 5/12/21 to 5/31/21, 20 days.
* Resident #20 did not receive a shower in June 2021. The report documented he refused a shower on 6/2/21, 6/9/21, 6/11/21, 6/15/21, 6/16/21, 6/22/21, and 6/24/21. There was no additional documentation Resident #20 was re-approached and/or offered a shower between the dates of his refusals.
On 7/22/21 at 11:26 AM, CNA #3 was asked about personal cares for Resident #20. She stated the facility did not have enough staff for the morning cares of residents. She stated due to not enough staff, CNA's were prioritizing assisting residents with toileting.
On 7/23/21 at 5:42 PM, the DON, with the RCN present, was asked about Resident #20's missed showers. The RCN stated it was a documentation issue.
Resident #20 did not receive showers per his care plan.
On 7/23/21 at 6:13 PM, the RCN stated shower aides were scheduled to work from 6:00 AM to 2:00 PM and from 2:00 PM to 8:00 PM. She stated shower aides were pulled off shower duty to work as CNAs on the floor. The RCN stated the charge nurse on the floor was responsible for coordinating showers among CNAs and the licensed nurses.
2. Resident #32 was admitted to the facility on [DATE], with multiple diagnoses including dementia with behavioral disturbance, stroke, and heart disease.
Resident #32's quarterly MDS assessment, dated 6/21/21, documented Resident #32 was severely cognitively impaired and required extensive assistance with personal hygiene (which included shaving, applying makeup, combing hair, etc.).
Resident #32's care plan documented she required extensive assistance by 1 staff for personal hygiene.
On 7/21/21 at 4:45 PM, Resident #32, a female, was observed in the common area with curling facial hair on her chin. Resident #32 stated she could not pluck her facial hair herself because she would pinch herself, but it was alright for the staff to pluck them.
The DON observed the discussion and stated Resident #32 had facial hair. She asked a CNA to pluck Resident #32's facial hair.
The facility did not provide personal grooming for Resident #32 as needed.
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, it was determined the facility failed to ensure residents received appropriate care ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, it was determined the facility failed to ensure residents received appropriate care to prevent and treat pressure ulcers. This was true for 2 of 4 residents (#37 and #630) reviewed for wounds. This deficient practice resulted in harm to Resident #37 and Resident #630 when they developed avoidable pressure ulcers in the facility. Findings include:
The National Pressure Injury Advisory Panel website, accessed on 7/28/21, defined pressure ulcer staging as follows:
Stage 1- Intact skin with a localized area of non-blanchable erythema (red discoloration of skin as a result of injury) which may appear differently in darkly pigmented skin. The presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes do not include purple or maroon discoloration; these may indicate a deep tissue pressure injury.
Stage 2 - Partial-thickness skin loss with exposed dermis (thick layer of living tissue below the epidermis which forms the true skin, containing blood capillaries, nerve endings, sweat glands, hair follicles, and other structures). The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Adipose (fat) is not visible, and deeper tissues are not visible. Granulation tissue (new connective tissue and microscopic blood vessels that form on the surfaces of a wound during the healing process), slough (non-viable yellow, tan, gray, green, or brown tissue), and eschar (dead or weakened tissue that is hard or soft in texture - usually black, brown, or tan in color) are not present. These injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel.
Stage 3 - Full-thickness loss of skin, in which adipose is visible in the ulcer and granulation tissue and epibole are often present. Slough and/or eschar may be visible. The depth of tissue damage varies by anatomical location; areas of significant adiposity can develop deep wounds. Undermining (when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound's edge) and tunneling (channels that extend from a wound into and through the tissue or muscle below) may occur. Fascia (thin casing of connective tissue that surrounds and holds every organ, blood vessel, bone, nerve fiber, and muscle in place), muscle, tendon, ligament, cartilage or bone is not exposed. If slough or eschar obscures the extent of tissue loss this is an Unstageable Pressure Injury.
The Lippincott Manual of Nursing Practice, 10th edition, pages 183-184, directed nurses to reposition residents every 2 hours to relieve pressure. The manual also listed risk factors for pressure ulcers, including malnourishment, edema (swelling caused by excess fluid trapped in the body's tissues), and immobility.
This guidance was not followed.
a. Resident #37 was admitted to the facility on [DATE], with multiple diagnoses including multiple sclerosis (a potentially disabling disease of the brain and spinal cord) and quadriplegia (paralysis of both arms and legs).
Resident #37's admission MDS assessment, dated 12/22/20, documented the following:
* He had no pressure ulcers on admission.
* He was at risk of developing pressure ulcers.
* He required extensive assistance with activities of daily living and required two plus staff assistance for bed mobility and transfers.
* He did not transition (move himself to change positions) or walk.
* He had impairment in his upper and lower extremities on both sides.
Resident #37's care plan, dated 12/14/20 and revised 4/6/21, documented he had the potential for pressure ulcer development related to decreased mobility, incontinence of bowel, skin frequently moist due to perspiration, and history of chronic non-healing pressure injuries. The care plan listed the goal was for Resident #37 to have intact skin, free of redness, blisters or discoloration, dated 12/15/20 and revised on 6/28/21. One of the interventions listed was Resident #37 was dependent on assistance for turning and repositioning and was to be turned/repositioned at least every 2 hours, and more often as needed or requested, initiated 12/15/20.
A hospital virtual visit (a face-to-face meeting with a health care professional using video technology without leaving the facility) report, dated 2/22/21, documented Resident #37 had a new Stage 3 pressure ulcer on each hip.
Resident #37's care conference report, dated 3/24/21, documented he was to be turned every 2 hours from side to side. The report stated staff were to document Resident #37's cares and turn schedule, and to notify the family if Resident #37 refused cares.
On 6/18/21, a care conference note documented Resident #37 was no longer able to be up in his chair in order to help heal his buttocks [pressure ulcer].
A virtual hospital report, dated 6/21/21, documented Resident #37 was having sacral (a triangular area in the lower back situated between the hipbones) decubitus (pressure) ulcer breakdown again. Resident #37's record did not include documentation as when the pressure ulcer originally developed after Resident #37 was admitted .
Resident #37's bed repositioning records from 6/24/21 through 7/14/21, documented he was not turned or repositioned every 2 hours or a total of 12 times during a 24-hour period as follows:
* Resident #37 was turned/repositioned 2 times on 7/4/21 and 7/13/21
* Resident #37 was turned/repositioned 3 times on 6/27/21, 6/28/21, 6/29/21, 7/1/21, 7/3/21, 7/6/21, 7/8/21, 7/11/21, and 7/14/21.
* Resident #37 was turned/repositioned 4 times on 7/5/21, 7/9/10, 7/10/21, and 7/12/21.
* Resident #37 was turned/repositioned 5 times on 6/24/21, 6/30/21, and 7/2/21.
* Resident #37 was turned/repositioned 6 times on 6/25/21, 6/26/21, and 7/7/21.
The length of time recorded between turing/repositioning of Resident #37 ranged from 2.5 hours (occurring twice) to 9 hours or more (17 times), and 18 hours (1 time).
On 7/20/21 at 11:35 AM, Resident #37 stated he was to be repositioned every hour, but it was not happening.
On 7/23/21 at 10:21 AM, the DON stated staff kept track of Resident #37's repositioning and refusals on the form hanging on the his door. The DON stated Resident #37's refusals and many of the dates were not documented on the form. The DON stated repositioning and refusals were not documented in the electronic record.
On 7/23/21 at 7:11 PM, when asked to review the repositioning documentation, the RCN stated there were lapses in Resident #37's repositioning. The RCN stated it was not documented Resident #37 was repositioned every 2 hours, or he refused repositioning.
b. Resident #630 was admitted to the facility on [DATE], with multiple diagnoses including urinary tract infection, bacteremia (bacteria in the blood), edema, moderate protein-calorie malnutrition, muscle weakness, and reduced mobility.
Resident #630's admission nursing evaluation, undated, documented Resident #630 had no pressure ulcers. The evaluation documented Resident #630 was an older adult and had edema in both lower extremities, which were both risk factors for pressure ulcers.
Resident #630's physician orders, dated 5/14/20, documented a weekly skin assessment was to be completed every Wednesday.
Resident #630's care plan, dated 5/15/20, documented Resident #630 was at high risk for skin impairment, and directed staff to turn Resident #630 every 2-3 hours.
Resident #630's skin integrity evaluation, dated 5/14/20, documented Resident #630 was at moderate risk for pressure ulcers, with the following risk factors:
* Her ability to walk was severely limited or nonexistent and she could not bear her own weight.
* She had a potential problem with skin friction or shear against sheets, chair, or other devices, and occasionally she slid down in her chair or bed.
Resident #630's pain evaluation, dated 5/27/20, documented she had pain at her tailbone when sitting and when laying, but she did not shift position in bed because her feet were elevated to decrease edema.
A weekly skin evaluation, completed on 5/27/20 (13 days after admission), documented Resident #630 had a 2 cm x 1.5 cm Stage 2 pressure ulcer on her sacrum.
Resident #630's ADL flowsheet from 5/14/20 through 6/6/20, documented she was not turned or repositioned every 2 to 3 hours as her care plan directed as follows:
* Resident #630 was turned/respositioned 1 time on 6/2/20 and 6/3/20.
* Resident #630 was turned/repositioned 2 times on 6/6/20.
* Resident #630 was turned/repositioned 3 times on 5/14/20, 5/15/20, 5/16/20, 5/17/20, and 5/31/20,
* Resident #630 was turned/repositioned 4 times on 5/26/20 and 6/1/20.
* Resident #630 was turned/repositioned 5 times on 5/19/20, 5/24/20, 5/27/20, 5/28/20, 5/29/20, 5/30/20, 6/4/20, and 6/5/20.
* Resident #630 was turned/repositioned 6 times on 5/25/20
* Resident #630 was turned/repositioned 7 times on 5/18/20, 5/20/20, 5/21/20, and 5/22/20
On 7/23/21 at 7:15 PM, the RCN said the facility's policy was to measure pressure wounds and start treatment upon discovery of the wound. When shown the ADL flowsheets, the RCN said Resident #630 was not repositioned every 2 hours, and she stated there was no documentation.
SERIOUS
(H)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0725
(Tag F0725)
A resident was harmed · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, Facility Assessment review, policy review, review of the Facility Assessment, review of I&A...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, Facility Assessment review, policy review, review of the Facility Assessment, review of I&A Reports, review of staffing schedules, and interviews with residents, family, and staff, it was determined the facility failed to ensure there were sufficient numbers of competent staff to meet supervision, ADL needs, medication administration, and answer call lights in a timely manner for residents. This was true for 16 of 22 residents (#2, #3, #6, #12, #20, #21, #25, #27, #29, #32, #35, #37, #38, #39, #141, and #630) reviewed for staffing concerns. This deficient practice caused residents physical harm from lack of sufficient staff when Resident #37 and Resident #630 developed pressure ulcers, Resident #6 had falls with injury, and Resident #39 had psychosocial harm due to embarrassment from lack of personal hygiene. This deficient practice also had the potential to effect the other 25 residents residing in the facility. Findings include:
The facility's Facility Assessment, 2021 stated, the facility provides services to residents who are one-person, two-person, and total assist. The assessment stated the Center has hired licensed staff and non-licensed staff to provide all the required services to the residents. The assessment also documented competencies for staff during the past year included but were not limited to:
* Person Centered Care
* Care of persons with Alzheimer's and Dementia
* Care of persons with mental/psychological disorders
* Skin Care
* Fall prevention
* Elopement
* Privacy and Dignity
* Bathing
The Facility Assessment was not followed.
1. Resident #12 was admitted to the facility 11/12/20 with multiple diagnoses including dementia and depression.
Resident #12's quarterly MDS assessment, dated 5/3/21, documented she was severely cognitively impaired and walked with a walker.
a. A nursing progress note, dated 12/21/20 at 5:42 PM, documented Resident #12 had exited the building at 5:00 PM and walked over to the assisted living building, on the same property. The note documented Resident #12 did not have injuries. The note documented Resident #12's family member and the physician were notified, and an order was received to place a wander guard bracelet on Resident #12's wrist.
A nursing progress note, dated 4/29/21 at 2:17 PM, documented a call was received from Resident #12's husband and he stated she was at their house. The note documented her husband stated Resident #12 was wearing the wander guard. The note documented staff had reported Resident #12 was attempting to exit the facility at approximately 10:30 AM and she was with a staff one-on-one until .she calmed down. The note documented Resident #12 was last seen by a nurse at approximately 11:30 AM. The note also documented Resident #12's husband stated he planned to bring her back to the facility after he visited with her.
An I&A report, dated and signed on 5/4/21, documented Resident #12 left the faciity on 4/29/21 without staff knowledge. The I&A report documented the facility became aware Resident #12 had left when her husband called the facility at 2:17 PM. Resident #12's husband reported she was at his home and her wander guard was in place on her wrist. The report documented the root cause of the elopement was due to Resident #12's poor safety awareness, confusion, and her missing family. The report documented the plan was to replace her wander guard bracelet and they ordered a transmitter to check the function of the wander guard device. The report also documented staff were to .complete routine visual checks on residents. Staff education provided.
It was unclear in the documentation from the facility the amount of time Resident #12 was away from the facility and without supervision.
On 7/23/21 at 11:45 AM, Resident #12's family member stated when she left the faciity on 4/29/21 her alarm was not working. She stated Resident #12 walked to a business complex near 21st Street and stated it was at least 1 to 2 miles . from the facility. Resident #12's family stated a couple picked her up in this area and dropped her off at her husband's house. The family member stated Resident #12's husband called the facility and notified them she was gone.
On 7/23/21 at 2:43 PM, the physician stated during a phone call he was not notified of Resident #12's elopement on 7/16/21.
On 7/23/21 at 6:05 PM, the DON, with the RCN present, was asked regarding Resident #12's risk for elopement, the RCN interrupted the DON's answer and stated, She has an alarm, and staff were alerted.
This failed practice placed Resident #12 at risk for serious harm, impairment, or death.
b. The Idaho Preadmission screening and resident review (PASARR), dated 11/12/20, documented Resident #12 had a history of a suicide attempt and suicidal talk and ideas. It stated she received mental health services on 12/9/19 and had a suicide attempt and/or gesture on 3/16/20.
On 7/15/20, a neuropsychological evaluation documented Resident #12 was hospitalized in a psychiatric facility in January 2020 due to increased depression, anxiety and suicidal ideation. The discharge recommendation from her psychologist regarding treatment and follow-up care documented Resident #12 should have regular supervision throughout the day and should not be left alone for extended periods of time. It documented Resident #12 should be seen for a psychiatric follow-up evaluation to monitor further cognitive decline and update treatment/supervision recommendations as needed.
Resident #12's care plan initiated on 12/22/20 documented no interventions for suicidal risk monitoring or behavioral health services.
On 6/29/21 at 12:21 PM, a progress note documented an appointment request was filled out for Resident #12 to see a mental health provider. There was no documentation in Resident #12's record that she was seen by a mental health provider after the appointment request was filled out.
On 7/16/21 at 1:10 PM, a progress note documented Resident #12 was walking down the oak hallway toward the exit. She did not respond when the nurse called her name, and she exited the building. The MDS nurse followed Resident #12 and asked her what she was doing, Resident #12 stated she was going to jump of [sic] the cliff.
The facility was situated on a hill with an approximate 50-foot drop 10 yards from the exit door. There was no fencing around the drop, and the hillside had medium sized rocks along the exposed side.
On 7/16/21 at 3:09 PM, Resident #12 was put on alert charting which documented staff were to monitor Resident #12 for wandering and encourage line-of-sight monitoring by staff when she was not with her family or sleeping. Resident#12's alert charting also directed staff to monitor her for depression and self-harm. There was no documentation in Resident #12's record the physician was notified related to her statement she was going to jump off the cliff.
Resident #12's record did not include behavioral monitoring for suicidal behaviors, triggers, interventions, or outcome. Resident #12's depression behavioral monitoring documented no for any depressive symptoms for May 2021 to July 2021.
On 7/23/21 at 3:14 PM, CNA #1 was interviewed regarding what line-of-sight care meant. CNA #1 stated that you must always have an eye on the patient, and they must always be within your visual field. CNA #1 stated you cannot do line-of-sight observations while walking up and down the hallway and periodically looking into the room at the resident. When asked if any residents were on line-of-sight care in the facility, CNA #1 stated no.
On 7/23/21 at 3:20 PM, CNA#2 was interviewed regarding line-of-sight care. CNA #2 stated that line-of-sight care was like 1-on-1 services. When asked if walking in the hallway and looking into a room to check a resident would be line-of-sight care CNA #2 stated no. When asked if any residents in the facility were on line-of-sight care CNA #2 stated she did not know.
On 7/22/21 at 5:38 PM, the lead DDCO was asked for the suicide precaution policy. On the document request form from the survey team, she documented the facility did not have one and wrote call 911 beside the request. She documented on the same form the facility had no line-of-sight procedure or policy.
On 7/23/21 at 9:50 AM, Resident #12 stated she felt sad every day, throughout the day, for several months. When asked if she had been offered psychiatric services she stated No, but I hope they will because it would help. When asked if anyone had asked her how she was feeling or if she was feeling sad, she stated only her husband had asked.
On 7/23/21 at 10:00 AM, LPN #1 was asked to describe what was being monitored on Resident #12's alert charting. LPN #1 stated she was new, and she did not know.
On 7/23/21 at 2:43 PM, the physician stated in a phone call he was not notified of Resident #12's suicidal elopement or her statement of her intent to jump off the cliff on 7/16/21.
On 7/23/21 at 5:50 PM, the RCN was asked if she was aware Resident #12 had a suicide attempt and it was documented on the PASRR I, she stated she could not find it. When a copy of the PASSAR I was given to her with the highlighted information regarding Resident #12's suicidal history, she stated So, I'm looking and I'm not seeing it. I can't find the form you have.
On 7/23/21 at 6:05 PM, the DON stated when residents have suicidal thoughts, staff would monitor that resident, or they would send them to the emergency department. She stated she based suicidal evaluation and interventions on risk, and she would assess a resident's risk related to elopement and suicide or send the resident to the ER for evaluation. When asked what Resident #12's risk was for suicidality and elopement, the RCN interrupted the DON's answer and stated, She has an alarm, and staff were alerted.
The facility did not provide Resident #12 necessary behavioral health care and services which placed Resident #12 at risk for serious harm, impairment, or death.
2. Residents were not turned and repositioned and subequently developed pressure ulcers.
The National Pressure Injury Advisory Panel website, accessed on 7/28/21, defined pressure ulcer staging as follows:
Stage 1- Intact skin with a localized area of non-blanchable erythema (red discoloration of skin as a result of injury) which may appear differently in darkly pigmented skin. The presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes do not include purple or maroon discoloration; these may indicate a deep tissue pressure injury.
Stage 2 - Partial-thickness skin loss with exposed dermis (thick layer of living tissue below the epidermis which forms the true skin, containing blood capillaries, nerve endings, sweat glands, hair follicles, and other structures). The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Adipose (fat) is not visible, and deeper tissues are not visible. Granulation tissue (new connective tissue and microscopic blood vessels that form on the surfaces of a wound during the healing process), slough (non-viable yellow, tan, gray, green, or brown tissue), and eschar (dead or weakened tissue that is hard or soft in texture - usually black, brown, or tan in color) are not present. These injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel.
Stage 3 - Full-thickness loss of skin, in which adipose is visible in the ulcer and granulation tissue and epibole are often present. Slough and/or eschar may be visible. The depth of tissue damage varies by anatomical location; areas of significant adiposity can develop deep wounds. Undermining (when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound's edge) and tunneling (channels that extend from a wound into and through the tissue or muscle below) may occur. Fascia (thin casing of connective tissue that surrounds and holds every organ, blood vessel, bone, nerve fiber, and muscle in place), muscle, tendon, ligament, cartilage or bone is not exposed. If slough or eschar obscures the extent of tissue loss this is an Unstageable Pressure Injury.
The Lippincott Manual of Nursing Practice, 10th edition, pages 183-184, directed nurses to reposition residents every 2 hours to relieve pressure. The manual also listed risk factors for pressure ulcers, including malnourishment, edema (swelling caused by excess fluid trapped in the body's tissues), and immobility.
This guidance was not followed.
a. Resident #37 was admitted to the facility on [DATE], with multiple diagnoses including multiple sclerosis (a potentially disabling disease of the brain and spinal cord) and quadriplegia (paralysis of both arms and legs).
Resident #37's admission MDS assessment, dated 12/22/20, documented the following:
* He had no pressure ulcers on admission.
* He was at risk of developing pressure ulcers.
* He required extensive assistance with activities of daily living and required two plus staff assistance for bed mobility and transfers.
* He did not transition (move himself to change positions) or walk.
* He had impairment in his upper and lower extremities on both sides.
Resident #37's care plan, dated 12/14/20 and revised 4/6/21, documented he had the potential for pressure ulcer development related to decreased mobility, incontinence of bowel, skin frequently moist due to perspiration, and history of chronic non-healing pressure injuries. The care plan listed the goal was for Resident #37 to have intact skin, free of redness, blisters or discoloration, dated 12/15/20 and revised on 6/28/21. One of the interventions listed was Resident #37 was dependent on assistance for turning and repositioning and was to be turned/repositioned at least every 2 hours, and more often as needed or requested, initiated 12/15/20.
A hospital virtual visit (a face-to-face meeting with a health care professional using video technology without leaving the facility) report, dated 2/22/21, documented Resident #37 had a new Stage 3 pressure ulcer on each hip.
Resident #37's care conference report, dated 3/24/21, documented he was to be turned every 2 hours from side to side. The report stated staff were to document Resident #37's cares and turn schedule, and to notify the family if Resident #37 refused cares.
On 6/18/21, a care conference note documented Resident #37 was no longer able to be up in his chair in order to help heal his buttocks [pressure ulcer].
A virtual hospital report, dated 6/21/21, documented Resident #37 was having sacral (a triangular area in the lower back situated between the hipbones) decubitus (pressure) ulcer breakdown again. Resident #37's record did not include documentation as when the pressure ulcer originally developed after Resident #37 was admitted .
Resident #37's bed repositioning records from 6/24/21 through 7/14/21, documented he was not turned or repositioned every 2 hours or a total of 12 times during a 24-hour period as follows:
* Resident #37 was turned/repositioned 2 times on 7/4/21 and 7/13/21
* Resident #37 was turned/repositioned 3 times on 6/27/21, 6/28/21, 6/29/21, 7/1/21, 7/3/21, 7/6/21, 7/8/21, 7/11/21, and 7/14/21.
* Resident #37 was turned/repositioned 4 times on 7/5/21, 7/9/10, 7/10/21, and 7/12/21.
* Resident #37 was turned/repositioned 5 times on 6/24/21, 6/30/21, and 7/2/21.
* Resident #37 was turned/repositioned 6 times on 6/25/21, 6/26/21, and 7/7/21.
The length of time recorded between turing/repositioning of Resident #37 ranged from 2.5 hours (occurring twice) to 9 hours or more (17 times), and 18 hours (1 time).
On 7/20/21 at 11:35 AM, Resident #37 stated he was to be repositioned every hour, but it was not happening.
On 7/23/21 at 10:21 AM, the DON stated staff kept track of Resident #37's repositioning and refusals on the form hanging on the his door. The DON stated Resident #37's refusals and many of the dates were not documented on the form. The DON stated repositioning and refusals were not documented in the electronic record.
On 7/23/21 at 7:11 PM, when asked to review the repositioning documentation, the RCN stated there were lapses in Resident #37's repositioning. The RCN stated it was not documented Resident #37 was repositioned every 2 hours, or he refused repositioning.
b. Resident #630 was admitted to the facility on [DATE], with multiple diagnoses including urinary tract infection, bacteremia (bacteria in the blood), edema, moderate protein-calorie malnutrition, muscle weakness, and reduced mobility.
Resident #630's admission nursing evaluation, undated, documented Resident #630 had no pressure ulcers. The evaluation documented Resident #630 was an older adult and had edema in both lower extremities, which were both risk factors for pressure ulcers.
Resident #630's physician orders, dated 5/14/20, documented a weekly skin assessment was to be completed every Wednesday.
Resident #630's care plan, dated 5/15/20, documented Resident #630 was at high risk for skin impairment, and directed staff to turn Resident #630 every 2-3 hours.
Resident #630's skin integrity evaluation, dated 5/14/20, documented Resident #630 was at moderate risk for pressure ulcers, with the following risk factors:
* Her ability to walk was severely limited or nonexistent and she could not bear her own weight.
* She had a potential problem with skin friction or shear against sheets, chair, or other devices, and occasionally she slid down in her chair or bed.
Resident #630's pain evaluation, dated 5/27/20, documented she had pain at her tailbone when sitting and when laying, but she did not shift position in bed because her feet were elevated to decrease edema.
A weekly skin evaluation, completed on 5/27/20 (13 days after admission), documented Resident #630 had a 2 cm x 1.5 cm Stage 2 pressure ulcer on her sacrum.
Resident #630's ADL flowsheet from 5/14/20 through 6/6/20, documented she was not turned or repositioned every 2 to 3 hours as her care plan directed as follows:
* Resident #630 was turned/respositioned 1 time on 6/2/20 and 6/3/20.
* Resident #630 was turned/repositioned 2 times on 6/6/20.
* Resident #630 was turned/repositioned 3 times on 5/14/20, 5/15/20, 5/16/20, 5/17/20, and 5/31/20,
* Resident #630 was turned/repositioned 4 times on 5/26/20 and 6/1/20.
* Resident #630 was turned/repositioned 5 times on 5/19/20, 5/24/20, 5/27/20, 5/28/20, 5/29/20, 5/30/20, 6/4/20, and 6/5/20.
* Resident #630 was turned/repositioned 6 times on 5/25/20
* Resident #630 was turned/repositioned 7 times on 5/18/20, 5/20/20, 5/21/20, and 5/22/20
On 7/23/21 at 7:15 PM, the RCN said the facility's policy was to measure pressure wounds and start treatment upon discovery of the wound. When shown the ADL flowsheets, the RCN said Resident #630 was not repositioned every 2 hours, and she stated there was no documentation.
3. Residents did not receive adequate staff supervision which resulted in falls.
The facility's policy for Fall Evaluation (Morse Scale) and Management, updated March 2018, documented the following:
* A licensed nurse was to complete the Morse Scale fall evaluation on admission. If the total Morse scale score was greater than 45, the resident was considered as having a high potential for falls.
* A licensed nurse completed re-evaluations with each fall and significant change in condition.
* After the resident has been evaluated and cared for and appropriate notifications have been made, the licensed nurse (LN) would evaluate their neurological assessment and monitor the resident for seventy-two hours for unwitnessed fall or falls that involve the resident's head striking a surface. The LN would update the Morse Scale, complete orthostatic vital signs, a progress note, a brief summary of the fall, the nursing evaluation, actions taken, who was notified, and the resident's condition. The LN would review and update the care plan with newly identified interventions as needed.
This policy was not followed.
Resident #6 was admitted to the facility on [DATE], with multiple diagnoses, including monoplegia (paralysis that impacts one limb) of the left leg, dementia, and anxiety disorder.
The facility's Neurological Evaluation policy, dated 9/14, documented residents' neurological status should be assessed following an unwitnessed fall or accident with injury to the head. The policy documented neurological assessments were to be completed every 15 minutes for 2 hours, every 30 minutes for 2 hours, every 1 hour for 4 hours, then every 8 hours for the remaining 64 hours after the fall.
This policy was not followed.
The admission Morse Fall scale assessment dated [DATE], documented Resident #6 was at high risk for falls.
Resident #6's care plan for fall risk, initiated on 4/15/21, documented staff were to anticipate and meet his needs, ensure his call light was within reach and encourage him to use it, ensure he was wearing appropriate footwear when ambulating, keep him in line-of-sight with frequent checks, and anticipate his toileting needs. The care plan did not specify what was meant by line-of-sight and frequent checks.
An admission MDS assessment. dated 4/21/21, documented Resident #6 was cognitively intact and required extensive assistance of one to two staff members for all daily care. He used a wheelchair for locomotion and had a history of falls prior to admission and in the facility.
A quarterly MDS assessment, dated 7/9/21, documented Resident #6's mental status had declined from cognitively intact to severely cognitive impaired.
A progress note, dated 4/13/21 at 1:42 PM, documented Resident #6, At this time resident has nearly fallen six times if not more. Therapy has been assisting as much as they can in monitoring him as he is requiring constant supervision and reminding for his safety.
Resident #6 had eleven falls in three months from 4/17/21 to 7/17/21, 9 unwitnessed falls and 2 witnessed falls. Resident #6 sustained injuries from 3 of the falls, 6/20/21, 7/3/21, and 7/17/21. Examples include:
a. An I&A report, dated 4/17/21 at 10:30 AM, and a nurse progress note dated 4/17/21 at 1:12 PM, documented Resident #6 had an unwitnessed fall. He was found seated between his wheelchair and bed. Resident #6 was confused, oriented to self only. He had a 4 cm by 2 cm skin tear on the back of his right arm. Resident #6 was not able to give a description of what happened.
Resident #6's care plan for fall risk was revised on 4/19/21, and the following interventions were added:
* Vital sign per center policy. Take blood pressure lying /sitting/ standing one time in the first 24 hours. Initiated on 4/19/21.
* Provide activities that promote excise and strength building when possible. Provide one on one activity if bed bound. Initiated on 4/19/21.
* Offer to lay down or rest in recliner between meals. Initiated on 4/19/21.
The I&A included an IDT review note, dated 4/22/21, which documented the root cause of the fall was Resident #6's poor safety awareness and impulsive behavior as he appeared to have fallen trying to transfer to bed. The IDT note documented the intervention developed to decrease his risk of falls was to offer assistance to bed or a recliner between meals.
b. An I&A report, dated 4/20/21 at 10:39 AM, and a nurse progress note dated 4/20/21 at 10:49 AM, documented Resident #6 had an unwitnessed fall. He was found on the floor beside his bed. His wheelchair was next to the head of the bed and the brakes were not locked on his wheelchair.
The I&A included an IDT review note, dated 4/23/21, which documented the root cause of the fall was Resident #6's poor safety awareness and impulsive behavior. New interventions were to apply an anti-roll back device to his wheelchair and continue with the previous interventions for his fall risk care plan.
Resident #6's fall risk care plan was revised to include a new intervention for Antirollback [sic] to be added to W/C [wheelchair] when available, initiated on 4/26/21.
c. An I&A report, dated 5/3/21 at 2:15 PM, and a nurse progress note dated 5/2/21 at 2:02 PM, documented Resident #6 had an unwitnessed fall. He was found on the floor with his buttocks facing the wheelchair and his bed. His wheelchair brakes were locked. Resident #6 said, I think I bumped the side of my head.
The I&A report included an IDT fall review note, dated 5/8/21, which documented the root cause of the fall was Resident #6's poor safety awareness, overestimating his own abilities, and weakness. The intervention to decrease Resident #6's falls was to check orthostatic blood pressure (a condition in which your blood quickly drops when you stand up from a sitting or lying position which may cause dizziness and fainting) for 3 days and to check his blood pressure and heart rate 4 times a day for 3 days to monitor for trends.
Resident #6's fall risk care plan was revised, on 5/3/21, to include the following new interventions:
* When the resident gets restless, offer food and fluids. Offer bathroom. Check to see if resident has any pain. Offer diversional activities.
* Follows the 4 R's:
- Relieve-ask about pain during the visit. Is anything needed to relieve pain?
- Reposition.
- Restroom, assist the resident to the restroom if needed.
- Reach, verify resident's items are within reach.
Resident #6's care plan was also revised to include a new intervention for drug regimen review related to the fall on 5/2/21, initiated on 5/7/21.
d. An I&A report, dated 5/15/21 at 3:00 PM, and a nurse progress note dated 5/15/21 at 4:39 PM, documented Resident #6 had an unwitnessed fall. He was found on the floor next to his bed with his back against the side of the bed, next to his wheelchair. Resident #6 was unable to describe what happened and was confused. Resident #6 had socks on with no shoes.
The I&A report included an IDT fall review note, dated 5/19/21, which documented the cause of the fall was related to Resident #6 removing his shoes and having poor safety awareness. The intervention to decrease Resident #6's fall risk was for non-skid socks to be worn while out of bed.
Resident #6's fall risk care plan was revised to include the new intervention for non-skid socks to be worn with his shoes when he was out of bed, initiated on 5/19/21.
e. An I&A report, dated 5/24/21 at 10:51 PM, and a nurse progress note dated 5/24/21 at 11:24 PM, documented Resident #6 had a witnessed fall of sliding off the bed.
The I&A report included an IDT fall review note, dated 5/25/21, which documented the fall occurred related to Resident #6's impulsive behavior and lack of safety awareness. A diagnosis of overreactive bladder was added as a contributing factor.
Resident #6's fall risk care plan was revised to include the new intervention for a 72 hour 1:1 time study, initiated on 5/25/21. The care plan did not specify what was meant by a 1:1 time study.
f. An I&A report, dated 5/30/21 at 1:13 PM, and a nurse progress note dated 5/30/21 at 1:21 PM, documented Resident #6 had an unwitnessed fall. He was sitting on the floor by the end of his bed, approximately two feet in front of his wheelchair. He said, I was going to take that plate and this cup out of my room.
The I&A report included an IDT fall review note, dated 6/3/21, which documented the fall occurred related to Resident #6's attempt to self-transfer and his poor safety awareness. The new intervention was for 1:1 staffing to further track his behaviors and try to identify patterns or fall triggers.
Resident #6's fall risk care plan was revised to include the new intervention of pick up dishes after resident finishes meals and pick up clutter, initiated on 6/3/21.
g. An I&A report, dated 6/7/21 at 12:20 PM, and a nurse progress note dated 6/7/21 at 12:29 PM, documented Resident #6 had an unwitnessed fall. He was lying on the floor by the staff bathroom without his wheelchair.
The I&A report included an IDT fall review note, dated 6/10/21, which documented the root cause of the fall was Resident #6's poor safety awareness and impulsive behavior. The intervention to decrease Resident #6's falls was to conduct an incontinence evaluation to assess if toileting would benefit him and decrease his impulsive behavior.
Resident #6's fall risk care plan did not include new interventions.
h. An I&A report, dated 6/18/21, and a nurse progress note dated 6/17/21 at 2:42 AM, documented Resident #6 had an unwitnessed fall. He was found sitting on the floor in his bathroom and he was confused.
The I&A report included an IDT fall review note, dated 6/18/21, which documented the root cause of Resident #6's fall was lack of awareness regarding safety limitations. The plan to decrease Resident #6's risk for falling was ongoing education, frequent checks, and staff would keep him in eyesight at all times.
Resident #6's fall risk care plan was revised to include new interventions, as follows:
* Do not leave the resident alone in the bathroom, initiated on 6/17/21.
* For no apparent acute injury, determine and address causative factors of the fall, initiated on 6/18/21.
i. An I&A report, dated 6/20/21 at 5:58 PM, and a nurse progress note dated 6/20/21 at 6:36 PM, documented Resident #6 had an unwitnessed fall. He was found lying next to his shoes on the floor in his bathroom with a 4 cm cut to the side of his head. Resident #6 continued to attempt self-transfers several times before being redirected to his evening meal. The family requested the resident to be sent to the emergency room (ER) for evaluation.
A progress note, dated 6/20/21 at 6:59 PM, documented Resident #6's family declined to send him to the ER after talking with paramedics who stated the ER would not do anything for Resident #6. The note documented the wound on Resident #6's head was a cut that was no longer bleeding.
The I&A report included an IDT fall review note, dated 6/22/21, which documented the root cause of the fall was Resident #6 was unaware of safety limitations. The intervention to prevent Resident #6's falling was to request a care conference related to the need for placement in a private facility with less stimulation, continue 1:1 resident in staff eyesight until accommodations are met related to safety. The review note also documented ongoing education was to continue with Resident #6 related to weakness and the need for one person to assist him with all transfers.
Resident #6's fall risk care plan had a revised intervention to keep him in-line of sight as able, continue frequent checks, and anticipate toileting needs, initiated on 4/15/21 and revised on 6/22/21.
j. An I&A report, dated 7/4/21 at 10:45 AM, and a nurse progress note dated 7/3/21 at 10:46 AM, documented Resident #6 had a witnessed fall. He had attempted to reach the newspaper on the nursing station counter and lost his balance. He was noted to have two cuts, one on his right temple area and the other on his right cheek, a small skin tear to his right wrist, and some bruising to both of his arms.
A progress note, dated 7/3/21 at 11:10 AM, documented Resident #6 was sent to the hospital for an evaluation.
The I&A report included an IDT fall review note, dated 7/4/21, which documented the facility would continue to monitor Resident #6, keeping him within vision of staff and continue with discharge planning.
Resident #6's care plan did not include new interventions.
Resident # 6's record included an In-service Education Summary, dated 7/3/21, which documented the topic [TRUNCATED]
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, resident and family member interview, and staff interview, it was determined the facility failed to provide adequate services necessary to maintain clean linens and a clean envir...
Read full inspector narrative →
Based on observation, resident and family member interview, and staff interview, it was determined the facility failed to provide adequate services necessary to maintain clean linens and a clean environment. This was true for 3 of 12 residents (#17, #20, and #38) reviewed for their personal environment. This deficient practice had the potential to result in psychosocial distress causing residents to be embarrassed by their environment. Findings include:
a. On 7/19/21 at 7:31 PM, Resident #20 was in his room in his bed. The top sheet on his bed was wet and stained with a yellow color and crumpled into a ball on the side of his bed. The fitted sheet and another folded sheet on his bed had a large wet oval from approximately shoulder height on the bed to 1 foot from the bottom of the bed. There were also two urinals on his window ledge beside his bed, both were filled with urine. Resident #20's room had an odor of urine.
On 7/19/21 at 7:35 PM, Resident #20 stated staff had last changed his incontinence brief and bed linen before breakfast that day.
b. On 7/22/21 at 11:17 AM, Resident #17 walked out of her room with a bag of trash that she stated she had bagged up for staff because her room was dirty and handed it to LPN #1.
c. On 7/22/21 at 2:10 PM, Resident #38's room was observed to have a pile of dirty towels on the floor of her room. Resident #38's family member stated those towels were from her baths on 7/21/21 and 7/22/21. Resident #38's family member stated no one had been in to remove them.
On 7/22/21 at 11:26 AM, CNA #3 stated there was not enough staff to strip beds and change the linens when they were wet. She stated residents were sometimes left in wet beds.
On 7/22/21 at 3:39 PM, the Head Housekeeper, with the Administrator present, stated she vacuumed and mopped the floors every day, and as needed. She stated she was the only housekeeper working that day, and she did all the laundry as well. She stated she works from 6:00 AM until 2:30 PM, Monday through Friday. When she was asked what happened during the night if something needed to be cleaned, the Administrator answered the question stating, We have a Swiffer for afterhours use.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and staff interview, it was determined the facility failed to ensure the MDS assessment acc...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and staff interview, it was determined the facility failed to ensure the MDS assessment accurately reflected the resident's status. This was true for 1 of 12 residents (Resident #12) whose MDS assessments were reviewed. This deficient practice had the potential for negative outcomes if the resident was not assessed and/or monitored due to inaccurate assessments. Findings include:
The Long-Term Care Facility MDS 3.0 RAI manual, version 1.17.1, effective 10/1/19, under section 1.3, Completion of RAI, included instructions for accuracy of MDS assessment as follows:
* Accurate assessment requires collecting information from multiple sources, some of which are mandated by regulations. Those sources must include the resident and direct care staff on all shifts, and should also include the resident's medical record, physician, and family, guardian, or significant other as appropriate or acceptable. It is important to note that information obtained should cover the same observation period as specified by the MDS items on the assessment and should be validated for accuracy (what the resident's actual status was during that observation period) by the IDT completing the assessment.
This instruction was not followed.
Resident #12 was admitted to the facility on [DATE], with multiple diagnoses including dementia and depression.
Resident #12's physician orders, dated 12/21/20, included checking the site of her wander guard bracelet and the wander guard function every shift.
Resident #12's admission care plan for elopement risk, initiated on 12/22/20, documented an intervention for elopement which included applying a wander guard to her wrist.
Resident #12's quarterly MDS assessments, dated 2/10/21 and 5/3/21, documented she was not using a wander/elopement alarm.
On 7/23/21 at 9:50 AM, Resident #12 was observed wearing a wander guard bracelet on her right wrist.
On 7/23/21 at 10:15 AM, the MDS nurse stated Resident #12 wore a wander guard device starting on 12/21/20 and continued to wear it now. The MDS nurse said she coded Resident #12's MDS Wander/ Elopement Alarm section wrong. She stated it should have been coded as yes, used daily in both of her quarterly MDS assessments, dated 2/10/21 and 5/3/21.
Resident #12's MDS assessments were not accurately coded to reflect her use of a wander guard for elopement.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, it was determined the facility failed to ensure the comprehensive resident-centered ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, it was determined the facility failed to ensure the comprehensive resident-centered care plan was timely and accurately developed and implemented to meet residents' needs for 1 of 12 residents (Resident #12) whose care plans were reviewed. This failure created the potential for physical harm and psychosocial distress if the residents did not receive appropriate care and treatment related to the delay or inaccurate plan of care. Findings include:
Long-Term Care Facility MDS 3.0 RAI Manual, version 1.17.1, effective October 1, 2019, under section 4.7 4.7 The RAI and Care Planning, accessed on 7/27/21, included requirements for resident care planning as follows:
* The care plan is driven not only by identified resident issues and/or conditions but also by a resident's unique characteristics, strengths, and needs. A care plan that is based on a thorough assessment, effective clinical decision making, and is compatible with current standards of clinical practice can provide a strong basis for optimal approaches to quality of care and quality of life needs of individual residents.
* The facilities have seven days after completing the admission MDS RAI assessment to develop or revise the resident's care plan.
Resident #12 was admitted to the facility on [DATE], with multiple diagnoses including dementia and depression.
The Idaho Preadmission Screening and Resident Review (PASRR) Level 1, dated 11/12/20, documented Resident #12 had major depressive disorder and anxiety for which she was taking medications. The PASRR also documented she had difficulty adapting to change, had a history of a suicide attempt, suicidal talk, and suicidal ideas. It stated she received mental health services in the hospital on [DATE] and had a suicide attempt or gesture on 3/16/20.
Resident #12's care plan, initiated on 11/17/20, included identification and interventions related to the use of her medications for depression and anxiety with goals for her to be free from discomfort or adverse reactions related to those medications.
A social services progress note, dated 11/20/20, documented Resident #12's daughter had called to make the facility aware Resident #12 received psychiatric services and she gave the name of the psychiatrist treating Resident #12. The note also documented Resident #12's daughter stated she had recently been evaluated via telehealth and requested the facility obtain documentation from the visit .so we have documentation she was seen and the outcome of that appointment.
Resident #12's care plan did not include specific and individualized interventions and goals related to her diagnoses of depression and anxiety on admission. There was no documentation in the care plan how she exhibited changes or increased depression and anxiety.
On 7/23/21 at 6:05 PM, Resident #12's PASRR Level 1 evaluation record was presented to the DON, with the DDCO, ED, and RCN present. The DON said she was unaware that Resident #12 had a history of suicide attempt or gesture on 3/16/20. The DON stated when residents have suicidal thoughts, staff would monitor that resident, or they would send them to the emergency department. She stated she would have assessed Resident #12's risk related to suicide or sent her to the ER for evaluation. When asked what Resident #12's risk was for suicidality with multiple elopements, the RCN stated, She has an alarm, and staff were alerted. That is my answer.
Resident #12's comprehensive care plan did not include interventions and goals related to her diagnoses and care upon admission.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review, and staff interview, it was determined the facility failed to ensure residents' care plan...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review, and staff interview, it was determined the facility failed to ensure residents' care plans were reviewed and/or revised as needed. This was true for 3 of 12 residents (#12, #32, and #37) whose care plans were reviewed for accuracy. This created the potential for physical and/or psychosocial harm if cares and/or services were not provided appropriately due to inaccurate information in the care plan. Findings include:
1. Resident #12 was admitted to the facility on [DATE], with multiple diagnoses including dementia and depression.
A social services progress note, dated 4/20/21 at 5:58 PM, documented staff reported to the SSD Resident #12 was displaying increased signs and symptoms of depression. The note documented behavior monitoring was in place.
A nursing progress note, dated 5/21/21 at 10:39 AM, documented Resident #12 informed her physician she slept frequently throughout the day, had a low energy level, and informed him I feel blue throughout the day.
A nursing progress note, dated 6/15/21 at 6:42 PM, documented Resident #12 was upset about her roommate not liking her and stated she was scared to go into her room. The nurse documented Resident #12 refused to go into her room until other arrangements were made for her to sleep in another room.
A nursing progress note, dated 6/16/21 at 6:45 AM, documented Resident #12 told the nurse I have to get out of here, I can't stay in the same room as her. The note documented Resident #12 was pointing to her roommate.
A nursing progress note, dated 6/16/21 at 6:49 AM, documented Resident #12 was afraid of her roommate and told the nurse she was not safe around her and she needed to leave the facility and go home.
A nursing progress note, dated 6/30/21 at 5:44 PM, documented Resident #12 was convinced she needed to go home and was slightly agitated with staff who attempted to redirect her.
A nursing progress note, dated 7/721 at 2:27 PM, documented Resident #12 was confused and Wanted to know why she was trapped in the basement of the building.
A nursing progress note, dated 7/16/21 at 1:10 PM, documented Resident #12 was walking down the hallway toward the exit door. She did not respond when the nurse called her name, and she exited the building. The MDS nurse followed Resident #12 and asked her what she was doing. Resident #12 stated she was going .to jump of [sic] the cliff.
Resident #12's care plan did not include interventions related to her behaviors exhibited due to her diagnosis of depression and anxiety. Resident #12's care plan did not include interventions related to her suicidal ideation.
On 7/23/21 at 5:50 PM, the RCN was asked, with the DDCO, ED, and DON present, if the facility had new elopement interventions in place after Resident #12's elopement incident on 4/29/21. The RCN stated she could not speak towards that; whatever is in the incident report is in the investigation, and we care planned it. We were not here. When the RCN was asked if she was aware Resident #12 recently had an elopement attempt with suicidal thoughts, she stated what was documented in the chart was she wanted to jump off a cliff. The RCN stated, She has an alarm, and staff were alerted.
2. Resident #32 was admitted to the facility on [DATE], with multiple diagnoses including stroke and heart disease.
Resident #32's care plan, dated 3/23/21, included her use of an antipsychotic medication with interventions related to symptoms and adverse effects of the use of the medication.
An admission MDS assessment, dated 3/25/21, documented Resident #32 had no behavioral symptoms.
A Psychotropic Drug and Behavior Quarterly & PRN (as needed) report for psychotropic medication dated 4/27/21, documented Resident #32 was prescribed quetiapine fumarate (an antipsychotic medication which works by altering brain chemistry to help reduce psychotic symptoms like hallucinations, delusions and disordered thinking) once a day. The report documented for non-drug interventions, Will get interventions in place. The report also documented for new target behaviors Will get behavior monitors in place.
Resident #32's care plan was not updated to include interventions related to her need for psychotropic medication and any behaviors associated with the use of the medication or her diagnosis for the medication.
The diagnosis of dementia with behavioral disturbance was added to Resident #32's record on 4/30/21.
A nursing progress note, dated 6/17/20 at 11:20 PM, documented Resident #32 showed an increase in agitation, throwing her arms and leg off the bed. It documented the nurse was unable to get a blood pressure reading due to Resident #32's increased agitation. The progress note documented Resident #32's son was called, informed of Resident #32's increased agitation and he agreed she needed to go to the hospital. Resident #32 left via emergency medical services transportation at 12:00 AM. She returned to the facility later the same day.
A nursing progress note, dated 6/18/20 at 3:47 AM, documented Resident #32 had returned from a local hospital and was still slightly agitated.
A nursing progress note, dated 6/18/21 at 1:11 PM, documented Resident #32 was agitated and refused to keep her clothing or blankets on when in bed.
A nursing progress note, dated 6/19/21 at 2:16 AM, documented Resident #32 was easily agitated with cares and assessment. She was thrashing arms and legs around.
The care plan did not identify or include interventions related to her dementia and/or behaviors.
A Psychotropic Drug and Behavior Quarterly & PRN report for psychotropic medication dated 6/21/21, documented Resident #32 was prescribed quetiapine fumarate once a day for dementia with behavioral disturbance. The report documented for non-drug interventions, Will get interventions updated and placed on care plan and in orders for nursing. The report also documented for new target behaviors Will get behaviors updated and placed on care plan and in orders for nursing. The report documented team recommendations were for Resident #32 to continue her medications and to have behavioral monitoring and interventions in place.
Resident #32's care plan was not updated to include interventions related to her need for psychotropic medication and any behaviors associated with the use of the medication or her diagnosis for the medication.
Resident #32's care plan for behavior problems related to her dementia was initiated on 7/2/21 and revised on 7/21/21.
On 7/23/21 at 7:15 PM, the RCN and DON stated interventions for a new condition should be added and started upon discovery.
Resident #32's care plan was not revised and updated to reflect her status and care needs for dementia with behaviors.
3. Resident #37 was admitted to the facility on [DATE], with multiple diagnoses of multiple sclerosis (a potentially disabling disease of the brain and spinal cord), right and left hip pressure ulcers, quadriplegia (paralysis of both arms and legs), and high blood pressure.
Resident #37's care plan for pain included the following intervention, Has implanted baclofen pump, monitored and refilled it at the pain clinic. Alert Pain clinic to any issues. The pump was a surgically implanted machine that delivered a muscle relaxant to Resident #37's spinal fluid.
Resident #37's record did not include documentation of his pain clinic visits. It could not be determined if Resident #37's baclofen pump was in use.
The DON and MDS nurse were interviewed together on 7/22/21 at 7:37 PM. They confirmed Resident #37 had an implanted baclofen pump when he was admitted to the facility. They stated the pump was not in use at the time and had not been used since his admission. The DON confirmed Resident #37's care plan was not correct because it included his baclofen pump as an active pain intervention.
Resident #37's care plan was not accurate.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review and staff interview, it was determined the facility failed to ensure professional standard...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review and staff interview, it was determined the facility failed to ensure professional standards of practice were followed related to management of wounds and completion of neurological checks. This was true for 2 of 12 residents (#6 and #12) reviewed for quality of care. Specifically:
* Resident #12 and Resident #6 were at risk for undetected neurological impairment when the facility did not complete neurological assessments after unwitnessed falls.
* Resident #6 was at risk for worsening skin impairment when the facility did not follow its policy and Resident #6's physician orders to complete weekly skin assessments.
Findings include:
1. The facility's Neurological Evaluation policy, dated 9/2014, documented residents' neurological status should be assessed following an unwitnessed fall or accident with injury to the head. The policy documented neurological assessments were to be completed every 15 minutes for 2 hours, every 30 minutes for 2 hours, every 1 hour for 4 hours, then every 8 hours for the remaining 64 hours after the fall.
This policy was not followed. Examples include:
a. Resident #6 was admitted to the facility on [DATE], with multiple diagnoses including monoplegia (paralysis that impacts one limb) of the left lower leg, dementia, and anxiety disorder.
An admission MDS assessment, dated 4/21/21, documented Resident #6 was cognitively intact. He required extensive assistance of one to two staff members for all daily cares. He used a wheelchair for locomotion, and he had a history of falling prior to admission to the facility and in the facility in the last month.
Resident #6's quarterly MDS assessment, dated 7/9/21, documented his mental status had declined and he had severe cognitive impairment.
A fall risk evaluation, dated 4/12/21, documented Resident #6 was at high risk for falls.
Review of I&A reports documented Resident #6 had 10 unwitnessed falls from 4/17/21 to 7/17/21. Resident #6's record did not include documentation of complete neurological assessments per the facility's policy as follows:
* 4/17/21: At 10:30 AM an I&A report documented Resident #6 had a fall. At 1:12 PM, a progress note documented Resident #6 was found seated between his wheelchair and the bed. He was confused and oriented to self only and had a 4 cm x 2 cm skin tear on the back of his right arm. There were no neurological assessments documented.
* 4/20/21: At 10:39 AM an I&A report documented Resident #6 had a fall. At 10:49 AM, a progress note documented Resident #6 was found on the floor beside his bed. His wheelchair was next to the head of his bed and the wheelchair breaks were not locked. Neurological assessments were not documented every 1 hour for the remaining 3 hours and every 8 hours for the remaining 64 hours per the facility's policy.
* 5/2/21: At 2:15 PM an I&A report documented Resident #5 had a fall. At 2:02 PM, a progress note documented Resident #6 had was found on the floor with his buttock facing the wheelchair and his bed. The note documented Resident #6 said, I think I hit my head. Neurological assessments were not documented every 1 hour for the remaining 1 hour and every 8 hours for the remaining 64 hours per the facility's policy.
* 5/15/21: At 3:00 PM an I&A report documented Resident #6 had a fall. At 4:39 PM, a progress note documented Resident #6 was found on the floor next to the bed with his back against the side of the bed next to his wheelchair. The note documented he was unable to describe what happened and was 'pleasantly confused. Neurologic assessments were not documented every 8 hours for the remaining 64 hours per the facility's policy.
* 5/30/21: At 1:13 PM an I&A Report documented Resident #6 had a fall. At 1:21 PM a progress note documented Resident #5 was found sitting on the floor by the end of his bed, approximately two feet in front of his wheelchair. Neurological assessments were not documented every 8 hours for the remaining 64 hours per the facility's policy.
* 6/7/21: At 12:20 PM an I&A Report documented Resident #6 had a fall. At 12:29 PM a progress note documented Resident #6 was found lying on the floor by the staff bathroom without his wheelchair. There were no neurological assessments documented.
* 6/18/21: An I&A report documented Resident #6 had a fall. At 2:42 AM a progress note documented Resident #6 was found sitting on the floor in his bathroom and was confused. Neurological assessments were not documented every 8 hours for the remaining 64 hours per the facility's policy.
* 6/20/21: At 5:58 PM an I&A report documented Resident #6 fell. At 6:36 PM A progress note documented Resident #6 was found lying next to his shoes on the floor in his bathroom with a 4 cm skin tear to the side of his head. There were no neurological assessments documented.
Review of I&A reports documented Resident #6 had a witnessed fall on 7/17/21. A progress note documented Resident #6 was sitting in his wheelchair by the nurse's station, attempted to pick up a bag of crackers from the floor, and fell out of his wheelchair. The note documented Resident #6 landed on the floor and hit the right side of his face, his shoulder, and his hip. The note documented the laceration on his right temple from the fall on 7/3/21 was reopened and was 4 cm by 0.2 cm. Neurological assessments were not documented every 8 hours for the remaining 16 hours per the facility's policy when there is an accident with injury to the head.
On 7/23/21 at 5:35 PM, the DON with the DDCO, ED, and RCN present, said if the neurological assessments were not documented on the neurological assessment sheet, then they were not completed.
b. Resident #12 was admitted to the facility on [DATE], with multiple diagnoses including dementia and depression.
Resident #12's fall risk assessment, dated 11/12/21, documented she was at high risk for falls.
An I&A report, dated 11/18/20 at 10:06 AM, and a nursing progress note dated 11/18/20 at 10:12 PM, documented Resident #12 had an unwitnessed fall. She was found on her knees by her bed.
Resident #12's record did not document neurological assessments were completed every 1 hour for 4 hours and every 8 hours for the remaining 64 hours per the facility's policy.
On 7/23/21 at 5:35 PM, the DON with the DDCO, the ED, and the RCN present, said if the neurological assessments were not documented on the neurological assessment sheet, then they were not completed.
2. The facility's Skin Integrity Policy, revised May 2019, documented the following:
* The licensed nurse was responsible for documenting a skin impairment identified on admission. This included measurements of size, color, presence of odor, exudate (fluid that leaks out of blood vessels into nearby tissues), and presence of pain. The skin impairment was documented in the nurse's notes and on the weekly wound evaluation form.
* Facility staff were responsible for evaluating wounds weekly and documenting the wound evaluation, measurement, and findings in the medical record.
This policy was not followed.
Resident #6 was admitted to the facility on [DATE], with multiple diagnoses including monoplegia (paralysis that impacts one limb) of the left leg, dementia, and anxiety disorder.
Resident #6's admission assessment, dated 4/21/21, documented Resident #6 was admitted with a Stage 2 (partial-thickness skin loss with exposed dermis [thick layer of tissue below the skin]) pressure ulcer.
A progress note, dated 4/12/21, documented Resident #6 had a pressure ulcer on his right buttock that measured 1.2 cm x 0.8 cm x 0.1 cm. The ulcer was pink, and blanchable (skin tissue that turns white when pressed with a fingertip and then immediately turns pink or red again when the pressure is removed).
A physician order, dated 4/14/21, directed staff to complete a weekly skin audit for Resident #6.
Resident #6's care plan, initiated 4/15/21, documented Resident #6 required a skin inspection during daily cares, and staff were to observe for redness, open areas, scratches, cuts, and bruises and report changes to the nurse.
A progress note, dated 4/17/21, documented Resident #6 had an unwitnessed fall and was found seated between his wheelchair and the bed. He was confused and oriented to self only and had a 4 cm x 2 cm skin tear on the back of his right arm.
Resident #6's skin and wound evaluation, dated 4/18/21, documented he had skin tears which were new and acquired in the facility.
A progress note, dated 6/20/21 documented Resident #6 had an unwitnessed fall and was found lying next to his shoes on the floor in his bathroom with a 4 cm skin tear to the side of his head. Resident #6's record did not include a weekly evaluation of the wound as directed by the facility's policy.
A progress note, dated 7/17/21 documented Resident #6 had a witnessed fall and was sitting in his wheelchair by the nurse's station and attempted to pick up a bag of crackers from the floor, and fell out of his wheelchair. The note documented Resident #6 landed on the floor and hit the right side of his face, his shoulder, and his hip. The note documented the laceration on his right temple from the fall on 7/3/21 was reopened and was 4 cm by 0.2 cm. Resident #6's record did not include a weekly evaluation of the wound as directed by their policy, and there was no weekly skin audit as directed by the physician's order on 4/14/21.
On 7/23/21 at 5:35 PM, when asked about weekly skin documentation, the RCN stated they were not completed.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, it was determined the facility failed to ensure residents received care and services...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, it was determined the facility failed to ensure residents received care and services necessary to achieve their highest practicable physical, emotional, and psychosocial well-being. This was true for 1 of 5 residents (Resident #32) reviewed for dementia care. This failure had the potential to result in psychosocial distress by interfering with the resident's ability to engage in meaningful relationships and maintain their dignity, autonomy, and independence. Findings include:
Resident #32 was admitted to the facility on [DATE], with multiple diagnoses including stroke, and heart disease.
An admission MDS assessment, dated 3/25/21, documented Resident #32 had no behavioral symptoms.
A nursing progress note, dated 6/17/20 at 11:20 PM, documented Resident #32 showed an increase in agitation, throwing her arms and leg off the bed. It documented the nurse was unable to get a blood pressure reading due to Resident #32's increased agitation. The progress note documented Resident #32's son was called, informed of Resident #32's increased agitation and he agreed she needed to go to the hospital. Resident #32 left via emergency medical services transportation at 12:00 AM. She returned to the facility later the same day.
A nursing progress note, dated 6/18/20 at 3:47 AM, documented Resident #32 had returned from a local hospital and was still slightly agitated.
A nursing progress note, dated 6/18/21 at 1:11 PM, documented Resident #32 was agitated and refused to keep her clothing or blankets on when in bed.
A nursing progress note, dated 6/19/21 at 2:16 AM, documented Resident #32 was easily agitated with cares and assessment. She was .thrashing arms and legs around.
A Psychotropic Drug and Behavior Quarterly & PRN (as needed) report for psychotropic medication dated 4/27/21, documented Resident #32 was prescribed quetiapine fumarate (an antipsychotic medication which works by altering brain chemistry to help reduce psychotic symptoms like hallucinations, delusions and disordered thinking) once a day. The report documented for non-drug interventions, Will get interventions in place. The report also documented for new target behaviors Will get behavior monitors in place. The report documented the team recommendation was to ask for an appropriate diagnosis for the medication.
The diagnosis of dementia with behavioral disturbance was added to Resident #32's record on 4/30/21.
Resident #32's care plan, dated 3/23/21, included her use of an antipsychotic medication with interventions related to symptoms and adverse effects of the use of the medication. The care plan did not identify or include interventions related to her dementia and/or behaviors.
A Psychotropic Drug and Behavior Quarterly & PRN report for psychotropic medication dated 6/21/21, documented Resident #32 was prescribed quetiapine fumarate once a day for dementia with behavioral disturbance. The report documented for non-drug interventions, Will get interventions updated and placed on care plan and in orders for nursing. The report also documented for new target behaviors Will get behaviors updated and placed on care plan and in orders for nursing. The report documented team recommendations were for Resident #32 to continue her medications and to have behavioral monitoring and interventions in place.
Resident #32's care plan for behavior problems related to her dementia was initiated on 7/2/21 and revised on 7/21/21, more than 3 months after it was identified and treated with psychotropic medications.
On 7/22/21 at 3:48 PM, the DON with DDCO present, stated interventions for Resident #32 were discussed during the psychotropic drug and behavior review with the IDT. The DDCO stated the IDT may begin behavior monitoring without a medication order.
On 7/23/21 at 7:15 PM, the RCN and DON stated interventions for a new condition or behavior should be added and started upon discovery.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, policy review, and staff interview, it was determined the facility failed to ensure infecti...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, policy review, and staff interview, it was determined the facility failed to ensure infection control and prevention practices were implemented and maintained for residents who received wound care and residents who required assistance with feeding by staff. This was true for 1 of 1 (Resident #1) observed for wound care. These failures had the potential to expose residents to the risk of infection from cross-contamination. Findings include:
The CDC (Center for Disease Control and Prevention) website, accessed on 7/24/21 and last reviewed on 1/8/21, stated, Healthcare personnel should use an alcohol-based hand rub or wash with soap and water for the following clinical indications:
- Immediately before touching a patient
- Before performing an aseptic task (e.g., placing an indwelling device) or handling invasive medical devices
- Before moving from work on a soiled body site to a clean body site on the same patient
- After touching a patient or the patient's immediate environment
- After contact with blood, body fluids, or contaminated surfaces
- Immediately after glove removal
2. The Journal of Wound, Ostomy, and Continence Care article Clean vs. Sterile Dressing Techniques for Management of Chronic Wounds A Fact Sheet, accessed on 7/29/21, stated Clean technique involves meticulous handwashing, maintaining a clean environment by preparing a clean field, using clean gloves and sterile instruments, and preventing direct contamination of materials and supplies. The article also stated, Clean technique is considered most appropriate for long-term care .
These guidelines were not followed.
Resident #1 was admitted to the facility on [DATE], with multiple diagnoses including chronic kidney disease, adult failure to thrive, stage 3 pressure ulcer of left ankle, and congestive heart failure.
Resident #1's Quarterly Review Assessment, dated 6/30/21, document she had one stage three unhealed pressure ulcer.
Resident #1's record, included the wound care order, dated 7/19/21, as follows:
Cleanse with NS [normal saline], apply Bactroban, cover with telfa, wrap with kerlix, tape in place. Change dressing daily and PRN [as needed].
On 7/22/21 at 11:04 AM, Resident #1's wound care was observed. During the observation, LPN #2 prepared to provide wound care for Resident #1's stage 3 pressure ulcer on her left ankle by donning the appropriate PPE for contact precautions. She removed Resident #1's wound dressing, cleansed the wound, then removed her gloves and donned new gloves before she applied Bactroban and dressed the wound. LPN #2 did not perform hand hygiene immediately after glove removal before donning new gloves.
During an interview on 7/22/21 at 3:00 PM, LPN #2 confirmed she did not perform appropriate hand hygiene between removing her gloves and donning new ones during Resident #1's wound care.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review, and staff interview, it was determined the facility failed to provide information regardi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review, and staff interview, it was determined the facility failed to provide information regarding advance directives, and/or periodically review and document discussions regarding advance directives, for 4 of 12 residents (#14, #32, #37, and #210) reviewed for advance directives. This failure created the potential for harm if a resident's medical treatment wishes were not followed due to a lack of accurate information in the resident's records. Findings include:
The facility's policy titled Advance Directive, dated 11/2016, stated the facility reviewed information regarding advance directives with each resident on admission and honored each advance directive that was provided. It stated upon admission each resident or resident's responsible party was asked if an advance directive had been prepared and made a copy of it for the resident's record. If they had no advanced directive, the facility provided a resident handbook with information about advance directives. It further stated each resident's advance directive was reviewed and discussed during a care plan conference and documented in the resident's record.
This policy was not followed.
a. Resident #32 was admitted to the facility on [DATE] with multiple diagnoses including dementia with behavioral disturbance, stroke, and heart disease.
Resident #32's admission assessment, dated 3/25/21, documented Resident #32 was severely cognitively impaired.
Resident #32's record included an advance directive dated 4/2011, ten years prior to admission, and did not include documentation in the care conference notes that it was discussed with the resident's representative.
b. Resident #210 was admitted to the facility on [DATE], with multiple diagnoses including chronic kidney disease, history of stroke, and diabetes mellites.
Resident #210's admission MDS assessment, dated 3/5/21, documented he was cognitively intact.
Resident #210's record did not include an advance directive or documentation of discussions regarding advance directives.
c. Resident #14 was re-admitted to the facility on [DATE], with multiple diagnoses including diabetes mellitus and lymphedema (a long-term condition where excess fluid collects in tissues causing swelling).
Resident #14's admission MDS assessment, dated 6/27/19, documented she had moderate cognitive impairment.
Resident #14's record did not include an advance directive or documentation of discussions regarding advance directives.
d. Resident #37 was admitted to the facility on [DATE], with multiple diagnoses of multiple sclerosis (a potentially disabling disease of the brain and spinal cord), right and left hip pressure ulcers, quadriplegia (paralysis of both arms and legs), and high blood pressure.
Resident #37's admission MDS assessment, dated 12/22/20, documented Resident #37 was cognitively intact.
Resident #37's record included an advanced directive dated 12/2019, one year prior to admission.
There was no documentation in the record that Resident #37's advance directive was discussed at the care conferences with Resident #37 or his representative after 12/2019.
On 7/21/21 at 12:00 PM, the SSD stated that upon admission each resident was asked for a copy of their advance directive. She stated if the resident did not have an advance directive the facility offered one and would provide the forms at a care conference. The SSD stated the advance directives were reviewed at the care conference of each resident 72-hours after admission and annually. The SSD stated when documenting care conferences, she did not check the advance directive box when it was discussed. The SSD stated the advance directive box was not checked indicating the facility did not review the advance directive with the resident and/or the resident's representative.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
Based on observation, record review, review of the Quality Assessment Performance Improvement (QAPI) plan, review of the QAPI meeting minutes, review of staffing, review of grievances, and resident an...
Read full inspector narrative →
Based on observation, record review, review of the Quality Assessment Performance Improvement (QAPI) plan, review of the QAPI meeting minutes, review of staffing, review of grievances, and resident and staff interview, it was determined the facility failed to take actions to identify, track performance, and resolve systemic problems. These failed practices directly impacted 23 residents (#1-#3, #6, #12, #14, #15, #17, #20, #21, #25 #27, #29, #30, #32, #34, #35, #37-#39, #141, #210, and #360), and had the potential to affect the other 24 residents residing in the facility. The facility failed to implement improvement actions to resolve identified insufficient staffing to meet resident needs regarding elopement, behavioral health services, and bathing. Findings include:
The facility's QAPI plan, dated 3/21/20, documented quality improvement is tied to the ability to identify and correct quality deficiencies any time they occur throughout the facility as well as providing opportunities for improvement. The plan stated the QAPI program will aim for safety and high quality with all clinical interventions and service delivery while emphasizing autonomy, choice, and quality of daily life for residents and family. The QAPI plan also stated the following:
*Identify and correct quality deficiencies any time they occur throughout the facility.
*Incorporate resident and staff input that reflects services provided to residents.
*Maintain a system to track and monitor adverse events that will be investigated every time they occur.
This plan was not followed.
There was no documentation resident, family, and staff concerns were evaluated through the QAPI process. Examples include:
1. Resident Council Meeting minutes, dated 1/27/21 to 7/14/21 were reviewed, and documented the following concerns:
* On 1/27/21, the minutes documented concerns regarding insufficient numbers of staff, call lights not answered in a timely manner, call light buttons not always in reach, beds made sloppily, laundry not picked up off the floor, and residents were not bathed/showered regularly.
The written response to the Resident Council, dated 1/29/21, documented call light audits were completed, CNAs were educated on checking on residents every 2 hours and picking up dishes and laundry in resident rooms, and a shower aide was being scheduled and showers were being tracked. The response did not address call lights being out of reach.
*On 2/17/21, the minutes documented residents stated they would like to have a restorative aide available to get more exercise and 2 residents wanted to walk daily but could not without a restorative aide. The minutes stated the food was still cold at meal times.
The written response to the Resident Council, dated 2/17/21, documented a restorative program was scheduled to start on 3/1/21, and residents were reviewed for who would get the best benefits from the restorative program. The response also documented more residents would be added once the program was established and as appropriate. There was no written response regarding meal temperatures.
* At the meeting dated 4/21/21, residents were concerned food was continuing to be served cold and one of the recent meals had very dry and tough pork chops.
The written response to the Resident Council, dated 4/23/21, documented the Dietary Manager was working with nursing and dietary staff to develop a plan of action for training them how to use a pellet warmer for plates.
*On 6/16/21, the minutes documented concerns about drinking water not being distributed, CNA staffing was not sufficient, and residents were not receiving eating assistance.
*On 7/14/21, the minutes documented concerns about drinking water not being distributed, beds were not made, toenails were not clipped, showers not done, call lights not in reach, and oxygen tanks not filled, available, or turned on or off.
On 7/21/21 at 10:10 AM, a meeting was conducted with residents to discuss their concerns. All of the residents who were present, #2, #3, #21, #27, #30, #35, and #141, stated there were staffing concerns related to resident cares. The residents stated drinking water was not distributed, staffing was insufficient particularly in the evening, before meals, and at bedtime. Two residents, Resident #21 and Resident #35, said they waited 2 hours to be assisted out of bed and dressed for the day today. Three of 7 residents in attendance, Resident #3, Resident #21, and Resident #35, said the staff did not do the needed task when the call light was on; they came back 1 or 2 times before it was completed. All residents said they have waited more than 1 hour for a call light, Resident #27 said she waited for 3 hours for a call light to be answered, and Resident #3 said she waited 1 hour for a call light to be answered. The 7 residents in attendance said their toenails were not clipped in the last two weeks.
All residents who attended the Resident Council meeting agreed there was not enough staff to provide showers. Resident #35 said she received a shower 3 1/2 weeks ago before receiving a shower this morning. One resident said they had not received a shower in the last 2 weeks. Resident #30 said she received a shower 2 weeks ago before receiving a shower this morning. Resident #3 said it had been 1 1/2 weeks since she had a shower.
During the Resident Council meeting, Resident #3 stated long waits for cares were ongoing, and the residents had to remind the staff about showers, call lights, and trash removal. Resident #2 stated the staff were not trained to use the sit to stand device, and that she was stuck standing with it for quite a while because the machine had stalled, and staff did not know what to do.
Resident concerns were not identified and addressed in the facility's QAPI program.
2. Resident grievances dated 3/15/21 to 6/16/21, documented the following concerns:
* On 3/15/21, a grievance documented a resident did not receive a shower before his outing with family. The action taken was the staff was educated regarding scheduled showers.
* On 4/13/21, a grievance documented a resident's medication was 4 hours late the night before, and when CNA's were asked when medications would be coming, they continually stated they did not know. The actions taken were educating the staff on better communication with residents and communicating resident concerns with the nurse.
* On 5/18/21, a grievance documented a resident waited 1-2 hours on average, for call lights to be answered, and as a result soiled her briefs, and had to sit in feces making her bottom sore and red. The grievance form documented the SS Director spoke with the resident and staff, and recommendations were to educate all staff regarding policies and procedures in answering call lights in a timely manner, educated the resident to allow the staff to assist with toileting and hygiene before and after meals, and call light audits were done weekly.
* On 6/14/21, a grievance documented a resident's family stated there was not enough staff to meet resident needs and the family had to let others into the building. The grievance form documented on 6/15/21 the DON spoke with family, confirmed the grievance, and the family reported they were happy with care and no abuse or neglect occurred. No other actions were documented.
* On 6/15/21, a grievance documented a resident call light was not answered while they sat on the toilet for 11 minutes and cried. The grievance documented CNA #4 stated the resident should understand she had to help others too. The grievance form documented the SS Director asked for the schedule for 2-night shifts prior, and confirmed CNA #4 worked that shift, but not the long wait.
* On 6/16/21, a grievance documented a resident reported they were in pain, CNA #4 came in turned off the call light and informed him the nurse would come in when able as the nurse had 50 other residents to care for. Resident #2 reported the nurse never came in. The grievance form documented the SS Director requested the physician consider pain meds that were scheduled instead of as needed, and the SS Director confirmed staff had worked that shift. No other actions were documented.
Resident and family concerns were not identified and addressed in the facility's QAPI program.
3. Staff were interviewed as follows:
On 7/22/21 at 11:26 AM, CNA #3 stated the facility did not have enough staff to meet resident needs in a timely manner, if at all. CNA #3 stated there was 1 CNA for two halls and most of those residents required 2 staff for assistance, so they did not get put back to bed when they requested or were tired. CNA #3 stated the CNA's did not have enough time to strip beds and complete morning cares before breakfast because there were only 1-2 CNA's in the building. CNA #3 stated required vital signs were not done because everyone was unable to keep up with cares and resident needs. She stated bowel movements were the priority, everything else was done later, or did not happen.
On 7/22/21, CNA #5, a shower aide, stated 2-3 times a week she was asked to work the floor instead of doing showers/bathing. CNA #5 stated the aides must then pick up the shower work. CNA #5 stated when she must pick up shower work, she was able to get to a couple of residents but not all who were scheduled to receive one that day.
On 7/23/21 at 3:14 PM, CNA #2 stated resident needs were not being met regarding 2-hour checks, bathing, and answering call lights. CNA #2 stated staff were too busy to clean rooms and change bed linens. CNA #2 stated on 7/11/21, all the residents on one of the halls were dirty with several crying because they had bowel movement on them for an extended period and had been up in their wheelchairs all night long because there was not enough staff to work the Hoyer lift and watch the other residents in the facility. She stated there were only two staff members at night in the facility and to use the Hoyer lift required 2 staff, so they could not do that and take care of other residents. CNA #2 stated the CNA's prioritize bowel movement cleaning and everything else goes to the wayside.
On 7/23/21 at 3:30 PM, CNA#1 stated night shift was the worst regarding lack of staffing. CNA#1 stated it was usually 1 nurse and 1 CNA working the night shift and 1 nurse and 2 CNA's on day shift, no matter what the schedule says. CNA #1 stated he usually did not have enough time to keep residents clean of bowel movements on both hallways and feed them dinner. He stated on weekends some residents do not get their dinner until an hour and thirty minutes after everyone else, because they required assistance with eating. CNA #1 stated one resident's room and care were better than most because the family came in to care for them and administration was aware of this.
On 7/23/21 at 7:26 PM, the DON stated the process for staff to bring concerns to QAPI was a suggestion box which then was taken to IDT and QAPI. When asked for an example of a process improvement project brought through the suggestion box to QAPI she stated she did not know and would have to look at the QAPI book or their electronic quality monitoring program. The DON stated every QAPI issue was identified and corrected. When asked how she knew if the QAPI plan was successful she stated she looked for a decrease in data.
The facility's QAPI minutes from 4/2021 to 6/2021 did not specify how they systematically approached and determined indicators or problem prone areas of concern related to resident care and facility services. The QAPI minutes did not include documentation of process improvement projects.
The facility's QAPI program failed to provide sufficient monitoring and oversight to sustain regulatory compliance as evidenced by the citations the facility received.
* Immediate Jeopardy was identified at F689 related to lack of supervision to prevent elopement and at F740 related to lack of behavioral health care services related to suicidal ideation.
* Refer to F677 as it relates to the failure of the facility to provide bathing and grooming.
* Refer to F686 as it relates to the failure of the facility to provide care and treatment to prevent pressure wounds.
* Refer to F725 as it relates to the failure of the facility to ensure there were sufficient numbers of staff to meet the needs of the residents.