WINNING WHEELS



Inspected within the last 6 months. Data reflects current conditions.
Winning Wheels nursing home has received a Trust Grade of F, indicating significant concerns about the quality of care provided. It ranks #664 out of 665 facilities in Illinois, placing it in the bottom tier, and #7 out of 7 in Whiteside County, meaning there are no local options rated lower. The facility’s performance trend is stable, with 17 issues reported consistently in recent years, suggesting persistent problems. Staffing is a weakness, rated at only 1 out of 5 stars, with a high turnover of 45%, which is slightly better than the state average of 46%. There are concerning findings, including a critical incident where a resident at high risk for elopement was found wandering outside and became physically aggressive, as well as serious issues where residents were not protected from abuse, leading to feelings of fear among them.
- Trust Score
- F
- In Illinois
- #664/665
- Safety Record
- High Risk
- Inspections
- Holding Steady
- Staff Stability ⚠ Watch
- 45% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $76,343 in fines. Lower than most Illinois facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 23 minutes of Registered Nurse (RN) attention daily — below average for Illinois. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 50 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Illinois average (2.5)
Significant quality concerns identified by CMS
Near Illinois avg (46%)
Higher turnover may affect care consistency
Well above median ($33,413)
Moderate penalties - review what triggered them
The Ugly 50 deficiencies on record
Jul 2025
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0605
(Tag F0605)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure psychotropic medications were prescribed for a defined duration for 1 of 5 residents (R12) reviewed for unnecessary medications in th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to complete a Preadmission Screening and Resident Review (PASARR) Level...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a dressing was in place for a resident with a ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a resident was transferred in a safe manner fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to date and time liquid nutrition when it was initiated ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to administer a medication as ordered by the physician for one of 18 r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review the facility failed to ensure a multidose insulin pen was discarded 28 days after being opened for 1 of 18 residents (R3) reviewed for medication stor...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide dental services for a resident which applies t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to change their gloves and perform hand hygiene in a man...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure residents rooms were free from pests which appl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review the facility failed to follow the pureed diet menu for 4 of 4 residents (R4, R16, R38 and R42) reviewed for menus in the sample of 18. The findings in...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review the facility failed to ensure residents on a pureed diet were served a meal in a form that meet their needs for 4 of 4 residents (R4, R16, R38 and R42...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review the facility failed to ensure a meal was served in a sanitary manner and faile...
Read full inspector narrative →
May 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to treat a residents (R1) urinary tract infection (UTI) for nearly 48 hours. This applies to 1 of 3 residents (R1) reviewed for improper nursi...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure controlled medications were signed off in the electronic narcotic inventory system at the time the controlled medicatio...
Read full inspector narrative →
Jan 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to utilize a glucose monitoring sensor per physician orders for 1 of 3 residents (R1) reviewed for physician orders in the sample...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to ensure residents received assistance with activities of daily living for 2 of 4 residents (R1, R2) reviewed for activities of ...
Read full inspector narrative →
Jul 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to ensure orders were in place for a resident with non-pressure skin injuries and failed to ensure a resident's central venous catheter dressin...
Read full inspector narrative →
Jun 2024
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide personal care for a resident in a manner to p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) R25's electronic face sheet printed on 6/13/24 showed R25 has diagnoses including but not limited to intracranial injury, epi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
2) The facility's document titled, Illinois Department Of Public Health Facility Report dated 5/3/24 showed, (R25) was sitting in hallway where wing meets hallway, a resident from another hallway star...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to obtain a Level 2 PASRR (Pre-admission Screening and Resident Review) for 2 of 5 residents (R61,R67) reviewed for PASRR screening in the sam...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide feeding assistance to 1 of 1 residents (R37) reviewed for a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to identify a resident's skin concern, assess the area, a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to prevent a medical device related pressure injury and ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a resident's splint was applied to prevent fur...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to safely transfer a hospice resident using a gait belt f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to keep a urinary drainage bag below the level of the bla...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. R67's electronic face sheet printed on 6/13/24 showed R67 has diagnoses including but not limited to cerebral infarction, hem...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, the facility failed to prepare and serve food in a clean, sanitary manner. This failure has the potential to affect all of the residents in the facil...
Read full inspector narrative →
May 2024
4 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to supervise a resident with exit-seeking behaviors to prevent her from...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure a resident (R4) was free from sexual abuse (by ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to report an allegation of abuse. This applies to one of three residents (R1) reviewed for abuse in the sample of 8.
The findings include:
The ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to investigate an allegation of abuse. This applies to one of three residents (R1) reviewed for abuse in the sample of 8.
The findings include:...
Read full inspector narrative →
Aug 2023
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the confidentiality of a resident's electronic ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure interventions were in place for a resident with...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure a resident's call light system was in working o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. R41's face sheet printed on 8/16/23 showed diagnoses including but not limited to cerebral palsy, heart disease, spinal steno...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation. interview and record review, the facility failed to ensure the kitchen was maintained in a clean and sanitary manner, and failed to cover prepared food. This applies to all resid...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected most or all residents
Based on observation. interview and record review, the facility failed to control the fly infestation throughout the facility. This applies to all residents who reside in the facility.
The findings in...
Read full inspector narrative →
Aug 2023
3 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure a resident was free from abuse for 1 of 3 resid...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure a resident was free from abuse for 1 of 3 resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to prevent a medication error for 1 of 3 residents (R1) ...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure the safety of a resident dependent upon staff f...
Read full inspector narrative →
May 2023
4 deficiencies
2 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to recognize and treat a resident with an infected Stage 4 pressure in...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to supervise a resident with difficulty swallowing at mealtime and fai...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to report an injury of unknown origin for 1 of 3 resident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to investigate injuries of unknown origins for 2 of 3 res...
Read full inspector narrative →
Mar 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement their abuse policy by not reporting an allegation of abus...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to report an allegation of abuse for one of five residents (R2) review...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s), 4 harm violation(s), $76,343 in fines, Payment denial on record. Review inspection reports carefully.
- • 50 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $76,343 in fines. Extremely high, among the most fined facilities in Illinois. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Winning Wheels's CMS Rating?
CMS assigns WINNING WHEELS an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Illinois, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Winning Wheels Staffed?
CMS rates WINNING WHEELS's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 45%, compared to the Illinois average of 46%. This relatively stable workforce can support continuity of care. RN turnover specifically is 62%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Winning Wheels?
State health inspectors documented 50 deficiencies at WINNING WHEELS during 2023 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 4 that caused actual resident harm, and 45 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Winning Wheels?
WINNING WHEELS is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 88 certified beds and approximately 74 residents (about 84% occupancy), it is a smaller facility located in PROPHETSTOWN, Illinois.
How Does Winning Wheels Compare to Other Illinois Nursing Homes?
Compared to the 100 nursing homes in Illinois, WINNING WHEELS's overall rating (1 stars) is below the state average of 2.5, staff turnover (45%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
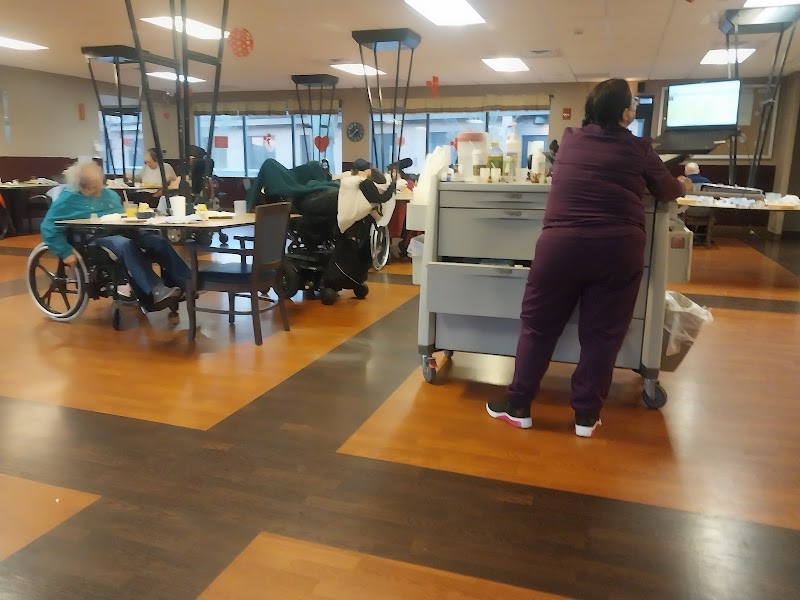
What Should Families Ask When Visiting Winning Wheels?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Winning Wheels Safe?
Based on CMS inspection data, WINNING WHEELS has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Illinois. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Winning Wheels Stick Around?
WINNING WHEELS has a staff turnover rate of 45%, which is about average for Illinois nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Winning Wheels Ever Fined?
WINNING WHEELS has been fined $76,343 across 2 penalty actions. This is above the Illinois average of $33,842. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Winning Wheels on Any Federal Watch List?
WINNING WHEELS is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.