BRICKYARD HEALTHCARE - ELKHART CARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Brickyard Healthcare - Elkhart Care Center has received a Trust Grade of F, indicating significant concerns about the quality of care provided. With a state ranking of #427 out of 505 facilities in Indiana, they fall in the bottom half, and they rank #11 out of 12 in Elkhart County, meaning only one local facility is performing worse. The facility has seen some improvement, as the number of reported issues decreased from 15 in 2024 to just 1 in 2025. Staffing is a relative strength, with a turnover rate of 28%, much lower than the state average of 47%, but the overall staffing rating is only 2 out of 5 stars, which is below average. However, the facility has concerning fines totaling $63,174, higher than 94% of Indiana facilities, and they have less RN coverage than 85% of state facilities, which could impact the level of care. Specific incidents raised serious alarms: one resident suffered from untreated pressure ulcers due to failure to follow treatment orders, leading to hospitalization and eventual death, while another resident with a Foley catheter did not have proper care or monitoring, resulting in sepsis and also death. Additionally, a resident requiring a modified diet did not receive appropriate supervision during meals, which resulted in choking and ultimately death. While there are some staffing strengths, these critical incidents highlight significant weaknesses that families should consider when researching this facility.
- Trust Score
- F
- In Indiana
- #427/505
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ✓ Good
- 28% annual turnover. Excellent stability, 20 points below Indiana's 48% average. Staff who stay learn residents' needs.
- Penalties ○ Average
- $63,174 in fines. Higher than 70% of Indiana facilities. Some compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 21 minutes of Registered Nurse (RN) attention daily — below average for Indiana. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 50 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Low Staff Turnover (28%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (28%)
20 points below Indiana average of 48%
Facility shows strength in staff retention, fire safety.
The Bad
Below Indiana average (3.1)
Significant quality concerns identified by CMS
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 50 deficiencies on record
Jan 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to implement their policy related to reporting an allegation of abuse for 1 of 3 residents reviewed for abuse. (Resident B)
Finding includes:
...
Read full inspector narrative →
Oct 2024
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected most or all residents
Based on observation, record review and interview, the facility failed to ensure food was
served at palatable temperatures in 1 of 1 kitchens observed (Main Kitchen). This deficient practice potential...
Read full inspector narrative →
Aug 2024
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to provide accurate orders for resuscitative wishes for 2 of 3 resident reviewed for advanced directives. (Residents 94 & 36)
Findings include...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to provide resident-centered activities for 1 of 3 resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview, the facility failed to ensure edema was monitored for 1 of 1 residents review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide a range of motion program to prevent further contractures for 1 of 2 residents reviewed for range of motion. (Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide a peripherally inserted central catheter care for 1 of 5 residents reviewed for infection control (Resident 266)
Find...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide adequate tracheostomy care for 1 of 1 resident reviewed for tracheostomy/ventilation. (Resident 93)
Finding includes:...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to verify controlled substance counts for 1 of 1 medication cart observed. (SW Unit)
Finding includes:
During a medication storag...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure an appropriate diagnosis for a resident who received an anti...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure staff change gloves and complete hand hygiene when providing perineal care for 1 of 1 resident reviewed for personal ca...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure resident funds were available on the same day of the request and for the desired amount for 4 of 4 residents reviewed for facility-m...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0570
(Tag F0570)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure a surety bond sufficiently covered the total monies in the Resident Fund account. This had the potential to affect the 56 residents ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During an observation of Resident 107, on 7/29/2024 at 10:00 A.M., a bottle of Glucerna 1.5 was infused at 60 milliliters per...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure comprehensive person-centered plans of care were created rel...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to ensure food was handled appropriately,
foods were sealed appropriately, and failed to date foods when opened. This had the p...
Read full inspector narrative →
Jul 2023
12 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure standards of care of visually observing a resident take their medications was followed for 1 of 1 residents randomly observed. (Reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure the Physician Orders for Scope of Treatment (POST) forms were accurately completed for 3 of 3 residents whose Advanced Directives we...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to notify a plysician timely of missed doses of unavailable medication for 2 of 5 residents whose medications were reviewed. ( Resident 26 & B...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure pertinent transfer and resident clinical information was completed for 1 of 3 residents reviewed for transfers. (Resident 72)
Findin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to provide transfer form information for 1 of 3 residents reviewed for hospitalization. (Resident 72)
Finding include:
During an interview, on...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to provide a care plan for the use of a continuous posit...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure showers were provided timely for 1 of 3 residents reviewed for activity of daily living (ADL) care. (Resident 47)
Find...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide sanitation of the continuous positive airway pressure (C-Pap) equipment for 1 of 3 residents reviewed for supportive ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure medications were available from the pharamacy for 2 of 4 residents reviewed for pain. (Resident 26 & B)
Findings include:
1. A record ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a safe, clean, and comfortable environment was...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure medications were kept in a locked cart when una...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to ensure the ceiling, oven, counters, and floor were clean and in good condition in the main kitchen; failed to ensure refriger...
Read full inspector narrative →
Apr 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0805
(Tag F0805)
A resident was harmed · This affected 1 resident
Based on record review and interview, the facility failed to provide the appropriate supervision and the appropriate textured diet for 1 of 3 residents reviewed for mechanically altered diets that res...
Read full inspector narrative →
Mar 2023
6 deficiencies
2 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Pressure Ulcer Prevention
(Tag F0686)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident who was admitted with pressure ulcers received ap...
Read full inspector narrative →
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Incontinence Care
(Tag F0690)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure thorough assessments and care was provided for the use of a ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interviews, the facility failed to ensure 2 of 3 residents received written notice of ro...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to monitor and follow physician orders regarding a Wound VAC (vacuum-a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to monitor 1 of 3 residents who were administered a diuretic. ( Reside...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0944
(Tag F0944)
Could have caused harm · This affected 1 resident
Based on record review and interviews, the facility failed to conduct quarterly Quality Assurance and Performance Improvement (QAPI) meetings. This deficient practice potentially affected all 90 resid...
Read full inspector narrative →
Oct 2021
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure residents were able to appeal a facility-initiated transfer ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
2. A record review was conducted, on 9/29/21 at 1:00 P.M., for Resident 32 and indicated his diagnoses included, but were not limited to, chronic obstructive pulmonary disease, post-traumatic stress d...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to ensure a care plan for smoking was developed for 1 of 21 residents whose care plans were reviewed. (Resident 10)
Finding inclu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
2. A clinical record review was completed on 9/2820/21 at 3:07 P.M., and indicated Resident 28's diagnoses included, but were not limited to: dementia, delusional disorder, retention of urine, and hal...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0659
(Tag F0659)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to administer medications per physician orders for 1 of 1 residents reviewed for physician orders (Resident 12).
Findings include:
On 9/28/21 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to follow a physician order regarding range of motion and hand splint application for a resident with a hand contracture. The def...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to follow care planned interventions for falls for 1 of 1 resident reviewed for accidents. (Resident 75)
Findings include:
During...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure Dietician recommendations for supplements were followed up timely for 2 of 7 residents reviewed for nutrition. (Residents 15 and 28)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure cleanliness of the oxygen concentrator and filter for 1 of 1 resident reviewed for oxygen therapy. (Resident 51)
Findin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure physician ordered medications were administered for 1 of 5 residents reviewed for unnecessary medications. (Resident 40)
Finding inc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
2. On 9/28/21 at 3:34 P.M., Resident 12's record was reviewed. Diagnoses included, but were not limited to, paranoid schizophrenia, bulimia nervosa, Parkinson's disease, and muscle wasting and atrophy...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interview and observation, the facility failed to ensure medications were properly stored, labeled appro...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on record review, observation and interview, the facility failed to ensure proper infection control practices were implemented related to not handling medications with an ungloved hand and not f...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. During an observation on 9/27/2021 at 3:16 P.M., Resident 15's nails and hair were dirty.
A clinical record review was comple...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interview and observation, the facility failed to ensure a clean, sanitary and comfortable environment w...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 28% annual turnover. Excellent stability, 20 points below Indiana's 48% average. Staff who stay learn residents' needs.
- • Multiple safety concerns identified: 2 life-threatening violation(s), 1 harm violation(s), $63,174 in fines. Review inspection reports carefully.
- • 50 deficiencies on record, including 2 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $63,174 in fines. Extremely high, among the most fined facilities in Indiana. Major compliance failures.
- • Grade F (4/100). Below average facility with significant concerns.
About This Facility
What is Brickyard Healthcare - Elkhart's CMS Rating?
CMS assigns BRICKYARD HEALTHCARE - ELKHART CARE CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Indiana, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Brickyard Healthcare - Elkhart Staffed?
CMS rates BRICKYARD HEALTHCARE - ELKHART CARE CENTER's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 28%, compared to the Indiana average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Brickyard Healthcare - Elkhart?
State health inspectors documented 50 deficiencies at BRICKYARD HEALTHCARE - ELKHART CARE CENTER during 2021 to 2025. These included: 2 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 1 that caused actual resident harm, and 47 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Brickyard Healthcare - Elkhart?
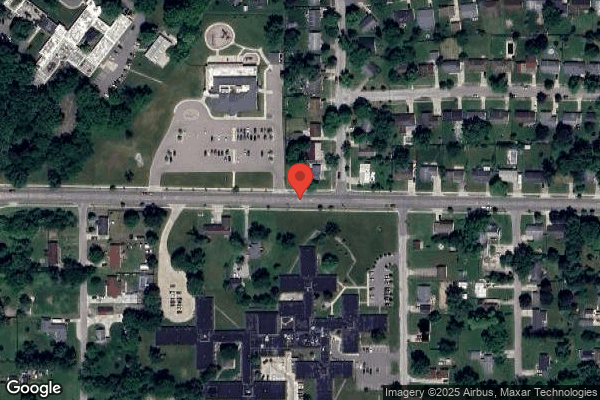
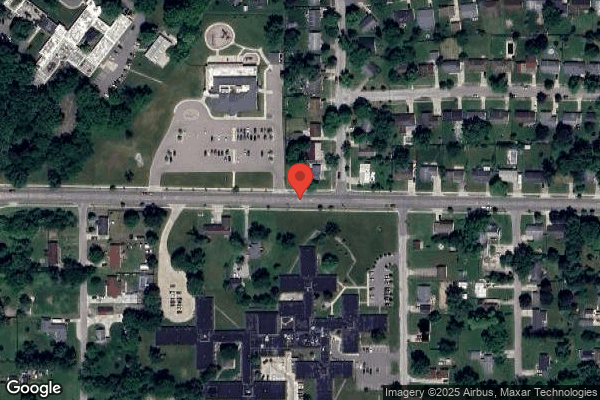
BRICKYARD HEALTHCARE - ELKHART CARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by BRICKYARD HEALTHCARE, a chain that manages multiple nursing homes. With 175 certified beds and approximately 126 residents (about 72% occupancy), it is a mid-sized facility located in ELKHART, Indiana.
How Does Brickyard Healthcare - Elkhart Compare to Other Indiana Nursing Homes?
Compared to the 100 nursing homes in Indiana, BRICKYARD HEALTHCARE - ELKHART CARE CENTER's overall rating (1 stars) is below the state average of 3.1, staff turnover (28%) is significantly lower than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Brickyard Healthcare - Elkhart?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Brickyard Healthcare - Elkhart Safe?
Based on CMS inspection data, BRICKYARD HEALTHCARE - ELKHART CARE CENTER has documented safety concerns. Inspectors have issued 2 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Indiana. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Brickyard Healthcare - Elkhart Stick Around?
Staff at BRICKYARD HEALTHCARE - ELKHART CARE CENTER tend to stick around. With a turnover rate of 28%, the facility is 18 percentage points below the Indiana average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly. Registered Nurse turnover is also low at 25%, meaning experienced RNs are available to handle complex medical needs.
Was Brickyard Healthcare - Elkhart Ever Fined?
BRICKYARD HEALTHCARE - ELKHART CARE CENTER has been fined $63,174 across 1 penalty action. This is above the Indiana average of $33,711. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Brickyard Healthcare - Elkhart on Any Federal Watch List?
BRICKYARD HEALTHCARE - ELKHART CARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.