WILDWOOD HEALTHCARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Wildwood Healthcare Center has received a Trust Grade of F, indicating significant concerns about the facility's quality of care. It ranks #408 out of 505 nursing homes in Indiana, placing it in the bottom half of facilities in the state, and #39 out of 46 in Marion County, meaning there are very few local options that are worse. However, the facility is improving, with issues decreasing from 8 in 2024 down to 2 in 2025. Staffing is a concern here with a low rating of 1 out of 5 stars, and while the turnover rate of 42% is better than the state average, there is less RN coverage than 98% of Indiana facilities, which can impact resident care. Specific incidents of concern include a resident suffering a burn due to improper maintenance of a heating device, another resident falling and fracturing a femur because they did not receive the proper assistance during a transfer, and a delay in addressing complications from a urinary catheter that resulted in hospitalization. Overall, while there are some positive trends, families should weigh the serious deficiencies against the improvements being made.
- Trust Score
- F
- In Indiana
- #408/505
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 42% turnover. Near Indiana's 48% average. Typical for the industry.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Indiana facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 16 minutes of Registered Nurse (RN) attention daily — below average for Indiana. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 51 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (42%)
6 points below Indiana average of 48%
Facility shows strength in quality measures, fire safety.
The Bad
Below Indiana average (3.1)
Below average - review inspection findings carefully
Near Indiana avg (46%)
Typical for the industry
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 51 deficiencies on record
Apr 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident was administered medications per their policy for 1 of 3 residents reviewed for medication compliance. (Resident B)
Find...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a resident was free from verbal abuse by staff for 1 of 3 residents reviewed for abuse. (Resident D)
Findings include:...
Read full inspector narrative →
Oct 2024
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure notification and documentation was provided to Resident 23 regarding a room change for 1 of 1 resident reviewed for room change.
Fi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure accurate care planning of Resident 56's bathing preferences, failed to assist a resident with shaving (Resident 120), ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
2. The clinical record for Resident 14 was reviewed on 10/29/2024 at 11:40 a.m. The medical diagnoses included cerebral palsy.
A Quarterly Minimum Data Set assessment, dated 8/10/2024, indicated Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
2. The clinical record for Resident 99 was reviewed on 10/25/24 at 12:45 p.m. The medical diagnoses included, but were not limited to, quadriplegia, acute infarction of the spinal cord, neuralgia (ner...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident had a care plan to address her individualized needs related to substance use disorder for 1 of 2 residents reviewed for h...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure 1 of 2 medical storage rooms were free of expi...
Read full inspector narrative →
May 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement interventions to eliminate and/or reduce a ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident's wound dressing was completed twice a day per physician's order for 1 of 3 residents reviewed for wounds. (Resident T)
F...
Read full inspector narrative →
Sept 2023
15 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to maintain a resident's dignity regarding possession of medications provided to him by nursing for 1 of 4 residents reviewed fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to protect the resident's right to be free from physical abuse by a resident for 1 of 4 residents reviewed for abuse (Residents 119).
Findin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident's facility-initiated discharge information was conveyed to the resident/resident representative and the discharge summary...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to send a copy of the notice of transfer or discharge to the representative of the Office of the State Long-Term Care (LTC) Ombudsman at the s...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to accurately complete a Preadmission Screening and Resident Review (PASRR) level I for 2 of 2 residents PASRR reviewed. (Resident 64 and Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure a resident had care plans to address her dementia, edema, and hypertension for 1 of 33 residents reviewed for care pla...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident's care plan was reviewed and revised quarterly and/or with significant changes in care by the interdisciplinary team and ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to ensure an orthotic (splint) hand device was provided for 1 of 1 residents reviewed for range of motion. (Resident 47)
Findings...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to honor food choices of a resident for 1 of 1 resident reviewed for choices (Resident 89).
Findings include:
The clinical recor...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, and record review, the facility failed to maintain an infection prevention and control program designed to provide a safe, sanitary and comfortable environment and prevent the tr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Smoking Policies
(Tag F0926)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to ensure residents extinguished cigarettes in proper receptacles. This had a potential to affect 64 of 64 residents that smoke....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected multiple residents
4. The clinical record for Resident 20 was reviewed on 9/7/23 at 2:57 p.m. The Resident's diagnosis included, but were not limited to, hypertension, anxiety, and depression.
A Quarterly MDS (Minimum ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to develop and implement a plan of care for a resident with intermitte...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure medications stored in the medication carts and medication rooms were labeled with the residents' names, dated with open...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure a safe, functional, sanitary, and comfortable environment for residents by: room curtains not properly hung or torn from hooks, holes ...
Read full inspector narrative →
Jun 2023
1 deficiency
MINOR
(B)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Deficiency F0804
(Tag F0804)
Minor procedural issue · This affected multiple residents
Based on observation, interview, and record review, the facility failed to provide palatable, attractive meals to 11 of 143 residents in the facility. (Residents H, J, L, M, N, P, Q, R, and 3 Anonymou...
Read full inspector narrative →
Feb 2023
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on interview and record review, the facility failed to provide a resident with adequate assistance of 2 staff members during a transfer. This deficient practice resulted in a fall with a fractur...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0774
(Tag F0774)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to follow their resident transportation policy when assisting a resident in making transportation arrangements to and from a physician's visit...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Smoking Policies
(Tag F0926)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to implement the facility smoking policy by not assuring residents did not share smoking materials, not assuring a resident was ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, record review, and interview, the facility failed to ensure food was stored and prepared under sanitary conditions related to: trash cans not having tight fitting lids; not label...
Read full inspector narrative →
Mar 2022
21 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Incontinence Care
(Tag F0690)
A resident was harmed · This affected 1 resident
Based on interview and record review, the facility failed to timely identify and address an indwelling urinary catheter complication resulting in hospitalization. (Resident 147)
Findings included:
The...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to do a self-administration assessment for a resident who self-administers medications for 1 of 1 resident randomly observed for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide a working bed control remote for 1 of 6 residents reviewed for environment (Resident 64).
Findings include:
The clini...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to care plan a resident's BKA (below knee amputation) fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. The clinical record for Resident 92 was reviewed on 2/23/22 at 11:50 a.m. The Resident's diagnosis included, but were not lim...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide in room activities of interest for 1 of 4 residents reviewed for activities (Resident 64).
Findings include:
The clin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident 104's clinical record was reviewed on 3/1/22 at 12:25 p.m. Resident 104's diagnoses included, but not limited to, di...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. The clinical record for Resident 149 was reviewed on 2/23/22 at 4:20 p.m. The Resident's diagnosis included, but were not lim...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide timely podiatry services for 1 of 1 residents reviewed for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to assess a resident's capabilities and deficits to dete...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure an additional inner cannula was at the bedside ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to develop an individualized behavior management plan fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to implement non-pharmalogical interventions prior to starting an anti...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0800
(Tag F0800)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a residents food preference was incorporated into their diet for 1 of 2 residents reviewed for choices. (Resident 359)
Findings incl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure a resident received physical therapy services upon re-admission to the facility for 1 of 2 residents reviewed for rehabilitation and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure staff were trained on abuse upon hire for 6 of 10 staff reviewed for abuse training. (CNA-Certified Nursing Assistant 20, CNA 21, CN...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. The clinical record for Resident 113 was reviewed on 2/24/22 at 9:18 a.m. The Resident's diagnosis included, but was not limi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. The clinical record for Resident 149 was reviewed on 2/23/22 at 4:20 p.m. The Resident's diagnosis included, but were not lim...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure food was stored and prepared under sanitary co...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0885
(Tag F0885)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure weekly notifications of the facility's COVID-19 positive status were provided to residents, representatives and families. This had a...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0888
(Tag F0888)
Minor procedural issue · This affected most or all residents
Based on interview and record review, the facility's vaccination policy did not include the process of tracking and securing COVID-19 vaccination status documentation of 2 of 5 staff reviewed for COVI...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Indiana facilities.
- • 42% turnover. Below Indiana's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: Federal abuse finding, 3 harm violation(s). Review inspection reports carefully.
- • 51 deficiencies on record, including 3 serious (caused harm) violations. Ask about corrective actions taken.
- • Grade F (20/100). Below average facility with significant concerns.
About This Facility
What is Wildwood Healthcare Center's CMS Rating?
CMS assigns WILDWOOD HEALTHCARE CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Indiana, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Wildwood Healthcare Center Staffed?
CMS rates WILDWOOD HEALTHCARE CENTER's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 42%, compared to the Indiana average of 46%. This relatively stable workforce can support continuity of care. RN turnover specifically is 57%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Wildwood Healthcare Center?
State health inspectors documented 51 deficiencies at WILDWOOD HEALTHCARE CENTER during 2022 to 2025. These included: 3 that caused actual resident harm, 46 with potential for harm, and 2 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Wildwood Healthcare Center?
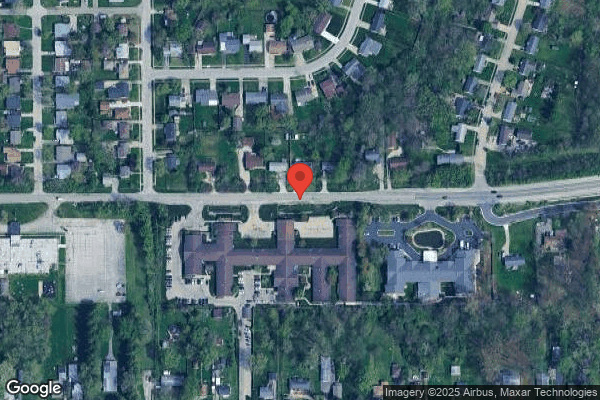
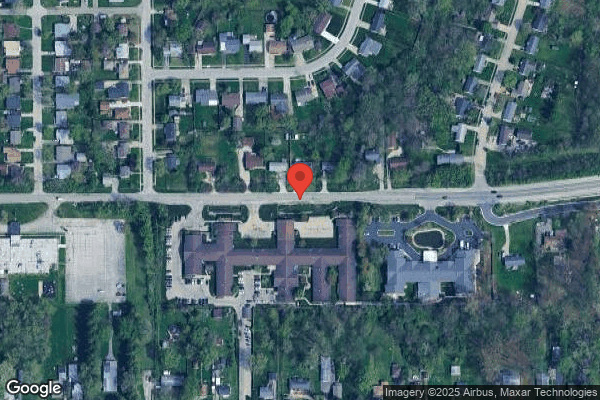
WILDWOOD HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by COMMUNICARE HEALTH, a chain that manages multiple nursing homes. With 160 certified beds and approximately 137 residents (about 86% occupancy), it is a mid-sized facility located in INDIANAPOLIS, Indiana.
How Does Wildwood Healthcare Center Compare to Other Indiana Nursing Homes?
Compared to the 100 nursing homes in Indiana, WILDWOOD HEALTHCARE CENTER's overall rating (2 stars) is below the state average of 3.1, staff turnover (42%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Wildwood Healthcare Center?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the substantiated abuse finding on record and the below-average staffing rating.
Is Wildwood Healthcare Center Safe?
Based on CMS inspection data, WILDWOOD HEALTHCARE CENTER has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Indiana. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Wildwood Healthcare Center Stick Around?
WILDWOOD HEALTHCARE CENTER has a staff turnover rate of 42%, which is about average for Indiana nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Wildwood Healthcare Center Ever Fined?
WILDWOOD HEALTHCARE CENTER has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Wildwood Healthcare Center on Any Federal Watch List?
WILDWOOD HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.