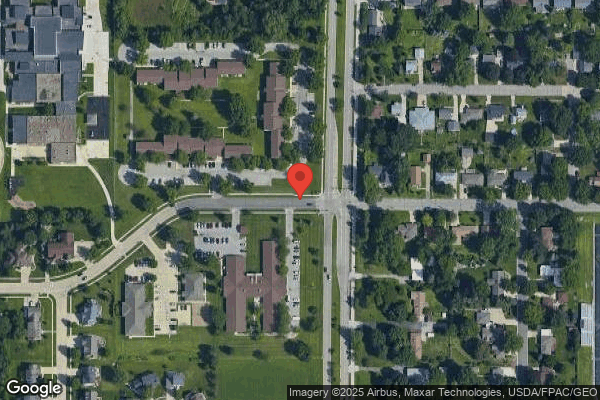
Cedar Falls Health Care Center
Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Cedar Falls Health Care Center has received a Trust Grade of F, indicating significant concerns about the quality of care provided. It ranks #258 out of 392 facilities in Iowa, placing it in the bottom half of all nursing homes in the state, and #9 out of 12 in Black Hawk County, meaning only three local options are worse. The facility is currently improving, with issues decreasing from 18 in 2024 to 2 in 2025. While staffing is a relative strength with a 3/5 rating and 0% turnover, indicating staff stability, the facility has concerning fines totaling $186,966, which is higher than 97% of Iowa facilities. Critical incidents noted include failures to prevent physical abuse among residents and inadequate assessments for necessary care, creating immediate jeopardy to resident safety. Overall, the home has strengths in staffing and quality measures but has serious weaknesses in health inspections and safety protocols.
- Trust Score
- F
- In Iowa
- #258/392
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- Turnover data not reported for this facility.
- Penalties ✓ Good
- $186,966 in fines. Lower than most Iowa facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 40 minutes of Registered Nurse (RN) attention daily — about average for Iowa. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 45 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Iowa average (3.0)
Below average - review inspection findings carefully
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 45 deficiencies on record
Mar 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and staff interviews the facility failed to report within the required time frame an allegation of abuse to Iowa Department of Inspection and Appeals and Licensi...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, facility medical record, family, volunteer, resident, and staff interviews the facility failed ...
Read full inspector narrative →
Dec 2024
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observation, clinical record review, policy review, manufacturer's instructions for use and staff interviews, the facility failed to ensure a medication error rate of less than five percent w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, clinical record review, policy review, and staff interview the facility failed to adhere to infection control practices while administering medication. Observations of the nursin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Based on observation, policy review, and staff interview the facility failed to serve hot food at a temperature of at least 135 degrees Fahrenheit (F) for 1 of 1 test tray requested. The facility repo...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, policy review, and staff interview the facility failed to ensure all staff entering the kitchen had their hair contained in a hair net for 2 of 2 observations. The facility repor...
Read full inspector narrative →
Oct 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0946
(Tag F0946)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on document review, policy review, and staff interviews, the facility failed to ensure door alarm checks and wander guard ...
Read full inspector narrative →
Aug 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, staff and family interview on 7/15/24 the facility failed to make the required notifications for residen...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, staff interview, and facility policy review the facility failed to following medication administration p...
Read full inspector narrative →
Jul 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff interview and policy review, the facility failed to provide services that met professiona...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to provide or offer a shower twice a week for 1 of 3 residents revie...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation and interviews, the facility failed to provide a safe and comfortable environment due to leaks in the ceiling in the hallway entering the main dining room and in the main dining r...
Read full inspector narrative →
Feb 2024
8 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, resident and staff interviews, and policy review the facility failed to assist 1 of 1 residents reviewed...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on interview, record review, and policy review, the facility failed to notify the resident or their representative of the policy for Bed Holds for 1 of 3 resident reviewed (Resident #3). Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to do a PASARR (pre-admission screening and resident review) Level 2 for 1 of 3 residents reviewed (Resident #19). The facility failed to do a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0646
(Tag F0646)
Could have caused harm · This affected 1 resident
Based on record review, staff interviews, and policy review the facility failed to submit a Preadmission Screening and Resident Review (PASRR) for reevaluation when 1 of 2 residents reviewed (Resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review, resident, staff, and Provider interviews, and policy review the facility failed to provide adequate assessment and intervention to 1 of 2 residents reviewed for hospitalization...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, resident, staff, and Provider interview, and policy review the facility failed to maintain records and c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, staff interviews, and policy review the facility failed to maintain records for 1 of 5 residents reviewe...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, staff interviews, and policy review the facility failed to maintain records for 1 of 5 residents reviewe...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, record review, family and staff interview, and facility policy review
the facility failed to provide adequate assessment and timely intervention for 1 of 3 residents reviewed (R...
Read full inspector narrative →
Jul 2023
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff and resident interviews, and observations the facility failed to provide appropriate supe...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff interviews, and observations the facility failed to obtain a discharge order for 1 of 3 d...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff and resident interviews and observations, the facility failed to complete weekly skin ass...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on clinical record review, staff and resident interviews, and observations the facility failed to appropriately secure narcotic medications, failed to complete a shift-to-shift narcotic count an...
Read full inspector narrative →
May 2023
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, interviews, and facility policy review the facility failed to ensure a safe transf...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, record review, staff and resident interview the facility failed to treat each resident with respect and dignity in a manner that promoted or enhanced quality of life for 1 of 4 r...
Read full inspector narrative →
Jan 2023
4 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation and resident and staff interviews, the facility failed to maintain a safe and secure environmental area in resident living spaces. The facility identified a census of 55 residents...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, hospital record review, resident, staff and Nurse Practitioner interviews and faci...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review, hospital record review, resident, staff and Nurse Practitioner interviews and faci...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on observation, clinical record review, resident, staff, and Nurse Practitioner (NP) interviews, and text messages, the facility staff failed to administer medications according to physician ord...
Read full inspector narrative →
Dec 2022
14 deficiencies
3 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, clinical record reviews, facility policy review, resident, and staff interviews, the facility failed to e...
Read full inspector narrative →
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Quality of Care
(Tag F0684)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, clinical record reviews, resident, family, and staff interviews, the facility failed to assess and interv...
Read full inspector narrative →
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident and staff interviews, record review and policy review, the facility failed to provide appropriate...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on clinical record review and staff interviews the facility failed to completely fill out the Skilled Nursing Facility (SNF) Advance Beneficiary Notice (ABN) of Non-coverage form CMS-10055 and N...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review and staff interview the facility failed to develop a comprehensive care plan incorp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, clinical record review and staff interview the facility failed to revise the care plan with a change in be...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. During an observation on 12/8/22 at 12:07 PM Staff O Registered Nurse (RN) completed a dressing change to Resident #5 right f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, staff and resident interviews and policy review, the facility failed to provide qualified ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to limit an as needed (PRN) psychotropic medication order to 14 days without a rational and failed to limit a PRN antipsychotic medicati...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected 1 resident
Based on personnel file review, staff interview and policy review, the facility failed to assure 4 of 6 staff reviewed met the requirement for Mandatory Adult Abuse training (Staff Q, Staff R, Staff S...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 6. The quarterly MDS dated [DATE] revealed Resident #38 had a BIMS score of 15 indicating intact cognition. The MDS documented t...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Transfer Notice
(Tag F0623)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review and staff interview the facility failed to inform the Long-Term Care Ombudsman office of a Resid...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0625
(Tag F0625)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review and staff interview the facility failed to provide a bed hold to 1 of 1 Resident (Resident #14) ...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0838
(Tag F0838)
Minor procedural issue · This affected multiple residents
Based on document review and interview, the facility failed to fully address the resident acuity needs in the facility assessment. The facility identified a census of 55 residents.
Findings include:
D...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 3 life-threatening violation(s), 2 harm violation(s), $186,966 in fines, Payment denial on record. Review inspection reports carefully.
- • 45 deficiencies on record, including 3 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $186,966 in fines. Extremely high, among the most fined facilities in Iowa. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Cedar Falls Health Care Center's CMS Rating?
CMS assigns Cedar Falls Health Care Center an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Iowa, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Cedar Falls Health Care Center Staffed?
CMS rates Cedar Falls Health Care Center's staffing level at 3 out of 5 stars, which is average compared to other nursing homes.
What Have Inspectors Found at Cedar Falls Health Care Center?
State health inspectors documented 45 deficiencies at Cedar Falls Health Care Center during 2022 to 2025. These included: 3 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 2 that caused actual resident harm, 37 with potential for harm, and 3 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Cedar Falls Health Care Center?
Cedar Falls Health Care Center is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by CAMPBELL STREET SERVICES, a chain that manages multiple nursing homes. With 70 certified beds and approximately 39 residents (about 56% occupancy), it is a smaller facility located in Cedar Falls, Iowa.
How Does Cedar Falls Health Care Center Compare to Other Iowa Nursing Homes?
Compared to the 100 nursing homes in Iowa, Cedar Falls Health Care Center's overall rating (2 stars) is below the state average of 3.0 and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Cedar Falls Health Care Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Cedar Falls Health Care Center Safe?
Based on CMS inspection data, Cedar Falls Health Care Center has documented safety concerns. Inspectors have issued 3 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Iowa. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Cedar Falls Health Care Center Stick Around?
Cedar Falls Health Care Center has not reported staff turnover data to CMS. Staff turnover matters because consistent caregivers learn residents' individual needs, medications, and preferences. When staff frequently change, this institutional knowledge is lost. Families should ask the facility directly about their staff retention rates and average employee tenure.
Was Cedar Falls Health Care Center Ever Fined?
Cedar Falls Health Care Center has been fined $186,966 across 2 penalty actions. This is 5.3x the Iowa average of $34,949. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Cedar Falls Health Care Center on Any Federal Watch List?
Cedar Falls Health Care Center is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.