ROSSVILLE HEALTHCARE & REHAB CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Rossville Healthcare & Rehab Center has received a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranking #280 out of 295 facilities in Kansas places it in the bottom half of nursing homes in the state, and #13 out of 15 in Shawnee County suggests only one local option is better. The facility's situation is worsening, with reported issues increasing from 3 in 2024 to 21 in 2025. Staffing is below average, earning 2 out of 5 stars, and while turnover is lower than the state average at 44%, the overall RN coverage is concerning as it is less than 86% of Kansas facilities, meaning residents may not receive the level of monitoring they need. Additionally, the facility has incurred fines totaling $79,034, which is higher than 86% of Kansas facilities and raises red flags about compliance with regulations. Specific incidents of concern include a critical finding where a resident with severe cognitive impairment, who was dependent on staff for assistance, had multiple falls, highlighting a risk for further injury. Another serious incident involved a resident who fell while being lowered from a wheelchair due to staff negligence, resulting in a serious head injury that required hospitalization. These events emphasize the need for improved safety protocols and staff training. Overall, while the nursing home has some staffing stability, the numerous serious deficiencies and poor trust rating warrant careful consideration for families researching care options for their loved ones.
- Trust Score
- F
- In Kansas
- #280/295
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ○ Average
- 44% turnover. Near Kansas's 48% average. Typical for the industry.
- Penalties ✓ Good
- $79,034 in fines. Lower than most Kansas facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 22 minutes of Registered Nurse (RN) attention daily — below average for Kansas. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 57 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (44%)
4 points below Kansas average of 48%
Facility shows strength in fire safety.
The Bad
Below Kansas average (2.9)
Significant quality concerns identified by CMS
Near Kansas avg (46%)
Typical for the industry
Well above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 57 deficiencies on record
Apr 2025
21 deficiencies
1 IJ (1 affecting multiple)
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
- R69's Electronic Medical Record (EMR) from the Diagnosis tab documented diagnoses of dementia (a progressive mental disorder characterized by failing memory and confusion), muscle wasting and atroph...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
The facility identified a census of 74 residents. The sample included 19 residents, with three reviewed for dignity. Based on observation, interview, and record review, the facility failed to provide ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
The facility identified a census of 74 residents. The sample included 19 residents. Based on observation, record review, and interview, the facility failed to ensure staff secured and protected the pr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
The facility identified a census of 74 residents. The sample included 19 residents, with three sampled residents reviewed for nutrition and hydration. Based on observation, record review, and intervie...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** - R6's Electronic Medical Record (EMR) from the Diagnosis tab documented diagnoses of epilepsy (brain disorder characterized by ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility identified a census of 74 residents. The sample included 19 residents, with five residents reviewed for pressure ul...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility identified a census of 74 residents. The sample included 19 residents, with two residents reviewed for positioning ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
The facility identified a census of 74 residents. The sample included 19 residents, with three sampled residents reviewed for nutrition and hydration. Based on observation, record review, and intervie...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility identified a census of 74 residents. The sample included 18 residents, with one resident reviewed for respiratory c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility identified a census of 74 residents. The sample included 19 residents. Based on observation, record review, and int...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
The facility identified a census of 74. The sample included 19 residents, with five sample residents reviewed for unnecessary medications. Based on observation, record review, and interview, the facil...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
The facility identified a census of 74. The sample included 19 residents, with five sample residents reviewed for unnecessary medications. Based on observation, record review, and interview, the facil...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
The facility identified a census of 74 residents. The sample included 19 residents, with four reviewed for reasonable accommodation of needs related to assistive devices. Based on observation, record ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
The facility identified a census of 74 residents. The facility identified 14 residents on Enhanced Barrier Precautions (EBP - infection control interventions designed to reduce transmission of resista...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected most or all residents
The facility identified a census of 74 residents. The sample included 19 residents, and five Certified Nurse Aides (CNA) were reviewed for yearly performance evaluations and the associated in-service ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
The facility identified a census of 74 residents with one kitchen and two dining rooms. Based on observation, record review, and interviews, the facility failed to follow sanitary dietary standards re...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected most or all residents
The facility identified a census of 74 residents. The sample included 19 residents. Based on observations, interviews, and record reviews, the facility failed to conduct a thorough facility-wide asses...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Data
(Tag F0851)
Could have caused harm · This affected most or all residents
The facility had a census of 74 residents. Based on interview and record review, the facility failed to submit complete and accurate staffing information to the federal regulatory agency through Payro...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
The facility identified a census of 45 residents. Based on observations, record reviews, and interviews, the facility failed to maintain an effective quality assessment and assurance (QAA) program to ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected most or all residents
The facility had a census of 74 residents. Five Certified Nurse Aides (CNA) were sampled for required in-service training. Based on record review and interview, the facility failed to ensure that five...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
The facility identified a census of 74 residents. Based on record review and interviews, the facility failed to maintain the posted daily nurse staffing data for the required 18 months.
Findings incl...
Read full inspector narrative →
Aug 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
The facility identified a census of 71 residents. The sample included three residents. Based on observation, record review, and interviews, the facility failed to ensure Resident (R) 1 remained free f...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0941
(Tag F0941)
Could have caused harm · This affected most or all residents
The facility identified a census of 71 residents. Based on record review and interviews, the facility failed to ensure Certified Nurse Aide (CNA) M received the required effective communication educat...
Read full inspector narrative →
Jun 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility identified a census of 70 residents. The sample included three residents. Based on record review and interviews, th...
Read full inspector narrative →
Dec 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility identified a census of 72. The sample included three residents. Based on observations, record review, and interview...
Read full inspector narrative →
Aug 2023
21 deficiencies
3 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** - R38's Electronic Medical Record (EMR) documented R38 had diagnoses of absence of left leg below knee, anemia (deficiency of he...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 70 residents. The sample included 21 residents, with five reviewed for accidents. Based on observat...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
The facility had a census of 70 residents. The sample included 21 residents with six reviewed for nutrition. Based on observation, record review, and interview, the facility failed to follow up and im...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
The facility had a census of 70 residents, with three reviewed for Center for Medicare and Medicaid Services (CMS) Beneficiary Liability notices. Based on record review and interview, the facility fai...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 70 residents. The sample included 21 residents, with one reviewed for restraints. Based on observat...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 70 residents. The sample included 21 residents with one reviewed for abuse. Based on observation, r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 70 residents. The sample included 21 residents with one reviewed for abuse. Based on observation, r...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 70 residents. The sample included 21 residents with one reviewed for hospitalization. Based on obse...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 70 residents. The sample included 21 residents. Based on observation, record review and interview, ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
The facility had a census of 70 residents. The sample included 21 residents with one reviewed for dialysis (the process of removing waste products and excess fluid from the body when the kidneys are n...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 70 residents. The sample included 21 residents, with six reviewed for side rails. Based on observat...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 70 residents. The sample included 21 residents with four reviewed for dementia (group of thinking a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 70 residents. The sample included 21 residents with six reviewed for unnecessary drugs. Based on ob...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 70 residents. The sample included 21 residents with six reviewed for unnecessary drugs. Based on ob...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
The facility had a census of 70 residents. The sample included 21 residents. Based on observation, record review and interview the facility failed to serve Resident (R) 60, on the memory unit, food at...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 70 residents. The sample included 21 residents with one reviewed for urinary catheter (tube inserte...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
- On 08/17/23 at 09:00 AM, observation of Hall 200 medication cart revealed the following:
Omeprazole (antacid or used to treat low magnesium) 20 milligrams (mg) 14 tablets expired 06/2023.
On 08/17/...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
The facility had a census of 70 residents. The sample included 21 residents. Based on record review and interview, the facility failed to use the services of a registered nurse for at least eight cons...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected most or all residents
The facility had a census of 70 residents. The sample included 21 residents. Based on record review and interview, the facility failed to complete performance reviews of all nurse aides, provide regul...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected most or all residents
The facility had a census of 70 residents. Based on record review and interview the facility failed to employ a designated, certified Infection Preventionist who was responsible for the facility's Inf...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected most or all residents
The facility had a census of 70 residents. The sample included 21 residents. Based on record review and interview, the facility failed to complete ensure certified nurse aides (CNA) received the requi...
Read full inspector narrative →
Jul 2023
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility identified a census of 70 residents. Based on observations, record review, and interviews, the facility failed to e...
Read full inspector narrative →
Feb 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
The facility identified a census of 67 residents. The sample included three residents with two reviewed for medication administration. The facility failed to ensure Resident (R) 1 remained free of sig...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
The facility identified a census of 67 residents. Based on observations, record review, and interviews, the facility failed to ensure proper face mask usage during the COVID-19 (an acute respiratory i...
Read full inspector narrative →
Jan 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility identified a census of 64 residents. The sample included three residents. Based on observation, interviews, and rec...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility identified a census of 64 residents. The sample included three residents with all three reviewed for limited range ...
Read full inspector narrative →
Dec 2021
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 61 residents. The sample included 16 residents with one reviewed for discharge. Based on observatio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 61 residents. The sample included 16 residents, with five reviewed for activities of daily living (...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 61 residents. The sample included 16 residents with five reviewed for unnecessary medications. Base...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The facility had a census of 61 residents. The sample included 16 residents with five reviewed for unnecessary medications. Base...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
The facility had a census of 61 residents. The sample included 16 residents. Based on observation, record review, and interview, the facility failed to provide an environment free of accident hazards ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
- 0n 12/09/21 at 08:55 AM, observation revealed Licensed Nurse (LN) I placed the basket with lancets and glucometer (medical device that helps to measure glucose or sugar levels in the blood) directly...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 44% turnover. Below Kansas's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 1 life-threatening violation(s), Special Focus Facility, 4 harm violation(s), $79,034 in fines. Review inspection reports carefully.
- • 57 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $79,034 in fines. Extremely high, among the most fined facilities in Kansas. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Rossville Healthcare & Rehab Center's CMS Rating?
CMS assigns ROSSVILLE HEALTHCARE & REHAB CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Kansas, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Rossville Healthcare & Rehab Center Staffed?
CMS rates ROSSVILLE HEALTHCARE & REHAB CENTER's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 44%, compared to the Kansas average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Rossville Healthcare & Rehab Center?
State health inspectors documented 57 deficiencies at ROSSVILLE HEALTHCARE & REHAB CENTER during 2021 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 4 that caused actual resident harm, 51 with potential for harm, and 1 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
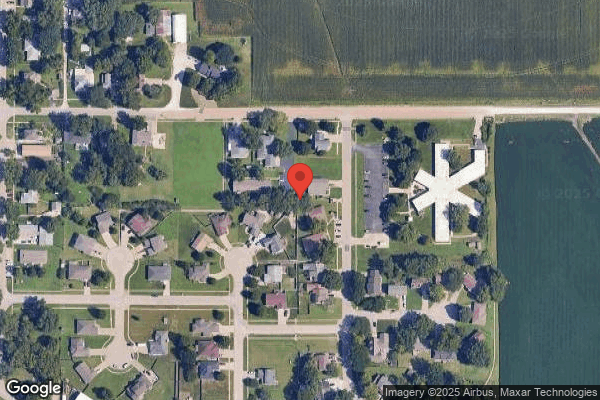
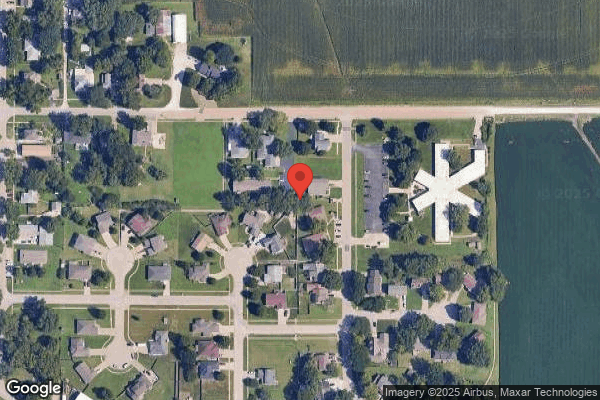
Who Owns and Operates Rossville Healthcare & Rehab Center?
ROSSVILLE HEALTHCARE & REHAB CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by RECOVER-CARE HEALTHCARE, a chain that manages multiple nursing homes. With 81 certified beds and approximately 74 residents (about 91% occupancy), it is a smaller facility located in ROSSVILLE, Kansas.
How Does Rossville Healthcare & Rehab Center Compare to Other Kansas Nursing Homes?
Compared to the 100 nursing homes in Kansas, ROSSVILLE HEALTHCARE & REHAB CENTER's overall rating (1 stars) is below the state average of 2.9, staff turnover (44%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Rossville Healthcare & Rehab Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Rossville Healthcare & Rehab Center Safe?
Based on CMS inspection data, ROSSVILLE HEALTHCARE & REHAB CENTER has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility is currently on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes nationwide). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Kansas. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Rossville Healthcare & Rehab Center Stick Around?
ROSSVILLE HEALTHCARE & REHAB CENTER has a staff turnover rate of 44%, which is about average for Kansas nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Rossville Healthcare & Rehab Center Ever Fined?
ROSSVILLE HEALTHCARE & REHAB CENTER has been fined $79,034 across 4 penalty actions. This is above the Kansas average of $33,869. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Rossville Healthcare & Rehab Center on Any Federal Watch List?
ROSSVILLE HEALTHCARE & REHAB CENTER is currently an SFF Candidate, meaning CMS has identified it as potentially qualifying for the Special Focus Facility watch list. SFF Candidates have a history of serious deficiencies but haven't yet reached the threshold for full SFF designation. The facility is being monitored more closely — if problems continue, it may be added to the official watch list. Families should ask what the facility is doing to address the issues that led to this status.