MEADOW PARK REHABILITATION AND HEALTHCARE CENTER



Inspected within the last 6 months. Data reflects current conditions.
Meadow Park Rehabilitation and Healthcare Center has received a Trust Grade of F, indicating significant concerns about the facility's overall care and management. Ranking #117 out of 219 facilities in Maryland places it in the bottom half, while being #22 out of 43 in Baltimore County suggests only one local option is better. The facility is improving, as it reduced its issues from 16 in 2022 to 8 in 2025. Staffing is a mixed bag; it has a 36% turnover rate, which is below the state average, but the RN coverage is concerning, being lower than 75% of other Maryland facilities. There have been some serious incidents, including a cognitively impaired resident not being monitored properly, which led to an attempted elopement, and an unlocked medication cart that posed a risk of unauthorized access to medications. Overall, while there are some strengths, the significant issues and low trust grade warrant careful consideration.
- Trust Score
- F
- In Maryland
- #117/219
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ○ Average
- 36% turnover. Near Maryland's 48% average. Typical for the industry.
- Penalties ⚠ Watch
- $17,220 in fines. Higher than 91% of Maryland facilities. Major compliance failures.
- Skilled Nurses ○ Average
- Each resident gets 34 minutes of Registered Nurse (RN) attention daily — about average for Maryland. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 48 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (36%)
12 points below Maryland average of 48%
Facility shows strength in quality measures, fire safety.
The Bad
Near Maryland average (3.0)
Meets federal standards, typical of most facilities
10pts below Maryland avg (46%)
Typical for the industry
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 48 deficiencies on record
Jun 2025
8 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, interviews and observations, it was determined that the facility staff failed to adequately monitor a co...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
Based on interviews and medical record reviews, it was determined that the facility failed to implement a process to ensure residents receive written notice of room changes. This was evident for 1 (Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected 1 resident
Based on staff interview it was determined the facility failed to provide residents with access to their funds 24 hours a day/7 days a week. This was found to be evident for 1 of 1 residents that were...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on interviews, observation and record review, it was determined that the facility failed to ensure the residents' personal property was kept from loss. This was evident for 1 (Resident # 65) of ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined that the facility staff failed to report a resident eloped from the facility within the 2-hour allotted timeframe. This deficient practice was ev...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, the facility staff failed to thoroughly investigate a complaint of abuse (Resident #120). This was evident for 1 out of 57 residents reviewed during a com...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to complete a Preadmission Screening and Resident Review (PASRR) II for a resident. This was found to be evident for 1 ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews it was determined that the facility staff failed to ensure a resident's medical record was accurate. This deficient practice was evident for 1 (#217) in 2...
Read full inspector narrative →
Jun 2022
16 deficiencies
1 IJ
CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. On 6/8/22 at 11:30 AM an unlocked medication and unattended (by staff) medication cart was observed with the lock protruding ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to maintain the dignity of residents by leaving Resident #45's face soiled with food after the resident was assisted with a meal and neglecting ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to accommodate the needs of a resident by failing to ensure a resident's call bell was in reach when needed (Residents #9 and Resident #51). Thi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observations and interviews it was determined the facility failed to provide a homelike environment as evidenced by residents having stained linen and soiled equipment in residents' rooms. Th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on administrative record review and interviews with facility staff it was determined the facility failed to complete an investigation into allegations of abuse. This was found to be evident for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview it was determined the facility staff failed to complete a Notice of Transfer when a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined the facility staff failed to ensure comprehensive Minimum Data Set (MDS) assessments were accurately coded. This was evident for 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, it was determined the facility failed to ensure that a resident's care plan intervention was implemented for making sure the call bell was within re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
2. The surveyor conducted an interview with a member of Resident #79's family on 6/10/22 at 1:30 pm. The family member complained that assigned facility failed to provide personal care to the resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review, observations and interview, the facility staff failed to follow a physician's orders by not consistently weighing , and for failing to follow physician orders for the administr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on medical record review, observation and interview it was determined that the facility failed to ensure a supplement was administered to a resident as ordered. This was found to be evident for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on medical record review and staff interview it was determined the facility staff failed to ensure that pharmacist recomm...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews it was determined that the facility failed to properly label and store residents' medicatio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
The facility failed to provide laboratory services to residents (Resident #79). This was evident for 1 of 1 resident investigated for laboratory services in the facility's annual survey.
The findings ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
3. On 6/14/2022 at 10:00 a.m. a review Resident #356's medical record revealed that LPN #29 documented on 2/6/2022 at 4:55 p.m. Resident was alert was alert verbally responsive this morning. She was l...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observations and interviews it was determined the facility staff failed to maintain infection control practices as evidenced by staff not maintaining a resident's oxygen tubing and disposing ...
Read full inspector narrative →
Apr 2019
24 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected 1 resident
Based on review of resident council meeting minutes and interview with residents and facility staff, it was determined the facility failed to give adequate responses to grievances that were presented ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on administrative record review, medical record review and interviews with facility staff it was determined the facility failed to notify the resident representative of a treatment change for a ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews with facility staff and residents, it was determined the facility failed to ensure that residents can submit grievances without fear of reprisal. This was...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) Resident #164 was transferred to the hospital on [DATE]. According to the progress note, a copy of the resident's medication ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview it was determined that the facility failed to ensure the development of a baseline ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
3) Review of the Resident #83's medical record was conducted on 4/9/19. Review of a physician order dated 4/9/19 revealed that the resident had a midline Intra-venous catheter (a soft skinny tube inse...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observations, medical record review and interviews with facility staff it was determined the facility failed to provide individualized activities for residents and failed to assist resident's...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview it was determined that the facility failed to ensure safety precautions were commun...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on medical record review, observation and interview it was determined that the facility failed to ensure supplements were administered to residents as ordered. This was found to be evident for 3...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined that the facility failed to ensure pain medication was administered in a timely manner. This was found to be evident for 1 out...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
Based on interviews with residents, review of resident council meeting minutes and interviews with facility staff it was determined the facility failed to have adequate staff to ensure that response t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on review of medical records and employee files and interviews it was determined that the facility failed to ensure skills competency was demonstrated by newly hired nurses and geriatric nursing...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on review of employee information and interview it was determined that the facility failed to ensure annual evaluations were being completed for nursing staff. This was found to be evident for a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on review of medical records and interview with staff it was determined that the facility failed to have an effective system in place to ensure pharmacist recommendations resulting from identifi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with facility staff it was determined that the facility staff failed to adequately monitor the use of antipsychotic medications used to treat a resident's ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
2) Observations of Nurse #21 and Nurse #2 during the 4/16/19 morning shift to shift medication cart sign out at 7:26 AM revealed that while they were checking the narcotic count for each individual re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observations it was determined the facility failed to consistently maintain a sanitary environment in the kitchen based on 2 random observations. This has the potential to affect any resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0840
(Tag F0840)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interviews with facility staff it was determined the facility failed to provide services from...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
2) Review of the medical record on 4/17/19 at 2:59 PM for Resident #20 revealed a consult completed on 10/15/18 from an Ear Nose and Throat specialist (ENT) with a recommendation to have a hearing tes...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
Based on medical record review and interview with the facility staff it was determined that the facility failed to ensure Minimum Data Set (MDS) assessments accurately reflected the resident's status ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Based on medical record review and interview it was determined that the facility failed to consistently ensure an interdisciplinary team, which included the resident, unit nurse manager, a geriatric n...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
6) Review of Resident #15's care plan on 4/11/19 revealed that a hospice intervention was currently on the care plan. Further review of the medical record revealed that hospice services were discontin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0742
(Tag F0742)
Could have caused harm · This affected multiple residents
Based on clinical records review and interview with the facility staff, the facility failed to ensure when a resident was verbalizing feelings of depression the facility clarified which behavioral hea...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected multiple residents
Based on medical record review and interview with staff it was determined that the facility failed to identify that the wrong dosage of medication was being discontinued which caused the resident to r...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 36% turnover. Below Maryland's 48% average. Good staff retention means consistent care.
- • Multiple safety concerns identified: 2 life-threatening violation(s). Review inspection reports carefully.
- • 48 deficiencies on record, including 2 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $17,220 in fines. Above average for Maryland. Some compliance problems on record.
- • Grade F (34/100). Below average facility with significant concerns.
About This Facility
What is Meadow Park Rehabilitation And Healthcare Center's CMS Rating?
CMS assigns MEADOW PARK REHABILITATION AND HEALTHCARE CENTER an overall rating of 3 out of 5 stars, which is considered average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Meadow Park Rehabilitation And Healthcare Center Staffed?
CMS rates MEADOW PARK REHABILITATION AND HEALTHCARE CENTER's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 36%, compared to the Maryland average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Meadow Park Rehabilitation And Healthcare Center?
State health inspectors documented 48 deficiencies at MEADOW PARK REHABILITATION AND HEALTHCARE CENTER during 2019 to 2025. These included: 2 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 46 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
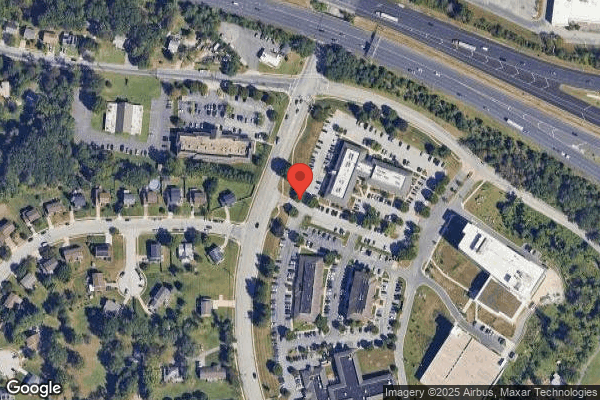
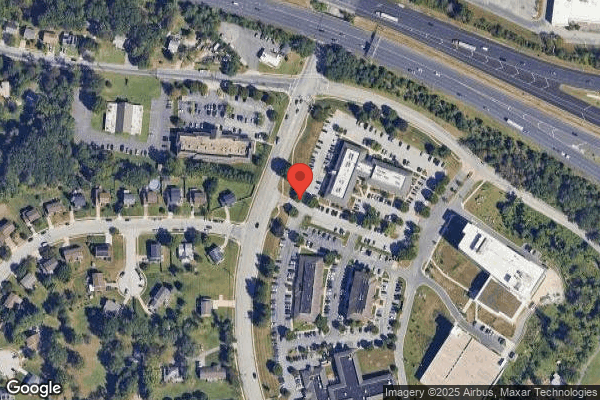
Who Owns and Operates Meadow Park Rehabilitation And Healthcare Center?
MEADOW PARK REHABILITATION AND HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by MARQUIS HEALTH SERVICES, a chain that manages multiple nursing homes. With 120 certified beds and approximately 115 residents (about 96% occupancy), it is a mid-sized facility located in CATONSVILLE, Maryland.
How Does Meadow Park Rehabilitation And Healthcare Center Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, MEADOW PARK REHABILITATION AND HEALTHCARE CENTER's overall rating (3 stars) is below the state average of 3.0, staff turnover (36%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Meadow Park Rehabilitation And Healthcare Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the below-average staffing rating.
Is Meadow Park Rehabilitation And Healthcare Center Safe?
Based on CMS inspection data, MEADOW PARK REHABILITATION AND HEALTHCARE CENTER has documented safety concerns. Inspectors have issued 2 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 3-star overall rating and ranks #100 of 100 nursing homes in Maryland. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Meadow Park Rehabilitation And Healthcare Center Stick Around?
MEADOW PARK REHABILITATION AND HEALTHCARE CENTER has a staff turnover rate of 36%, which is about average for Maryland nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Meadow Park Rehabilitation And Healthcare Center Ever Fined?
MEADOW PARK REHABILITATION AND HEALTHCARE CENTER has been fined $17,220 across 1 penalty action. This is below the Maryland average of $33,251. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Meadow Park Rehabilitation And Healthcare Center on Any Federal Watch List?
MEADOW PARK REHABILITATION AND HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.