SHADY GROVE NURSING AND REHABILITATION CENTER



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Shady Grove Nursing and Rehabilitation Center has received a Trust Grade of D, indicating below-average quality and some concerns about their care practices. They rank #171 out of 219 facilities in Maryland, placing them in the bottom half, and #30 out of 34 in Montgomery County, meaning there are few local options that perform better. The facility is currently worsening, with reported issues increasing from 10 in 2024 to 41 in 2025. While staffing is a relative strength with a 3 out of 5-star rating and a lower turnover rate of 30%, there are significant weaknesses, including a serious incident where a resident suffered a severe fracture due to improper use of a mechanical lift. Additionally, there have been concerns about hand hygiene practices, as staff have been observed not washing hands between assisting different residents, which poses an infection risk. Overall, families should weigh these strengths and weaknesses carefully when considering this facility.
- Trust Score
- D
- In Maryland
- #171/219
- Safety Record
- Moderate
- Inspections
- Getting Worse
- Staff Stability ○ Average
- 30% turnover. Near Maryland's 48% average. Typical for the industry.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Maryland facilities.
- Skilled Nurses ○ Average
- Each resident gets 37 minutes of Registered Nurse (RN) attention daily — about average for Maryland. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 82 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (30%)
18 points below Maryland average of 48%
Facility shows strength in quality measures, fire safety.
The Bad
Below Maryland average (3.0)
Below average - review inspection findings carefully
16pts below Maryland avg (46%)
Typical for the industry
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 82 deficiencies on record
Jul 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0659
(Tag F0659)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to ensure that only qualified staff provided residents with activities of daily living (ADL) care. This was evident for...
Read full inspector narrative →
Jun 2025
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on observation, interview, record review, facility policy review, and review of manufacturer's guidelines for mechanical lifts and for mechanical lift slings, the facility failed to follow the g...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, interview, record review, and facility policy review, the facility failed to assess a resident whose medication was left at bedside and who desired to self-administer medication ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview, record review, facility document review, and facility policy review, the facility failed to ensure nonverbal and/or cognitively impaired residents were assessed during an abuse inv...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record review, facility document review, and facility policy review, the facility failed to ens...
Read full inspector narrative →
Mar 2025
36 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observations and interviews it was determined that the facility staff failed to ensure residents had access to their call bells to notify the staff for assistance when needed. This deficient ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, it was determined that facility staff failed to ensure a resident was dressed in their per...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on record review and interviews it was determined that the facility staff failed to have a system in place to ensure that copies of the resident's Advanced Directives had been obtained and maint...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined that the facility staff failed to ensure a resident received a skilled nursing facility beneficiary notice prior to discharge. This deficient pra...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
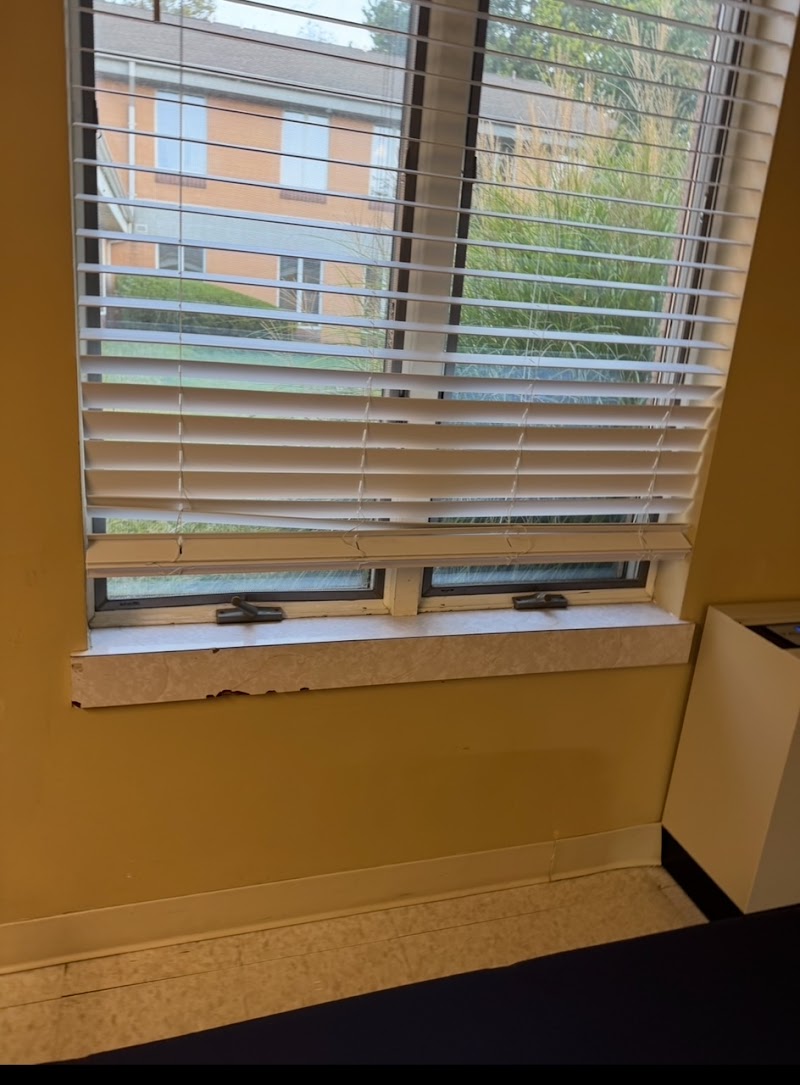
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews it was determined that the facility staff failed to provide a homelike environment for the ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, it was determined that the facility failed to develop and implement written policies and...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on record review and interviews it was determined that the facility staff failed to complete a thorough investigation of alleged incidents of abuse and an injury of unknown origin. This deficien...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, it was determined that the facility failed to include the resident care plan goals w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, it was determined that facility staff failed to provide written notification of tran...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, it was determined that the facility failed to document the orientation and preparati...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and medical record review, it was determined the facility staff failed to notify the resident/resident repres...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, it was determined that the facility failed to ensure a resident's quarterly assessment w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on record review and interview with facility staff, it was determined that the facility staff failed to ensure Preadmission Screening and Resident Review (PASARR) forms were completed correctly....
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0660
(Tag F0660)
Could have caused harm · This affected 1 resident
Based on record reviews and staff interviews, it was determined that the facility failed to assess residents quarterly for discharge planning goals. This deficient practice was evident for 2 (#52, #95...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interviews it was determined that the facility staff failed to ensure residents were receivin...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observations, record reviews, and interviews, it was determined that the facility staff failed to ensure a recommendation for diagnostic testing was completed, a resident was weighed monthly ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on record review and interview with resident and staff, it was determined that the facility failed to reorder a urinary sample for the purpose of diagnosing and treating which caused a delay in ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interviews with resident and staff, it was determined that the facility staff failed to provide additional nourishment to a resident as ordered by the physicia...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on observations, record review, and interviews it was determined that the facility staff failed to failed to ensure each resident has a sufficient supply of prescribed pain medication and ensure...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview with facility staff, it was determined that the facility failed to obtain informed consent prior to the initiation of a resident's bed rails. This was...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0710
(Tag F0710)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview with staff, it was determined that that facility failed to ensure a resident had orders in place to maintain immediate care needs of a resident with ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected 1 resident
Based on record reviews, and interviews, it was determined that facility staff failed to ensure the physician notes reflected a review of the residents total care. This deficient practice was evident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview with staff, it was determined that the facility 1) failed to ensure that an account of all controlled drugs was complete and accurate. This was found...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on medication administration observation, record review, and interviews with staff, it was determined that the licensed facility staff failed to ensure medication error rate of less than 5 perce...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation and interviews with staff, it was determined that the facility failed to ensure that all medications and medical treatment supplies were stored safely and labeled properly. This w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0790
(Tag F0790)
Could have caused harm · This affected 1 resident
Based on observation, medical record review, and interviews it was determined that the facility staff failed to ensure that a resident who had poor dentition received dental services. This deficient p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and interviews, it was determined that facility staff failed to ensure availability of personal protective...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
Based on observations and interviews it was determined that the facility staff failed to make necessary repair in the kitchen. This deficient practice was discovered during the recertification survey....
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected 1 resident
Based on observation, record review and staff interview, it was determined the facility failed to conduct regular inspection of all bed frames, mattresses, and bed rails to identify areas of possible ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
Based on record review and interviews, it was determined that the facility staff failed to notify the state agency of allegations of abuse within the two-hour allotted timeframe. This deficient practi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on record reviews and interviews, it was determined that the facility failed to develop a care plan to manage the resident's new medical diagnosis. This deficient practice was evident for 1 (#25...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
Based on record review and interviews it was determined that the facility staff failed to adhere to professional nursing standards regarding implementing physician orders, medication administration ti...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on observations, record reviews, and interviews with staff, it was determined that the facility failed to ensure precautions were taken for residents' individual safety in need of supervision wh...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observations and interviews it was determined that the kitchen staff failed to store and label food to prevent potential foodborne illnesses, cover their hair to prevent food contamination, a...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on medical record review and interviews it was determined that the facility staff failed to 1) document a resident's personal belongings, 2) failed to maintain medical records in accordance with...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview with staff it was determined that the facility staff failed to: 1) ensure the resident's pe...
Read full inspector narrative →
Mar 2024
10 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0563
(Tag F0563)
Could have caused harm · This affected 1 resident
Based on the review of a complaint, observations, interviews, and review of facility policy, it was determined that the facility failed to have a system in place to allow for visitor access to the fac...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on the review of a complaint, medical record review and interview, it was determined that the facility failed to notify the resident/representative (RP) of a change in condition. This was eviden...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, the facility staff failed to report to the Office of Health Care Quality (OHCQ) an...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview it was determined that facility staff failed to ensure the Preadmission Screening and Resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) Once the facility staff completes an in-depth assessment (Minimum Data Set) of the resident, the interdisciplinary team meet ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview with facility staff it was determined the facility staff failed to ensure preventat...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, the facility staff failed to administer medication as ordered by the physician. Th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
2) On 3/19/24 at 10:51 AM a review of complaint #MD00201930 revealed on 1/26/24 a complaint was received by the state agency. The complaint read that Resident #17 reported to facility staff that s/he ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined the facility failed to maintain complete and accurate medi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0923
(Tag F0923)
Could have caused harm · This affected 1 resident
Based on surveyor observation, it was determined that the facility failed to have adequate ventilation to ensure good air quality circulation to keep all Nursing Units of the facility odor free. This ...
Read full inspector narrative →
Jan 2021
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review, resident and staff interviews, it was determined that the facility staff failed to notify residents' physician and family of a significant weight change. This finding was evide...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility's staff failed to develop and implement a base line care plan for a pressure ulcer. This finding was evident for...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on resident record review and facility staff interview, it was determined that the facility staff failed to develop comprehensive patient centered care plans for 2 of 30 residents reviewed durin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on surveyor observation, resident representative interview and staff interviews, it was determined that the facility's staff failed to provide assistance with activities of daily living to resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on surveyor observation, clinical record review and interviews with facility staff, it was determined that the facility failed to ensure residents were provided with an environment free of accid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record review, resident interview and staff interviews, it was determined that the facility staff failed to address a significant weight loss for Resident #51. This finding was evident for 1 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interviews, it was determined that the facility staff failed to maintain complete and a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the clinical record and facilty staff interview, it was determined that the facility staff failed to review a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0678
(Tag F0678)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor observation, review of the clinical record, and staff interviews, it was determined that facility failed to en...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
4. On 01-15-2021, medical record review of Resident #77 revealed the resident did not receive a 9:00 AM dose of antipsychotic medication (Paliperidone ER Tablet Extended Release 3 mg 2 tabs) on 01-15-...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected multiple residents
Based on observation, clinical record review and staff interview, it was determined that the facility's staff failed to ensure feeding and fluids were administered accurately for 2 of 2 residents sele...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
2. On 01-15-2021, a review of Resident #77's clinical record revealed a physician's order for antipsychotic medication (Paliperidone ER Tablet Extended Release 3 mg, give 2 tabs at 9:00 AM daily) for ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 01-12-2021 at 10:00 AM, surveyor observation revealed Resident #31 had a medical port (med port) implanted in the right ch...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor observation and facility staff interview it was determined that the facility failed to ensure nursing staff ha...
Read full inspector narrative →
Apr 2019
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident and staff interview, surveyor review of the clinical records, it was determined that facility staff failed to ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on surveyor review of the clinical record and facility staff interview, it was determined that the facility staff failed to promptly notify the resident representative or responsible party when ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on family and staff interview, and review of facility policies and personnel files, it was determined that the facility staff failed to revise the abuse, neglect and exploitation policy to refle...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on family and staff interview, and review of facility policy it was determined that the facility staff failed to report an allegation of abuse in a timely manner. This finding was evident for 1 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor observation, family interview, and review of the clinical record it was determined that the facility staff fai...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on surveyor review of the clinical record, it was determined that the facility staff failed to develop a plan of care to address a resident receiving an anticoagulant medication. This finding wa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on surveyor review of the clinical record and interview with facility staff, it was determined that the facility staff failed to ensure the appropriate standards of nursing practice by obtaining...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on surveyor review the clinical record and interviews with the resident and facility staff it was determined that the facility staff failed to follow physician's orders. This finding was evident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on surveyor review of the clinical record and interview of facility staff, it was determined that the facility failed to ensure that PRN (as needed) orders for psychotropic drugs were limited to...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on surveyor observation of medication pass, review of the facility's policy and procedure for medication administration and interview with facility staff, it was determined that licensed facilit...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor observations of medication pass and interview with the facility staff, it was determined that the facility fai...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0840
(Tag F0840)
Could have caused harm · This affected 1 resident
Based on surveyor review of the clinical record and resident and staff interviews, it was determined that the facility staff failed to coordinate care with an ophthalmologist for resident #113. This f...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
3. On 04-11-19, surveyor review of the clinical record for resident #12 revealed no quarterly review of care plans since 10-13-18. In addition, there was no evidence in the clinical record that care p...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on surveyor observation and staff interview it was determined that facility staff failed to follow proper infection control standards by improperly disinfecting glucose testing machines (glucome...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Transfer Notice
(Tag F0623)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor review of the clinical record, interview with resident and facility staff, it was determined that the facility...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Medical Records
(Tag F0842)
Minor procedural issue · This affected multiple residents
Based on surveyor review of the clinical record and interview with facility staff, it was determined that the facility staff failed to ensure accurate clinical documentation in residents' clinical rec...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Food Safety
(Tag F0812)
Minor procedural issue · This affected most or all residents
Based on surveyor observation and staff interviews, it was determined that the facility staff failed to store food under sanitary conditions. These findings were evident during the surveyor's initial ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Maryland facilities.
- • 30% turnover. Below Maryland's 48% average. Good staff retention means consistent care.
- • 82 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade D (45/100). Below average facility with significant concerns.
About This Facility
What is Shady Grove's CMS Rating?
CMS assigns SHADY GROVE NURSING AND REHABILITATION CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Shady Grove Staffed?
CMS rates SHADY GROVE NURSING AND REHABILITATION CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 30%, compared to the Maryland average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Shady Grove?
State health inspectors documented 82 deficiencies at SHADY GROVE NURSING AND REHABILITATION CENTER during 2019 to 2025. These included: 1 that caused actual resident harm, 78 with potential for harm, and 3 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
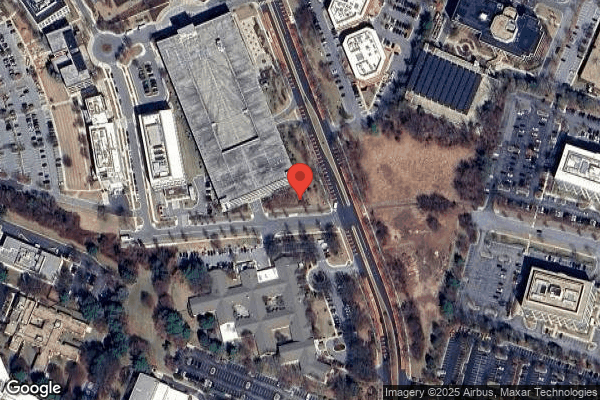
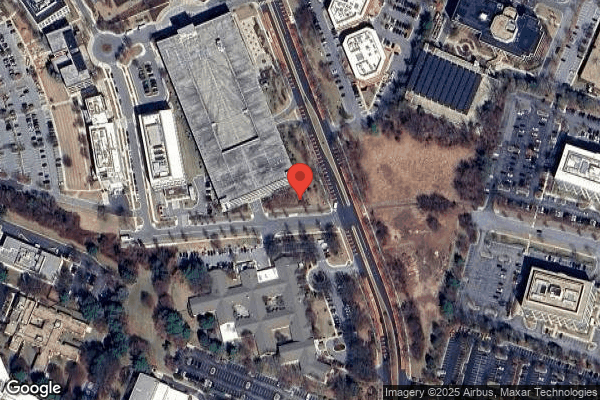
Who Owns and Operates Shady Grove?
SHADY GROVE NURSING AND REHABILITATION CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by LIFEWORKS REHAB, a chain that manages multiple nursing homes. With 144 certified beds and approximately 132 residents (about 92% occupancy), it is a mid-sized facility located in ROCKVILLE, Maryland.
How Does Shady Grove Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, SHADY GROVE NURSING AND REHABILITATION CENTER's overall rating (2 stars) is below the state average of 3.0, staff turnover (30%) is significantly lower than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Shady Grove?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Shady Grove Safe?
Based on CMS inspection data, SHADY GROVE NURSING AND REHABILITATION CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Maryland. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Shady Grove Stick Around?
SHADY GROVE NURSING AND REHABILITATION CENTER has a staff turnover rate of 30%, which is about average for Maryland nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Shady Grove Ever Fined?
SHADY GROVE NURSING AND REHABILITATION CENTER has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Shady Grove on Any Federal Watch List?
SHADY GROVE NURSING AND REHABILITATION CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.