CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0678
(Tag F0678)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, it was determined that the facility failed to have an effective system in place to...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, it was determined that the facility failed to have an effective system in place to correctly identify the appropriate decision maker regarding health care decisions and that the resident/health care decision maker's wishes regarding CPR were clearly documented in the medical record to ensure CPR was performed if needed. This was evident for 4 out 51 Residents, (Resident #328, #30, # 97 #55), reviewed for advanced directives during a survey.
The facility's failure to ensure that each resident had only one active MOLST, led to the determination that immediate jeopardy existed. The facility was notified of this determination on [DATE] at 6:25 PM. Surveyors accepted the facility's plan to remove the immediacy on [DATE] at 11:00PM. The plan was validated, and the immediate jeopardy was removed on [DATE] at 5:05 PM.
The findings include:
A Maryland MOLST, (Medical Orders for Life-Sustaining Treatment) form is used for documenting a resident's specific wishes related to life-sustaining treatments. The MOLST form includes medical orders for Emergency Medical Services (EMS) and other medical personnel regarding cardiopulmonary resuscitation (CPR) and other life-sustaining treatment options for a specific patient. The orders on a MOLST are commonly referred to as code status.
1) On [DATE] at 8:02 AM, a review of medical records revealed Resident # 328, was admitted to the facility for rehabilitation following a hospital stay. Further review revealed a MOLST( MOLST #1) order, dated [DATE].
A review of MOLST #1 revealed that Resident #328 was not to receive CPR ( Do not resuscitate) if the resident experienced cardiac arrest. Continued review revealed the physician obtained the information, not by speaking to the Resident but by communicating with the resident's representative or surrogate.
On [DATE] at 1:45 PM, the Regional Social Worker (Staff # 17) provided an additional MOLST order, (MOLST #2) for Resident #328. Further review of MOLST #2 revealed the MOLST was dated [DATE] and was still active. Further review of the MOLST #2 revealed that Resident #328 was to receive CPR ( full code ) in the event the resident experienced cardiac arrest. Continued review revealed the physician obtained this information by speaking directly to the resident.
Further review of Resident #328's medical record revealed the following orders for the resident's code status:
On [DATE] at 10:28 PM order for full code
On [DATE] at 5:74 PM order for Do Not Resuscitate (DNR)
On [DATE] at 11:29 AM order for Full Code
On 9//13/24 at 5:02 PM DNR/DNI active for one day
On [DATE] at 5:47 PM order for DNR
On [DATE] at 10:14 AM, a review of the Minimum Data Set (MDS) assessment, with an Assessment Reference Date (ARD) of [DATE] section C indicated that the resident did not have any cognitive decline as evidenced by a Brief Interview for Mental Status (BIMS) score of 15 out of 15.
On [DATE] at 10:15 AM, Resident # 328's medical records were reviewed and there was no documentation that the resident was incapable of making health care decisions.
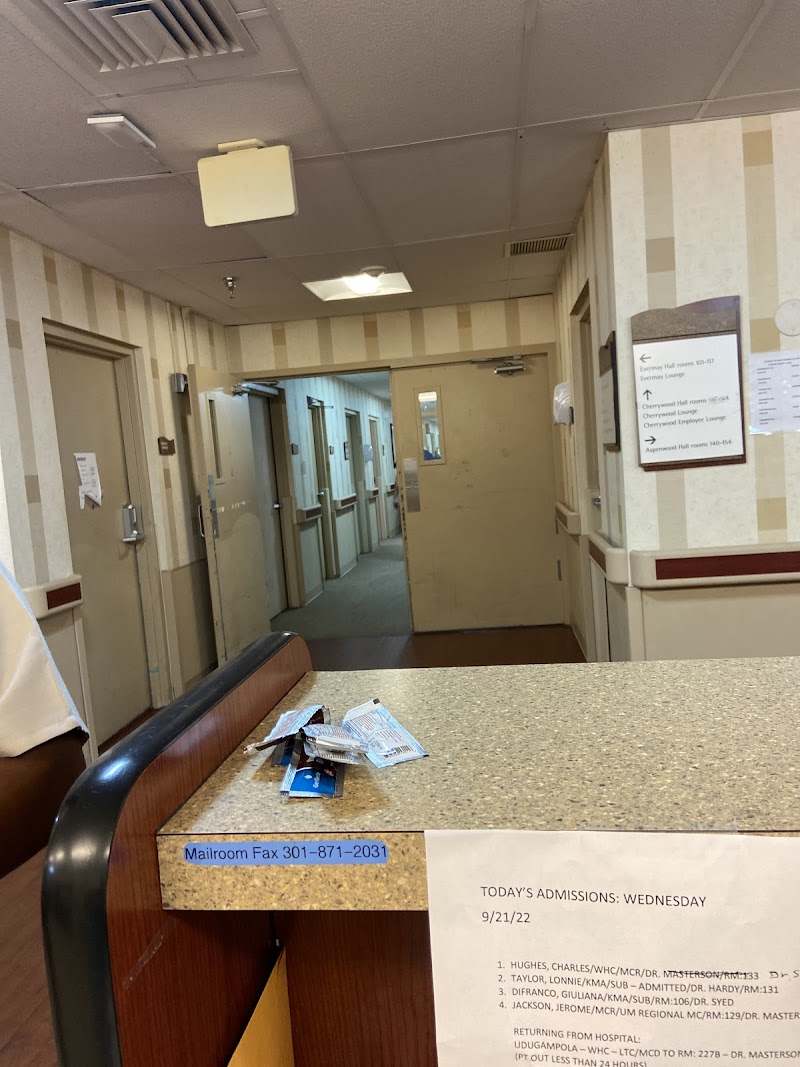
On [DATE] at 1:43 PM, Nurse Staff #18 was interviewed regarding what actions she would take if Resident #328 became unresponsive and was not breathing. During the interview, staff #18 reported she would call for help and request another nurse to verify the code status of resident #328. Staff # 18 reported that the resident's profile page documented full code (perform CPR). Staff # 18 then showed the surveyor a MOLST form on the computer screen. The MOLST form indicated the resident was a DNR. The nurse reported she would follow the MOLST and would not perform CPR. She reported that to further verify the code status of a resident she would refer to the MOLST Binder. Staff #18 reported that the MOLST binder contains all the resident's most current MOLST orders and is kept at the nurse's station.
On [DATE] at 2:29 PM, the Director of Nursing (DON) was interviewed regarding Resident #328 having 2 active MOLSTs with orders that contradicted each other in the medical record. During the interview, she reported that MOLST #1 was completed at the hospital, and sent with the resident to the facility. Additionally, MOLST #2 was completed at the facility. The DON reported that staff should follow the most recent MOLST as indicated by the date on the MOLST. She reported, that a voided MOLST should have a line through it. The DON reported that MOLST #2 was the correct order because it was completed at the facility and therefore more recent than MOLST# 1 which was completed at the hospital.
On [DATE] at 3:13 PM, an interview was conducted in Resident # 328 room with the resident and the resident's family, which included the resident's power of attorney (POA). During the interview, Resident #328 and Resident # 328's POA (Resident's daughter) clearly communicated that the resident did not want CPR if s/he suffered a cardiac arrest.
On [DATE] at 3:17 PM, resident# 328's family member (not POA) reported that he was with Resident # 328 when the resident was admitted to the facility. He reported that he and the resident agreed to receive CPR if s/he suffered cardiac arrest. The next day he realized they made a mistake. He reported he had spoken to a nurse at the nurse's station and told her that Resident # 328's true wishes were to not have CPR performed if s/he suffered a cardiac arrest. He reported that the nurse told him that it was not a problem, and they had the paperwork from the Resident's primary physician indicating that the resident's code status was Do not resuscitate, DNR.
On [DATE] at 2:56 PM, Social Services personnel (Staff #11) were interviewed. During the interview, she reported, that before a care plan meeting for Resident #328, she obtained Resident #328's code status under the profile section in the medical records. Staff #18 reported that she did not actually review the MOLST, and at the time, she did not discuss the code status of Resident #328 with the resident or the resident's family during the meeting.
2) On [DATE] at 10:05 AM, Resident #97 's MOLST order dated [DATE] was reviewed. The review revealed that the residents' wishes were communicated to the physician through the resident's surrogate, per the authority granted by the Health Care Decisions Act. Further review revealed that the resuscitation status chosen was No CPR, DNR option B.
On [DATE] at 10:10 AM, a review of progress notes revealed a social services note, dated [DATE] at 12:39, A review of the note revealed that the Regional Social Worker (Staff #17) contacted resident #97's emergency contact representative to confirm the DNR status on file.
On [DATE] at 10:15 AM, further review of electronic health records failed to reveal certifications of incapacity for Resident #97. The resident's BIMS score was 15/15 indicating the resident was cognitively intact.
On [DATE] at 11:45 AM, During an interview with the medical director, he reported that he is familiar with resident # 97 and his opinion was that the resident has capacity.
On [DATE] at 11:00 AM, the above concerns were discussed with the administrator. He reported that he would reeducate the staff involved and re-audit the residents.
On [DATE] at 4:00 PM, a review of 8 percent of the facility residents failed to reveal any additional issues with residents' MOLST orders.
On [DATE] at 4:48 PM, The administrator reported that the 2 outstanding concerns were corrected.
On [DATE] at 4:50 PM. a review of Resident #97 medical record revealed a new MOLST dated [DATE]. A review of the MOLST revealed that the Medical Director communicated with Resident #97 regarding their wishes. Further review revealed that the residents' wishes were not the same as the resident's representative. The resident wished to receive resuscitative treatment (CPR) if s/he would suffer cardiac arrest.
On [DATE] at 4:50 PM, a review of resident # 97's MOLST revealed that the MOLST certification for the basis of these orders, was the resident and the order was for CPR.
On [DATE] at 4:51 PM, review of the Residents code status listed in the resident profile was a full code.
4) On [DATE] at 1:00 PM, a review Resident #55's electronic medical record (EMR) revealed the resident resided in the facility for long term care since 2020, and, following a brief hospitalization in [DATE], the resident was readmitted into the facility. Review of Resident #55's 5-day assessment with an assessment reference date (ARD) of [DATE] documented Resident #55's BIMS (brief interview for mental status) summary score was 15, indicating the resident was cognitively intact.
Continued review of Resident #55's EMR revealed 3 active MOLST forms; none of the MOLST forms had been voided when a new MOLST had been completed. In the EMR, under the document tab, Resident #55 had 1) an active MOLST signed and dated [DATE] that documented Resident #55 elected, CPR (resuscitation) status, 2) an active MOLST form that was signed and dated [DATE] that documented Resident #55 elected No CPR, Option A-2, Do not intubate (DNI): Comprehensive efforts may include limited ventilatory support by CPAP or BiPAP, but do not intubate, and, 3) Resident #55 had an active MOLST signed and dated [DATE] that documented Resident #55's elected CPR (resuscitation) status was Attempt CPR. None of the scanned MOLST forms had been voided by the practitioner when a new MOLST had been created, indicating the resident's MOLSTs were active. A copy of Resident #55's MOLST forms was requested and provided on [DATE].
Further review of Resident #55's EMR, revealed, on [DATE], at 12:45 PM, in a medical progress note, the physician documented s/he was asked to evaluate advance care planning and MOLST with Resident #55, advance care planning was reviewed, the MOLST reviewed and completed. There was no other documentation in the progress note to indicate the discussion the physician had with Resident #55 which led to the resident's DNR order.
In a medical progress note on [DATE] at 12:49 PM, the physician documented s/he was asked to evaluate advance care planning and MOLST with Resident #55, and advance care planning was reviewed, MOLST reviewed and completed. There was no other documentation in the progress note to indicate the discussion the physician and Resident #55 had which resulted in a change in the resident's wishes for life sustaining treatment, and a new MOLST.
The presence of more than one active conflicting MOLST in Resident #55's medical record, put the staff at risk of failing to accurately confirm the resident's wishes regarding cardiopulmonary resuscitation (CPR) and implement medical treatment based on the resident's wishes.
On [DATE] at 10:51 PM, Staff #20, Licensed Practical Nurse (LPN), Regional Director of Clinical
Reimbursement was made aware of the finding that Resident #55 had more than one unvoided MOLST in his/her medical record and the concern with the resident having more than one conflicting MOLST. Staff #20 acknowledged the concerns at that time, and indicated the administration was aware of the concern with active, conflicting MOLSTS in resident records.
Failures to identify residents that have the capacity (maintain the ability to make their healthcare decisions), failure to honor residents' wishes for life-sustaining treatments, and failure to maintain one accurate MOLST in a resident's medical record, put the resident at risk of not receiving the correct orders for life-sustaining treatments. Immediate action was needed to ensure that residents who wished life-sustaining treatment would receive that treatment if needed and were not just left to die and/or that residents who did not want life-sustaining treatments, did not endure those treatments unnecessarily. As a result of these findings, an Immediate Jeopardy situation was identified on [DATE] at 6:30 PM, and the facility was provided with the Immediate Jeopardy Template at that time.
The facility's failure to ensure each resident had only one active MOLST, led to the determination that immediate jeopardy existed. The facility was notified of this determination on [DATE] at 6:25 PM. Surveyors accepted the facility's plan to remove the immediacy on [DATE] at 11:00PM. The plan was validated, and the immediate jeopardy was removed on [DATE] at 5:05 PM.
The facility submitted a removal plan on [DATE] at 7:43 PM and again on [DATE] at 9:18 PM, which was not accepted. The facility submitted another plan to remove the immediacy on [DATE] at 9:52 PM, which again was not accepted. On [DATE] at 10:40 PM, the administrator provided an additional plan that was accepted by the survey team and OHCQ (The Office of Healthcare Quality) on [DATE] at 11:00 PM.
The following corrective measures were established on [DATE] at 8:50 AM
Social workers will complete a 100% audit of all alert and oriented residents and all non-alert and oriented resident's representative(s) via conversation to ensure they have an active and correct MOLST uploaded in their chart. All old MOLST forms will be voided and uploaded to ensure that the correct MOLST form is followed.
ADON will educate weekend supervisors and 3-11 & 11-7 weekday supervisors on the process of uploading new residents ' MOLST into the electronic healthcare record upon admission.
The Regional Director of Admissions will educate the admissions director and admissions coordinator on the process of uploading new residents' MOLST into PCC upon admission.
The Regional Director of social services will educate social workers to discuss MOLST and code status with residents and/or representative(s) during care plans, that all residents are to have an active and completed and uploaded in their chart, that CPR/DNR status are found in the residents ' chart under the document section and titled active MOLST that any changed MOLST will be voided and reflected on the chart, and that the order for code status matches the MOLST.
ADON will educate licensed nurses and physicians that all residents are to have an active and correct MOLST completed and uploaded in the chart, that CPR/DNR status ' are found in the residents; chart under the document section titled active MOLST, that any changed MOLST will be voided and reflected on the chart, and that the order for code status matches the active MOLST.
On [DATE], the facility provided an audit list of the MOLST forms which was to include all the residents in the facility. An initial review of the audit list failed to reveal 2 current residents (Resident #84, #13).
On [DATE] at 8:50 AM the Administrator was interviewed regarding the audit. During the interview, he confirmed that the audit was not acceptable, since it was incomplete.
On [DATE] at 9:50 am - an updated MOLST Audit list was provided to the survey team from the NHA.
On [DATE] at 10:10 AM, the NHA was interviewed to ask about any additional evidence to be provided, and he said this was the current evidence, and confirmed the previous evidence of education to staff regarding MOLST documentation.
On [DATE] at 10:00 AM, the facility audits were completed as part of their correction plan and were reviewed. A random 10 percent of the facility's residents were reviewed for accurate MOLST forms.
3) On [DATE], a review of Resident #30's medical record revealed a Minimum Data Set assessment, with a reference date of [DATE], that revealed the resident has a BIMS (Brief Interview for Mental Status) of 4/15 indicating the resident had severe cognitive impairment.
On [DATE] at approximately 5:00 PM, review of the electronic health record revealed 4 active current MOLST forms. Three of the MOLSTs, (dated [DATE], [DATE], and [DATE]) included orders for No CPR (DNR) and one (dated [DATE]) included orders to perform CPR (full code).
Further review of the MOLST, dated [DATE] and signed by Physician #31, revealed in the section for Certification for the Basis of these Orders the physician had initialed the section Mark this line if the patient or authorized decision maker declines to discuss or is unable to make a decision about these treatments. This section of the MOLST also included the following: The patient's or authorized decision maker's participation in the preparation of the MOLST form is always voluntary. If the patient or authorized decision maker has not limited care, except as otherwise provided by law, CPR will be attempted and other treatments will be given. The [DATE] MOLST included an order to perform CPR (full code).
Review of the progress note completed by Physician #31 for a visit conducted on [DATE] revealed an acknowledgement that the resident was previously a long term care resident at the facility prior to a recent hospitalization. The progress note also included: Code Status: I reviewed/completed the MOLST form with [name of Resident #30] on [DATE] and the patient is Full Code. Further review of this progress note revealed the resident was alert and oriented x1 and had AMS (altered mental status) -- baseline.
Further review of the medical record revealed a Physician Certification Related to Medical Condition, Decision Making, and Treatment Limitations, dated and signed by Physician #31 on [DATE], which indicated the resident lacks adequate decision making capacity (including decisions about life-sustaining treatments). Further review of the medical record failed to reveal a second certification that the resident lacked decision making capacity, since the [DATE] certification indicating the resident had capacity.
Review of the resident's Advance Directive included the identification of a Health Care Agent and an Alternative Health Care Agent. Both of these agent's contact information was found in the Contacts section of the resident Profile in the electronic health record.
Further review of the medical record failed to reveal documentation to indicate that an attempt was made to consult the resident's healthcare agent prior to establishing the full code MOLST on [DATE].
An interview was conducted with Physician #31 on [DATE] at 2:31 PM. She reported she sees new admissions and follows the resident while at the facility short term, and confirmed she does not see the residents when they are in long term care. When asked about completing a MOLST when a resident is re-admitted , the physician reported in this facility she has to fill out a brand new MOLST everytime the resident is admitted . She reported if the resident obviously has dementia and can't complete the form and no poa [health care agent] is available then the resident would have to be a full code by default. When asked if she looks to see if there is a valid MOLST she responded: if one is available to me. When asked about Resident #30, Physician #31 indicated she did not recall the resident. After surveyor reviewed the concerns related to Resident #30's MOLST, the physician reiterated that this facility requires a new MOLST be completed regardless of the old MOLST.
During the [DATE] interview, when asked about the process of putting the order into the EHR system, the Physician #31 reported there is a binder that we put the signed MOLST into and then the nursing staff put the order into the EHR.
Further review of the electronic health record for Resident #30 revealed an order, dated [DATE] for DNR. This order was signed by Physician #31 on [DATE]. The physician signed the DNR order two days after completing a MOLST which included orders for CPR (Full Code).
Further review of the medical record revealed a Multidisciplinary Care Conference note for a meeting held on [DATE]. Review of this note revealed the resident and the Health Care Agent participated in the meeting. The following was found in the Social Work Summary section: .Resident is alert and oriented x 3. MOLST updated reviewed and on file; Code Status; full code In the last section of this note, labeled Resident/Family Care Level Review, revealed Do Not Resuscitate was checked.
Further review of the EHR revealed an order, dated [DATE] for FULL CODE. This was signed by Physician # 33 on [DATE]. This was two weeks after Physician #31 completed the MOLST with orders for CPR (full code).
On [DATE] at 10:54 PM, surveyor reviewed with the corporate Social Worker #17 the findings that the resident had DNR orders in place until [DATE] despite the MOLST on [DATE] indicating full code, also reviewed the discrepancy in the [DATE] care plan note which indicated the social worker discussed with family and resident that resident was a full code, but at the end of the note DNR was marked. Surveyor also reviewed the concern that there was only one certification of incapacity for the resident with a BIMS of 4. The SW #17 acknowledged the need to re-evaluate the resident's code status.
On [DATE] at approximately 8:30 AM, review of the EHR revealed a note dated and signed by SSD #19 on [DATE] at 3:30 PM that stated: SW [social worker] followed up with [Health Care Agent] from the previous call on [DATE] regarding current code status and [Health Care Agent] requested code status be changed to DNR. Further review revealed a new MOLST, dated [DATE], which indicated that the orders were based on instructions in the patient's advance directive and included orders for No CPR.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, it was determined that the faciltiy failed to have an effective system in place to...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, it was determined that the faciltiy failed to have an effective system in place to ensure code status was discussed with residents and or their responsible party when new MOLSTs were created. This was found to be evident for 3 (Resident #30, #23. #97) out of 17 residents reviewed for code status during the survey. The findings include:
1). A Maryland MOLST, (Medical Orders for Life-Sustaining Treatment) form is used for documenting a resident's specific wishes related to life-sustaining treatments. The MOLST form includes medical orders for Emergency Medical Services (EMS) and other medical personnel regarding cardiopulmonary resuscitation (CPR) and other life-sustaining treatment options for a specific patient. The orders on a MOLST are commonly referred to as code status.
On [DATE] at 10:05 AM, Resident #97's MOSLT order, dated [DATE], was reviewed. The review revealed an order for Resident #97 not to receive CPR (DNR) if s/he should suffer cardiac arrest. Further review revealed the physician did not speak to Resident #97 about their wishes regarding CPR, but only communicated with the resident representative.
On [DATE] at 10:10 AM, review of progress notes revealed a social services note, dated [DATE] at 12:39 PM, that revealed Regional Social worker (Staff # 18) contacted Resident #97 personal representative to confirm the residents DNR status on file. Further review failed to reveal that Resident #97 was consulted.
On [DATE] at 10:15 AM, further review of medical records failed to reveal certifications of incapacity for Resident #97. In addition, the resident's BIMS score was 15/15 indicating s/he was cognitively intact.
On [DATE] at 10:20 PM, during a brief interview with the Administrator, he reported that he would review the Residents MOLST form and code status with the Medical Director.
On [DATE] at 11:45 AM, during an interview with the medical director he reported that he was familiar with resident # 97 and his opinion was that the resident had capacity.
On [DATE] at 4:50 PM,. review of Resident #97 medical record revealed a new MOLST, dated [DATE]. Review of the MOLST revealed that the Medical Director communicated with the Resident #97 regarding his wishes. Further review revealed that the residents' wishes were not the same as the resident's representative and that the resident wished to receive resuscitative treatment (CPR) if s/he would suffer cardia arrest.
2) Review of Resident #30's medical record revealed the resident has resided at the facility for several years and whose diagnoses included, but was not limited to, high blood pressure, kidney disease, major depressive disorder and dementia. Review of the Minimum Data Set assessment, with a reference date of [DATE], revealed the resident had a BIMS (Brief Interview for Mental Status) of 4 indicating severe cognitive impairment. The resident had a brief hospitalization in [DATE] and was then re-admitted to the facility.
Review of the electronic health record revealed that, prior to the hospitalization in [DATE], the resident had orders for No CPR. The most recent MOLST (Maryland Orders for Life Sustaining Treatment) found for the resident prior to [DATE] was documented as having been discussed with the resident and included orders for No CPR (DNR). The resident also had previous MOLSTs from 2020, which were also for No CPR and indicated they were the result of discussion with the residents health care agent as named in the advance directives.
On [DATE], a new MOLST was completed that included orders for CPR (full code). Review of this MOLST revealed it was completed because the patient or authorized decision maker declined to discuss or was unable to make a decision about these treatments. This MOLST was completed by Physician #31.
An interview was conducted with Physician #31 on [DATE] at 2:31 PM . She reported that she sees new admissions and follows the resident while here short term, and confirmed she does not see the residents when they are long term care. When asked about completing a MOLST when a resident is re-admitted , the physician reported that, in this facility she has to fill out a brand new MOLST everytime the resident is readmitted . She reported thst, if the resident obviously has dementia and can't complete the form and no POA [power of attorny/health care agent] is available then the resident would have to be a full code by default. When asked if she looks to see if there is a valid MOLST she responded: if one is available to me. When asked about Resident #30, Physician #31 indicated she did not recall the resident.
Review of the resident's Advance Directive included the identification of a Health Care Agent and an Alternative Health Care Agent. Both of these agents' contact information was found in the Contacts section of the resident Profile in the electronic health record.
No documentation was found to indicate that attempts were made to contact the Health Care Agent prior to changing the resident's code status from No CPR (DNR) to CPR (full code).
Further review of the medical record revealed a Multidisciplinary Care Conference note for a meeting held on [DATE]. Review of this note revealed that the resident and the Health Care Agent participated in the meeting. The following was found in the Social Work Summary section: .Resident is alert and oriented x 3. MOLST updated reviewed and on file; Code Status; full code In the last section of this note, labeled Resident/Family Care Level Review, it was revealed that Do Not Resuscitate (No CPR) was checked.
No documentation was found for the week between the establishment of the full code MOLST on [DATE] and the care plan meeting on [DATE] to indicate the Health Care Agent was informed of the change in code status. Review of the care conference note revealed conflicting documentation regarding the resident's code status.
On [DATE] at 10:01 AM, interview with the current Social Service Director (SSD #19) reported that the resident had dementia and a psychiatric diagnosis and confirmed that she would consult with the Health Care Agent if permission was needed for anything. SSD #19 also reported she had addressed code status with the Health Care Agent in the past and that the resident was a full code.
Further review of the medical record on [DATE] revealed a Discharge Planning Progress Note, written and signed by SSD #19 on [DATE] which stated: Resident has an advance directive of FULL CODE. Resident/family aware. This was more than two weeks after the code status was changed.
3) Review of Resident #23's medical record revealed the resident was admitted in [DATE] after a hospitalization. Review of the [DATE] Minimum Data Set (MDS) assessment revealed the resident was rarely or never understood, had functional limitations in range of motion on both sides for upper extremities (arms) and impairment on one side for lower extremities (legs). The resident was dependent on staff for activities of daily living and for eating. The resident was receiving occupational, speech and physical therapy.
During an interview with the resident's Health Care Power of Attorney (HCPOA) on [DATE] at 1:22 PM revealed concerns regarding not being informed about the resident's care.
On [DATE], further review of the medical record revealed two cerifications that the resident lacked adequate decision making capacity (including decisions about life-sustaining treatments). These incapacity certifications were completed on [DATE] by Physician #56 and on [DATE] by Nurse Practitioner #57.
Further review of the medical record revealed that a MOLST was completed on [DATE] by Physician # 31. In the section for Certification for the Basis of these Orders the physician had initialed the section Mark this line if the patient or authorized decision maker declines to discuss or is unable to make a decision about these treatments.
On [DATE] at approximately 3:10 PM, the Director of Nursing reported that when a resident comes from the hospital, the MOLST from the hospital remains in place until the practitioner updates the MOLST. The practitioner has to re-assess the MOLST, if the resident is not capable they have to review it with the family member.
Further review of the medical record failed to reveal documentation to indicate the resident's medical POA was contacted to discuss the code status when the MOLST was completed on [DATE]. No physician progress note was found to indicate Physician #31 examined or assessed the resident in June, July or August.
Review of the resident's profile section of the electronic health record revealed the name and contact information for the the residents Medical Power of Attorney.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on interview, and observation, it was determined that the facility failed to ensure that a resident received services with dignity. This was evident for 1 (Resident #42), out of 132 residents ob...
Read full inspector narrative →
Based on interview, and observation, it was determined that the facility failed to ensure that a resident received services with dignity. This was evident for 1 (Resident #42), out of 132 residents observed during a survey. The findings include:
On 9/13/24 at 8:33 AM, Resident # 42 was interviewed. During the interview, he reported that sometimes the facility staff entered his room without knocking.
On 9/13/24 at 840 AM, during an interview with Resident #42, a certified nursing assistant (CNA) (Staff #10) entered the room and delivered a lunch tray.
An observation during the interview with Resident #42 on 9/13/24 at 840 AM, failed to reveal that Staff #10 knocked before entering the room.
On 9/13/24 at 9:01 AM, Staff # 10 was interviewed. During the interview, Staff #10 reported that she introduced herself to the resident earlier in the morning, but she confirmed she did not knock when bringing the resident his/her lunch tray. Staff #10 reported that she just found out she had to knock prior to entering a room.
On 9/20/24 10:50 AM, the above concern was discussed with the Administrator and Director of nursing. No additional information was provided.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
2) Resident #24 was admitted to the facility in August of 2024. A review on 9/11/24 at 12:29 PM of the resident's medical records failed to reveal an advance directive.
Subsequent review of Resident ...
Read full inspector narrative →
2) Resident #24 was admitted to the facility in August of 2024. A review on 9/11/24 at 12:29 PM of the resident's medical records failed to reveal an advance directive.
Subsequent review of Resident #24's medical records revealed that s/he was certified by the attending physician as having adequate decision-making capacity on 8/29/24. Furthermore, a review of the resident's care plan indicated that s/he had an advance directive.
On 9/12/24 at 1:37 PM, the Social Services Coordinator (Staff #11) was interviewed. Staff #11 explained the social services department's process with advance directive when a resident is admitted to the facility. Staff #11 reported that she had not handled the advance directives with the residents and that it was the Director of Social Services (Staff #19) who would usually go over the mater with the resident when they are admitted . However, Staff #11 indicated that Staff #19 was currently out on vacation.
Shortly after and during the interview with Staff #11, Staff #19 joined the conversation through telephone conference. Staff #19 reported that the advance directives are discussed with residents within 24 to 48 hours upon admission and documented in assessments under the Discharge planning psychosocial assessment category. She further reported that if a resident had a care plan that indicated that they have an advance directive, then that meant that we were able to obtain one from them.
On 9/13/24 at 9:07 AM, Resident #24's medical records for assessments were reviewed and revealed the Discharge Planning Psychosocial Assessment was highlighted in red and indicated that it was 14 days overdue.
On 9/13/24 at 10:01 AM, Staff #11 was asked to produce a copy of Resident #24's advance directive.
Later on, at 12:57 PM, Staff #11 was approached by the surveyor and was asked about the earlier request for documentation. Staff #11 reported that she reviewed the resident's medical records and was not able to find his/her advance directive. Staff #11 indicated that she spoke with Resident #24's family member who was at the facility and reported that the resident had one and would give the facility a copy.
In another interview with Staff #11 accompanied by the Regional Social Worker and Discharge Planning Specialist (Staff #17) on 9/13/24 at 2:31 PM, both staff were asked, prior to today, do you have documentation that the advance directive was discussed with the resident? Staff #17 provided the surveyor a copy of the Discharge Planning Psychosocial Assessment that was dated 9/13/24 at 1:34 PM. Both Staff #11 and #17 confirmed that the advance directive had not been discussed with the resident prior to today.
On 9/20/24 at 1:29 PM, the concern was discussed with the Director of Nursing (DON) that the facility failed to ensure the resident's right to formulate an advanced directive by failing to provide information to a capable resident. The DON acknowledged the concern.
Based on records review and interviews, it was determined that the facility failed to provide residents with information to formulate an advance directive. This was evident in 3 (Resident #24, #37, #55) of 17 residents reviewed for advance directives.
The findings include:
1). An advance directive is a written statement of a person's wishes regarding medical treatment, often including a living will, made to ensure those wishes are carried out should the person be unable to communicate them to a doctor. It is a legal document in which a person specifies what actions should be taken for their health if they are no longer able to make decisions for themselves because of illness or incapacity.
On 9/17/24 at 2:27 PM, a review of Resident #37's clinical record revealed that there was no documentation related to advance directives. Further review revealed a document written by the facility's Medical Director on 7/18/24 that indicated the resident had capacity to make decisions.
On 9/20/24 at 11:23 AM, another record review revealed a care plan meeting note dated 4/11/24, which contained a discussion regarding Resident #37's code status but did not mention any review of advance directives or offer for the resident to complete an advance directive. A review of the progress notes and Assessments sections of the medical record revealed no additional documentation by social services staff regarding advance directives.
On 9/20/24 at 11:39 AM, an interview with the Director of Social Work (SW #19) was conducted. She said that advance directive information was normally offered and asked for at the time a resident was admitted , but not usually discussed during care plan meetings. When asked if Resident #37 had been asked about Advance Directive information or been offered the information, she replied that the resident preferred that their family was asked about any decisions. When SW #19 was asked to show evidence of this in the clinical record, she could find none, and further confirmed that SW #19 had not had any discussions with Resident #37's family regarding advance directives.
On 9/20/24 at 1:14 PM, an interview with the Director of Nursing (DON) was conducted to review that Resident #37 had not received information regarding advance directives. The DON acknowledged the finding.
3). A review of Resident #55's electronic medical record (EMR) on 9/10/24 at 1:38 PM failed to reveal to reveal evidence that Resident #55 had an advanced directive in place.
On 9/12/24 at 10:20 AM, further review of the EMR revealed Resident #55 resided in the facility for long term care since 2020, and, following a brief hospitalization in the beginning of August 2024, the resident was readmitted into the facility. Review of Resident #55's 5-day assessment with an assessment reference date (ARD) of 8/13/24 documented Resident #55's BIMS (brief interview for mental status) summary score was 15, indicating the resident was cognitively intact.
Continued review of Resident #55's medical record failed to reveal documentation to indicate Resident #55 had an advanced directive, that the resident's right to formulate an advanced directive had been discussed with the resident, or that advanced directives and its provisions were periodically addressed with the resident, as preferences may change over time.
On 9/16/24 at 12:25 PM, the above concerns were discussed with Staff #19, Director of Social Services. At that time, Staff #19 confirmed the above findings, and offered no further comments at that time
The Director of Nurses (DON) was made aware of the above concerns on 9/20/24 at 3:30 PM, and the DON acknowledged the concerns at that time.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined that the facility failed to notify a resident's representative of changes in the resident's treatment. This was found to be evident for ...
Read full inspector narrative →
Based on medical record review and interview, it was determined that the facility failed to notify a resident's representative of changes in the resident's treatment. This was found to be evident for 1 out of (Resident #23) one resident reviewed for notification of change.
The findings include:
During an interview with the resident's Health Care Power of Attorney (HCPOA) on 9/11/24 at 1:22 PM concerns were revealed regarding the HCPOA not being informed about the resident's care.
On 9/17/24, review of Resident #23's medical record revealed the resident was admitted in June 2024 after a hospitalization. Review of the 6/11/24 Minimum Data Set (MDS) assessment revealed the resident was rarely or never understood, had functional limitations in range of motion on both sides for upper extremities (arms) and impairment on one side for lower extremities (legs). The resident was dependent on staff for activities of daily living and for eating. The resident was receiving occupational, speech and physical therapy.
On 9/17/24, further review of the medical record revealed two cerifications that the resident lacked adequate decision making capacity.
On 9/17/24 at 4:02 PM, further review of the medical record revealed a new medication was started on 6/26/24, Metoprolol 12.5 mg two times a day for high blood pressure. No documentation was found to indicate the HCPOA was notified of the start of this new medication.
Further review of the medical record revealed the attending physician changed on 7/1/24. A Medical Discharge Summary progress note was completed by Physician #56 on 7/1/24. No documentation was found to indicate the HCPOA was notified that the attending physician was changing.
On 9/17/24 at approximately 3:10 PM, the Director of Nursing reported that, when there is a change in the primary care provider to a different primary care provider for the health organization who is responsible for initial short term skilled care at the facility, the healthcare organization should contact the other provider. She also reported the prior primary care provider should inform the family of the change.
On 9/18/24 at approximately noon, surveyor reviewed the concerns with the DON regarding the lack of documentation to indicate the HCPOA was notified of the medication change or the change in the primary care provider.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0605
(Tag F0605)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined that the facility administered an intramuscular injection of an antipsychotic medication without adequate indication. This was found to ...
Read full inspector narrative →
Based on medical record review and interview, it was determined that the facility administered an intramuscular injection of an antipsychotic medication without adequate indication. This was found to be evident for one (Resident #30) out of five residents reviewed for unnecessary medication.
The findings include:
1) Review of Resident #30's medical record revealed that the resident had resided at the facility for several years and whose diagnoses included, but were not limited to: high blood pressure, kidney disease, major depressive disorder and dementia. Review of the Minimum Data Set assessment, with a reference date of 6/5/24, revealed the resident had a BIMS (Brief Interview for Mental Status) of 4 indicating severe cognitive impairment.
Review of the medical record revealed that the resident was seen about once a month by either the Psychiatrist #37 or the Psychiatric Nurse Practitioner (NP) #36.
Review of the June 2024 Medication Administration Record (MAR) revealed that the resdient received IM injections of haloperidol (Haldol) and diphenhydramine (Benedryl) on 6/9/24 for aggressive behaviors.
Haldol is an antipsychotic medication. Benedryl is an antihistamine medication.
Review of the Medication Administration Record (MAR) revealed areas for nursing staff to document resident behaviors on the day, evening and night shifts. Review of the MAR revealed staff can document based on the following coding: 1 - compulsive; 2 - pacing continuously; 3 - Continuously screaming and yelling; 4 - danger to others; 5 - danger to self; 6- false beliefs; 7 - finger painting feces; 8 - spitting; 9 - other. On 9/16/24, review of the documentation for this monitoring for June, July, August and September thru the 16th, 2024 revealed only a check mark for each shift.
On 9/16/23 at 3:52 PM, interview with Nurse #8 revealed a check on the behavior monitoring sheets meant that the resident did not display any of those behaviors.
On 9/16/24 at 3:58 PM, interview with the unit nurse manager #12 revealed that, when the nurses see this item on the computer they have to answer yes or no. The unit nurse manager confirmed that the checks indicated the resident was not displaying those behaviors.
Further review of the MAR revealed there was another section to document other psychiatric symptoms: 1- mood swings; 2 - sad; 3 - continuous crying; 4 - withdrawn; 5 - depressed; 6 - angry; 7 - poor eye contact; 8 - other. Review of the nursing documentation from June, July, August and September thru the 16th, 2024 revealed that staff documented every shift either a 0 or an N, thus indicating the resident was not experiencing these symptoms.
During the 9/16/24 interview with the unit nurse manager #12, surveyor reviewed the concern that the documentation did not support the administration of two IM medications in June. At 4:39 PM, the unit nurse manager presented the surveyor with a 6/8/24 change in condition note.
Review of the Change in Condition Evaluation note, with an effective date of 6/8/24 at 7:21 PM, revealed it was signed by Nurse #43. The note indicated it was about behavioral symptoms that had started in the afternoon and that since the change in condition occurred the symptoms had gotten better. The nurse documented the following in the section to summarize: [name of resident #30] was observed verbally abusive and throwing personal items towards [his/her] roommate in their shared room. [Name of resident #30] was highly agitated, and the roommate appeared distressed but physically unharmed. The writer calmly approached [resident #30] maintained a safe distance and used a soft reassuring tone to ask [him/her] step outside from the room and immediately called additional staff support to de-escalate the situation. Successfully separate the resident by escorting [Resident #30] to quiet and secure area. Further review of this note revealed the psychiatrist #37 was notified at 6:40 PM and ordered to transfer the resident out to the hospital, however the resident refused to go to the hospital; psychiatrist #37 was contacted again and gave a STAT order for Haloperidol (Haldol) 2 mg IM (intramuscular injection) and Benedryl 25 mg IM; and additional orders for lab work to be obtained the following day.
STAT orders are to be given right away.
On 9/16/24 at 4:41 PM surveyor reveiwed the concern with the Director of Nursing (DON) that the 6/8/24 change in condition note does not support the need for IM HALDOL and IM Benedryl. The DON indicated she would investigate.
Further review of the medical record revealed a Health Status Note with an effective time of 6/8/24 at 8:14 PM and written by Nurse #29. This note states: Resident exhibited aggressive behavior towards [his/her] roommate, throwing things and using inappropriate words as well. Further review of the note revealed the DON contacted the psychiatrist who gave the order to transfer resident via 911, the Health Care Agent (HCA) was notified and the psychiatrist spoke with the HCA who agreed to the transfer, when 911 arrived the resident refused to go. When the HCA was notified that the resident declined to be transfered the .[name of HCA] stated if my [relationship] decline to go to hospital I cannot forced [him/her]. [Name of Psychiatrist #37] notified and new orders given. Haldol 2 mg IM x 1, Benedryl 25 mg IM X 1 .
Further review of the medical record failed to reveal documentation to indicate the resident was continuing to exhibit aggressive behavior after the resident was seperated from roommate.
On 9/17/24 at 11:31 AM surveyor reviewed the concern with the Director of Nursing that the IM Haldol and the IM Benedryl were administereed without adequate indicate for use. Surveyor requested any additional documentation the facility may have regarding this concern.
On 9/23/24 at 10:40 AM an interview was conducted with the psychiatrist #37, in the presence of the Director of Nursing regarding the orders for the IM medications. The psychiatrist confirmed he would offer a by mouth medication prior to ordering an IM but that it was an emergency call, they had to do something, the psychosis was getting worse and the resident was out of control. He confirmed that he was told at the time the resident was attacking staff. The psychiatrist reports he ordered the Benedryl with the Haldol to avoid side effects of the Haldol. Surveyor reviewed the concern that the note that accompanied the orders failed to include documentation to indicate the resident was attacking staff, or others, after initially being removed from the room with the roommate.
Review of the orders revealed the order for the IM Haldol was put in by Nurse #29 on 6/8/24 at 7:52 PM and included the following instructions: Inject 2 mg intramuscularly one time only for aggressive behavior until 6/8/24 23:59 [11:59 PM]. The order for the IM Benedryl was put in by Nurse #29 at 7:32 PM and included the following instructions: Inject 25 mg intramuscularly one time only for aggressive behavior until 6/8/24 23:59.
Further review of the MAR revealed Nurse #43 administered that the resident's regularly scheduled 9:00 PM oral medications, which included atorvastatin for high cholesterol; depakote for mood stabilization; iron for anemia; and seroquel for psychosis. No documentation was found to indicate the resident refused to take these oral medications on the evening of 6/8/24. No documentation was found to indicate that Nurse #43 administered the IM Haldol or the IM Benedryl.
Further review of the MAR failed to reveal documentation to indicate that the IM Haldol or the IM Benedryl were administered on 6/8/24. The MAR did reveal documentation that both these injections were administered by Nurse #46 at 1:51 AM on 6/9/24. Review of the behavior monitoring documentation on the MAR revealed that Nurse #46 documented that the resident was not displaying behavioral issues during the night shift that started on 6/8/24.
On 9/23/24 at 11:30 AM, surveyor reviewed with Psychiatrist #37 the concern that the order was put in around 7:30 PM on 6/8/24, but the IM injections were not documented as administered until 1:50 AM on 6/9/24 by a different nurse. Psychiatrist #37 indicated that the injections should have been given STAT and questioned if this was just late documentation.
On 9/23/24 at 11:36 AM, review of Nurse #46 punch card information revealed that the nurse was off on 6/7/24. Nurse #46 punched in at 11:40 PM on 6/8/24 and punched out at 7:44 AM on 6/9/24.
On 9/23/24 at 11:44 AM, surveyor reviewed with the DON that the nurses who documented the behaviors on 6/8/24 and obtained the orders did not administer the IM injections and the that the nurse that did administer the injections was not in the facility when the STAT order was given.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on records review and interviews, it was determined that the facility failed to prevent further potential abuse while an investigation was in progress as evidenced by an inaccurate immediate ass...
Read full inspector narrative →
Based on records review and interviews, it was determined that the facility failed to prevent further potential abuse while an investigation was in progress as evidenced by an inaccurate immediate assessment of the alleged victim. This was evident in 1 (Resident #232) of 5 residents reviewed for abuse.
The findings include:
Resident #232 resided in the facility for 20 days. An allegation of abuse on behalf of the resident was reported, related to a facility reported incident (FRI) with intake number MD00208964.
A review of the investigation packet for the FRI was conducted on 9/20/24 at 9:09 AM. The review revealed the different steps the facility took to prevent further potential abuse of an alleged victim including a pain assessment conducted by the Director of Nursing (DON).
The pain assessment with an effective date of 8/20/24 at 4:57 PM indicated the following:
Pain presence: No pain in the last 5 days
Pain frequency: Rarely or not at all
Pain Interference with Therapy activities: Does not apply- have not received rehab in past 5 days
Pain management: On a scheduled pain medication
Comments: Resident denies any pain at this time
A review of Resident #232's electronic Medication Administration Record (eMAR) on 9/20/24 at 9:32 AM, revealed that s/he was on and received an as needed pain medication at least once every day, each time with a pain score ranging from 4/10 to 10/10, since it was prescribed from over 5 days from when the pain assessment was conducted by the DON.
On the same day at 10:06 PM, the Director of Rehab (Staff #27) was interviewed about Resident #232. Staff #27 reported that the resident was receiving rehabilitation services when s/he was in the facility. Staff #27 provided documentation that confirmed Resident #232 was on their case load for 4 weeks from 8/10/24.
On 9/20/24 at 10:59 AM, the DON and the Nursing Home Administrator (NHA) was interviewed regarding the concerns with the pain assessment. The DON reported that she documented that the resident had no pain in the last five days because she focused on the resident's shoulder. When asked about her documentation regarding the resident not receiving therapy in the past 5 days, both staff agreed that the documentation was inaccurate. Also, the pain management was documented inaccurately as the resident was only on an as needed medication regimen, and in the comment section of the assessment, the DON did not indicate that she was only referring to the resident's shoulder. The concern was discussed that an immediate assessment of an alleged victim was done inaccurately to prevent further potential abuse. Both the NHA and DON acknowledged the concern.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to ensure that essential information was provided to emergency department staff when a resident went to the hospital. T...
Read full inspector narrative →
Based on record review and interview, it was determined that the facility failed to ensure that essential information was provided to emergency department staff when a resident went to the hospital. This was evident for 1 resident (Resident #10) of 2 residents reviewed for hospitalization during the recertification survey.
The findings include:
On 9/10/24 at 12:37 PM, a review of Resident #10's medical record revealed a physician's order for an emergency room transfer for abdominal pain on 9/04/24. Further record review revealed a transfer form completed by Licensed Practical Nurse (LPN #34) dated 9/04/24, that contained clinical information regarding the resident's status.
On 9/12/24 at 9:50 AM, Resident #10 was observed in bed but did not respond to the surveyor's spoken greeting. A sign on the wall above the resident's bed indicated that the resident had a device for ASL [American Sign Language] Interpreter. The device was not present in the room, and the resident refused further interaction at that time.
On 9/12/24 at 11:10 AM, a review of Resident #10's clinical record revealed a hospital discharge summary that documented Resident #10 was deaf. A review of the transfer form, dated 9/04/24 and completed by Staff #34, revealed that the section regarding the resident's communication needs was blank. There was no indication on the document that the resident was deaf or used any communication devices.
On 9/17/24 at 11:47 AM, Licensed Practical Nurse (LPN #34) was interviewed and when she was asked to review Resident #10's transfer form documentation, she confirmed that there was no information regarding the resident's deafness or need for communication device on the transfer form.
On 9/17/24 at 1:03 PM, an interview with the Director of Nursing (DON) was conducted. She was informed that Resident #10's transfer form, dated 9/04/24, lacked any information regarding the resident's need for a communication device or ASL interpreter. She was asked to provide any additional evidence that the hospital staff were informed of the resident's communication needs, but none was provided by the end of the survey.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to provide a resident with a notice of transfer when the resident transferred to the hospital. This was evident for 1 r...
Read full inspector narrative →
Based on record review and interview, it was determined that the facility failed to provide a resident with a notice of transfer when the resident transferred to the hospital. This was evident for 1 resident (Resident #10) of 2 residents reviewed for hospitalization. The findings include:
On 9/10/24 at 12:37 PM, a review of Resident #10's medical record revealed a physician order for an emergency room transfer for abdominal pain on 9/04/24. Further record review revealed no Notice of Transfer documents were present.
On 9/17/24 at 11:47 AM, an interview with Licensed Practical Nurse (LPN #34) was conducted. During the interview, Staff #34 reviewed Resident #10's documents and confirmed that there was no transfer notice in the resident's record.
On 9/17/24 at 1:03 PM, an interview with the Director of Nursing (DON) was conducted. She was informed that there was no evidence that a transfer notice was provided to the resident when the resident was transferred to the hospital on 9/04/24. She was asked to provide any additional evidence, but none was provided by the end of the survey.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to provide a resident a bed hold notice when the resident transferred to the hospital. This was evident for 1 resident ...
Read full inspector narrative →
Based on record review and interview, it was determined that the facility failed to provide a resident a bed hold notice when the resident transferred to the hospital. This was evident for 1 resident (Resident #10) of 2 residents reviewed for hospitalization.
The findings include:
On 9/10/24 at 12:37 PM, a review of Resident #10's medical record revealed a physician's order for an emergency room transfer for abdominal pain on 9/04/24. Further record review revealed no bed hold notice in the resident's chart.
On 9/17/24 at 11:47 AM, an interview with Licensed Practical Nurse (LPN #34) was conducted. During the interview, Staff #34 reviewed Resident #10's documents related to the hospital transfer on 9/04/24 and Staff #34 confirmed that there was no bed hold notice in the resident's record.
On 9/17/24 at 1:03 PM, an interview with the Director of Nursing (DON) was conducted. She was informed that there was no evidence that a bed hold notice was provided to the resident when the resident was transferred to the hospital on 9/04/24. She was asked to provide any additional evidence, but none was provided by the end of the survey.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on medical record review, observation, and interviews, it was determined that the facility failed to ensure that Minimum Data Set (MDS) assessments were accurately documented. This was evident f...
Read full inspector narrative →
Based on medical record review, observation, and interviews, it was determined that the facility failed to ensure that Minimum Data Set (MDS) assessments were accurately documented. This was evident for 1 (#107) of 1 resident reviewed for behavior.
The findings include:
The Minimum Data Set (MDS) is an assessment of the Resident that provides the facility with the information necessary to develop a care plan, provide the appropriate care and services to the Resident, and modify the care plan based on the Resident's status.
A record review on 9/16/24 at 11:13 AM found that Resident #107 was admitted to the facility in April 2024. The continued review contained four MDS assessments, dated 4/24/24, 5/23/24, 6/3/24, and 9/3/24, for Resident #107. All the MDS assessments documented in section GG that Resident #107 had an impairment in range of motion (ROM) to both sides of his/her lower extremities.
Observation of Resident #107 on 9/16/24 at 1:16 PM showed the Resident lying supine in bed with knees bent. Staff #8, a licensed practical nurse, was at the Resident's bedside. She reported that the Resident was ambulatory when asked if he/she had any contractions to his/her extremities. Staff #8 then asked the Resident if s/he wanted to walk. The Resident got up from bed and began to walk around by the bedside.
In an interview on 9/16/24 at 1:46 PM, staff #4, the MDS nurse, said that typically, the MDS would be documented with impairment to a resident's ROM after assessing that a resident was unable to his/her limbs. Staff also added that, if a resident were able to ambulate, then impaired ROM to the lower extremities would not be coded on the MDS. Staff #4 confirmed that Resident #107's MDS assessments dated 4/24/24, 5/23/24, 6/3/24, and 9/3/24 were all documented in error.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
Based on records review and interviews, it was determined that the facility failed to ensure that the Preadmission Screening and Resident Review (PASRR) form was completed for a newly admitted residen...
Read full inspector narrative →
Based on records review and interviews, it was determined that the facility failed to ensure that the Preadmission Screening and Resident Review (PASRR) form was completed for a newly admitted resident. This was evident for 1 (Resident #50) of 2 residents reviewed for PASRR.
The findings include:
Preadmission Screening and Resident Review is federally mandated and must be completed for all applicants in nursing facilities which participate in the Maryland Medical Assistance Program regardless of an applicant's payment source. The purpose of the screening is to help ensure that residents are not inappropriately placed in nursing homes for long term care. Everyone who applies for admission to a nursing facility must be screened for evidence of serious mental illness (MI) and/or intellectual disabilities (ID), developmental disabilities (DD), or related conditions.
Resident #50 was admitted in the facility in late 2024. A brief review of the resident's medical record on 9/11/24 at 12:41 PM revealed an incomplete PASRR form, dated 8/22/24.
A subsequent review of the PASRR form of Resident #50 was conducted on 9/13/24 at 10:38 AM. The review revealed that the form had 4 parts:
A. Exempted hospital discharge - indicated that the remainder of the form must be completed as directed.
B. Intellectual disabilities and related conditions - indicated that the resident was not considered to have ID or related conditions.
C. Serious mental illness- this part had 4 questions that were unanswered.
D. Categorical advance group determination- this part had instructions above that stated, if the individual is considered to have MI or ID or a related condition, complete part D of this form. Otherwise, skip part D and sign below; this part was skipped.
The Social Services Director (Staff #19) was interviewed regarding PASRR on 9/16/24 at 10:43 AM. Staff #19 reported that residents who are transferred from hospitals come with a form and indicated that a new one was done in the facility within the 1st week of admission when there was a change in status or if the forms were incomplete.
A review of Resident #50's medical record was conducted with Staff #19, and she confirmed that the PASRR form was incomplete and came from the hospital, and that the facility did not complete a new one during admission. Staff #19 stated, We have a lot of residents that are in and out, but it should have been done.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on review of the medical record and interview with staff, it was determined that the facility staff 1) failed to provide residents/representatives with a copy of their baseline care plan that in...
Read full inspector narrative →
Based on review of the medical record and interview with staff, it was determined that the facility staff 1) failed to provide residents/representatives with a copy of their baseline care plan that included a summary of the resident's medication. This was evident for 1 (#380) of 4 residents reviewed for pain management.
The findings include:
On 9/11/24 at 10:24 AM, during an interview, when asked if the resident or his/her representative received a written summary of the resident's initial care plan along with a summary of the resident's medications since s/he was admitted to the facility, Resident #380 indicated s/he had not, and deferred to his/her family member representative who was present during the interview. At that time, Resident #380's representative stated they had not been given a copy of the baseline care plan, however after requesting a copy of the resident's medications, a copy of the resident's medication list was given to the representative. In addition, the resident and his/her representative stated that the resident's baseline care plan and medications had not been reviewed with them.
On 9/13/24 at 9:00 AM, per the resident representative's request, the surveyor again met with the resident and his/her representative. At that time, the resident and his/her representative expressed concerns about the residents stay and reported that they had not yet spoken to the social worker or anyone else about the Resident #380's plan of care while in the facility, and again reported that they had not been provided with a copy of the resident's baseline care plan.
On 9/19/24 at 10:29 AM, a review of Resident #380's electronic medical record (EMR) revealed that, on 9/5/24 at 8:20 PM, in an Admission/readmission Nursing Collection assessment tool, baseline care plans for Resident #380 had been initiated. Continued review of the medical record revealed a Baseline Care Plan Initiation form, dated 9/6/24 at 5:58 AM, which stated, Baseline Care Plan, 1. Initiation of Baseline Care Plan, which was followed by 3 statements: 1. I have initiated the care plan items included on the admission assessment and completed the baseline care plan, 2. Baseline care plan has been reviewed with the resident/and or responsible party, and 3. Copy of baseline care plan and copy of medications have been given to the resident and or responsible party. Each of the statements were checked, indicating the care plan had been initiated, reviewed with the resident or responsible party, and the resident. There was no other documentation found in the medical record to indicate the baseline care plan and the resident's medications had been discussed with the resident or the resident's responsible party.
The documentation in the Baseline Care Plan Initiation form, contradicted Resident #380's and his/her representative's statement that the facility staff had not reviewed the baseline care plan with them, and that they had not been provided with a copy of the baseline care plan.
On 9/19/24 at 3:40 PM, during an interview, the Director of Nurses (DON) stated the Unit Manager (UM) was responsible for following up with the resident or the resident's representative regarding the baseline care plan, and if the resident was capable, the UM provided him/her with a copy of the baseline care plan and a copy of his/her medications. At that time, the DON was made aware of the above concerns with Resident #380 and his/her responsible party report that baseline care plans were not reviewed with the resident and that the resident had not been provided a copy of his/her care plans. The DON acknowledged the concerns and offered no further comments at that time.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined that the facility failed to ensure that nursing staff did not document administration of g-tube feedings that they had not actually prov...
Read full inspector narrative →
Based on medical record review and interview, it was determined that the facility failed to ensure that nursing staff did not document administration of g-tube feedings that they had not actually provided. This was found to be evident for one (Resident #23) out of one resident reviewed for g-tube feeding.
The findings include:
Review of Resident #23's medical record revealed that the resident was admitted in June 2024 after a hospitalization. The resident's diagnosis included dysphagia which is difficulty swallowing and the resident had a g-tube for the administration of nutrition. The resident was admitted with orders that nothing was to be given by mouth, and a g-tube with orders for bolus feedings of Jevity 1.5 four times a day.
A bolus is when a large amount of feeding is given at one time.
Further review of the medical record revealed there were two different enteral feed (g-tube) orders in effect from 6/6/24 until they were both discontinued on 7/26/24.
The first order, placed on 6/6/24 at 4:22 AM, was for Jevity 1.5 425 ml bolus four times a day every 6 hours per protocol. Review of the Medication Administration Record (MAR) revealed these feedings were scheduled for midnight, 6:00 AM, noon and 6:00 PM. Review of the MAR revealed a check mark to indicate that the 425 ml bolus feed was administered as ordered four times a day from 6/6/24 until the order was discontined on 7/26/24, except for one dose on 7/4/24 at 6 am that was noted to be blank.
The Jevity 1.5 provides 1.5 calories per ml, thus a 425 ml bolus provides 638 calories per bolus and four bolus per day would provide 2550 calories per day.
The second g-tube feeding order was placed on 6/6/24 at 12:51 PM and was for Jevity 1.5 one carton 4 times a day.
Review of the MAR revealed documentation that staff administered one carton of the Jevity 1.5 four times a day at 9:00 AM; 1:00 PM, 5:00 PM and 9:00 PM every day from 6/6/24 until the order was discontinued on 7/26/24.
Further review of the medical record revealed a 7/26/24 registered dietitian (Staff #30) note which documented that the resident's weight on 6/7/24 was 132 lbs and on 7/8/24 the weight was 125 lbs which was considered a significant weight loss. The tube feeding was providing 1420 calories per day and the resident was receiving an additional 180 calories from a supplement which totaled 1600 calories per day. Needs do not appear to be met with current rate as evidenced by wt loss. Recommend changing TF regimen Jevity 1.5 1 carton q3hour [every 3 hours], 6 times a day. The new regimen would provide 2130 calories per day.
Further review of the medical record revealed that a new g-tube order was put in place on 7/26/24 at 2:35 PM for one carton Jevity 1.5 bolus 6x/day. There was a notation that this feeding would provide 2130 cals per day. This order was discontinued on 9/18/24.
On 9/17/24 at 1:10 PM, review of the medical record revealed an order, dated 8/28/24 to hold the 10 AM bolus feed. There was also an order for dysphagia advanced texture diet for lunch only on 8/28/24.
Review of the MAR revealed staff documented the Jevity bolus feeds were administered 6 times a day as ordered every day from 7/27/24 thru 9/17/24, except for two feedings that were due scheduled to be administered on 9/5/24 at 10:00 AM and 1:00 PM. The area to document these feedings were noted to be blank, no documentation to see nurse's note or that these two feedings were held.
Further review of the medical record on 9/18/24 revealed the RD #30 had seen the resident on 9/17/24 and entered a note at 5:31 PM. This note acknowledged that the resident was now receiving lunch only and tube feeding for all other meals. It documented the current tube feeding as being Jevity 1.5 bolus 6 x/day. The note failed to include a notation that there was a current order to hold the 10 AM feeding.
On 9/18/24 10:01 AM, surveyor asked Nurse #59, who was assigned to care for the resident, when the next bolus feed would occur. The nurse reported that the resident was eating now, that s/he gets a bolus at 6 AM the next was not until the evening. She then confirmed that she was not administering the 10 AM or the 1 PM bolus feeds.
Review of the September 2024 MAR revealed that Nurse #59 had documented the 10 AM and 1:00 PM feedings on September 2, 3, 4, 6, 7, 8, 9, 11, 12, 13, 14, 16, and 17. Three other nurses also documented administering the 10 AM dose after the order to hold the 10 dose was in effect.
On 9/18/24 at 10:08 AM, the unit nurse manager #12 reported the resident received bolus feeds and proceeded to check the documentation in the computer. She went on to report the resident gets lunch only and bolus of Jevity 1.5 six times a day. When asked if the 10 oclock feeding was held, the unit nurse manager responded: yes for lunch and then she clarified that the resident was getting 5 bolus. After reviewing the MAR, the unit nurse manager stated: they were signing for it but not giving it and confirmed the order in August to hold the 10 AM feed.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, it was determined that the facility failed to ensure that residents' communication needs were met. This was evident for 1 complaint (#MD00209021) of ...
Read full inspector narrative →
Based on observation, interview and record review, it was determined that the facility failed to ensure that residents' communication needs were met. This was evident for 1 complaint (#MD00209021) of 5 complaints reviewed during the recertification survey. This had the potential to affect all deaf residents.
The findings include:
On 9/10/24 at 12:14 PM Resident #10 was observed in bed with their eyes closed and appeared to be asleep. A sign above the resident's bed indicated to use an interpreter line IVR instructions and included a company name - o, which indicated to call a phone number and say the language and the call would be connected to an interpreter. A second sign on the wall indicated that to communicate using ASL [American Sign Language] to request a tablet from Admissions, go to the interpreter app, choose the video button, hit the call button and the app would search for a live interpreter. The bottom of the sign stated Staff, tablet must be returned to Admissions once patient discharges. No such tablet was observed in the resident's room.
On 9/12/24 at 8:03 AM, a review of complaint # MD00209021 revealed multiple concerns regarding Resident #10's care that related to the resident's inability to communicate with staff.
On 9/12/24 at 8:07 AM, in an interview with the complainant via deaf relay service, the complainant reported that Resident #10 had multiple needs that were not met due to the lack of communication with the facility staff.
On 9/12/24 at 9:50 AM an interview was attempted with Resident #10 who was sitting in bed eating. The surveyor showed the resident their state surveyor identification badge and the resident made a writing gesture in the air. The surveyor pointed to the sign regarding the tablet for a video interpreter, and the resident shook their head to indicate no. There was no paper in the resident's room to write a note.
On 9/12/24 at 10:40 AM in another attempt to interview Resident #10, the surveyor provided a pad of paper and pen, and the resident wrote need interpreter and law. The surveyor wrote a note that the surveyor nurse was investigating the communications concerns and other issues. A Licensed Practical Nurse (LPN #8) was in the room and when asked she said that the resident's IVR device was downstairs because it was not working. LPN #8 left the room and came back with a piece of paper, but the resident refused further interview. LPN #8 was interviewed in the hallway and said the IVR tablet was in the admissions office since the device was not charging properly.
On 9/12/24 at 11:10 AM, a review of Resident #10's care plan revealed a problem for risk for complications related to impairment of communication. The associated interventions lacked any information regarding the use of a live video interpreter using a tablet device, the use of a white board, or the use of pen and paper to communicate with the resident.
On 9/12/24 at 2:06 PM, an interview with the Director of Nursing (DON) was conducted. The DON said Resident #10 was non-compliant with using the video interpreter device and instead used written notes to communicate. When asked why the communication strategies were not listed on the resident's care plan, the DON did not answer.
On 9/18/24 at 11:09 AM, an interview with the Admissions Director (Staff #34) and Assistant Admissions Director (Staff #35) was conducted by telephone. Staff #34 said that when Resident #10 was admitted , the Admissions office gave the resident a facility-owned iPad which had the interpretation software downloaded on it. She explained that the device was placed in the resident's room and instructions were posted on the wall, and the resident was also provided with pen and paper, and a white board. Staff #34 described how the software worked to easily connect to a live ASL video interpreter. When asked why the device was not in the resident's room, Staff #34 said that there was an error logging in and that the software crashed on us. When asked how long the device had been unavailable, Staff #34 said almost a month, and Staff #35 said about a week and a half. When asked if there was any alternative provided by the interpretative service, they both said no.
On 9/18/24 at 11:31 AM the surveyor called the company that managed the software to confirm the software problem that Staff #34 had reported. A voice message was left with technical support.
On 9/18/24 at 12:39 PM, an email was received from the company in response to the voice message left by the surveyor, and an email reply was sent to ask if the software had not worked in the past week and a half.
On 9/18/24 at 12:59 PM an email reply was received from a complany representative which stated There have not been any disruptions to the interpretaive service in that timeframe.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on medical record review, and staff interviews, it was determined the facility staff failed to ensure that dependent resident's personal hygiene needs were adequately met by providing incontinen...
Read full inspector narrative →
Based on medical record review, and staff interviews, it was determined the facility staff failed to ensure that dependent resident's personal hygiene needs were adequately met by providing incontinent care in a timely manner. This was evident for 1 (Resident #16) out of 132 residents reviewed during the survey process.
The finding include:
On 9/17/24 at 5:40 AM, an observation was made of the second-floor nursing units.
On 9/17/24 at 5:44 AM, an observation revealed the call light flashing above Residents #16's room, along with an accompanying audible alarm.
On 9/17/24 at 5:51 AM, an observation was made of the Assistant Director of Nursing (ADON) entering Residents #16's room.
On 9/17/24 at 5:51AM, an observation was made of the call light turned off and the ADON exiting the room.
On 9/17/24 at 5:52 AM, Resident #16 was interviewed. During the interview s/he reported that s/he had first put her call light on at 5:10 AM. Resident #16 stated that the nurse came in shortly after 5:10 AM and told her/him that he would get someone to come in and assist her/him. Resident #16 reported that s/he told him s/he need to be changed and requested that he not turn off the light when he left. Resident #16 reported that the nurse stated it was company policy to turn off the light. In addition, s/he reported that the ADON just came in a turned off the light and said she would get someone to help her. Resident #16 reported that s/he had been sitting in their stool for 40 minutes.
On 9/17/24 at 6:00 AM, an observation was made of nighttime nurse supervisor RN (Staff # 38) entering Residents #16 room.
On 9/17/24 at 6:05 AM, Nurse RN (Staff # 39) was interviewed. During the interview he confirmed that the Resident #16 put her/his call light on around 5:10AM and that he did go in and turn it off. Also, Staff #38 reported that he told her/him that he would get a nursing assistant (CNA) to come and assist her.
On 9/17/24 at 6:20 AM, an observation was made of the nighttime nurse supervisor (Staff # 38) exiting Resident #16 room.
On 9/17/24 at 6:20 AM, during a brief interview was conducted with the nighttime nurse supervisor (Staff # 38). During the interview she reported that she just provided incontinent care to Resident #16 who was incontinent of bowel and bladder.
On 9/17/24 at 9:05 AM, Resident #16 Material Data Set section GG, dated 8/28/24 was reviewed. The review revealed the resident was always incontinent of bowel and bladder and that the resident was dependent on staff for toiletings needs. Continued review of section C revealed that the Resident was assessed to have a BIMS of 15. (BIMS of 15 indicates no cognitive decline)
On 9/17/24 at 7:3 AM, the ADON was interviewed regaridng a resident waiting 50 minutes to be changed after reporting to a nurse that they needed incontinent care. During the interview she reported the time frame goal for the staff to answer a residents call light is 5 minutes. She reported that the expectation is that staff answer call lights and determine the urgency of the request, and it's okay to have someone come back in a few minutes and assist the resident. The ADON reported that it is her expectation that a resident does not sit in a stool soiled brief for more than 10 minutes, due to the risk of skin breakdown in the perineal area.
On 9/20/24 at 10:25 AM, The surveyor requested the facility call light policy.
On 9/20/24 at 10:29 AM, The Nursing Home administrator reported that the facility did not have a call light policy.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on record review, observations and interviews, it was determined the facility failed to accurately assess the presence of pressure injuries and implement pressure prevention therapies. This was ...
Read full inspector narrative →
Based on record review, observations and interviews, it was determined the facility failed to accurately assess the presence of pressure injuries and implement pressure prevention therapies. This was evident for 2 (Resident #328, #109) out of 5 residents reviewed for pressure injuries. The findings include:
1.On 9/11/24 at 8:02 AM, a review of medical records revealed that Resident # 328 was admitted to the facility for rehabilitation following a hospital stay.
On 9/11/24 at 2:59 PM, review of orders for Resident #328 failed to reveal any orders for pressure preventions.
On 9/12/24 at 8:06 AM, a review of Resident # 328's hospital discharge summary revealed a list of discharge conditions. Review of the discharge instructions failed to reveal that Resident had a pressure injury.
On 9/12/24 at 8:09 AM, a review of the medical records titled admission Nursing/readmission Collection Tool, with an effective date of 8/31/2024 6:10 PM, revealed a section to document a skin observation. Review of the skin observation section revealed that a head to toes skin assessment was completed for Resident #328. Further review failed to reveal any pressure injuries of skin discoloration in the sacral area.
On 9/12/24 at 8:11 AM, a review of the medical records titled Skilled Daily Observations, with the effective date of 8/31/20 9:47 PM, revealed a section to document skin conditions and interventions provided during the shift. Further review revealed a question on the form: does the resident have a pressure injury? The question was answered, no. Continued review failed to reveal any pressure injury preventions or interventions that were provided.
On 9/12/24 at 8:16 AM, a review of the medical records titled Skilled Daily Observations with an effective date of 9/1/24 10:13 PM, revealed a section to document the skin conditions and interventions provided during the shift.? Further review revealed, a question on the form: does the resident have a pressure injury? The question was answered, no. Continued review failed to reveal any pressure injury prevention interventions were provided or that a wound was present.
On 9/12/24 at 8:27 AM, a review of the medical records titled Skilled Daily Observations with an effective date of 9/2/24 at 9:39PM, revealed a section to document skin conditions and interventions provided during the shift. Further review revealed a question on the form: does the resident have a pressure injury? The question was answered no. Continued review failed to reveal any pressure injury prevention interventions were provided.
On 9/12/24 at 8:30 AM, a review, of the medical records titled Skin Observation Tool-V2 with an effective date 9/3/24 at 13:26 AM and completed by the facilities wound nurse (Staff #41), revealed that Resident #328 had a stage 2 pressure injury on the sacrum (buttocks area).
On 9/12/24 at 8:35 AM, a review of the medical records titled Skilled Daily Observations with an effective date of 9/4/24 at 11:36PM, revealed a section to document skin conditions and interventions provided during the shift. Further review revealed a question on the form: does the resident have a pressure injury? The questions was answer, no. Continued review of the pressure injury preventions/interventions provided during the shift were listed as; pressure reducing device for chair, pressure reducing device for bed, and with turning and repositioning.
On 9/12/24 at 8:27 AM, a review of the medical records titled Skilled Daily Observations with an effective date of 9/5/24 at 10:12 PM, revealed a section to document skin conditions and interventions provided during the shift. Further review revealed a question on the form: does the resident have a pressure injury? The answer was recorded as no. Continued review failed to reveal that any pressure injury prevention or interventions were provided.
On 9/11/24 at 2:55 PM, review of the material data set (MDS) assessment, dated 9/6/2024, revealed that Resident #328 had a stage 2 pressure injury. Further review revealed that the pressure injury was present upon admission.
On 9/12/24 at 9:00 AM, the MDS coordinator was interviewed regarding the wound being documented as being present on admission. During the interview, she reported that she used the information based on the wound nurse's documentation completed on 9/3/24. She reported that she did not use the information from the admission skin assessment completed on 8/31/24 (the date of admission).
On 9/12/24 at 9:48 AM, the wound care nurse LPN (Staff # 41) was interviewed. During the interview, she reported that the expectation is that the nursing staff can identify and document any concerns with skin integrity. She reported that, if a nurse is unable to determine the exact stage of a pressure injury, the nurse should have described the wound by location, size, color, open or closed, and odor. This observation should have been documented and reported to the wound nurse. The wound nurse reported that the nurse admitting the resident to the facility can request wound prevention orders from the physician. She reported that her expectation of orders for a suspected pressure injury would include, an order for turning and repositioning and a supportive mattress. On 9/12/24, Review of Wound assessment report from Nurse Practitioner Staff #45) dated 9/9/24, revealed that the residents wound was documented as a stage 3 pressure injury.
A stage 2 pressure injury is when there is a partial thickness loss of dermis (skin) presenting as a shallow open ulcer with a red or pink wound bed, without slough or bruising. May also presents an intact or open/ruptured blister.
A Stage 3 A pressure injury where there is full thickness tissue loss. Subcutaneous fat may be visible,
but bone, tendon, or muscles not exposed. Slough may be present but does not obscure the depth of tissue loss.
On 9/13/24 at 8:12 AM during a brief interview, the Wound Care Nurse (staff #41) confirmed that there were no pressure injury prevention orders for Resident #323 prior to 9/12/24.
On 9/20/24 at 10:50 AM, the above concerns were discussed with the administrator and the Director of Nursing. No additional information was provided to the survey team.
2. On 9/10/24 10:23 AM, an observation of Resident #109's, a long-term resident of the facility, room was made. The observation revealed that a pair of green heel protection boots (used for heel pressure relief) were in the resident's closet. Further observation revealed a very thin pillow under residents' legs with the residents' heels laying against the bed.
On 9/10/24 at 10:24 AM, during a brief interview with Resident's #109 family member he/she reported that the staff have never put the green booties on the resident.
On 9/11/24 at 10:23 AM, an observation was made of Resident # 109 in her bed supine with head of bed elevated about 30 degrees. The green heel protection booties were not on the resident and the Resident' s heels were laying against the bed. The resident's family was in the room and reported: that is how s/he has been lying this way all day and that the booties are in closet.
On 9/11/24 at 3:00 PM, an observation was made in Resident # 109 room. Observation revealed the residents heals were against laying against the bed and the green heel protection booties were in the closet.
On 9/12/24 at 10:55 AM, review of orders revealed an order with a start date of 7/12/14 for Heel boots to bilateral feet as resident allows, while in bed. Remove every shift and assess skin for any deconditioning of current sites or new areas of concern.
On 9/16/24 at 4:00 PM, an observation in resident #109 room was made. Observation revealed a pair of green heel protection booties in the closet. Further observation revealed resident laying in bed with heels laying against the bed.
On 9/19/24 at 12:33 PM, an observation in resident #109 room was made. Observation revealed a pair of green booties in the closet. Further observation revealed resident laying in bed with heels laying against the bed and bed linen.
On 9/19/24 at 12:34 PM, Nurse RN (Staff # 48) was interviewed. She reported that she has regularly provided care to Resident # 109. She reported that she did not know if the resident had an order for bilateral heel protection boots and needed to check.
On 9/19/24 at 12:46 PM, nurse RN (Staff #48) reported that the resident does have boots but she does not have them on because they are in the laundry.
On 9/19/24 at 12:42 PM, the first floor Unit Manager RN (Staff # 14) and surveyor, made an observation of the laundry room to look for Resident # 109's boots. The observation of the laundry room failed to reveal Resident #109s green heel protection booties. Laundry manager said there were no green heel protection booties in the laundry.
On 9/19/24 at 12:44 PM, the laundry manager (Staff #49) reported there were no heal boots in the laundry.
On 9/19/24 at 12:48 PM, Staff #48 and the surveyor made an observation of Resident #109s room. Observation revealed a pair of green booties in the closet. Further observation revealed staff #48 taking the boots out of the closet and attempting to put them on the resident. However, the resident refused to wear the heel boots.
Review of progress notes from 9/10/24 to 9/19/24 at 12:00 PM, failed to reveal documentation that the resident refused wearing the green heel protection booties.
9/12/24 at 9:48 AM, the Wound Care Nurse, LPN (Staff # 41) was interviewed. During the interview she reported that the green heel protection booties were used as a device to prevent pressure injuries on the heels. Her expectations were that the nursing staff would notify her if residents refused to comply with pressure injury prevention therapies such as wearing heel protection booties. Staff #41 continued: if a resident refuses a pressure injury prevention therapy, that alternative therapies would be tried.
On 9/20/24 at 10:50 AM, the above concerns were discussed with administrator and the Director of Nursing. No additional information was provided to the survey team.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, it was determined that the facility failed to develop a care plan to ensure that a...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, it was determined that the facility failed to develop a care plan to ensure that advances in mobility that were achieved during therapy were maintained. This was found to be evident for one (Resident #23) out of three residents reviewed for falls during the survey. The findings include:
Review of Resident #23's medical record revealed that the resident was admitted in June 2024 after a hospitalization. Review of the 6/11/24 Minimum Data Set (MDS) assessment revealed that the resident had functional limitations in range of motion on both sides for upper extremities (arms) and impairment on one side for lower extremities (legs). The resident was dependent on staff for activities of daily living. The resident was receiving occupational, speech and physical therapy in June.
On 9/17/24 at 1:58 PM, review of the medical record failed to reveal a Multidisciplinary Care Conference note that would indicate a care plan meeting had occurred during the resident's admission.
On 9/18/24 at 10:17 AM, the unit nurse manager #12 was interviewed. During this interview she reported the resident was finished with physical therapy but was unable to provide information regarding what therapy's recommendations were upon dishcarge and stated: I can't see the note. She confirmed the resident was continuing to receive occupational and speech therapy.
On 9/18/24 at 10:29 AM, the Rehab Director #27 was interviewed. When asked how information from the therapist were conveyed to nursing staff when discharged , the Rehab Director reported that it was verbal and that they would occasionally do an inservice. When asked about a restorative nursing program, the Rehab Director reported they did not have a restorative nursing aide.
On 9/18/24 at 11:00 AM, the Rehab Director presented the surveyor with the resident's physical therapy Discharge summary, dated [DATE]. The Rehab Director reported that the resident had made great progress in therapy and at the time of discharge, the resient's gait distance (walking) was 125 feet with hand held assist and could transfer from chair to bed and bed to chair with contact guard.
A transfer with contact guard assist means the care giver places one or two hands on the resident to help with balance but no other assistance is provided.
When asked if the ability to walk and transfer with contact guard was reflected in the resident's care plan, the Rehab Director replied: it might be. When asked if the resident should continue to walk, the Rehab Director reported that because of cognitive deficits, this would not be realistic to maintain but that theortically could have been walking to the dining room. Surveyor clarified that the resident could be doing some walking, to which the Rehab Director responded: yes, [s/he could] with support obviously. The Rehab Director indicated that therapy personnel would be part of a care plan meeting for a short term (skilled) admission.
On 9/18/24, after requesting documentation from the Director of Nursing of any care plan meetings that occurred for the resident, staff provided a note completed by the unit nurse manager titled Care plan meeting dated 9/3/24 that stated: Care plan meeting held with resident's [family members]. Resident medications reviewed with no concerns voiced. Plan of care continues.
No documentation was found to indicate who attended the 9/3/24 meeting other than the family and the unit nurse manager who wrote the note. No documentation was found to indicate that members of the interdisciplinary team attended the meeting, or provided input. No documentation was found to indicate that a respresentative from the therapy department attended or provided input for the 9/3/24 care plan meeting.
Review of care plan addressing the resident's risk for falls revealed a revision date of 9/13/24. The interventions included, but were not limited to : Resident is a hoyer lift transfer with 2 GNAs. This intervention was created and initiated on 8/14/24.
A hoyer lift is a mechanical lift used for residents who are completely dependent on staff for transfers. A hoyer lift pad is placed under the resident and then attached to the lift. Two staff members would then use the mechanical lift to raise the resident from the bed and transfer to a chair or vice versa.
During the 9/18/24 11:00 AM interview, surveyor reviewed with the Rehab Director that the current care plan indicated the resident required a hoyer lift with 2 GNA assist, in place since 8/14/24. The Rehab Director responded: could have been at that time. Surveyor also reviewed the concern that the unit nurse manager was unable to verbalize any recommendations made by therapy.
Further review of the 8/27/24 Physical Therapy Discharge summary revealed Prognosis to Maintain CLOF [current level of function] = Excellent with strong family support, excellent with consistent staff support. Depsite indicating strong family and consistent staff support, the discharge recommendation failed to include recommendations for either the family or staff to assist the resident in maintaining the current level of functioning. In the sections for Restorative Program and Functional Maintenance Program the Physical Therapist documented : Not Indicated at this time. The documented Discharge Recommendation was Quarterly assessment to improve/maintain highest levels of functional mobility.
On 9/18/24 at 11:52 AM, the unit nurse manager #12 reported the resident does stand with one person assist and in regard to walking, she reported: if we see [him/her] get up, we walk around with [him/her]. The unit nurse manager indicated they did conduct staff training but confirmed it was not documented. Surveyor reviewed the concern that the care plan still stated the resident required a hoyer lift for transfers, the unit manager indicated she would update this information.
On 9/18/24 at 12:11 PM, when asked if the facility has any restorative nursing, the Director of Nursing responded: No.
On 9/18/24 at approximately 12:45 PM, the Rehab Director presented the surveyor with a form that he reported was just created to help facilitate communication with nursing staff regarding a resident's status when a resident is discharged since they (nursing) are unable to access rehabs notes.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observations, and interviews, it was determined that the facility failed to have a system in pla...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observations, and interviews, it was determined that the facility failed to have a system in place for monitoring residents who have been identified as high risk for elopement. This was evident for 1 (#59) of 6 residents reviewed for accidents.
The findings include:
The Minimum Data Set (MDS) is an assessment of the Resident that provides the facility with the information necessary to develop a care plan, provide the appropriate care and services to the resident, and modify the care plan based on the Resident's status.
A care plan is a guide that addresses each Resident's unique needs. It is used to plan, assess, and evaluate the effectiveness of the Resident's care.
A medical record review for Resident #59 on 9/18/24 at 10:45 AM showed that Resident #59 had been residing in the facility since May 2020. Diagnoses included Schizophrenia (a chronic mental illness that affects a person's thoughts, feelings, and behaviors). The review also noted that Resident #59 was able to ambulate independently.
Continued review contained a care plan focus for Resident #59 that stated that the Resident is at risk for elopement related to Schizophrenia. The review also found an MDS assessment for Resident #59 dated 8/3/24, which had documented that the Resident had severely impaired cognition.
Further review contained an elopement risk tool assessment, dated 8/8/24, for Resident #59.
An elopement risk tool assessment helps determine who is at risk of leaving the facility without supervision. It is scored by adding up the scores assigned to each assessed area. 0 - 7 is low risk, 8 - 9 means at risk for elopement/exit seeking, and 10 is above High Risk.
The assessment documented that Resident #59 Has history of elopement/exit seeking (past hospitalization or history from resident/family) and scored a 10, meaning s/he was above high risk for elopement/exit seeking.
Observation of Resident #59 on 9/18/24 at 10:48 AM noted him/her off the 2nd-floor unit where s/he resided. The Resident was sitting on a couch in the lounge on the 1st-floor unit hallway leading to the front desk and not wearing any monitoring device. The Resident stated, I'm waiting here to go home. Resident #59 could neither state his/her room number nor the name of the facility where s/he resided. The Resident seemed confused.
In an interview on 9/18/24 at 10:50 AM, staff #22, a certified nurse aid, was asked to name all the residents on the second-floor unit who were at high risk for elopement. Staff #22 responded that Resident #59 was at high risk for elopement because s/he was confused and always going downstairs.
In an interview on 9/18/24 at 11:25 AM, staff #12, a unit manager, stated that a wander guard bracelet for monitoring was placed on any resident identified as high risk for elopement. Staff #12 also added that the Resident's name with their picture would be placed on the elopement list at the front desk. However, the interview failed to show that staff was monitoring Resident #59 for exit-seeking behaviors, and a review of the elopement binder at the front desk did not include his/her name and picture.
In an interview on 9/18/24 at 12:17 PM, the director of nursing stated that the facility placed a wander guard bracelet only on residents who exhibited exit-seeking behaviors.
However, the interview failed to show that the facility was monitoring Resident #59 for exit-seeking behaviors even though an earlier review of Resident #59's elopement risk tool assessment dated [DATE] contained documentation that s/he had Has history of elopement/exit seeking (past hospitalization or history from resident/family).
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to identify a resident with a critically low body mass index (BMI) and failed to have a policy and procedure in place t...
Read full inspector narrative →
Based on record review and interview, it was determined that the facility failed to identify a resident with a critically low body mass index (BMI) and failed to have a policy and procedure in place to measure residents' height. This was evident for 1 resident (Resident #17) of 5 residents reviewed for nutrition during the recertification survey and had the potential to affect all residents.
The findings include:
Body Mass Index (BMI) is a measurement of weight relative to height. It is used as a reliable screening measure for underweight, overweight, or obesity.
On 9/11/24 at 9:34 AM, a review of Resident #17's weight and height documentation in the electronic record revealed:
Weight
9/05/24 = 105.7 lbs Mechanical Lift
8/05/24 = 106.4 lbs Mechanical Lift
7/30/24 = 106.1 lbs Mechanical Lift
7/23/24 = 106.0 lbs Mechanical Lift
Height
7/23/24 = 61.0 inches lying down
12/16/16 = 72.0 inches Standing
12/08/16 = 72.0 inches Standing
On 9/16/24 at 3:41 PM in an interview with the Director of Nursing (DON), she was asked about the difference in Resident #17's height in 2024 and 2016 and she was asked what process the facility used to measure residents' height. She said she was not sure and would check. When she was asked about the staff who documented the height of 61 inches, she replied that the staff no longer worked at the facility.
On 9/19/24 at 2:12 PM another interview was conducted with the DON regarding the discrepancy in Resident #17's height documentation. She agreed to check the resident's height that day. The surveyor asked to speak to the dietitian, and the DON said the dietitian (Staff #30) was not in the building today but would be here tomorrow.
On 9/19/24 at 2:45 PM, the DON brought a copy of the facility's weight monitoring and tracking policy and said the facility does not have a policy for measuring residents' height. She also said she measured the resident's height today using a tape measure that she had in her hand and said the resident's height was 70 inches. The dietitian's (Staff #30) phone number was requested, provided, and a voice message was left.
On 9/20/24 at 9:16 AM, an interview with the Regional Dietitian (Staff #24) was conducted. She said that she was a contractor employed by NutraCo, employed since 9/09/24, and started work at the facility on Wednesday 9/18/24. When she was asked if dietitians made in person visits to residents, Staff #24 refused to answer the question and instead explained that the company had a hybrid program and offered to provide the policy.
A review of Resident #17's dietitian progress note, dated 9/16/24, and written by Staff #30, was conducted with
Staff #24. Staff #30 had documented that the resident's BMI was 20, and weight was 106 lbs. When Staff #24 reviewed the resident's weight history, Staff #24 stated that the resident's weight was stable since July 2024 and this was the indicator used to determine treatment. When Staff #24 was asked to review the resident's height documentation, she noticed the discrepancy between 61 inches and 72 inches documented. When asked what Resident #17's BMI would be for a height of 70 inches (the height the DON measured on 9/19/24) and a weight of 106 lbs, Staff #24 calculated that Resident #17's BMI was actually 15.
On 9/20/2024 at approximately 11:00 AM, Staff #24 provided surveyors with hybrid policy and procedure for the dieticians at the facility and she also reported that the dietician, Staff #30, no longer worked at the facility as of 9/19/24 and provided the surveyor with the phone number of the director of Nutraco for any questions. A review of the hybrid policy revealed no clarification on whether dietitians made in person visits to residents.
On 9/20/24 at 10:34 AM, a telephone interview was conducted with the Medical Director who was also Resident #17's attending physician. He said that the dietitian was responsible for monitoring residents' nutritional status and for entering the appropriate orders and treatments. He also said that he relied on the dietitian to bring any concerns to the weekly risk meetings, and that in between meetings, the dietitian would call him and made recommendations. The Medical Director reviewed Resident #17's weight and height entries, acknowledged the discrepancies, and then was informed of the recheck of the resident's height and new BMI calculation of 15. The Medical Director said that he was unaware of the resident's BMI of 15 and that this was a critical value.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined that the facility failed to ensure that feedings via a g-tube were administered as ordered and failed to ensure a plan to try to restore...
Read full inspector narrative →
Based on medical record review and interview, it was determined that the facility failed to ensure that feedings via a g-tube were administered as ordered and failed to ensure a plan to try to restore oral eating was established. This was found to be evident for one (Resident #23) out of one resident reviewed for tube feeding.
The findings include:
Review of Resident #23's medical record revealed the resident was admitted in June 2024 after a hospitalization. The resident's diagnosis included dysphagia which is difficulty swallowing and the resident had a g-tube for the administration of nutrition. The resident was admitted with orders that nothing was to be given by mouth, and a g-tube with orders for bolus feedings of Jevity 1.5 four times a day.
A bolus is when a large amount of feeding is given at one time.
Further review of the medical record revealed there were two different enteral feed (g-tube) orders in effect from 6/6/24 until they were both discontinued on 7/26/24.
The first order, placed on 6/6 at 4:22 AM, was for Jevity 1.5 425 ml bolus four times a day every 6 hours per protocol. Review of the Medication Administration Record (MAR) revealed these feedings were scheduled for midnight, 6:00 AM, noon and 6:00 PM. Review of the MAR revealed a check mark to indicate the 425 ml bolus feed was administered as ordered four times a day from 6/6 until the order was discontined on 7/26, except for one dose on 7/4 at 6 am was noted to be blank.
The Jevity 1.5 provides 1.5 calories per ml, thus a 425 ml bolus provides 638 calories per bolus and four bolus per day would provide 2550 calories per day.
This first order also included instructions to document the amount of feeding provided every 8 hours. Further review of the medical record failed to reveal documentation of the actual amount of Jevity that was being administered during each bolus feed or every 8 hours as ordered.
The second g-tube feeding order was placed on 6/6/24 at 12:51 PM and was for Jevity 1.5 one carton 4 times a day. The order includes a notation that, in addition to the Jevity, the resident would also be receiving ALP (Active Liquid Protein) 30 ml three times a day and that this would provide an additional 300 calories and that the resident would receive a total of 1720 cals per day.
Review of the manufacturers website revealed the Jevity 1.5 cartons are 8 ounces. There are only 236 ml per 8 ounces. The website indicated that there were 355 calories per 8 ounce carton, so four bolus per day would provide 1420 calories per day from the Jevity.
Review of the MAR revealed documentation that staff administered one carton of the Jevity 1.5 four times a day at 9:00 AM; 1:00 PM, 5:00 PM and 9:00 PM every day from 6/6/24, until the order was discontinued on 7/26/24.
Further review of the medical record revealed a 7/26/24 registered dietitian (Staff #30) note which documented that the resident's weight on 6/7 was 132 lbs and on 7/8 the weight was 125 lbs which was considered a significant weight loss. The resident's estimated caloric need per day were 1710- 2000 calories. The dietitian's summary revealed that the resident appeared to have a significant weight loss over 1 month which was unfavorable and unplanned, the tube feeding was providing 1420 calories per day and the resident was receiving an additional 180 calories from a supplement which totaled 1600 calories per day. Needs do not appear to be met with current rate as evidenced by wt loss. Recommend changing TF regimen Jevity 1.5 1 carton q3hour [every 3 hours], 6 times a day. The new regimen would provide 2130 calories per day.
No documentation was found to indicate the weight loss identified on 7/8/24 was addressed by the dietitian prior to 7/26/24.
Further review of the medical record revealed a new g-tube order was put in place on 7/26/24 at 2:35 PM for one carton Jevity 1.5 bolus 6x/day. There was a notation that this feeding would provide 2130 cals per day. This order was discontinued on 9/18/24.
Review of the MAR revealed staff documented the Jevity bolus feeds were administered 6 times a day as ordered every day from 7/27/24 thru 9/17/24, except for two feedings that were due scheduled to be administered on 9/5/24 at 10:00 AM and 1:00 PM. The area to document these feedings were noted to be blank, there was no documentation to see nurse's note or that these two feedings were held.
On 9/17/24 at 1:10 PM, review of the medical record revealed an order, dated 8/28/24 to hold the 10 AM bolus feed. There was also an order for dysphagia advanced texture diet for lunch only on 8/28/24.
Further review of the medical record on 9/18/24 revealed the RD #30 had seen the resident on 9/17/24 and entered a note at 5:31 PM. This note acknowledged that the resident was receiving lunch only and tube feeding for all other meals. It documented the current tube feeding as being Jevity 1.5 bolus 6 x/day. The note included the following weights: 6/7: 132 lbs; 8/5: 132 lbs and 9/4: 132 lbs. The recommendation was to continue the diet and tube feeding as ordered. The note failed to include notation that there was a current order to hold the 10 AM feeding.
On 9/18/24 10:01 AM, surveyor asked Nurse #59, who was assigned to care for the resident, when the next bolus feed will occur. The nurse reported that the resident was eating at the time, that s/he would get a bolus at 6 AM the next was not until the evening. She then confirmed that she was not administering the 10 AM or the 1 PM bolus feeds.
On 9/18/24 at 10:08 AM, the unit nurse manager #12 reported the resident received bolus feeds and proceeded to check the documentation in the computer. She went on to report the resident gets lunch only and bolus of Jevity 1.5 six times a day. When asked if the 10 oclock feeding was held, the unit nurse manager responded: yes for lunch and then she clarified that the resident was getting 5 bolus'. After reviewing the MAR, the unit nurse manager stated: they are signing for it but not giving it and confirmed the order in August to hold the 10 AM feed.
On 9/18/24 at 1:54 PM, surveyor reviewed the concern with the DON that the RD assessment from yesterday failed to address the order to hold the 10 AM feeding which meant resident is only receiving 5 bolus feedings per day, not the 6 as indicated in the RD note.
Continued review of the medical record on 9/23/24, revealed a note completed by RD #24 on 9/18/24 which revealed Noted NP [nurse practitioner] order 8/28 for holding TF @ 10am to help promote oral intakes, per nursing staff holding bolus has benefited [him/her] as [s/he] has been able to eat well and has great appetite for lunch (intakes of 50-100% per nursing charts). I discussed TF regimen w/dtr [daughter] today via phone. Dtr agrees to adjust the amount of bolus provided while taking into consideration current oral intakes. Will also d/w SLP [speech therapist] possibility of evaluation to determine if frequency of meals could be increased. The recommendations included adjusting the tube feeding orders to Jevity 1.5 1 carton 4 x/day and speech therapy for diet eval.
A corresponding physician order for the Jevity 1.5 1 carton 4 x/day was found for 9/18/24.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined that the facility failed to provide behavioral health monitoring to ensure a resident's highest practicable mental and psychosocial well...
Read full inspector narrative →
Based on medical record review and interview, it was determined that the facility failed to provide behavioral health monitoring to ensure a resident's highest practicable mental and psychosocial well being.This was found to be evident for 1 (Resident #30) out of 5 residents reviewed for unnecessary medications.
The findings include:
Review of Resident #30's medical record revealed the resident had resided at the facility for several years and whose diagnoses included, but was not limited to: high blood pressure, kidney disease, major depressive disorder and dementia. Review of the Minimum Data Set assessment, with a reference date of 6/5/24, revealed the resident had a BIMS (Brief Interview for Mental Status) of 4 indicating severe cognitive impairment.
Review of the medical record revealed that the resident was seen about once a month by either the Psychiatrist #37 or the Psychiatric Nurse Practitioner (NP) #36.
1) Review of the Psychiatric NP #36's note, dated 2/7/24, revealed the resident's current psychiatric medications included Seroquel (an antipsychotic) 25 mg two times a day and Zoloft (Sertraline- an antidepressant) 50 mg daily. The Treatment Plan/Recommendation section included: Continue Current Meds. No documentation was found in this note to indicate a GDR of the Zoloft was being considered or planned.
Further review of the medical record revealed that the resident was receiving the antidepressant medication, Sertraline 50 mg one time every day from 10/24/23 until 2/29/24. On 2/29/24, the Sertraline 50 mg every day order was discontinued by the primary care physician #26. A new order was put in place on 2/29/24 for Sertraline 25 mg one time a day for 90 days. The medication was not renewed after the 90 days was completed. This tapering down and then discontinuation of a psychoactive medication is referred to as a gradual dose reduction (GDR).
Review of the Psychiatrist #37's note, dated 3/25/24, revealed a notation that the resident was currently being treated with Zoloft and that the current dose was 25 mg every day. However, no documentation was found to indicate the 25 mg every day dose was a recently initiated GDR. The Treatment Plan/Recommendations section included: GDR is not recommended at this time as the benefit of the medication outweigh the risks of dosage reduction.
Review of the Psychiatric NP #36's notes, dated 5/8/24 and 5/15/24, revealed the resident's current psychiatric medications included Serorquel (an antipsychotic) 25 mg two times a day and Zoloft (Sertraline) 25 mg daily. The Treatment Plan/Recommendation section included: Continue Current Meds. No documentation was found in this note to indicate there was a plan to continue the GDR of the antidepressant.
The 2/29/24 order for Sertraline for 90 days was completed at the end of May. No documentation was found to indicate that the resident had received this antidepressant since May 2024.
Further review of the medical record revealed a change in condition note that revealed on 6/8/24, the resident was highly agitated and was observed being verbally abusive and throwing items at the resident's roommate. The psychiatrist #37 was notified, there was an order to transfer the resident to the hospital. After the resident refused the transfer, the psychiatrist was notified and there was then an order for IM Haldol (an antipsychotic) and IM Benedryl (an antihistamine) for aggressive behavior. These IM medications were administered on 6/9/24 at 1:50 AM.
Review of the Psychiatric NP #36's notes, dated 6/12/24, revealed the following: Chart reviewed; Spoke with staff regarding patient's progress; No new behavioral concerns reported; No agitation, irritability or aggression noted this visit. The Treatment Plan/Recommendation section included: Continue Current Meds. No documentation was found in this note regarding the recent discontinuation of the antidepressant medication or the 6/8/24 episode which resulted in the use of an IM antipsychotic medication.
Review of the Psychiatrist #37's notes, dated 6/17/24 and 7/15/24, revealed a notation that the resident was current being treated with Zoloft, Depakote and Seroquel.
On 9/23/24 at approximately 9:00 AM, surveyor reviewed the concern with the Director of Nursing that the resident's antidepressant was stopped but no documentation was found to indicate this was a planned GDR. The DON then provided a copy of the 2/29/24 order to discontinue the Zoloft which included GDR in the area to document the reason for discontinuation. No other documentation was provided at the time.
On 9/23/24 at 10:40 AM, an interview was conducted with the psychiatrist #37, in the presence of the Director of Nursing. When asked if psychiatric providers were involved in GDRs, the Psychiatrist reported the nurse practitioner (NP) sat with the staff to review for GDR. When asked if he expected the NP to document a GDR, psychiatrist #37 responded: yes, of course, she would document the dose of the GDR. Surveyor reviewed the concern that the resident's antidepressant was reduced and then stopped at the end of May, but no documentation was found in the NP notes to address this GDR.
2) Review of the Medication Administration Record (MAR) revealed areas for nursing staff to document resident behaviors on the day, evening and night shifts. Review of the MAR revealed staff could document based on the following coding: 1 - compulsive; 2 - pacing continuously; 3 - Continuously screaming and yelling; 4 - danger to others; 5 - danger to self; 6- false beliefs; 7 - finger painting feces; 8 - spitting; 9 - other. On 9/16/24, review of the documentation for this monitoring for June, July, August and September thru the 16th, 2024 revealed only a check mark for each shift.
On 9/16/23 at 3:52 PM interview with Nurse #8 revealed that a check on the behavior monitoring sheets meant that the resident had none of those behaviors.
On 9/16/24 at 3:58 PM, interview with the unit nurse manager #12 revealed that, when the nurses see this item on the computer, they have to answer yes or no. The unit nurse manager confirmed that the checks indicated that the resident was not displaying behaviors. After reviewing the September MAR with the unit nurse manager, surveyor asked if that was an accurate assessments of the resident, the unit nurse manager stated: no. When asked where were staff documenting the resident's behaviors, the manager indicated they were supposed to use the MAR.
Further review of the MAR revealed there was another section to document other psychiatric symptoms: 1- mood swings; 2 - sad; 3 - continuous crying; 4 - withdrawn; 5 - depressed; 6 - angry; 7 - poor eye contact; 8 - other. Review of the nursing documentation from June, July, August and September thru the 16th, 2024 revealed that staff documented every shift either a 0 or an N, thus indicating the resident was not experiencing these symptoms.
Based on review of the behavior monitoring documentation being completed every shift by nursing staff, the resident was not experiencing any behaviors of concern for June, July, August or September.
On 9/17/24 review of the physician orders revealed the resident had orders for Seroquel 25 mg twice a day from November 2023 until 6/17/24.
Review of the 6/17/24 psychiatrist #37 note revealed documentation to indicate staff was reporting the resident was getting aggressive with the roommate and there was a documented plan to increase the Seroquel dose to 50 mg two times a day. This increase occurred more than a week after the 6/8/24 incident resulting in the order for the IM Haldol and after the 6/12/24 NP visit in which the NP documented that she spoke with staff regarding the resident's progress and there were no new behavioral concerns reported.
From 6/17/24 until 7/10/24, the order was for Seroquel 50 mg two times a day.
Further review of the physician orders revealed from 7/10/24 until 9/17/24, the order was for Seroquel 100 mg two times a day.
On 7/15/24, there was a new order for Risperdal (antipsychotic) 0.5 mg two times a day that was in effect until 9/5/24.
Review of the 7/15/24 psychiatrist #37 note revealed documentation to indicate staff was reporting the resident was getting aggressive toward roommate due to paranoia to the point they had to move the resident out of the room. The note documents the start of the Risperdal 0.5mg twice a day for paranoia and stated if the resident does well with Risperdal, would consider tapering off Seroquel.
Review of the Psychiatric NP #36's notes, dated 8/7/24, revealed staff reporting episodes of getting aggressive towards roommate and does not want a roommate. The note included a notation of Risperdal 0.5 mg bid (two times a day) and included a plan to Continue Current Meds.
Further review of the medical record on 9/17/24 revealed that, on 9/5/24, there was a new order for Risperdal 1 mg two times a day that was currently in effect. No documentation was found to indicate why this antipsychotic medication was increased on 9/5/24.
Review of the Psychiatric NP #36's notes, dated 9/11/24, revealed: Chart reviewed; Spoke with staff regarding patient's progress; No new behavioral concerns reported; Per staff [s/he] has been stable and has not exhibited symptoms of depression, mania, anxiety, psychosis or self-injurious behavior. The note did include Risperdone 1 mg bid in the list of current psychiatric medications but failed to address why the dose was double less than a week before this visit. The note included the plan to Continue Current Meds.
On 9/17/24 at 11:31 AM, surveyor reviewed the concern with the Director of Nursing regarding the increase in the antipsychotic medication without adequate indication. Reviewed that the behavior monitoring sheets since June failed to reveal documentation of behaviors to indicate the need for this increase. Surveyor requested any additional documentation they may have regarding this concern.
On 9/23/24, review of the medical record revealed a note written by the NP #36 which included the plan to attempt GDR on seroquel to 100 mg at time of sleep.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3). A brief review of Resident #50's medical record indicated that s/he was admitted to the facility in August of 2024.
On 9/13...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3). A brief review of Resident #50's medical record indicated that s/he was admitted to the facility in August of 2024.
On 9/13/24 at 12:43 PM, the Director of Nursing (DON) was interviewed regarding the facility's process with Medication Regimen Review (MRR). The DON reported that, after the initial review, the consultant pharmacist reviews all the resident's medication orders monthly. When an irregularity is identified, the pharmacist sends the report via email to the DON. The DON prints the report and hands it to the physician, the physician then writes their response on the report and hands it back to the DON. Finally, the DON then makes the changes with the resident's medication regimen per the attending physicians' response.
On another interview with the DON on 9/16/24 at 11:33 AM, she reported that physician response from recommendation by the pharmacist for MRR can be found either in the doctor's note or the written response on the reports are scanned in the resident's medical record and were titled Actual Meds.
On 9/17/24 at 10:57 AM, the MRR for Resident #50 with a reference date of 8/26/24 was reviewed. The review indicated that irregularities were identified by the pharmacist.
Subsequently at 11:00 AM, Resident #50's medical record was reviewed but failed to reveal the attending physician's response to the irregularities identified.
On 9/17/24 at 11:34 AM, the concern was discussed with the DON, and she indicated that she would review Resident #50's medical record to look for the physician note or the written response that she scans and attaches to the resident's medical record.
Later that day at 1:17 PM, the DON reported and confirmed that the attending physician had not documented his response to the pharmacy recommendations and stated, I looked in the resident's medical record, but I did not find any.
2) On 9/17/24 at 11:53 AM, a review of Consultant Pharmacist medication reviews revealed a New admission Medication Review for Resident #78, that had a review date of 7/1/24 at 3:08 PM, and the printed statement Please consider the following Pharmacist recommendations in assessing this resident's drug regimen. The provider and/or nursing staff should respond appropriately. Recommendations marked clinically significant should be resolved by midnight the next calendar day, copied to the MDS (Minimum Data Set) Coordinator and filed in the Resident's chart appropriately. The statement was followed by the heading, Drug Therapy Problems Identified, and pharmacist documentation of 5 irregularities with Resident #78's medication, the significance of the recommendations, the pharmacist's recommended action for the provider, and an area for the practitioner to document any comments and/or action taken in response to the pharmacist's recommendations.
The medication review form documented the drug therapy problems identified with Resident #78's medications as follows:
2a) Resident #78 was prescribed the medications, Gabapentin (Neurontin) (seizure & nerve pain medication), Lexapro (Escitalopram) (antidepressant), Oxycodone (narcotic pain medication), and Oxycontin (oxycodone) oral tablet ER (extended release), with recommendations marked clinically significant.
The pharmacist documented the risks of concurrent use of 3 or more different central nervous system (CNS) active medications that should be avoided in older adults [AGE] years of age and older due to an increased risk of falls, with the recommended action for the provider, the patient is currently receiving the above medication(s which is considered a high-risk medication for an elderly patient. Please evaluate, consider using a safer alternative, or document a risk/benefit analysis within the patient medication record for continued utilization. Following the pharmacist's recommendation, no documentation was found to indicate the attending physician reviewed the above identified irregularities and/or the action taken or not taken to address the irregularities.
2b) Resident #78 was prescribed the medication, Enoxaparin (Lovenox) (anticoagulant) (blood thinner) Sodium Injection, with recommendations marked clinically significant. The pharmacist documented that a stop date for use of the medication was needed, and the recommended action for the provider, resident is currently receiving the above medication which is normally subject to a stop date. Please evaluate this resident to see if it is appropriate to DC (discontinue) the medication at this time. If you wish to continue drug therapy, please indicate rational for use below
Following the pharmacist's recommendation, no documentation was found to indicate the attending physician reviewed the above identified irregularities and/or the action taken or not taken to address the irregularities.
2c) Resident #78 was prescribed the medication, Amlodipine Besylate (Norvasc) (lowers blood pressure), with recommendations marked clinically significant, and wrote the recommended action for the provider, The patient was receiving the above medication(s) at home prior to their admission but is not noted on the current facility orders. Please evaluate and consider restoring if appropriate.
Following the pharmacist's recommendation, no documentation was found to indicate the attending physician reviewed the above identified irregularities and/or the action taken or not taken to address the irregularities.
2d) Resident #78 was prescribed the medications, Aspirin EC (enteric coated) (anti-inflammatory) (blood thinner) delayed release 81 MG, Enoxaparin (Lovenox) Sodium Injection, with recommendations marked high risk. The pharmacist wrote the recommended action for provider, please consider changing this pharmacotherapy and indicate as per below. If continuing therapy, please document your response to assure this facility's compliance with CMS regulations, which was followed by a checklist with 3 possible practitioner responses.
None of the potential responses had been checked by the practitioner, and no documentation was found to indicate the attending physician reviewed the above identified irregularities and/or the action taken or not taken to address the irregularities.
2e) Resident #78 was prescribed Metformin (Glucophage) (anti-diabetic) (lowers blood sugar), with recommendations marked nursing, and the pharmacist documented the pharmacist's this medication should generally be taken with food or a meal to prevent gastric irritation and/or GI bleeding.
Following the pharmacist's recommendations, there no documentation in the medication review to indicate the attending physician reviewed the identified irregularities and/or the action taken or not taken to address the irregularities.
Continued review of the Resident #78's medical record failed to reveal documentation to indicate the irregularities identified by the pharmacist were reviewed by the attending physician, timely acted upon and documented in the resident's medical record.
On 9/18/24 at 5:11 PM, the DON was made aware that a review of the resident's medical record failed to reveal evidence the attending physician reviewed and responded to the pharmacist identified irregularities with Resident #78's medication. The DON acknowledged the concerns at that time, and indicated that if found, evidence of the provider's response would be provided to the surveyor. No additional information was provided to the surveyor by the time of exit on 9/23/24.
Based on medical record review and interview with staff, it was determined that the facility failed to ensure that Irregularities identified by the pharmacist were reviewed by the attending physician, timely acted upon and documented in the resident's medical record. This was evident for 3 (#30, #78, 50 ) of 5 residents reviewed for unnecessary medications.
The findings include:
1) Review of Resident #30's medical record revealed the resident had resided at the facility for several years and whose diagnoses included, but was not limited to: high blood pressure, kidney disease, major depressive disorder and dementia.
On 9/16/24, review of the medical record revealed a Consultant Pharmacist's Recommendation to Physician, dated 5/6/24, which stated: Federal guidelines state antipsychotic drugs should have an attempt at a gradual dose reduction (GDR) twice per year for the first year in 2 different quarters with at least 1 month between attempts, then annually thereafter. This resident has been taking Seroquel 25 mg bid [two times a day] since (11/2/2023) without a GDR. Could we attempt a dose reduction at this time to perhaps 25 mg daily to verify this resident is on the lowest possible dose? If not, please indicate response below:.
Further review of the medical record failed to reveal documentation to indicate either the primary care provider, or the psychiatric provider, reviewed or addressed this recommendation.
On 9/16/24 at 4:37 PM, the Director of Nursing reported that they were unable to find a response to the May pharmacy recommendation.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined that the facility failed to ensure the resident was free from unnecessary psychotropic medications. This was found to be evident for 1 (...
Read full inspector narrative →
Based on medical record review and interview, it was determined that the facility failed to ensure the resident was free from unnecessary psychotropic medications. This was found to be evident for 1 (Resident #30) out of 5 residents reviewed for unnecessary medications.
The findings include:
Review of Resident #30's medical record revealed the resident had resided at the facility for several years and whose diagnoses included, but was not limited to: high blood pressure, kidney disease, major depressive disorder and dementia. Review of the Minimum Data Set assessment, with a reference date of 6/5/24, revealed the resident had a BIMS (Brief Interview for Mental Status) of 4 indicating severe cognitive impairment.
Review of the medical record revealed the resident was seen about once a month by either the Psychiatrist #37 or the Psychiatric Nurse Practitioner (NP) #36.
1) Further review of the medical record revealed a change in condition note that, on 6/8/24, the resident was highly agitated and was observed being verbally abusive and throwing items at the resident's roommate. The psychiatrist #37 was notified, and there was an order to transfer the resident to the hospital. After the resident refused the transfer the psychiatrist was notified and there was then an order for IM Haldol (an antipsychotic) and IM Benedryl (an antihistamine) for aggressive behavior. These orders were entered between 7:30 PM and 8:00 PM. These IM medications were administered on 6/9/24 at 1:50 AM.
No further documentation was found to indicate the resident was continuing to experience aggressive behaviors in the five hours between the medication being ordered and the administration of the IM antipsychotic medication.
On 9/23/24 at 11:30 AM, surveyor reviewed with Psychiatrist #37 the concern that the order was put in around 7:30 PM on 6/8/24, but the IM injections were not documented as administered until 1:50 AM on 6/9/24 by a different nurse. Psychiatrist #37 indicated the injections should of been given STAT and questioned if this was just late documentation.
On 9/23/24 at 11:36 AM, review of Nurse #46's punch card information revealed the nurse was off on 6/7/24. Nurse #46 punched in at 11:40 PM on 6/8/24 and punched out at 7:44 AM on 6/9/24.
On 9/23/24 at 11:44 AM, surveyor reviewed with the DON that the nurses who documented the behaviors on 6/8/24 and obtained the orders did not administer the IM injections and the that the nurse that did administer the injections was not in the facility when the STAT order was given.
Cross reference to F 605
2) Continued review of Resident #30's medical record revealed behavior monitoring documentation being completed every shift by nursing staff. Based on review of this documentation, the resident was not experiencing any behaviors of concern for June, July, August or September.
On 9/17/24, review of the physician orders revealed that the resident had orders for Seroquel 25 mg twice a day from November 2023 until 6/17/24.
Review of the 6/17/24 psychiatrist #37 note does reveal documentation to indicate that staff was reporting the resident was getting aggressive with the roommate and there was a documented plan to increase the Seroquel dose to 50 mg two times a day. This increase occurred more than a week after the 6/8/24 incident resulting in the order for the IM Haldol and after the 6/12/24 NP visit in which the NP documented that she spoke with staff regarding the resident's progress and there were no new behavioral concerns reported.
From 6/17/24 until 7/10/24, the order was for Seroquel 50 mg two times a day.
Further review of the physician orders revealed that, from 7/10/24 until the time of the survey, the order was for Seroquel 100 mg two times a day.
On 7/15/24, there was a new order for Risperdal (antipsychotic) 0.5 mg two times a day that was in effect until 9/5/24.
Review of the 7/15/24 psychiatrist #37's note revealed documentation to indicate staff was reporting the resident was getting aggressive toward their roommate due to paranoia to the point they had to move the resident out of the room. The note documented the start of the Risperdal 0.5mg twice a day for paranoia and stated if the resident does well with Risperdal, will consider tapering off Seroquel.
Review of the Psychiatric NP #36's notes dated 8/7/24 revealed staff reporting episodes of getting aggressive towards roommate and not wanting a roommate. The note includes a notation of Risperdal 0.5 mg bid (two times a day) and included a plan to Continue Current Meds.
Further review of the medical record on 9/17/24 revealed that, on 9/5/24, there was a new order for Risperdal 1 mg two times a day that was currently in effect. No documentation was found to indicate why this antipsychotic medication was increased on 9/5/24.
Review of the Psychiatric NP #36's notes, dated 9/11/24, revealed: Chart reviewed; Spoke with staff regarding patient's progress; No new behavioral concerns reported; Per staff [s/he] has been stable and has not exhibited symptoms of depression, mania, anxiety, psychosis or self-injurious behavior. The note did include Risperdone 1 mg bid in the list of current psychiatric medications but failed to address why the dose was doubled less than a week before the 9/11/24 visit. The note included the plan to Continue Current Meds.
On 9/17/24 at 11:31 AM, surveyor reviewed the concern with the Director of Nursing regarding the increase in the antipsychotic medication without adequate indication. Reviewed that the behavior monitoring sheets since June failed to reveal any documentation of behaviors to indicate the need for the increase. Surveyor requested any additional documentation regarding this concern.
On 9/23/24, further review of the medical record revealed a note written by the NP #36 on 9/18/24, which included the plan to attempt GDR on seroquel to 100 mg at time of sleep.
Cross reference to F 740
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
1) An observation of medication administration on 9/16/24 at 8:13 AM showed that staff #21, a certified medicine aid (CMA), prepared and administered 6 medications to Resident #78.
Following the medi...
Read full inspector narrative →
1) An observation of medication administration on 9/16/24 at 8:13 AM showed that staff #21, a certified medicine aid (CMA), prepared and administered 6 medications to Resident #78.
Following the medication administration, a review of Resident #78's medication administration record (MAR)for September 1 to September 16, 2024, was done. The review noted an attending provider's order for Resident #78 for Empagliflozin Oral Tablet 10 MG (Empagliflozin) Give 1 tablet by mouth one time a day for DM. The medication was recorded as given on 9/16/24 at 08:29.
However, the surveyor did not observe the medicine being administered to the resident.
In an interview on 9/16/24 at 12:28 PM, staff #21 said she did not administer the medication even though she signed that she did.
On 9/17/24 at 9:31 AM, the surveyor reviewed with the Director of Nursing the medication error of not administering the antidiabetic medicine on 9/16/24 as ordered.
Based on observation, medical record review and interview, it was determined the facility failed to maintain a medication error rate of less than 5%. This was found to be evident based on 3 errors identified out of 25 opportunities for error. The findings include:
1) On 9/13/24 at 9:45 AM, during an observation of medication administration, Staff 13, Licensed Practical Nurse (LPN) was observed dispensing 5 pills into a medication cup and administering the pills to Resident #383. One of the pills dispensed and administered to Resident #383 by mouth was Calcium 600 mg (milligram) tablet.
Following the medication observation, a review of Resident #383's September 2024 Medication Administration Record (MAR) revealed an 8/30/24 order for Calcium 600 mg (milligram) + Vitamin D3 (Cholecalciferol) 20 mcg (microgram) give 0.5 tablet by mouth one time a day, that Staff #13 documented as given on 9/13/24.
The medication ordered was a combination drug of Calcium 600 mg and Vitamin D3 20 mcg, which was different than the Calcium 600 mg tablet Staff #13 administered to Resident #383. Staff #13 committed a medication error by administering the wrong medication to Resident #383 and failing to administer the correct combination of medication as ordered.
2) On 9/13/24 at 10:10 AM, during an observation of medication administration, Staff #13, LPN, was observed dispensing 12 pills into a medication cup and administer the pills to Resident #122. One of the pills dispensed and administered to Resident #122 by mouth was a Vitamin B-12 1000 mcg tablet.
Following the medication observation, a review of Resident #122's September 2024 MAR revealed an 8/20/24 order for Vitamin B12 (Cyanocobalamin) tablet 500 mcg one time a day that Staff #13 documented as given on 9/13/24.
The dose of the Vitamin B12,1000 mcg dose which was administered to the resident, was different than the Vitamin B12, 500 mcg which was ordered. Staff #13 committed a medication error while administering the medication to Resident #122 by failing to administer the right dose of Vitamin B-12 medication.
The above medication administration error concerns were discussed with Staff #13, LPN on 9/13/24 at 4:20 PM, and Staff #13 confirmed the medication administration errors at that time, with no comments.
The Director of Nurses was made aware of the above medication error concerns on 9/20/2024 at 3:30 PM. The DON acknowledged the concerns and offered no further comments at that time.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected 1 resident
Based on the interview and review of relevant documentation, it was determined that the facility failed to have a full time clinically qualified Food Service Director and failed to ensure scheduled co...
Read full inspector narrative →
Based on the interview and review of relevant documentation, it was determined that the facility failed to have a full time clinically qualified Food Service Director and failed to ensure scheduled consultations from a qualified dietitian or other clinically qualified nutrition professional. This was evident for 1 (Staff #62) of 1 Food Service Director reviewed for required credentialing.
The findings include:
On 9/14/24 at 12:30 PM, an interview was conducted with the current Food Service Director (FSD-Staff #62) who reported she had worked at the facility for 4 years but was not a Certified Dietary Manager. Surveyor requested the FSD's current credentials. The FSD confirmed that the facility's Registered Dietitian (RD) was not involved in the running of the kitchen, and indicated she thought the facility did not currently employ a full time RD.
State regulations require in a nursing home with more than 50 beds, overall supervisory responsibilities for the food service department and food production shall be assigned to a full-time qualified dietetic service supervisor. The state regulations define a dietetic service supervisor as a person who:
a) Is a graduate of a dietetic technician program approved by the American Dietetic Association;
(b) Is a graduate of a dietetic technician program approved by the American Dietetic Association;
(c) Is a certified dietary manager who has successfully completed the required course and maintains certification as required by the certifying board for the Dietary Managers Association;
(d) Is a graduate of a State-approved course that provided 90 or more hours of classroom instruction in food service supervision and has experience as a supervisor in a health care institution with consultation from a dietitian; or
(e) Has training and experience in food service supervision and management in a military service equivalent in content to §B(15)(b) and (d) of this regulation. [ See COMAR S0790-10.07.02.21B]
Review of FSD #62's credentials failed to reveal documentation to indicate the FSD was a qualified dietitian or other clinically qualified nutrition professional.
On 9/16/24 at 2:30 PM, the FSD #62 reported there was a Registered Dietitian (RD) on call but she did not meet regularly with the RD.
On 9/18/24 at 1:21 PM, surveyor informed the District Manager (Staff 64) of the concern that the FSD credentials did not meet the state regulation and that there was no RD consulting on a regular basis. He reported the FSD was enrolled in CDM program thru Univ of Florida and he thought that as long as they were enrolled that was good enough. Surveyor requested any additional documentation they may have.
The District Manager provided documentation that the FSD #62 was enrolled in a Nutrition Foodservice Professional Training Pathway I course on 5/28/24.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, and interview, it was determined that the facility failed to ensure clean dishes were stored and maintained in a manner to prevent contamination. This practice had the potential ...
Read full inspector narrative →
Based on observation, and interview, it was determined that the facility failed to ensure clean dishes were stored and maintained in a manner to prevent contamination. This practice had the potential to affect all the residents in the facility.
The findings include:
On 9/10/24, an initial tour of the kitchen was conducted at 7:30 AM. During this tour, surveyor observed in the dishwashing room a cart with approximately 20 cups, in stacks of about 4-5 where the cups were inverted and stored open area down on a tray. Significant moisture was noted in all of these cups. The dietary aide (Staff #61) reported these cups were for lunch. Surveyor then asked the [NAME] (Staff 63) to observe the glasses; at first the [NAME] said that the staff will wipe them. When surveyor repeated this statement back, the [NAME] then said: will send them thru the washer again and let them air dry.
The practice of storing dishes prior to being completely air dried is known as wet nesting. Wet nesting creates conditions in which microorganism can grow.
On 9/12/24 at 11:45 AM, during a revisit to the kitchen surveyor observed a tray, similar to the one observed on 9/10/24, with 6 stacks of 5 cups each with moisture noted in the cups. These cups were on a cart with a drink container. The District Manager (Staff #64) confirmed these cups were to be used with lunch service. Surveyor reviewed the concern regarding the wet nesting found on day 1 of the survey and again today. District manager then proceeded to place the cups in rack to air dry.
2) On 9/10/24 during the initial kitchen tour, surveyor noted the tray with the cups had significant chipping.
On 9/12/24 at 11:45 AM, during a revisit to the kitchen, chipped trays were again observed while trays were being prepared.
On 9/12/24 at 12:30 PM while observing a test tray with the Food Service Director, surveyor noted the test tray with a chip. Surveyor discussed the observations of multiple chipped trays with the FSD. The FSD reported they have ordered new trays but they were non back order. Surveyor requested documentation to support this.
As of time of survey exit on 9/23/24 at 1:00 PM, no documentation was provided to indicate new trays were on order.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility failed to document clinical assessments. This was evident for 1 resident (Resident #17) of 5 residents reviewed for nutrition ...
Read full inspector narrative →
Based on record review and interview, it was determined that the facility failed to document clinical assessments. This was evident for 1 resident (Resident #17) of 5 residents reviewed for nutrition during the recertification survey.
The findings include:
On 9/11/24 at 9:34 AM, a review of Resident #17's height and weight documentation was conducted. There were 3 entries in the Height Summary:
7/23/24 61.0 inches lying down
12/16/16 72.0 inches Standing
12/08/16 72.0 inches Standing
On 9/19/24 at 2:12 PM, an interview with the Director of Nursing (DON) was conducted to review the discrepancy in the resident's documented heights., 72 inches, and 61 inches. When asked to confirm the resident's current height, the DON agreed to measure the resident's height.
On 9/19/24 at 2:45 PM, the DON informed the surveyor that she measured the resident's height today and it was 70 inches.
On 9/23/24 at 8:54 AM, an updated printout of Resident #17's height measurements was requested. When the DON provided the printed copy, there were no additional entries beyond 7/23/24. The record did not contain the measurement obtained by the DON on 9/19/24. When the DON was asked where the measurement of 70 inches on 9/19/24 was recorded, she confirmed that she did not document it and that she did not think she needed to do so.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
3. On 9/12/24 at 2:25 PM, the Director of Housekeeping (Staff #49) was interviewed regarding the facility's process with laundry. Simultaneously, while Staff #49 explained the facility's process, a to...
Read full inspector narrative →
3. On 9/12/24 at 2:25 PM, the Director of Housekeeping (Staff #49) was interviewed regarding the facility's process with laundry. Simultaneously, while Staff #49 explained the facility's process, a tour of the laundry room was conducted with the surveyor.
While Staff #49 explained the different areas of the facility's laundry room, an observation was made on 9/12/24 at 2:31 PM, of Hoyer/lifting pads or sling and washable chucks/underpads hanging on a platform over the bins containing soiled laundry.
Staff #49 was questioned about the observation, and she indicated that all of the lifting pads and washable chucks have been washed and were placed in that location for drying. She further indicated that the items could not be put in the dryer because it would ruin them.
A Hoyer lift is a patient lift used by caregivers to safely transfer patients. It can be used for lifting patients from the floor or onto a healthcare bed. The lift also can assist in other surface-to-surface patient transfers, such as moving from a bed to a bath or chair. The sling or lifting pads are made of durable materials placed under the individual with straps that attach to the lift or sling bar.
Underpads are absorbent sheets that lay between the user and the furniture or bed that the user is laying or sitting on. They help to absorb any fluid due to incontinence to avoid leakage and damage to the furniture or bed.
Subsequently, at 2:37 PM, the assigned Laundry Aide (Staff #58) arrived in the laundry room for her shift. Staff #58 began her shift by removing the washed laundry and placed them in a bin with rollers. While still in the soiled area of the laundry room, Staff #58 donned disposable gloves, a gown, and a face shield, and proceeded to load the washer with the soiled laundry. After removing the personal protective equipment and discarding them, Staff #58 rolled the bin, with the washed laundry in them, to the clean side of the laundry room where the dryers were located.
On 9/12/24 at 3:01 PM, Staff #49 was invited to come back in the laundry room and the concerns that the surveyor had observed were reported to both Staff #49 and #58. The concern was that the lifting pads and washable chucks were being hung dried in the soiled area of the laundry room; and that Staff #58 was observed to process soiled laundry while the clean laundry was in close proximity, about 3 feet away. Both staff verbalized understanding that these observations were concerns with cross contamination. Staff #49 instructed Staff #58 to rewash all the items immediately, including the lifting pads and chucks, and to find an area in the clean side of the laundry room to hang them for drying afterwards. Both staff thanked the surveyor.
Based on record review, observation, and interview, it was determined the facility failed to maintain a resident's medical equipment in proper sanitary conditions and failed to process linens in a manner that prevents cross contamination. This was evident for 2 (Resident #88, #330) out of 2 residents, reviewed for urinary catheter or urinary tract infection during a survey and evident in 1 of 1 laundry room observations during the recertification survey and had the potential to affect all residents of the facility.
.The findings include:
1. 0n 9/10/24 at 2:29 PM, review of medical records revealed that Resident #88 was a long-term resident of the facility. Further review revealed that Resident # 88 had a foley catheter in place and was being treated for a urinary tract infection.
On 9/13/24 at 8:53 AM, an observation was made in Resident #88's room. The observation revealed the Foley tubing was attached to the lower bar on his/her bed and the drainage bag was resting on the floor.
On 9/13/24 at 9:14 AM, an observation was made with the Unit Manager LPN, (Staff # 12) and the Assistant Director of Nursing in Resident #88's room. Staff #12 stated that the Foley urine drainage collection bag was touching the floor because the bag was attached to the lower rung of the bed, and the bed was in the low position. Staff #12 reported she would fix the bag immediately and educate the staff on maintaining the Foley urine drainage bag, off the floor and under sanitary conditions.
On 9/20/24 at 10:50 AM, The above concerns were discussed with administrator and the Director of Nursing. No additional information was provided to the survey team.
2. On 9/11/24 at 9:40AM, review of Resident # 330s medical records revealed that Resident #330 was admitted to the facility with a tracheostomy.
A tracheostomy (also called a tracheotomy) is an opening surgically created through the neck into the trachea (windpipe) to allow air to fill the lungs. After creating the tracheostomy opening in the neck, surgeons insert a tube through it to provide an airway and to remove secretions from the lungs.
On 9/11/24 at 11:45 AM, an observation of Resident #330 revealed that the resident was receiving oxygen. The equipment used to administer the oxygen included a condensation reservoir bag. Further observation revealed the reservoir bag was resting on the floor.
On 9/11/24 at11:46 AM, an observation with first floor Unit Manager LPN (Staff #14) was made in Resident # 330 room.
On 9/11/24 at 11:47 AM, brief Interview with she reported that bag should not be resting on the floor and the tubbing may be too long. Unit manager stated she would correct the situation.
09/20/24 10:50 On 9/20/24 at 10:50 AM, The above concerns were discussed concerns with administrator and the Director of nursing. No additional information was provided to the survey team.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
2) On 9/17/24 at 3:20PM, Resident #328, admitted to the facility for rehab, was interviewed. During
the interview Resident # 328's family expressed concerns regarding the resident's bathroom.
On 9/17/...
Read full inspector narrative →
2) On 9/17/24 at 3:20PM, Resident #328, admitted to the facility for rehab, was interviewed. During
the interview Resident # 328's family expressed concerns regarding the resident's bathroom.
On 9/17/24 at 3:22PM, an observation was made of Resident #328 bathroom. The observation
revealed that the safety rail next to the toilet was loose. The fasteners affixing the rail to the wall
were exposed, with a visible hole in the dry wall.
09/17/24 08:16 AM, the maintenance Director (Staff # 25 ) and surveyor made an observation of
Resident #328's bathroom. The maintenance director confirmed that the safety rail in the
bathroom was loose and needed repair.
Based on family and staff interview, and observation, it was determined the facility failed to maintain electrical equipment in safe operating condition and failed to maintain a bathroom safety rail in a safe operating condition. This was evident for 1 of 1 microwave observed during the survey and evident for 1 residents room.
1) On 9/20/24 at approximately 10:00 AM, Resident #380's family member asked if the surveyor had seen the microwave in the 1st floor pantry where residents could have food reheated. The family member then stated that the interior of the microwave was rusty and s/he was concerned the microwave was not safe to use.
9/20/24 at 10:05 AM, observation of microwave revealed the white coating on the walls and floor of the microwave was peeling with areas of coating missing, exposing areas of rust. This included a larger, irregular area, approximately 7-inch x 1 inch, in the back floor of the microwave, where the coating was missing, and peeling, and the area in the microwave was rusted. Also, on the left interior wall of the microwave, there was an irregular area, approximately 3 inches in diameter where the coating was missing, and the microwave wall was rusted.
On 9/20/24 at 10:15 AM, accompanied by Staff #25, Maintenance Director, a second observation of the 1st floor pantry microwave was made. At that time, Staff #25 was made aware of the concern with the rusted microwave, had been reported to the surveyor by a resident's family member. Following the observation of the interior of the microwave, Staff #25 confirmed the findings and stated that nursing had never notified maintenance that there was a problem with the microwave. Staff #25 reported that the rusted microwave should not be used, and indicated the microwave would be disposed of. Staff #25 was then observed removing the microwave and carrying it out of the building.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on observation and staff interviews, it was determined that the Facility failed to have the call light within reach of a dependent resident. This was evident for 1 (#402) of 3 residents reviewed...
Read full inspector narrative →
Based on observation and staff interviews, it was determined that the Facility failed to have the call light within reach of a dependent resident. This was evident for 1 (#402) of 3 residents reviewed for Activity of Daily need (ADL) dependence during a revisit survey.
The finding include:
On 12/18/23 at 2:00 PM Resident #402 was observed lying in bed half asleep, further observation revealed that the call light could not be found. The resident was asked about their call light, and they stated that they did not know where it was. At 2:03 PM a Geriatric Nursing Assistant (GNA) #16 was called into the resident's room. She was asked how resident calls for assistance, and she said resident can use the call light. She was asked about the whereabouts of the call light. Staff #16 proceeded to look for the resident's call light. She searched around the room and underneath the resident's bed but could not find it. She asked the resident, and s/he said they did not know where it was. She searched some more and finally located it tucked inside the top drawer of the resident's nightstand; she pulled it out and clipped it next to the resident on the bed linen stating that night shift must have left it inside the drawer.
At 2:10 PM, the Director of Nursing (DON) was made aware of the findings and that this was a concern.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, it was determined that the facility failed to maintain a safe, clean, comfortable and homeli...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview, it was determined that the facility failed to maintain a safe, clean, comfortable and homelike environment. This was found to be evident on both floors of the nursing facility. The findings include:
1) On 9/16/24 between 1:00 PM - 2:00 PM, surveyor and the Maintenance Director #25 toured several resident rooms on both floors of the facility. During this tour, five out of nine bathrooms observed failed to have a functioning air vent exhaust system. When it was discovered that the exhaust in room [ROOM NUMBER]'s bathroom was not functioning, the Maintenance Director removed the vent cover and examined the vent with a flashlight, and stated he was not sure why there was no exhaust. In addition to room [ROOM NUMBER], the exhaust vents were found not to be working in the bathrooms in rooms 123; 205; 207; or. 231.
The concern regarding the ventilation system was addressed with the Nursing Home Administrator (NHA) on 9/18/24 at 4:20 PM.
2) On 9/10/24 at 12:27PM, Resident #55 reported the air conditioner unit in his/her room was not working and had not been working all summer. The resident reported it had been ok since the heat didn't bother him/her much, altough it did bother the roommate. The resident went on to express a concern that the heat might not work.
During an interview with the Maintenance Director on 9/16/24 at 12:50, he reported they have some back up units and if they can't fix a unit, then they will replace it. The director indicated he was aware that Resident #102's unit was not working and had just put in an order for a replacement.
On 9/18/24 at 4:20 PM, suveyor informed the NHA that multiple housekeeping and maintenance concerns were identified during the survey.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
Based on record review and interview, it was determined that the facility failed to honor residents' right to self-determination. This was evident for 1 resident (Resident #37) of 17 residents reviewe...
Read full inspector narrative →
Based on record review and interview, it was determined that the facility failed to honor residents' right to self-determination. This was evident for 1 resident (Resident #37) of 17 residents reviewed for Medical Orders for Life Sustaining Treatments (MOLST) documentation related to the Immediate Jeopardy investigation during the recertification survey. This had the potential to affect all residents who could make their own decisions.
The findings include:
On 9/13/24, an Immediate Jeopardy situation was declared due to conflicting resuscitation (code status) instructions for Resident #328. As a result of this situation, the facility conducted an audit to confirm all residents' choice of code status.
On 9/17/24 at 2:27 PM, a review of Resident #37's clinical records revealed that the resident was evaluated by the Medical Director on 7/18/24 and was determined to have capacity to make decisions.
On 9/17/24 at 2:39 PM, a review of documentation was conducted to verify that the facility had confirmed Resident #37's code status choice. The record contained a progress note, dated 9/17/24, written by Regional Social Work Director (SW #17) that stated Regional SWDP contacted patient's family to confirm full code status. The documentation did not include the name of the person contacted. A review of Resident #37's profile revealed 2 family members listed, a daughter and a sibling.
On 9/18/24 at 9:50 am, the Nursing Home Administrator (NHA) provided the survey team with an updated resident MOLST audit list and said that the list was correct and accurate.
On 9/19/24 at 9:34 AM, a review of the facility's audit list revealed that the facility alleged that Resident #37's code status had been confirmed.
On 9/19/24 at approximately 11:45 AM, during an interview with the Medical Director, Resident #37's clinical documentation was reviewed. Although the Medical Director had documented that the resident had capacity to make decisions, SW #17 documented that she asked the resident's family about the resident's code status but did not indicate the resident was asked. The Medical Director confirmed that Resident #37 should have been asked about his code status choice and that there was no evidence this was done.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 8). On 9/18/24 at 2:09 PM, an observation of room [ROOM NUMBER]-B was conducted. There was a hole in the drywall behind the resi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 8). On 9/18/24 at 2:09 PM, an observation of room [ROOM NUMBER]-B was conducted. There was a hole in the drywall behind the resident's bed at the level of the floor that measured approximately 8 inches long and 8 inches high and a 2-inch gaping hole.
On 9/18/24 at 2:15 PM, Licensed Practical Nurse (LPN #8) was interviewed in room [ROOM NUMBER]-B and when asked if she was aware of the hole in the wall, she said that the bed frame must have damaged it. When asked if the Maintenance Director was aware of the damaged wall, she said she was not sure but would ask him to come to the room.
On 9/18/24 at 2:25 PM, the Maintenance Director (Staff #25) was interviewed in room [ROOM NUMBER]-B and confirmed the damaged wall but said he was not aware of it. He described the process for staff to notify maintenance of any maintenance concerns; staff told the unit clerk and the unit clerk entered the information into the maintenance system which prompted a notification in the application that he used to track facility maintenance issues.
On 9/20/24 at 1:14 PM, an interview with the Director of Nursing (DON) was conducted to review that the wall was damaged in room [ROOM NUMBER]-B. The DON acknowledged the finding.
Based on observation and interview, it was determined that the facility failed to maintain a safe, clean, comfortable and homelike environment. This was found to be evident on both floors of the nursing facility. The findings include:
1a) On 9/10/24 at 2:37 PM, surveyor noted carpet in hallway near room [ROOM NUMBER] was stained in multiple areas. Continued observations made throughout the survey, on both the first and second floor, revealed multiple stains to the carpeting. On 9/13/24 at 10:04 AM during an interview with the Housekeeping Supervisor (Staff #49), she reported they have cleaned the carpets but the stains were still there and she was hoping they could pull them up. On 9/16/24 at 12:50 PM, in an interview with the Maintenance Director (Staff #25) it was reported that the facility had a plan in motion for the carpets and was just told by their supervisor a few weeks ago to get some quotes.
The NHA was made aware of the concern regarding the carpeting on 9/18/24 at 4:20 PM.
1b) On 9/11/24 at 9:48 AM, surveyor observed in room [ROOM NUMBER] in front of the HVAC (heating airconditioning and ventilation ) unit 6 floor imitation wood planks missing out of floor creating debits in the floor. Trim on wall opposite residents bed was coming off.
On 9/11/24 at 10:15 AM, surveyor observed in room [ROOM NUMBER] loose wooden floor planks in front of the HVAC unit. On 9/11/24 at 11:36 AM, observation in room [ROOM NUMBER] revealed wooden planks in the floor that were loose/coming off. On 9/11/24 at 12:50 PM, surveyor observed loose and missing floor tiles/ wooden planks in front of HVAC unit in room [ROOM NUMBER]. The tour of the facility on 9/16/24 with the Maintenance Director revealed several rooms on the first floor that had floors that were covered with a laminate that looked like wooden planks in which areas of the planks were missing. This included room [ROOM NUMBER] with a plank approximately 10 inches long missing; room [ROOM NUMBER] with loose planks in front of the HVAC unit which the Maintenance Director stated they needed to be glued down; and in room [ROOM NUMBER] which had multiple missing planks. As of time of survey exit on 9/23/24 at 1:00 PM, no documentation was provided to indicate new carpets or other flooring were ordered.
2a) On 9/11/24 at 1:01 PM, surveyor observed holes in Resident #378's bed linen.
On 9/11/24 at 11:38 AM surveyor observed Resident #13 in bed. A dime sized hole was noted in the fitted sheet near the foot of the bed. On 9/16/24 at 2:22 PM, the housekeeping supervisor reported laundry staff are suppose to check the sheets to make sure they are clean and without holes. She indicated sheets with holes should not go up to the units. Surveyor reviewed the concern that there were two seperate observations by surveyors of sheets with holes during the first few days of the survey.
2b) On 9/10/24 at 1:05 PM, Resident #55 reported a concern about not having sheets that fit [his/her] bed, indicating the facility only has 1 bariatric fitted sheet. A bariatric bed is larger than a standard sized bed.
On 9/16/24 at 2:22 PM, the housekeeping supervisor reported she had ordered bariatric sheets but was having a hard time getting them back after use. She confirmed the bariatric sheets were not coming back to the laundry. On 9/17/24 at 8:48 AM the Housekeeping supervisor provided documentation to support that bariatric sheets were ordered in April and August but confirmed that they had not been returned to laundry (for cleaning).
3) On 9/10/24 at 12:41 PM, observation of Resident #95's wheelchair revealed the padding on the right and left arm rest had multiple cracks. On 9/18/24 at 10:25 AM, surveyor and unit nurse manager observed Resident #95 in his/her wheelchair. The unit manager acknowledged the cracks in the arm rests and stated she would have them changed.
4a) On 9/11/24 at 10:42 AM surveyor observed a hole in wall where main door meets the wall in room [ROOM NUMBER]. On 9/13/24 at 1:45 PM observation in room [ROOM NUMBER]revealed the hole remains in the wall behind the door, additional concerns identified at this time included bed side table with damage; baseboard in bathroom with damage; and damage to the dresser. On 9/13/24 at 1:50 PM, surveyor observed the damage found in room [ROOM NUMBER] with housekeeper (Staff #60). Staff #60 reported the hole in the wall had been reported to maintenance. She also reported that she had reported the light not working on the computer [electronic reporting system], and that they fixed the bathroom light but not the room light.
4b) On 9/11/24 at 12:57 PM, observation of the bathroom in room [ROOM NUMBER] revealed a rectangular shaped hole under the sink approximately 10 inches by 3 inches where the plumbing was located. Additionally, the cord for the emergency call light was noted to be missing from the bathroom. On 9/11/24 at 3:14 PM surveyor informed the DON of the observation of no call bell cord on the emergency call bell in the bathroom.
5) On 9/11/24 at 11:33 AM, interview with Resident #24's family member revealed a concern with room cleaning, reporting it takes a long time for them to clean and they don't clean outside the schedule.
5a) On 9/11/24 at 12:57 PM, surveyor observed a brownish smudge on the wall behind the headboard of bed A in room [ROOM NUMBER]. Additionally, some of the laminate strip was noted to be missing on the side table, on part of the dresser drawer and along about half of the footboard.
On 9/13/24 at 10:04 AM, interview with the housekeeping supervisor revealed the resident rooms are cleaned every day, including the resident's bathroom. She reported they dust, sweep, mop, clean the window sills, check the walls and check the wheelchairs. She reports, if told to, they will clean the wheelchairs. If any environmental/maintenance issue are identified the staff should let her know and that they also have an electronic way to report concerns.
On 9/13/24 between 10:05-10:30AM, surveyor and housekeeping supervisor toured the facility.
On 9/13/24 at 10:15 AM, surveyor and housekeeping supervisor observed the brown smudge, like a swirled line, on an approxiately three x two inch area on the wall behind 240 bed A's headboard. Surveyor informed the supervisor this brown smudge was observed a few days earlier during the survey. The supervisor indicated she would have housekeeping wipe that off. Also observed damage to the baseboards in the bathroom, which housekeeping supervisor indicated had not been reported to her, and stated they may have thought already reported. Surveyor also pointed out the large hole under the sink, supervisor indicated this is a maintenance issue but indicated she would submit a report now that she was aware.
6b) On 9/11/24 at 11:06 AM, surveyor observed, in the bathroom of room [ROOM NUMBER], multiple brown spots on the wall to the left of the bathroom door and next to the emergency call light.
Additionally in the room paint was missing to the left and right of the mounted TV; and a large area of paint was missing under the hand sanitizer dispenser to the left of the outside bathroom door.
On 9/13/24, during the tour of the facility with the housekeeping supervisor, surveyor and supervisor observed the brown spots on the wall in the room [ROOM NUMBER]'s bathroom. Surveyor informed her they had previously been observed two days prior. Supervisor indicated the housekeeper should have caught this.
6c) On 9/16/24 at 3:45 PM, observation, with nurse #8, of the 2nd floor shower room, revealed cracked flooring, with an approximately 3 x 5 inch area missing; blue pads for shower bed observed with multiple cracks of approximatley 5 to 8 inch in length. On 9/16/24 at 4:10 PM, observation of the 2nd floor shower room was made with the unit nurse manager #12 who reported they wipe the showers down between residents. At that time, brown spots were observed on the floor of the shower and the unit nurse manager stated that it looked like stool and she indicated she would have the area cleaned. The unit nurse manager also observed and acknowledged the damage to flooring and the cracks in the pads to the shower chairs.
7) On 9/16/24 between 1:00 PM-2:00 PM during a tour of the facility with the maintenance director, surveyor observed 4 ceiling tiles with brown stains in the hallway between room [ROOM NUMBER] and 109.; and 3 ceiling tiles with brown stains between room [ROOM NUMBER] - 102. The Maintenance Director acknowledged the stains and indicated he thought it was from condensation from the air conditioner.
On 9/18/24 at 4:20 PM, suveyor informed the NHA that multiple housekeeping and maintenance concerns were identified during the survey.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on medical record review and staff interview, it was determined that the facility staff failed to develop and implement a comprehensive, resident centered care plan for a resident receiving psyc...
Read full inspector narrative →
Based on medical record review and staff interview, it was determined that the facility staff failed to develop and implement a comprehensive, resident centered care plan for a resident receiving psychotropic medications. This was evident for 1 (#78) of 5 residents reviewed for unnecessary medications, and 1 #(78) of 5 residents reviewed for unnecessary medications.
A care plan is a guide that addresses the unique needs of each resident. It is used to plan, assess and evaluate the effectiveness of the residents care
The findings include:
1) On 9/18/24 at 12:04 PM, a review of Resident #78's medical record documented the resident was admitted to the facility at the end of June 2024 and had a diagnosis which included depression.
Review of Resident #78's September 2024 Medication Administration Record (MAR) revealed an 8/20/24 order for Escitalopram Oxalate (Lexapro) (antidepressant) (psychotropic medication) by mouth one time a day for Depression that was documented as given every day from 9/1/24 to 9/13/24.
Review of Resident #78's care plans revealed a care plan with the focus, the resident has behaviors related to depressive disorder, initiated on 8/13/24, with the goal, the resident' s behaviors will not cause them or other resident' s distress thru the review period, that had 3 interventions, administer, medications as ordered, physician review of medications as needed, and remove resident from environment.
The care plan was not comprehensive, and resident centered, with no indication in the care plan of theresident's behaviors for which a psychotropic medication had been prescribed. In addition, the care plan failed to have measurable goals and interventions, including non-pharmaceutical interventions, to assist the resident with his/her behaviors.
The Director of Nurses (DON) was made aware of the above concerns on 9/18/24 and offered no comments at that time.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
4). On 9/10/24 at 11:53 PM, Resident # 109, a long-term resident of the facility and her/his family were interviewed. During the interview, Resident # 109 and her/his family reported that s/he just si...
Read full inspector narrative →
4). On 9/10/24 at 11:53 PM, Resident # 109, a long-term resident of the facility and her/his family were interviewed. During the interview, Resident # 109 and her/his family reported that s/he just sits in her/his bed all day and that he/she would like more interaction with the staff.
On 9/12/24, Resident #109's care plan was reviewed. The review revealed that the resident prefers or requires 1:1 activity. Further review revealed that activity preferences of the resident should be reviewed with the resident or the resident's representative if the resident was unable to communicate preferences.
On 9/12/24, Resident # 109's activity assessment was reviewed. The review revealed that the facility staff were interviewed regarding the residents' preferences for activities three days after the resident was admitted . Further review revealed a section titled past activity interests with 10 questions regarding the residents past activity interest. Review of this section revealed that 0 out of the 10 questions were answered on the assessment form.
On 9/12/24 at 3:58 PM, the Activity Director (Staff #9) reported that she documented all 1:1 activity done with residents at the facility in an activity binder. In addition, she reported that, if a resident cannot communicate what they like or dislike, she would interview the facility and staff and residents' family to obtain this information.
On 9/12/24 at 4:00 PM, observation of the activity logbook with the activity director failed to reveal that Resident #109 received any 1:1 activity since her/his admission in the facility.
On 9/12.24 at 4:01PM, continued interview with Staff # 9 revealed that she was aware that the resident family member visited the resident almost every day, but she had never interviewed the family to obtain information about resident's activity preferences.
On 9/20/24 at 10:50 AM, The above concerns were discussed concerns with admin and the DON. No additional information was provided to the survey team.
Based on medical record review, observation and interviews, it was determined that the facility failed to ensure that activities were provided to meet the needs of the residents. This was found to be evident for 4 (Resident #30, #95,
#13 and #109) out of 4 residents reviewed for activities during the survey.
The findings include
1) On 9/11/24 at 10:40 AM, Resident #30 was observed alone in his/her room in a wheelchair by, no music or other activity was observed at that time.
On 9/12/24, review of Resident #30's medical record revealed the resident had resided at the facility for several years and whose diagnoses included, but were not limited to: high blood pressure, kidney disease, major depressive disorder and dementia. Review of the Minimum Data Set (MDS) assessment, with a reference date of 6/5/24, revealed that the resident had a BIMS (Brief Interview for Mental Status) of 4 indicating severe cognitive impairment.
Review of the 9/5/24 MDS Section B revealed that the resident had clear speech and the ability to be understood and to understand others. Continued review of the 9/5/24 MDS revealed that the resident was interviewed in regard to activity preferences. This assessment revealed it was somewhat important for the resident to listen to music s/he liked and to go outside to get fresh air when the weather is good.
Review of the care plans revealed a plan initiated 10/30/23, with a revision date of 9/10/24 that stated: [Resident's name]'s behaviors have reduced. Resident prefers to attend group activities such as BINGO, group reminiscing, holiday celebrations, movie watching. The stated goal was that the resident would be satisfied with group activities thru the review period. The interventions included: activity calendar and assist resident to group activities as needed.
Further review of the care plans revealed another plan, initiated on 9/5/24 with a revision date of 9/10/24, that stated: [Resident #30's name] requires 1:1 activities due to being unwilling to participate in other activities , [his/her] behavior is unstable. The stated goal was that the resident will be satisfied with their 1:1 activities provided thru the review period. The interventions included: explore likes and dislikes of activities; provide 1:1 activities in the room or location that is the resident's preference as needed; and review activities preferences with the resident or resident representative if the resident is unable as needed.
No documentation was found in the care plan to reflect the activity assessment that indicated it was somewhat important for the resident to listen to music s/he liked, or to go outside when the weather was nice.
Further review of the medical record failed to reveal documentation to indicate the facility held an interdisciplinary care plan meeting since October 2023.
Further review of the medical record revealed a Multidisciplinary Care Conference note for the meeting held on 10/31/23. Review of this note failed to reveal documentation to indicate anyone from the activity department attended the meeting or provided input/summary as evidenced by blanks in the section of the note for activities staff to provide a summary.
On 9/12/24 at 3:38 PM interview with the Activity Director (Staff #9) revealed she had been the director for almost two months but worked at the facility as an activity assistant for 2 years. She confirmed she conducted the MDS assessment and created the care plans. She reported there was documentation for activity participation in the electronic health record and that she had a file for documentation of 1:1 visits. Surveyor was unable to view activity participation in the electronic health record, when asked to show surveyor documentation of participation in the computer the Activity Director was unable to do so. The Activity Director then indicated she would provide the 1:1 documentation.
On 9/12/24 at 4:19 PM the Activity Director provided documentation of a 1:1 Activities Log that had documentation of a 1:1 visit on 4/27/24 for Resident #30. She later confirmed this was the only documentation for Activities for Resident #30.
2) On 9/10/24 at 12:08 PM, Resident #95 was observed up and dressed and sitting in a wheelchair in the hallway.
On 9/11/24 at 10:07 AM, the resident was again observed sitting in the hallway in a wheelchair alone; At 10:44 AM, the resident was observed still in the wheelchair in the hallway but had wheeled self about half way down hall and was interacting with the staff working at a cart. On 9/11/24 at 12:04 PM, the resident was observed sitting in a wheelchair in the doorway of the resident's room. Resident was not observed to be attending any group activites on either 9/10/24 or 9/11/24. No observations were made of activity staff engaging with the resident.
On 9/12/24, a review of Resident #95's medical record revealed the resident had resided at the facility for a over one year and whose diagnoses include, but not limited to, dementia and lung disease.
Review of the 1/24/24 MDS assessment revealed that the resident's family was interviewed in regard to Activity Preferences. This assessment revealed it was very important to listen to music the resident liked and to participate in religious activities.
Review of the care plans revealed a plan for 1:1 Activities: [Resident #95's name] prefers or requires 1:1 activities due to being unable or unwilling to participate in other activities. The goal is [Resident] will be satisfied with their 1:1 activities provided thru the review period. The interventions include: provide 1:1 activities in the room or location that is the residents preference as needed and review activities preferences with the resident or resident representative if the resident is unable as needed. These interventions were established in August 2023 and have not been updated or personalized since then; although the goal included a notation by the unit nurse manager that it was revised on 7/29/24. The care plan failed to reflect the January assessment that listening to music and attending religious activites were very important to the resident.
Further review of the medical record failed to reveal documentation to indicate a care plan meeting had occurred since December 2023.
On 9/12/24 at 10:54 AM, the resident's responsible party reported being at the facility frequently. She also confirmed that there had been no recent care plan meetings.
On 9/12/24 at 4:27 PM, the Activity Director reported that the resident attended a celebration outside around 3:30 in the afternoon, indicated that the resident stayed for about 10 minutes then wanted to go back. The Activity Director was unable to provide documentation to support that the resident attended activities or was provided 1:1 visits. Surveyor also reviewed the concern regarding the failure to update the care plan interventions.
3) Review of Resident #13's medical record revealed the resident had resided at the facility for more than one year and whose diagnoses included, but were not limited to, dementia, heart disease and diabetes. Review of the 2/17/24 MDS assessment revealed that the resident was interviewed for Activity Preferences and that it was somewhat important to do things with groups of people; to go outside to get fresh air when the weather is good and to participate in religious services or practices.
Review of the care plans revealed a plan initiated on 8/30/24 for 1:1 Activities: the resident prefers or requires 1:1 activities due to being unable or unwilling to participate in other activities. The goal was the resident will be satisfied with their 1:1 activities provided thru the review period, there was a notation that this goal was revised by the unit nurse manager on 9/3/24. The interventions include: explore likes and dislikes of activities; provide 1:1 activities in the room or location that is the residents preference as needed and review activities preferences with the resident or resident representative if the resident was unable as needed. This care plan failed to reflect the February assessment that indicated it was somewhat important to do things with groups; to go outside to get fresh air or to attend/participate in religious services.
On 9/12/24 at 4:11 PM, surveyor was unable to find any activity documentation in the electronic health record for Resident #13 and proceeded to look through the 1:1 Activitiy log book. The Activity Director reported she could not locate the 1:1 documentation for this resident but stated: I know [he/she] came to the birthday bash and sometimes attends the master gardener, and sometimes the bible study.
On 9/18/24 at 4:20 PM, surveyor reviewed the concern regarding the facility's failure to provide activities with the Nursing Home Administrator and the Director of Nursing. As of time of survey exit on 9/23/24 at 1:00 PM, no additional documentation was provided to indicate activity participation or 1:1 visits for Residents #30, #95 or #13.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected multiple residents
3) In an interview with Resident #50 on 9/11/24 at 10:15 AM, s/he indicated that it was very important for him/her to receive pain medication on time. Timely administration of his/her pain medication ...
Read full inspector narrative →
3) In an interview with Resident #50 on 9/11/24 at 10:15 AM, s/he indicated that it was very important for him/her to receive pain medication on time. Timely administration of his/her pain medication prevents the pain from being unmanageable which makes it difficult for the resident to relax and sleep.
On 9/13/24 at 9:56 AM, Resident #50's medical record was reviewed and revealed a care plan for pain management with interventions to administer medications, notify physician as indicated, and to observe for indicators of pain. There was no evidence that non-pharmacological interventions were included to manage the resident's pain.
Current orders for Resident #50 were reviewed on 9/13/24 at 10:12 AM. The review revealed orders for the resident to be monitored for pain every shift and an opioid to be given routinely every six hours to control pain and discomfort. There was no evidence that non-pharmacological interventions were included to manage the resident's pain.
Opioids - Opioids are a class of drugs that derive from, or mimic, natural substances found in the opium poppy plant. Opioids work in the brain to produce a variety of effects, including pain relief. Opioid is the proper term, but opioid drugs may also be called opiates, painkillers, or narcotics.
On 9/16/24 at 12:23 PM, the facility's pain management policy, provided by the Director of Nursing (DON), was reviewed and indicated that non-pharmacological interventions are attempted prior to medication administration and were to be documented in the medical record.
On 9/16/24 at 2:09 PM, the narcotic count sheet for Resident #50 was reviewed in contrast with the electronic Medication Administration Record (eMAR). The review revealed that on 8/28/24, 9/7/24, and 9/10/24, Licensed Practical Nurse (LPN Staff #18) documented that she pulled the resident's narcotic pain medication at 2 PM when it was scheduled to be administered at 12 PM.
A medication administration audit report was provided by the DON, for the 3 dates stated above, that revealed the actual time the nurses were documenting their medication administration. A review of the report on 9/17/24 at 11:44 AM revealed that Resident #50's narcotic pain medication was administered late on 8/28/24, 12 PM dose was administered at 1:27 PM by Staff #18; on 9/7/24, 12 AM dose was administered at 2:10 AM by Registered Nurse (RN Staff #53); and on 9/10/24, 12 AM dose was administered at 1:38 AM by Registered Nurse (RN Staff #54), 6 PM dose was administered at 7:28 PM by Staff #18.
On 9/17/24 at 12:09 PM, Staff #18 was interviewed about her process for pain management. Staff #18 reported that when a resident complained of new pain she would notify the physician and for pain that was known or old pain, she would administer pain medication and recheck the resident after an hour to see if the medication was effective. Staff #18 failed to report that she would attempt non-pharmacological interventions prior to medication administration.
Staff #18 also reported her process with narcotic medications and when she documents on the narcotic count sheet. The concern was discussed that on 3 occasions, she documented that the 12 PM dose of Resident #50's pain medication was pulled at 2 PM. Staff #18 indicated that it was an error in documentation, and stated, I was not able to write the #1 to make it a #12. She further reported that the time the nurses sign the eMAR would be more accurate anyway and that they have an hour before or an hour after the schedule to administer medications.
The concerns were discussed with the DON that Resident #50's medical record failed to reveal that non-pharmacological interventions were attempted prior to administering pain medications and of the 3 days that was reviewed for medication administration, the nurses had administered the resident's pain medication late on 4 occasions. The DON verbalized understanding and acknowledged the concern.
2). On 9/10/24 at 7:23 AM in an observation of Resident #57, the resident was in bed and appeared to be asleep. The resident's family was at the bedside and was interviewed, and said the resident had reported pain from their sacral ulcer.
On 9/17/24 at 11:11 AM, a review of Resident #57's physician orders revealed that there were no active orders for any pain medication. A review of the September 2024 Medication Administration Record (MAR) revealed a section titled pain monitoring with an entry on 9/16/24 and that indicated that the resident's pain was 0 and was documented by Certified Medicine Aide (CMA #16). A review of the resident's September 2024 Treatment Administration Record (TAR) revealed documentation that the resident's sacral ulcer dressing was changed daily.
On 9/17/24 at 12:01 PM in an interview with Licensed Practical Nurse (LPN #34), she said that Resident #57 sometimes complained of pain, usually in their foot or shoulder. When LPN #34 was asked about the medicine aide's entries for pain monitoring on the resident's MAR, LPN #34 said that a medicine aide should not document a resident's pain, and that pain assessment and monitoring should be done by a licensed nurse.
On 9/18/24 at 2:15 PM in a follow up interview with Staff #34, she was asked if she was aware there were no pain medications ordered for Resident #57. Staff #34 replied that she thought the resident had Tylenol ordered but the CMA gave the resident's medications, so she was not sure.
On 9/18/24 at 1:07 PM, an interview with the Director of Nursing (DON) was conducted to review Resident #57's documentation of pain monitoring by the CMA. The DON said no CMA should document pain monitoring; it should be done by the nurse. The September 2024 MAR pain monitoring entries were reviewed with the DON and an additional 8 days were found where Staff #16 documented pain monitoring for Resident #57.
On 9/19/24 beginning at 10:57 AM, an interview was conducted with the Medical Director to review multiple clinical concerns. When he was informed that Resident #57 had a sacral wound but had no pain medications ordered, he responded that he was unaware of it and that any resident who had a sacral ulcer would be likely to have pain and should have pain medications ordered.
Based on interview and observation, it was determined that the facility 1). failed to provide a Resident with a physician ordered pain medication. 2). failed to ensure that residents' pain was evaluated and managed. 3). failed to develop and implement non-pharmacological interventions prior to administering pain medication and failed to administer the pain medication on time. This was evident for 3 (Resident # 31, # 57 #50,) out of 4 residents reviewed for pain management during a survey.
The finding include:
1). On 9/16/24 at 11:19 AM, Resident #31, a long-term care resident, requested an interview with surveyor. During the interview, s/he expressed concerns that he/she was not receiving his/her oxycodone pain medication.
On 9/16/24 at 11:53 AM, Resident #31's physician orders were reviewed. The review revealed an order for oxycodone HCL oral tablet 20mg 4 times a day for pain management.
On 9/16/24 at 11:55 AM, Resident 31's Medication administration record review revealed that from September first through September 16th at 8:00 AM, the resident received his medication 42 times out of the 62 times the medication was scheduled to be administered.
On 9/16/24 at 12:00 PM, review of progress notes revealed that no reason was documented when the oxycodone was not administered.
The Oxycodone HCL 20mg was not administered as prescribed the following date and times
9/1/24
8:00 AM
call made to the pharmacy pending delivery
9/1/24
2:00 PM
pending delivery
9/1/24
8:00 PM
awaiting delivery
9/2/24
8:00 AM
awaiting pharmacy to delivery
9/2/24
2:00 PM
awaiting pharmacy to send medications medications
9/2/24
8:00 PM
awaiting pharmacy to delivery medications
9/3/24
2:00 PM
awaiting pharmacy delivery
9/3/24
8:00 PM
awaiting pharmacy approval
9/4/24
2:00 AM
awaiting pharmacy approval
9/4/24
2:00 PM
awaiting pharmacy to send the medication
9/8/24
2:00 AM
No documentation as to why medication was not documented as administered on the MAR.
9/15/24
8:00 AM
Not administered pharmacy called
9/15/24
2:00 PM
Not administered
9/15/24
8:00 PM
PRN medication exposed
9/16/24
2:00 AM
Awaiting delivery from pharmacy
9/16/24
8:00 AM
Pending pharmacy delivery
On 9/16/24 at 12:23 PM, Nurse LPN (Staff # 8) was interviewed. She reproted that she was familiar with Resident #31's care. During the interview, she reported that the resident's medication was not available. She reported that it was her understanding that the residents insurance would not pay for the medication and that was why the pharmacy had not delivered the medication. She reported that last time Resident # 30 was administered his pain medication was 9/15/24 at 2:00AM.
On 9/16/24 at 2:10 PM, The Director of Nursing (DON)was interviewed. She reproted she is familiar with the care of Resident #31 and problems with his medication delivery. She repsoted she thought it was an insurance issue. The DON reported that the facility was responsible for obtaining the medications for a resident once they are admitted .
09/16/24 at 3:38 PM. the DON reported that the facility would ensure that the resident received his ordered medication, She stated the nurses were aware and were able to order ahead of time to ensure the medications were availabe for administration when scheduled.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected multiple residents
4). On 9/18/24 at 2:09 PM an observation of Resident #57 was conducted. The resident was in bed and the bed had half rail bed rails on both sides of the bed.
On 9/18/24 at 2:15 PM, an interview was co...
Read full inspector narrative →
4). On 9/18/24 at 2:09 PM an observation of Resident #57 was conducted. The resident was in bed and the bed had half rail bed rails on both sides of the bed.
On 9/18/24 at 2:15 PM, an interview was conducted with Licensed Practical Nurse (LPN #34) at Resident #57's bedside. LPN #34 was asked to check if the bed rail was secure and when she checked, it she said it was too loose and said she would call the Maintenance Director to repair it.
On 9/18/24 at 2:25 PM, the Maintenance Director (Staff #) came to Resident #57's room and was interviewed. He tested the bed rail and said that it was too loose and that he would repair it. He said he did regular checks on bed rails but was unaware that this one was loose.
On 9/20/24 at 1:14 PM in an interview with the Director of Nursing (DON), she said she was unaware of that Resident #57's bed had a loose bed rail. She was asked to provide any additional evidence for this observation but none was provided by the end of the survey.
Based on observation, medical record review, and staff interview, it was determined that prior to the installation or use of bed rails, the facility failed to ensure, 1) appropriate alternatives were identified and used, 2) the resident's risk of injury or entrapment was assessed, 3) the risks and benefits of bed rails was discussed with the resident/representative, 4) informed consent for bed rails was obtained, and 5) failed to ensure that a care plan with measurable objectives and specific interventions was developed for a resident's use of a bed rail. 6) that monitoring and supervision were provided during the resident's use of the bed rails, This was evident for 4 (#78, #380, #13, #57) of 4 residents reviewed for side rails.
The findings include:
Bed rails are adjustable bars that attach to the bed and are available in a variety of types, shapes, and sizes. As enablers, bedrails facilitate movement and may promote independence. Entrapment is an event in which a resident is caught, trapped, or entangled in the space in or about the bed rail.
1) On 9/11/24 at 11:00 AM, an observation was made of Resident #78 lying in bed with bilateral bed rails attached to the resident's bed. On 9/18/24 at 2:39 PM, Resident #78 was again observed lying in bed, and bilateral bed rails were observed attached to the resident's bed.
On 9/18/24 at 12:04 PM, a review of Resident #78's medical record revealed an Admission/readmission Collection Tool, with an effective date, 6/30/24 at 10:41 PM, that included a Bed Side Rail Tool with the heading Nursing Evaluation and Consent Tracking, followed by 8 bed rail evaluation questions. The evaluation asked, Does the resident need bed rails for positioning and/or rising from supine to sitting/standing position as mobility enabler? and documented the response, No, indicating Resident #78 did not need bed rails as a mobility enabler for positioning and/or rising. The responses to the remaining questions were blank, with no other documentation found in the bed rail evaluation tool.
Continued review of Resident #78's medical record failed to reveal a physician's order for the resident's use of bed rails. In addition, the medical record failed to reveal documentation that, prior to the installation or use of the bed rails, appropriate alternatives were identified and used, the resident's risk of injury or entrapment was assessed, that the risks and benefits of bed rails was discussed with Resident #78 or resident representative and informed consent obtained. The medical record failed to reveal documentation of monitoring and supervision provided during the resident's use of the bed rails and failed to reveal a care plan with measurable objectives and specific interventions for use of the bed rail had been developed for Resident #78.
2) On 9/11/24 AT 10:37 AM, an observation was made of Resident #380 lying in bed and bilateral bed rails were observed attached to the resident's bed
On 9/19/24 at 3:36 PM, a review of Resident #380s medical record revealed an Admission/readmission Collection Tool with an effective date of 9/5/24 at 8:20 PM, that revealed a Bed Side Rail Tool, followed by 8 bed rail evaluation questions. The evaluation asked, Does the resident need bed rails for positioning and/or rising from supine to sitting/standing position as mobility enabler? and had the documented response, No, indicating Resident #380 did not need bed rails as a mobility enabler for positioning and/or rising. The responses to the remaining questions were blank, with no other documentation found in the bed rail evaluation tool.
Continued review of Resident #380's medical record failed to reveal a physician's order for the resident's use of bed rails. In addition, the medical record failed to reveal documentation that prior to the installation or use of the bed rails, appropriate alternatives were identified and used, the resident's risk of injury or entrapment was assessed, that the risks and benefits of bed rails was discussed with Resident #380 or resident representative and informed consent obtained. The medical record reviewed failed to reveal documentation of monitoring and supervision provided during the resident's use of the bed rails and failed to reveal a care plan with measurable objectives and specific interventions for use of the bed rail had been developed for Resident #380.
3) On 9/11/24 at 11:36 AM, an observation was made of Resident #13 lying in bed and a quarter side rail in the up position was observed attached to the right side of the resident's bed.
On 9/18/24 at 3:28 PM, a review of Resident #13's medical record revealed the resident resided in the facility for long term care since the end of July 2022 and had multiple diagnosis which included dementia. Review of the resident's quarterly assessment with an assessment reference date of 8/19/24 revealed Resident #13's Brief Interview For Mental Status (BIMS) summary score was 3, indicating the resident had severe cognitive impairment.
Further review of Resident #13's medical record revealed a Bed Side Rail Tool with an effective date of 5/1/14 at 12:04 PM with the heading Nursing Evaluation and Consent Tracking, followed by 8 bed rail evaluation questions. The bed rail evaluation tool asked, Does the resident need bed rails for positioning and/or rising from supine to sitting/standing position as mobility enabler? with the documented response, Yes, indicating the resident used the bed rails for positioning and/or as a mobility enabler, however, the evaluation tool also documented bed rails were not indicated as a mobility enabler at that time. The bed side rail tool documented bed rails were a resident/representative preference and a ½ partial bed rail was on the right side of Resident #13's bed. The Bed Side Rail tool also included the question, Risk verses benefits and consent obtained for side rails, and documented the response patient/resident, indicating the consent for the side rails was obtained from the resident, however, no documentation was found to indicate what were the risks verses benefits of side rails that were discussed with Resident #13. In the bed side rail tool, was a heading, Plans for side rail reduction which was followed by the statement, explain the plan and update the care plan, that had the printed response, Daughter, and documented the bed rail did not restrict the patient/resident movements,
Continued review of Resident #13 medical record failed to reveal a physician's order for the resident's use of bed rails, failed to reveal documentation that prior to the installation or using the bed rails, appropriate alternatives were identified and used, and failed to reveal documentation that an assessment of the resident, the bed, the mattress, and rail for entrapment risk (which would include ensuring bed dimensions are appropriate for resident size/weight), and was assessed. The medical record review failed to reveal documentation of any monitoring and supervision provided during the resident's use of the bed rails and failed to reveal a care plan with measurable objectives and specific interventions for use of the bed rail had been developed for Resident #13.
On 9/19/24 at 3:40 PM, the above concerns related to bed rails were discussed with the Director of Nurses (DON), who acknowledged the concerns and offered no further comments at that time.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected multiple residents
2a) A brief look into Resident #24's medical record indicated that s/he was admitted in August of 2024 with diagnoses that included congestive heart failure.
Congestive heart failure (CHF) is a seriou...
Read full inspector narrative →
2a) A brief look into Resident #24's medical record indicated that s/he was admitted in August of 2024 with diagnoses that included congestive heart failure.
Congestive heart failure (CHF) is a serious condition that occurs when the heart can't pump enough blood to meet the body's needs. This causes fluid to build up in the body's organs, which is known as congestive. Most patients will be started on a diuretic when they are first diagnosed with heart failure to help relieve congestion
A diuretic is any substance that promotes diuresis, the increased production of urine. This includes forced diuresis. A diuretic tablet is sometimes colloquially called a water tablet. There are several categories of diuretics. All diuretics increase the excretion of water from the body, through the kidneys.
A review of Resident #24's medication orders on 9/12/24 at 9:09 AM include an order of a diuretic to be given in the morning with instructions to hold for a systolic blood pressure less than 110 and update the physician.
Blood pressure (BP) is often written as an upper and lower number. Systolic blood pressure (SBP) is the upper number. It measures the pressure in the arteries during heart muscle contraction.
On 9/12/24 at 10:06 AM, Resident #24's BP report was reviewed and revealed that, on 9/6/24, the resident's BP was 105/60, documented by Registered Nurse (RN Staff #48) at 7:40 AM.
Subsequently, at 10:14 AM, Resident #24's electronic Medication Administration Record (eMAR) was reviewed and revealed that, on 9/6/24, Staff #48 administered the diuretic that was scheduled at 8:00 AM.
On 9/17/2024 at 1:08 PM, the concern was discussed with the Director of Nursing (DON) that Staff #48 did not hold the administration of the diuretic per instructions. The DON acknowledged the concern but offered no explanation.
2b). Resident #50 was admitted in August of 2024 with diagnoses that included Chronic Pain.
A review of Resident #50's medical record on 9/13/24 at 10:12 AM, revealed a narcotic pain medication order to be administered every 6 hours as needed for pain. this order had a start date of 8/24/24 and was discontinued on 8/28/24.
Opioids - Opioids are a class of drugs that derive from, or mimic, natural substances found in the opium poppy plant. Opioids work in the brain to produce a variety of effects, including pain relief. Opioid is the proper term, but opioid drugs may also be called opiates, painkillers, or narcotics.
A subsequent review of Resident #50's electronic Medication Administration Record (eMAR) on 9/16/24 at 2:09 PM, indicated that the narcotic pain medication was administered on 8/27/24 at 4:10 PM for a pain score of 0 by Licensed Practical Nurse (LPN Staff #55).
The findings in Resident #50's eMAR was discussed with the Director of Nursing (DON) on 9/17/24 at 1:17 PM. The DON acknowledged the concern and agreed that pain medications should not be administered when there are no reports/complaints of pain. the DON offered no explanation as to why Staff #55 administered the narcotic pain medication for a pain level of 0.
3) A medical record review completed for Resident #78 on 9/16/24 at 8:30 AM found an attending provider's order, dated 7/10/24, that stated, Lidocaine External Patch 5 % (Lidocaine) Apply to back topically one time a day for pains in back, CDI (clear, dry, and intact) skin only take off after 12 hours.
Further review contained Resident #78 medication administration record for August 2024. The review showed that the patch was placed on Resident #78's back daily from August 1 to September 16, 2024; however, it failed to show that the patch was removed daily.
Lidocaine Patch is used to manage pain. Depending on the product, the patch may be left on the skin for up to 8 or 12 hours. Applying too many patches or topical systems or leaving them on too long may cause serious side effects.
In an interview on 9/16/24 at 12:28 PM, staff #21, a certified medicine aide (CMA), reported that the attending provider's order for Resident #78's Lidocaine patch was incomplete because it did not contain the time to remove it. Therefore, there was no place in the medication administration record (MAR) to sign for the removal.
In an interview on 9/17/24 at 9:31 AM, the director of nursing (DON) confirmed that the attending provider's order for Resident #78's Lidocaine patch did not contain a removal time or schedule and, therefore, did not have a place on the MAR for the nurses who removed it to document.
Based on medical record review and staff interview, it was determined the facility failed to keep a resident's drug regimen free from unnecessary drugs by 1) failing to follow physician ordered blood pressure parameters for administering medication, and 2) failing to ensure prescribed medications had adequate parameters in place to indicate when to administer as needed medications for pain. 3) failing to ensure that an attending provider's orders for a resident's topical anesthetic medication included a time to remove it This was evident for 3 (#78, # 25, # 50) of 5 residents reviewed for unnecessary medications, and 1 (#380) of 4 residents reviewed for pain management.
The findings include:
1) On 9/13/24 at 12:36 PM, a review of Resident #78's medical record revealed the resident was admitted to the facility at the end of June 2024 following an acute hospitalization with multiple diagnosies including left hip fracture, and hypotension (low blood pressure).
1a) Review of Resident #78's July 2024 Medication Administration Record (MAR) revealed a 7//1/24 order for Oxycontin (oxycodone) (narcotic) tablet by mouth two times a day for pain level greater than 5 for 30 days, hold for S (systolic) BP (blood pressure) (1st number of a BP) less than 110, hold for excessive sedation, which was discontinued on 7/11/24. The MAR documented that Resident #78 received the Oxycontin two times a day, every day from 7/2/24 to 7/10/24.
There was no documentation in the MAR to indicate that Resident #78's blood pressure was monitored prior to the administration of the oxycontin, and that the Oxycontin had been administered within the parameters of the physician's order. In addition, there was no documentation in the MAR to indicate Resident #78's pain level was assessed prior to the administration of the narcotic medication, and there was no documentation to indicate the effectiveness of the medication in managing the resident's pain.
1b) Review of Resident #78's September 2024 MAR) revealed an 8/13/24 order for Midodrine (treats low BP), Give 1 tablet by mouth three times a day for hypotension (low BP) hold for SBP more than 130. The Midodrine was documented as given at 9:00 AM on 11 (9/3, 9/4, 9/5, 9/6, 9/7, 9/8, 9/9, 9/10, 9/11, 9/12, 9/13) of 11 days in September 2024, documented as given at 1:00 PM on 10 (9/3, 9/4, 9/5, 9/6, 9/7, 9/9, 9/10, 9/11, 9/12, 9/13) of 11 days in September, and the Midodrine was documented as given on 7 (9/3, 9/5, 9/7, 9/8, 9/9, 9/11, 9/12) of 10 days in September 2024 with no documentation found in the MAR to indicate the resident's BP was monitored prior to the administration Midodrine and that the Midodrine had been administered within the parameters of the physician's order.
The above concerns were discussed with the Director of Nurses (DON) on 9/18/24 at 5:11 PM, with no response offered at that time.
2) On 9/19/24 at 10:55 AM, a review of Resident #380's medical record was conducted. Review of Resident #380's September 2025 MAR revealed a two orders for medication which were prescribed to be administered as needed for pain. The resident had a 9/5/24 order for Acetaminophen (Tylenol) Oral Tablet 325 MG (milligrams) give 2 tablets by mouth every 4 hours as needed for pain, and a 9/6/24 order for Percocet Oral Tablet 10-325 MG (Oxycodone w/ Acetaminophen) give 1 tablet by mouth every 4 hours as needed for pain. There was no indication in either order as to when to give which medication, the Acetaminophen or the Percocet, first for pain.
The above concerns were discussed with the Director of Nurses on 9/19/24 at 3:40 PM. DON acknowledged the concerns at that and offered no further comments.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0800
(Tag F0800)
Could have caused harm · This affected multiple residents
Based on observation, review of meal tickets and interview, it was determined the facility failed to ensure residents were served the correct portions and items as indicated on their meal tickets. Thi...
Read full inspector narrative →
Based on observation, review of meal tickets and interview, it was determined the facility failed to ensure residents were served the correct portions and items as indicated on their meal tickets. This was found to be evident for one out of one test tray obtained during the survey.
The findings include:
On 9/11/24 at 10:44 AM, Resident #115 reported the physician had advised him/her to get a high protein diet but there seemed to be a disconnect because the resident was not getting that diet consistently.
On 9/12/24 at 11:45 AM, observation of the tray line revealed a 1/2 cup scoop was being used for the portions, except for the beef pepper steak (Chopped up thinnly sliced beef) which was being served by the [NAME] (Staff #63) with a set of tongs. When asked about this practice, the [NAME] confirmed only using the tongs and proceeded to pick up a portion stating it was three ounces.
During this observation, surveyor picked a tray at random from trays already made up and on the food cart. A copy of the ticket was obtained. The ticket was for Resident # 35 and indicated the tray was suppose to include:
Grilled cheese sandwich 1 sandwich
Sugar snap peas 1 cup
Mashed potatoes 1/2 cup
Dinner roll
Margarine 1 each
Tossed salad with dressing
Chocolate pudding parfait 1/2 cup
Hot Tea
The observation of this test tray did not match the ticket for the following items:
Sugar snap peas: half cup
No dinner roll
no chocolate pudding parfait; instead it was a chocolate cream pie
On 9/12/24 at 1230 PM, the test tray was observed by the Food Service Director (Staff #62) who confirmed the pea serving was half a cup; that there was no dinner roll and that they made a mistake in regard to the chocolate cream pie being serviced rather than the parafait. She confirmed all the scoops being used during the tray service line were half cup.
Surveyor reviewed the concern with the FSD #62 that a resident had made a report about not receiving the correct portions. Also reviewed the concern that the cook was not using a scoop for the chopped meat , she confirmed the scoop should of been used.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected multiple residents
Based on observation, medical record review and staff interview, it was determined the facility failed to conduct a regular inspection of all bed frames, mattresses, and bed rails, as part of a regula...
Read full inspector narrative →
Based on observation, medical record review and staff interview, it was determined the facility failed to conduct a regular inspection of all bed frames, mattresses, and bed rails, as part of a regular maintenance program to identify areas of possible entrapment and failed to ensure the equipment was inspected and maintained according to manufacturer's recommendations and requirements and timeframes. This was evident for 3 (#78, #380, #13) of 3 residents reviewed for bed side rails and had the potential to affect all residents. The findings include:
On 9/11/24 AT 10:37 AM, an observation was made of Resident #380 lying in bed and bilateral bed rails were observed attached to the resident's bed. On 9/11/24 at 11:00 AM, an observation was made of Resident #78 lying in bed and bilateral bed rails were observed attached to the resident's bed, and on 9/18/24 at 2:39 PM, Resident #78 was again observed lying in bed with bilateral bed rails observed attached to the resident's bed.
On 9/11/24 at 11:36 AM, an observation was made of Resident #13 lying in bed. At that time, a quarter side rail in the up position was observed attached to the right side of the resident's bed.
On 9/18/24 at 4:50 PM, during an interview, Staff #25, Maintenance Director, indicated he was employed as the maintenance director for approximately 1 year. When asked if the facility assured the inspection of all bed frames, mattresses, and bed rails, as part of their regular maintenance program, Staff #25 stated that since he had been at the facility, one audit of resident beds had been done to make sure there was no gap between the mattress and the rail, but that routine bed audits were not done. Staff #25 reported that the bed audit only included resident beds on the first floor of the facility, and an audit of the resident beds on the second floor had not been completed. Staff #25 indicated when there was a problem with a resident's bed, mattress or siderail, the problem would be reported to maintenance by nursing or housekeeping, and maintenance replaced the mattress as needed. Staff #25 indicated that maintenance did not add rails to resident beds unless instructed to do so. Staff #25 stated that if an existing resident bed had a bed rail that broke, the facility might have a spare rail to replace it, however, new beds purchased for the facility didn't come with rails, and a bed rail could not be added to those beds.
Following the interview, the concerns with failing to conduct regular inspection of all bed frames, mattresses, and bed rails, to prevent risk of entrapment, and ensure the equipment was inspected and maintained according to manufacturer's recommendations, requirements, and timeframes were discussed with Staff #25, who at that time, indicated understanding of the concerns.
The Director of Nurses was made aware of the concerns on 9/19/24 at 3:40 PM, and the DON acknowledged the concerns with no further comments offered at that time,
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 7). On 9/11/24 at 12:31 PM, a review of Resident #10's clinical record revealed a care plan entry that stated SKIN IMPAIRMENT: t...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 7). On 9/11/24 at 12:31 PM, a review of Resident #10's clinical record revealed a care plan entry that stated SKIN IMPAIRMENT: the resident has a skin impairment, Date Initiated: 07/25/2024, Created on: 07/25/2024, Created by: [Licensed Practical Nurse (LPN #47)].
On 9/16/24 at 2:13 PM, an interview was conducted with the Director of Nursing (DON) who said the resident does not have any skin issues.
On 9/17/24 at 11:41 AM, an interview with unit nurse, LPN #34, was conducted and she explained that Resident #10 had an issue with the skin on their leg, but it was healed now. When asked what the process was for revising the care plan, Staff #34 said usually either the unit manager or the social worker updated resident care plans, she said that she did not really know how to do it.
On 9/17/24 at 1:01 PM, the DON was interviewed again and confirmed that Resident #10's skin issue remained on the care plan but should have been discontinued as the resident no longer had any skin issues.
8). On 9/16/24 at 10:35 AM, a review of Resident #100 revealed care plan meeting documentation, dated 11/29/23.
On 9/16/24 at 10:44 AM, the Director of Social Work (SW #19) was interviewed and asked when Resident #100's last care plan meeting was held. SW #19 said the last care plan meeting was held on 11/29/23 and confirmed that the resident should have had care plan meetings February 2024, May 2024, and August 2024 but did not.
6). On 9/10/24 at 7:34 AM, Resident #84, a long-term resident of the facility, was interviewed. During the interview s/he reported that s/he could not recall the last care plan meeting that she attended.
On 9/11/24 at 11:36 AM, review of a progress note revealed a care plan meeting on 1/29/24. Further review failed to reveal any additional care plan meetings in 2024.
On 09/12/24 at 3:09 PM, a review of assessment documents titled Multidisciplinary care conference, revealed the resident had care plan meetings on 6/2/23, 10/14/22 and 1/29/24.
On 09/12/24 at 1:52 PM, during an interview with the Director of Social Services (Staff #19), she reported that care plan meetings should be quarterly.
On 09/12/24 03:45 PM, during an interview the Director of Nursing, it was confirmed that Resident #84 had only one care plan in 2024.
On 09/19/24, the Director of Nursing provided the care planning policy with an effective date of 11/01/2019. Review of the care plan revealed the quarterly care plan meeting should occur after the quarterly assessment.
On 09/20/24 at 10:50 AM, review of concerns with the Administrator and the Director of Nursing provided no additional information to the survey team.
4) On 9/11/24 at 10:57 AM, when asked if the resident attended care plan meetings and participated in his/her care planning, Resident #78 stated that s/he could not recall attending care plan meetings.
On 9/13/24 at 12:36 PM, a review of Resident #78's medical record revealed the resident was admitted to the facility at the end of June 2024. Review of Resident #78's MDS assessments revealed assessments which included a 5-day admission assessment with an assessment reference date (ARD) of 7/4/24 and quarterly assessment with an ARD of 8/28/24.
Continued review of the medical record failed to reveal documentation to indicate that a care plan meeting had been conducted following Resident #78's admission assessment with an ARD of 7/4/24, or that an interdisciplinary care plan meeting had been conducted following Resident #78's quarterly assessment with an ARD of 8/28/24.
On 9/16/24, at approximately 2:30 PM, Staff #20, Licensed Practical Nurse (LPN), Regional Director Of Clinical Reimbursement, was made aware of the concern that there was no evidence a care conference had been conducted with Resident #78 since his/her admission assessment. ARD 7/4/24 or since the resident's quarterly assessment 8/28/24. Staff #20 confirmed the findings, and no further comments were offered at that time.
Continued review of Resident #78's medical record on 9/18/24 at 12:04 PM, revealed that, on 6/30/24 at 10:41 PM, in an admission/readmission nursing note, the nurse documented that Resident #78 was admitted to the facility following a hospitalization with a chief complaint of a fall which resulted in a hip fracture.
Continued review of Resident #78's medical record revealed on 7/10/24 at 2:00 PM, in a SBAR (Situation, Background, Assessment, Recommendation) (a standard way to communicate medical information) Summary for Providers note, the nurse documented Resident #78 had a fall, and the resident was found kneeling at the bedside.
Review of Resident #78's care plans revealed a care plan, the resident is at risk for falls r/t (related to) unsteady gate, created on 6/30/24, with the goal, the resident will not have an injury related to a fall through the review period. The care plan had 2 interventions, place common items within reach of the resident and remind the resident to use their call light to ask for assistance with ADLs (activities of daily living), created on 6/30/24, and included 2 interventions, place bed in lowest position while resident is in bed, and therapy referral, created 7/11/24, which was after the resident's fall on 7/10/24.
In a SBAR Summary for Providers note, on 7/17/24 at 9:10 PM, the nurse documented that Resident #78 had a fall, and indicated the physician was notified and a urinalysis, and urine culture and sensitivity were ordered. There was no summary of the observation, and no other documentation in SBAR to indicate the circumstances around the resident's fall.
Continue review of Resident #78's medical record failed to reveal documentation to indicate that, following the resident's fall on 7/17/24, Resident #78's fall care plan was reviewed for effective interventions and failed to reveal evidence that following the resident's quarterly assessment with an ARD of 8/28/24, Resident #78's care plans were reviewed by the interdisciplinary team and revised based on the changing goals, preferences and needs of the resident and in response to current interventions.
On 9/18/24 at 5:11 PM, the Director of Nurses (DON) was made aware of the above concerns on 9/18/24 at 5:11 PM, and the DON offered no further comments at that time.
5). On 9/12/24 at 10:20 AM, a review of the EMR (Electronic Medical Record) revealed Resident #55 resided in the facility for long term care since 2020 and was readmitted to the facility following a brief hospitalization in the beginning of August 2024.
Review of Resident #55's completed MDS assessments revealed a 9/10/23 quarterly assessment, a 12/11/23 quarterly assessment, a 3/10/24 annual assessment, a 6/10/24 quarterly assessment, and an 8/13/24 5-day assessment. Review of Resident #55's most recent 5-day assessment with an assessment reference date (ARD) of 8/13/24 documented Resident #55's BIMS (brief interview for mental status) summary score was 15, indicating the resident was cognitively intact.
Further review of Resident #55's medical record revealed, on 10/3/23 at 11:30 AM, in a Multidisciplinary Care Conference note, Social Services indicated Resident #55 had an interdisciplinary team (IDT) care plan meeting on that date. No further documentation was found in Resident #55's medical record to indicate that IDT care plan meetings had been conducted with Resident #55 following his/her completed MDS assessments with an ARD 12/11/23, 3/10/24, 6/10/24 and 8/13/24.
On 9/16/24 at 12:25 PM, the above concerns were discussed with Staff #19, Director of Social Services. At that time, Staff #19 indicated that there had been a turnover of social services staff which affected the long-term care conferences, and that it was most likely no care conferences were done during that time. Staff #19 then confirmed that a care plan meeting had not been conducted with Resident #55 following since October 2023 and following each assessment.
Based on medical record review and interview, it was determined that the facility failed to
have an effective system in place to ensure interdisciplinary care plan meetings were
occurring after assessments; and failed to ensure care plans were being reviewed and
revised as needed. This was found to be evident for 8 (Resident #30; #23; #95; #78, #55. #84, #10, #100 ) out of 17 residents reviewed during the survey
The findings include:
1) Review of Resident #30s medical record revealed the resident had resided at the
facility for several years and whose diagnoses included, but were not limited to, high blood
pressure, kidney disease, major depressive disorder and dementia. Review of the
Minimum Data Set assessment, with a reference date of 6/5/24, revealed the resident
has a BIMS (Brief Interview for Mental Status) of 4 indicating severe cognitive
impairment.
On 9/13/24 at 11:09 AM, the unit nurse manager #12 reported care plan meetings are
scheduled and family and residents are invited, and that therapy, dietary, social work
and nursing also attend. When asked how the physicians or nurse practitioners are
involved in the care plans, the unit manager reported if the family has concerns they
would ask the physician to call the family and then referred the surveyor to the
Multidisciplinary Care Conference note. The unit nurse manager confirmed that
whenever there is a care conference this note will be used.
Further review of the Multidisciplinary Care Conference note template revealed
an area for summaries from nursing, dietary, recreation, social work, pharmacy,
restorative/PT/OT, and the physician. There is also a section at the end for
Resident/Family expectation/Concerns and Care Level Review.
Further review of the medical record revealed a Multidisciplinary Care Conference note
for a meeting held on 10/31/23. Review of this note revealed the participants included a
registered nurse, social worker, resident and the health care agent. Although in the
attendance section Registered Nurse is checked, no documentation was found in the note
to identify the name of the nurse that attended. The areas of the note for
input/summaries from nursing, dietary, recreation (Activities), pharmacy, restorative and
physician were all noted to be blank.
On 9/16/24, review of Resident #30's medical record failed to reveal documentation to
indicate a care plan meeting has occurred since the 10/31/23 meeting. This information
was reviewed with the SSD #19 during an interview on 9/16/24 at 10:01 AM. The SSD
reported she attempted a care plan meeting but there should be a note that the Health
Care Agent (HCA) declined. Further review of the medical record revealed a Discharge
Planning Progress note, signed by SSD #19 on 6/19/24, which indicated that the HCA
declined a transfer and included the following: SW notified resident that a care plan
meeting would be initiated to support a possible transfer and provide more information
from the IDT team. Further review of the medical record failed to reveal documentation
to indicate that a care plan meeting was scheduled as indicated in the 6/19/24 note.
2) Review of Resident #23's medical record revealed the resident was originally
admitted to the facility in June 2024. Review of the 6/11/24 Minimum Data Set (MDS)
assessment revealed the resident had functional limitations in range of motion on both
sides for upper extremities (arms) and impairment on one side for lower extremities
(legs). The resident was dependent on staff for activities of daily living. The resident
was receiving occupational, speech and physical therapy in June.
During an interview with the resident 39's Health Care Power of Attorney (HCPOA) on
9/11/24 at 1:22 PM revealed concerns regarding not being informed about the resident's
care.
On 9/17/24 at 1:58 PM, review of the medical record failed to reveal a Multidisciplinary
Care Conference note that would indicate a care plan meeting had occurred during the
resident's admission.
On 9/18/24, after requesting documentation from the Director of Nursing of any care plan that may have occurred for the resident, staff provided a note completed by the unit
nurse manager titled Care plan meeting dated 9/3/24 that stated: Care plan meeting
held with resident 23's [family members]. Resident medications reviewed with no concerns
voiced. Plan of care continues. No documentation was found to indicate who attended the 9/3/24 meeting other than the family and the unit nurse manager who wrote the note. No documentation was found to indicate other members of the interdisciplinary team attended the meeting, or
provided input.
On 9/18/24 at 11:00 AM, the Rehab Director presented the surveyor with the resident's physical therapy Discharge summary, dated [DATE]. The Rehab Director reported the resident
had made great progress in therapy and at the time of discharge the resident's gait
distance (walking) was 125 feet with hand held assist and could transfer from chair to
bed and bed to chair with contact guard. (A transfer with contact guard assist means the care giver places one or two hands onthe resident to help with balance but no other assistance is provided).
When asked if the ability to walk and transfer with contact guard was reflected in the
resident's care plan, the Rehab Director replied that it might be. When asked if the resident
should continue to walk, the Rehab Director reported that, because of cognitive deficits
this would not be realistic to maintain but that theortically could have been walking to the
dining room. Surveyor clarified that the resident could be doing some walking, to which
the Rehab Director responded: yes, [s/he] could with support obviously. The Rehab
Director indicated that therapy personnel would be part of a care plan meeting for a
short term (skilled) admission.
No documentation was found to indicate a respresentative from the therapy department
attended or provided input for the 9/3/24 care plan meeting.
Review of care plan addressing the residents risk for falls revealed a revision date of
9/13/24. The interventions included, but were not limited to, : Resident is a hoyer lift transfer
with 2 GNAs. This intervention was created and initiated on 8/14/24. No
documentation was found to indicate that, when the revision was completed on 9/13/24
that the person completing the revision was aware that the resident was no longer using
a hoyer lift.
A hoyer lift is a mechanical lift used for residents who are completely dependent on staff
for transfers. A hoyer lift pad is placed under the resident and then attached to the lift.
Two staff members will then use the mechanical lift to raise the resident from the bed
and transfer to a chair or vice versa.
During the 9/18/24 11:00 AM interview, surveyor reviewed with the Rehab Director that
the current care plan indicated the resident required a hoyer lift with 2 GNA assist, in
place since 8/14/24. The Rehab Director responded that it could have been so at that time.
On 9/18/24 at 11:52 AM, the unit nurse manager #12 reported the resident does stand
with one person assist and in regard to walking, she reported: if we see [him/her] get up
we walk around with [him/her]. The unit nurse manager indicated they did conduct staff
training but confirmed it was not documented. Surveyor reviewed the concern that the
care plan still stated the resident requireda hoyer lift for transfers, the unit manager
indicated she would update this information.
3) On 9/12/24, review of Resident #95's medical record revealed the resident had
resided at the facility for a over one year and whose diagnoses included, but were not limited
to, dementia and lung disease.
Review of the 1/24/24 MDS assessment revealed the resident's family was interviewed
in regard to Activity Preferences. This assessment revealed it was very important to
listen to music the resident liked; and to participate in religious activities.
Review of the care plans revealed a plan for 1:1 Activities: [Resident #95 name]
prefers or requires 1:1 activities due to being unable or unwilling to participate in other
activities. The goal is [Resident] will be satisfied with their 1:1 activities provided thru
the review period. The interventions included: provide 1:1 activities in the room or
location that is the residents preference as needed and review activities preferences
with the resident or resident representative if the resident is unable as needed. These
interventions were established in August 2023 and have not been updated or
personalized since then; although the goal included a notation by the unit nurse
manager that it was revised on 7/29/24. The care plan failed to reflect the January
assessment that listening to music and attending religious activites were very important
to the resident.
Further review of the medical record failed to reveal documentation to indicate a care
plan meeting had occurred since December 2023.
On 9/12/24 at 10:54 AM the resident's responsible party reported being at the facility
frequently. She also confirmed that there have been no recent care plan meetings.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected most or all residents
Based on observation, interview and record review, it was determined that the facility failed to post nursing staffing. This was evident during the staffing investigation portion of the recertificatio...
Read full inspector narrative →
Based on observation, interview and record review, it was determined that the facility failed to post nursing staffing. This was evident during the staffing investigation portion of the recertification survey and had the potential to affect all residents, residents' representatives and visitors. The findings include:
On 9/10/24 at 7:00 AM, the survey team entered the facility. A brief observation revealed a staffing list on the reception desk which contained a list of nursing staff by unit and by shift.
On 9/12/24 at 8:52 AM, an interview with the Staffing Coordinator (Staff #3) was conducted to review the staff posting at the reception desk. Staff #3 provided multiple copies of the daily staffing lists that were posted at the reception desk and explained that they listed nurse staffing for each unit and each shift. She further explained that staff were expected to initial or sign next to their name when they arrived at the facility to work. There were also handwritten names which she explained were orientee staff names written next to the staff who were training them that shift. Staff #3 confirmed that the forms did not contain the resident census nor a total actual hours worked for nursing. She confirmed that the facility did not post a document that had all actual nursing hours worked and resident census.
On 9/12/24 at 9:24 AM, an interview with the Nursing Home Administrator (NHA) was conducted to review the nursing staff posting documents and he confirmed that they did not contain the facility census or the actual nursing hours worked. The NHA said he would ask the staffing coordinator for more information about it. No further information was provided by the end of the survey.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on pertinent document review and interview, it was determined that the facility failed to address identified issues with t...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on pertinent document review and interview, it was determined that the facility failed to address identified issues with the facility MOLST forms to ensure that residents wishes regarding CPR treatments were correctly documented in the residents' medical record. This has the potential to affect all residents in the facility.
The findings are:
A Maryland MOLST, (Medical Orders for Life-Sustaining Treatment) form is used for documenting a resident's specific wishes related to life-sustaining treatments. The MOLST form includes medical orders for Emergency Medical Services (EMS) and other medical personnel regarding cardiopulmonary resuscitation (CPR) and other life-sustaining treatment options for a specific patient. The orders on a MOLST are commonly referred to as code status.
The facility's annual survey conducted on [DATE] through [DATE] identified non-compliance for the failure to have a system in place to properly void MOLST forms and ensure there was only one active MOLST in a Residents electronic health record.
On [DATE] at 10:57 AM, the Facility's Medical Director was interviewed. During the interview, he reported that he was aware of concerns in [DATE] regarding the facility's failure to have a process in place to correctly void residents MOLST orders.
On [DATE] at 11:12?AM, the Medical Director provided documentation (emails) of correspondence with Assistant Attorney General, Counsel for Health Decisions Policy, regarding the proper voiding of MOLST forms. Further review of the emails revealed that the Facility Administrator and Director of Nursing were cced on the correspondence. Continued review revealed the following response from the Assistant Attorney General was sent on [DATE] and included the following. There are various ways to manage voided MOLST forms, but each provider must establish a system that works in their facility. The appropriate staff must be trained in the established system. The system described would not be deficient in and of itself, but if their own staff could not explain the system, a deficiency may result.
[DATE] 01:47 PM, The Facility Administrator (NHA) and the Director of Nursing (DON) were interviewed. They reported that the Administrator and the DON oversee the facilities quality assurance and performance improvement program (QUAPI). The DON and the NHA reported that they were not aware of the MOLST concerns identified by the Medical Director in April and these concerns had not been discussed in QUAPI.
0n [DATE] review of the QUAPI documents provided by the facility revealed that the following concerns were identified by the facility: Pressure ulcer reduction, In house staff communication, re-hospitalization. Continued review failed to reveal that MOLST forms were identified as an issue.
On [DATE], the Facility Administrator (NHA) provided the quality assurance committee meeting with attendance sheets for [DATE] through [DATE], Review of the attendance sheets failed to reveal that the Medical Director attended the meetings in [DATE], [DATE], and [DATE] and failed to attend a meeting after he identified the concerns with the MOLST.
On [DATE] at 3:44 PM, during an interview with the NHA, he confirmed that the Medical Director (Staff # 26) was absent from 3 consecutive monthly QUAPI meetings (equivalent to 1 quarterly meeting) [DATE] through [DATE], and there was no substitute medical director in attendance.
[DATE] 10:50 AM, the above concerns were addressed with Administrator. He reported that the facility was in the process of developing an effective system that accurately recorded the residents' resuscitative wishes on the MOSLT form and would educate the facility staff on this system.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and interviews, it was determined that the facility failed to establish a quality assurance committee th...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and interviews, it was determined that the facility failed to establish a quality assurance committee that included a medical director at every quarterly meeting.
The findings include:
On 9/19/24, the Facility Administrator (NHA) provided the quality assurance committee meeting with attendance sheets [DATE] through August 2024. Review of the attendance sheets failed to reveal that the medical director attended the meetings in May 2024, June 2024, and July 2024.
On 9/19/24 at 3:44 PM during an interview, the NHA confirmed that the Medical Director (Staff # 26) was absent for three monthly consecutive meetings, which is equivalent to one quarterly meeting in the time period of September 2023, through August 2024. In addition, the NHA reported that there was not a substitute medical director that attended the quality assurance committee meetings in May 2024, June 2024 and July 2024.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0941
(Tag F0941)
Could have caused harm · This affected most or all residents
Based on record review and interview, it was determined that the facility failed to ensure that staff had training in interpersonal communication. This was evident for 9 staff (NHA, DON, ADON, SW #11,...
Read full inspector narrative →
Based on record review and interview, it was determined that the facility failed to ensure that staff had training in interpersonal communication. This was evident for 9 staff (NHA, DON, ADON, SW #11, SW #19, Staff #27, Staff #12, Staff #14, LPN #28, and Staff #29) of 10 staff training records reviewed during the extended survey portion of the recertification survey and had the potential to affect all residents.
The findings include:
On 9/19/24 at 10:29 AM, extended survey task triggered due to an Immediate Jeopardy situation related to duplicate but conflicting Medical Orders for Life Sustaining Treatment (MOLST) and resuscitation code status documents in resident records, which was determined on 9/13/24.
In the morning of 9/19/24, The Director of Human Resources was asked to provide the training records for the Nursing Home Administrator (NHA), Director of Nursing (DON), Assistant Director of Nursing (ADON), both Social Workers (SW#11 & SW #19), the Director of Rehabilitation (Staff #27), the Unit Managers (Staff #12, Staff #14), and 2 Licensed Practical Nurse (LPN) nursing supervisors (LPN #28, LPN#29), for a total of 10 staff.
On 9/19/24 at 3:09 PM, a review of the training records revealed that 9 staff (NHA, DON, ADON, SW #11, SW #19, Staff #27, Staff #12, Staff #14, LPN #28, and Staff #29) lacked any evidence of communication training.
On 9/20/24 at 2:07 PM, an interview with the NHA was conducted to review the finding of the lack of communication training for 9 of 10 staff reviewed. He acknowledged the finding.