COPPER RIDGE NURSING AND ASSISTED LIVING CENTER




Inspected within the last 6 months. Data reflects current conditions.
Copper Ridge Nursing and Assisted Living Center has received a Trust Grade of F, indicating significant concerns and poor quality of care. With a state rank of #194 out of 219 facilities in Maryland and a county rank of #9 out of 10, they are in the bottom half of both rankings. However, the facility is showing an improving trend, as the number of issues has decreased from 18 in 2022 to 15 in 2025. Staffing is rated average with a turnover rate of 59%, which is concerning compared to the state average of 40%. The facility has incurred $62,017 in fines, which is higher than 92% of Maryland facilities, pointing to repeated compliance issues. While they have average RN coverage, recent inspector findings revealed serious issues, such as failing to properly assess and treat pressure ulcers, which led to a resident developing a severe stage 4 ulcer. Additionally, they did not conduct required interdisciplinary care plan meetings for several residents, and there were lapses in investigating allegations of abuse and neglect. Overall, while there are some strengths in staffing and a slight improvement in issues, the significant deficiencies and concerns make it essential for families to thoroughly consider their options.
- Trust Score
- F
- In Maryland
- #194/219
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 59% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $62,017 in fines. Higher than 71% of Maryland facilities. Some compliance issues.
- Skilled Nurses ✓ Good
- Each resident gets 46 minutes of Registered Nurse (RN) attention daily — more than average for Maryland. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 63 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Maryland average (3.0)
Significant quality concerns identified by CMS
13pts above Maryland avg (46%)
Frequent staff changes - ask about care continuity
Above median ($33,413)
Moderate penalties - review what triggered them
11 points above Maryland average of 48%
The Ugly 63 deficiencies on record
Jun 2025
15 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on a review of facility investigative materials, resident medical records, and interviews with facility staff, it was determined the facility failed to ensure that a resident remained free of ve...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0605
(Tag F0605)
Could have caused harm · This affected 1 resident
Based on review of the medical record and interview with facility staff, it was determined the facility failed to ensure: 1) a psychotropic medication prescribed as needed (PRN), had an end date that ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0628
(Tag F0628)
Could have caused harm · This affected 1 resident
Based on review of the medical record and interview with facility staff, it was determined the facility failed to provide written notice of the bed hold policy to the resident/resident representative ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of medical records and interview with facility staff, it was determined that the facility failed to ensure that ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on review of medical records and interviews with facility staff, it was determined that the facility failed to follow physician orders for a resident. This was evident for 2 (Residents #6 and #2...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on a review of resident medical records and interviews with facility staff, it was determined that the facility failed to ensure drug records were maintained in a manner that allowed for reconci...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews with facility staff, it was determined that the facility failed to document/respond to recommendations made by consulting pharmacists in a timely manner. ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on clinical record review and staff interview, it was determined that the facility nursing staff failed to ensure medications were administered or withheld according to physician's orders. This ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, resident interview, and staff interview, it was determined that the facility staff failed to en...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation and staff interview, it was determined that the facility staff failed to discard protein drinks past their use by date. This was evident for 2 out of 3 unit-based kitchens observe...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on record review and staff interviews, the facility failed to adequately monitor and track residents receiving antibiotics. This deficiency was evident for 2 (Resident #22 and #166) out of 4 res...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interviews, the facility failed to adequately screen residents for eligibility and document their pneumococcal and influenza (Flu) vaccination status. This def...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on medical record review, staff employee file review, and staff interview, it was determined the facility failed to maintain document related to residents' and staff' COVID-19 vaccination status...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on observation and interviews, it was determined that the facility failed to ensure that all residents were adequately equipped with the ability to call for assistance, if needed, through a comm...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Based on a review of resident medical records and interviews with facility staff, it was determined that the facility failed to conduct care plan meetings of the interdisciplinary team for residents a...
Read full inspector narrative →
Nov 2022
18 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on complaint allegations, medical record review, and interviews of staff, it was determined that the facility failed to, 1...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on complaint, reviews of a closed medical record and staff interview, it was determined that the facility staff failed to ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) On 11/16/22 at 11:09 AM a review of facility-reported incident MD00182508 revealed that on 3/19/22 Resident #17 was following...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review it was determined the facility failed to report allegations of abuse and injuries of an unknown source within 2 hours of the allegation to the regulatory agency an...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility failed to ensure a resident's discharge was documented in the medical record to include the resident's status at...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined that the facility failed to notify the resident/resident r...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview it was determined the facility staff failed to 1) conduct an accurate, compre...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, and staff interview, it was determined the facility staff failed to ensure the Minimum Data Set ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on a medical record review, and staff interview, it was determined that the facility staff failed to 1) develop and implem...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility staff failed to revise and update a comprehensive care plan for monitoring a resident with inappropriate sexual ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview it was determined that the facility staff failed to monitor blood sugar level...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined that the facility failed to 1) ensure a resident admitted ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on complaint, reviews of a closed record, and staff interview, it was determined that the facility staff failed to obtain ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0710
(Tag F0710)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interviews it was determined that the resident's attending physician and Certified Registered...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on complaints, review of a closed medical record, and staff interview, it was determined the facility failed to timely pro...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) On 11/14/22 at 2:00 PM a review of complaint #MD00178305 revealed that on 1/14/22 Resident #4 was transferred to [XX hospital...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
Based on interview, review of facility reported incident investigations and policy, it was determined the facility failed to thoroughly investigate allegations of abuse, neglect, misappropriation of r...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview it was determined the physician and nurse practitioner's progress notes were ...
Read full inspector narrative →
Sept 2021
22 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
Based on observation rounds, it was determined the facility failed to maintain dignity for a resident when a staff member wrote the date and time on a pain patch after applying it. This was evident fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined that the facility staff failed to ensure that residents were able to exercise their right of self-determination, as evidenced by denying a resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
2) On 9/14/21 at 9:21 AM, Resident #262 reported an allegation of abuse to a surveyor. Resident #262 reported that, during the evening of his/her admission, he/she had gotten out of bed and on the way...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
4) A baseline care plan is a set of instructions for facility staff to provide care that is effective and resident-centered until a comprehensive care plan can be developed and implemented. The baseli...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
3) On 9/21/21, a record review was conducted for resident # 28. There was a care plan meeting held on 5/29/21 with the sisters of Resident # 28. There was no care Plan meeting for Aug. 2021 due to lac...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and observation of resident # 35, it was determined that facility failed to turn and reposition a resident wh...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on complaint, a facility reported investigation, and interview with the ombudsman and facility staff, it was determined that 1) RN staff #11 failed to replace an empty oxygen tank for resident #...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
Based on observation and interview with GNA, facility failed to have sufficient staff on the Eastern Shore unit on 9/13/21 7-3 shift. This was evident for 34 out of 34 residents.
Findings include:
Th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on reviews of administrative records and staff interview, it was determined that the nursing administrative staff failed to 1) conduct a yearly performance review on 2 (#40, # 43) out of 5 geria...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0741
(Tag F0741)
Could have caused harm · This affected 1 resident
Based on reviews of administrative records and staff interview, it was determined that the nursing administrative staff failed to ensure that 5 ( GNAs #22, 40, 41, 42, 43) out of 5 geriatric nursing a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, and facility documentation review, it was determined the facility failed to discard medications after the expiration date. This was evident for 1 of 2 nursing un...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
2) During a a dining observation on 9/13/21 at 9:45 AM, of Resident #261 being served his/her breakfast tray, it was revealed that Resident #261's preferences had not been provided as evidenced by the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected 1 resident
Based on complaint, observation, and staff interview, it was determined that the facility staff failed to provide a resident with a meal within the required time frame. This was evident for 2 (Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
4) On 9/21/21 at 10:56 AM, a review of Resident #263's medical records revealed on the Treatment Administration Record (TAR) for 5/2021, an order initiated on 5/3/21, that read, Sacrum: cleanse with w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, it was determined that the facility staff had failed to conduct quality assurance meetings...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, it had been determined that the facility failed to have a process in place to prevent the spread of infection by ensuring 1) that residents had been offered...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected 1 resident
Based on the review of employee records and staff interview, it was determined that the facility failed to have documentation that Geriatric Nursing Assistance's (GNA) were given 1) in-service trainin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected multiple residents
Based on reviews of the facility's investigation, the facility reported incident, and staff interview, it was determined that the facility failed to protect a resident from abuse. This was evident for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
A medical record review for Resident #263 on 9/15/21 at 10:21 AM, revealed that Resident #263 had the following care plans initiated on 3/16/21 for pain: The resident has potential for acute and chron...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected multiple residents
Based on observations, review of daily staffing records, and staff interview, it was determined the facility failed to post the total number and actual hours worked by categories of Registered nurses,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected multiple residents
Based on review of facility records and an interview with staff, it was determined the facility failed to revise and document an accurate up-to-date facility-wide assessment. This was evident during r...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation and staff interview, it had been determined that the facility had not implemented infection control practices to prevent the spread of COVID 19 as evidenced by facility staff to w...
Read full inspector narrative →
Sept 2018
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined that the facility failed to have a system in place to 1) ensure that required documentation regarding a resident's transfer and appeal ri...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
2) A review of the resident's medical record on 9/14/18 at 10:09 AM revealed a diagnosis including osteoarthritis, dementia with behavioral disturbances, Alzheimer's disease and a patient of hospice. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined the facility staff failed to prevent the development of a pressure ulcer for a functionally and cognitively impaired resident (Res...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0772
(Tag F0772)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with facility staff, it was determined that the facility failed to complete a physician ordered lab on a Resident (#21) This was evident in 1 of 5 resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0775
(Tag F0775)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined that the facility failed to ensure laboratory test results were kept in the resident's medical record for review by medical pr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview with staff it was determined that the facility failed to ensure documentation of ce...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on record review and staff interview it was determined that the facility failed to put a system in place to ensure proper infection surveillance policies and procedures are in place by not imple...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on record and staff interview it was determined that the facility failed to put a system in place to ensure that there is documentation in the resident's medical record of the information/educat...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 1 harm violation(s), $62,017 in fines. Review inspection reports carefully.
- • 63 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $62,017 in fines. Extremely high, among the most fined facilities in Maryland. Major compliance failures.
- • Grade F (5/100). Below average facility with significant concerns.
About This Facility
What is Copper Ridge Nursing And Assisted Living Center's CMS Rating?
CMS assigns COPPER RIDGE NURSING AND ASSISTED LIVING CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Copper Ridge Nursing And Assisted Living Center Staffed?
CMS rates COPPER RIDGE NURSING AND ASSISTED LIVING CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 59%, which is 13 percentage points above the Maryland average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 79%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Copper Ridge Nursing And Assisted Living Center?
State health inspectors documented 63 deficiencies at COPPER RIDGE NURSING AND ASSISTED LIVING CENTER during 2018 to 2025. These included: 1 that caused actual resident harm and 62 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Copper Ridge Nursing And Assisted Living Center?
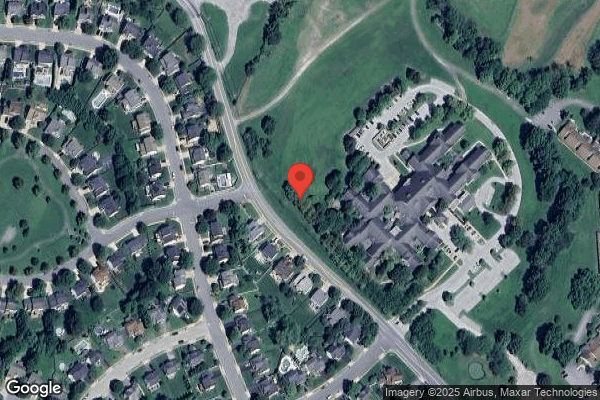
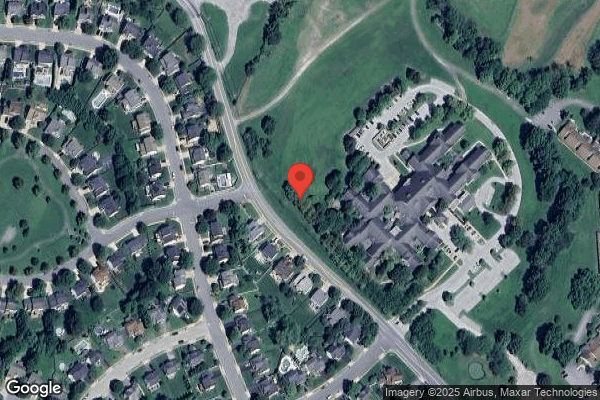
COPPER RIDGE NURSING AND ASSISTED LIVING CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 66 certified beds and approximately 65 residents (about 98% occupancy), it is a smaller facility located in SYKESVILLE, Maryland.
How Does Copper Ridge Nursing And Assisted Living Center Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, COPPER RIDGE NURSING AND ASSISTED LIVING CENTER's overall rating (1 stars) is below the state average of 3.0, staff turnover (59%) is significantly higher than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Copper Ridge Nursing And Assisted Living Center?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the substantiated abuse finding on record and the facility's high staff turnover rate.
Is Copper Ridge Nursing And Assisted Living Center Safe?
Based on CMS inspection data, COPPER RIDGE NURSING AND ASSISTED LIVING CENTER has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Maryland. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Copper Ridge Nursing And Assisted Living Center Stick Around?
Staff turnover at COPPER RIDGE NURSING AND ASSISTED LIVING CENTER is high. At 59%, the facility is 13 percentage points above the Maryland average of 46%. Registered Nurse turnover is particularly concerning at 79%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Copper Ridge Nursing And Assisted Living Center Ever Fined?
COPPER RIDGE NURSING AND ASSISTED LIVING CENTER has been fined $62,017 across 1 penalty action. This is above the Maryland average of $33,699. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Copper Ridge Nursing And Assisted Living Center on Any Federal Watch List?
COPPER RIDGE NURSING AND ASSISTED LIVING CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.