ORCHARD HILL REHABILITATION AND HEALTHCARE CENTER



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Orchard Hill Rehabilitation and Healthcare Center has a Trust Grade of F, indicating significant concerns regarding the quality of care provided. It ranks #168 out of 219 facilities in Maryland, placing it in the bottom half, and #33 out of 43 in Baltimore County, meaning there are only a few worse options locally. The facility is worsening, with issues increasing from 14 in 2024 to 19 in 2025. Staffing is a concern, with a turnover rate of 58%, which is significantly higher than the state average of 40%, indicating instability among caregivers. The facility has faced $75,840 in fines, which is higher than 87% of Maryland facilities, suggesting ongoing compliance problems. While they have slightly above-average quality measures, specific incidents raise serious concerns. For example, one resident suffered a pelvic fracture and hematoma after rolling out of bed due to insufficient staff assistance, and another experienced bilateral femur fractures under similar circumstances. Additionally, there were issues with food safety practices, such as improperly maintained food service equipment and expired food items, which could affect all residents. Overall, families should weigh these significant weaknesses against the facility's limited strengths.
- Trust Score
- F
- In Maryland
- #168/219
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 58% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $75,840 in fines. Lower than most Maryland facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 39 minutes of Registered Nurse (RN) attention daily — about average for Maryland. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 92 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Maryland average (3.0)
Below average - review inspection findings carefully
12pts above Maryland avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
10 points above Maryland average of 48%
The Ugly 92 deficiencies on record
Mar 2025
19 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews with facility staff, it was determined that the facility failed to provide residents with ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review and interview with facility staff, it was determined that the facility staff failed to notify a provider and/or resident representative of a significant weight loss for a reside...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, resident interview, and staff interview it was determined that the facility staff failed to ensure showers maintained proper temperatures. This was evident for 1 out of 4 nursing...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0637
(Tag F0637)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews with facility staff, it was determined that the facility failed to complete a significant ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interview with residents, review of medical records and interview with facility staff, it was determined that the facility failed to hold care plan meetings of the interdisciplinary team for ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and medical record review it was determined the facility failed to ensure medical orders were followed for the provision of thickened liquids. This was evident for 1 (...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on medical record review and staff and resident interviews, it was determined that the facility failed to monitor/access residents related to potentially leading to smoking accidents. This was e...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of medical records and interview with facility staff, it was determined that the facility failed to monitor and ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews with residents and staff, it was determined that the facility staff failed to obtain/monitor pre and post-dialysis body weights. This is evident for 1 (Re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected 1 resident
Based on observation it was determined that the facility staff failed to post staffing information in an easily accessible location. This was evident for 4 out of the 7 days of the recertification/com...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and staff interview it was determined that the facility staff failed to ensure medications are kept in a se...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0790
(Tag F0790)
Could have caused harm · This affected 1 resident
Based on observation, review of medical records, and interviews with residents and staff, it was determined that the facility failed to ensure that residents received necessary and/or recommended dent...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0840
(Tag F0840)
Could have caused harm · This affected 1 resident
Based on review of medical records and interview with facility staff, it was determined that the facility failed to 1) ensure contracted services for wound care were timely documented in the medical r...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on review of the facility records and interview with facility staff, it was determined that the facility failed to monitor and track antibiotic usage. This was evident by 1) the delayed start of...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on a review of the resident medical records and interview with facility staff, it was determined that the facility failed to ensure that drug records were maintained in a manner that allowed for...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected multiple residents
Based on observation and interview, it was determined the facility failed to ensure the kitchen steam table was maintained in safe operating condition. This was evident for one out of one steam tables...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview it was determined the facility failed to: 1) ensure food items were labeled, 2) ensure food items were discarded appropriately, 3) ensure the freezer was maintained ...
Read full inspector narrative →
Oct 2024
14 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of facility reported incidents, medical record review, facility documentation review, and staff interviews, it w...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, the facility staff failed to notify the resident's physician and/or resident's rep...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of a facility reported incident, medical record review, and staff interview, it was determined the facility fail...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on reviews of facility reported incidents with documentation and interview, it was determined the facility failed to report allegations of abuse within 2 hours of the allegation to the regulator...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. The facility failed to ensure a thorough investigation was conducted when mistreatment was alleged by Resident #43.
Resident...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined the facility staff failed to ensure Minimum Data Set (MDS) assessments were accurately coded. This was evident for 2 (#59, #24) of...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on review of a facility reported incident, record review, and staff interview it was determined that facility staff failed to update care plans when there were changes in resident needs and fail...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, the facility staff failed to provide treatment/services to prevent/heal pressures ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, the facility staff failed to provide respiratory care treatment for residents (Res...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, the facility failed to ensure a resident's drug regimen was free from an unnecessa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0840
(Tag F0840)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation and interview, the facility staff failed to obtain outside services for residents in...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on administrative and medical record reviews and interview, it was determined the facility failed to maintain complete and...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and resident and staff interview, it was determined that the facility staff failed to maintain the resident...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. The facility failed to ensure accurate skin assessments were completed for Resident #56.
Resident #56 was admitted to the fac...
Read full inspector narrative →
Jun 2021
32 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, and interview, it was determined the facility staff failed to provide an environmen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined the facility staff failed to notify Resident #69's Responsible Party (RP) when a medication was discontinued. This was evident for 1 of 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, staff interview, and review of administrative records, it was determined that the facility faile...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation on 6/25/21 at 11:49 AM, the facility staff failed to replace ripped and torn screens in rooms 209, 211, 213, and 215. This was evident for 4 out of 15 rooms observed for ripped sc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on medical record review it was determined the facility staff failed to notify the Office of Health Care Quality (OHCQ) of an injury of unknown origin to Resident #69. This was evident for 1 of ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined that the facility failed to document that information was provided to the acute care facility when a resident was transferred there...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview with staff it was determined that the facility failed to ensure that the resident, ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0624
(Tag F0624)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility failed to orient, prepare, and document a resident's preparation for a transfer to the hospital. This was exempl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview it was determined that the facility staff failed to accurately code the resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview it was determined that facility staff failed to develop and implement comprehensive c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on medical record review and observation, it was determined the facility staff failed to provide nursing care within the standards of practice for Residents #84 and #210. This was evident for 2 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
Based on review of a closed medical record and staff interview, it was determined that the facility staff failed to provide a resident with a completed discharge summary (Resident #112). This was evid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation and interview it was determined the facility staff failed to provide thorough groomi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview, the facility staff failed to provide treatment/services to prevent/heal pressures ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, medical record review and interview with a resident, it was determined that the facility failed to provide safety equipment for a resident that smokes. This was identified for Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined the facility staff failed to thoroughly assess and intervene when Resident #53 was noted with a decrease in urinary continence. This was ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** The surveyor reviewed Resident #470's medical record on 6/28/21 at 12:55 PM. The review revealed that Resident #470 was admitted...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
Based on interview and medical record review, it was determined the facility failed to maintain enough nursing staff to meet resident care needs in a timely manner for residents. This deficient practi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on medical record review, it was determined the facility staff failed to ensure that Resident #80 was free from unnecessary medications. This was evident for 1 of 5 residents selected for review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on record review and observation of medication administration, it was determined the facility staff failed to maintain an error rate below 5%. Observation of medication administration resulted i...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based upon observation, staff interview and medical record review it was determined that facility staff failed to assist a resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview it was determined that the facility staff failed to promote self determination for ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0570
(Tag F0570)
Could have caused harm · This affected multiple residents
Based on facility documentation and interview, the facility staff failed to provide evidence that the facility had purchased a surety bond to assure the security of all the residents' personal funds d...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
Based on record review and staff interview it was determined that the facility failed staff to provide residents and/or their representative (RP) with the proper paper documentation of the facilities ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview it was determined the facility staff failed to ensure the care plan meeting occurre...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of resident medical records and interviews with residents and facility staff, it was determined that the facilit...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. The facility staff failed to provide Resident #261 with a therapeutic diet.
During interview with the Resident on 6/16/21 at ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5. Review of Resident #82's medical record on 6/21/21 revealed the resident was admitted to the facility on [DATE] with diagnosi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Interview with the Nursing Home Administrator, Director of Nursing and Corporate Nurse on 6/30/21 at 2:00 PM were notified of th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, review of employee health records and interview; the facility staff failed to: 1.) thoroughly screen for i...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations of the facility's kitchen food services, and staff interview it was determined that the facility failed to maintain food service equipment in a manner that ensures sanitary food ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on observations, review of daily staffing records, and staff interview it was determined the facility failed to post the total number and actual hours worked by categories of registered nurses, ...
Read full inspector narrative →
Sept 2018
27 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 09/19/18 at 07:19 AM during room observations surveyor observed Unit Manager (UM) walked into room [ROOM NUMBER] without k...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on interviews and review of medical records it was determined that the facility staff failed to provide showers to the resident as per preference and request. This was found to be evident for 1 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected 1 resident
Based on interviews with residents and facility staff it was determined the facility failed to give adequate responses to grievances that were presented by the resident council. This was found to be e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0568
(Tag F0568)
Could have caused harm · This affected 1 resident
Based on interview and review of personal funds account statements it was determined that the facility failed to ensure quarterly statements were provided to residents or the resident's responsible pa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0577
(Tag F0577)
Could have caused harm · This affected 1 resident
Based on interview and observation, it was determined that the facility failed to have the facility survey results in a location accessible to residents and in a location that is frequented by residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with facility staff, it was determined that the facility was unable to provide documentation that a notification of medication non-coverage (NOMNC) was pro...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interviews it was determined that the facility failed to have an effective system in place to ensure ma...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on interviews with residents and staff it was determined the facility failed to have a system in place that allows residents to report grievances without fear of reprisal. This was found to be e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on a review of facility reported incident and investigation it was determined that the facility failed to protect a resident from verbal abuse. This was found to be evident for 1 out of 4 reside...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on review of the medical record, facility investigation documentation and interviews it was determined that the facility failed to ensure complete and thorough investigations of abuse allegation...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
5. On 09/21/18 Resident # 114's medical records were reviewed. This review revealed a health status note written on 8/9/2018 at 12:15 PM that the resident had a change in condition, the physician was ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
5. On 09/21/18 Resident # 114's medical records were reviewed. This review revealed a health status note written on 8/9/2018 at 12:15 PM revealed that the resident had a change in condition, the physi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Assessments
(Tag F0636)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. On 09/26/28 at 3:09 PM a review of Resident #83's medical record was conducted. The resident was admitted to the facility in ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with the facility staff it was determined that the facility failed to ensure Quarterly Minimum Data Set (MDS) assessments accurately reflected the resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on review of the medical record and interview it was determined that the facility failed to have a system in place to provide a summary of the interim plan of care to the resident or responsible...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
2. Review on 9/24/18 at 11:36 AM of the medical record for Resident #58 revealed diagnosis including schizophrenia and bipolar disorder in addition to neuro-pathic pain which Neurontin was ordered as ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
Based on medical records review and interview with staff it was determined that the facility failed to provide treatment and follow-up care for a resident regarding visual impairments. This was eviden...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0712
(Tag F0712)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined that the facility failed to ensure the primary care physician saw the residents at least once every 60 days. This was found to be evident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected 1 resident
Based on interviews with residents and staff and a review of pertinent documentation, it was determined the facility failed to have sufficient staff to provide services in the main dining room allowin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on review of employee files and interview with staff it was determined that the facility failed to have evidence of skills assessment for geriatric nursing assistants(GNAs) hired within the past...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations it was determined the facility failed to date medications upon opening them and remove expired medications. This was found to be evident for 3 out of 3 medication carts reviewed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined that the facility failed to ensure an order for a dental consult was followed. This was found to be evident for 1 out of the 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
Based on observation and interview it was determined that the facility failed to ensure foods listed as allergies were not served to residents as evidenced by the service of eggs to a resident with do...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. A review of the facility's Infection Prevention Control Program (IPCP) was conducted with the Quality Assurance /IPCP Nurses ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on record review and staff interview it was determined that the facility failed to put a system in place for monitor, identify, investigate, actual and potential communicable diseases and infect...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
2. On 9/24/18 Resident #62's care plans were reviewed. This review revealed a care plan for psychotropic medications. This care plan was created on 3/28/18 with multiple revisions on 6/4/18, 9/4/18 an...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
3. During a tour of unit 3 on 9/22/18, this surveyor observed Resident #22 sitting in a chair rocking back and forth, the television was turned off. Further observation of the resident on 9/23/18 the ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 1 harm violation(s), $75,840 in fines. Review inspection reports carefully.
- • 92 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $75,840 in fines. Extremely high, among the most fined facilities in Maryland. Major compliance failures.
- • Grade F (15/100). Below average facility with significant concerns.
About This Facility
What is Orchard Hill Rehabilitation And Healthcare Center's CMS Rating?
CMS assigns ORCHARD HILL REHABILITATION AND HEALTHCARE CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Orchard Hill Rehabilitation And Healthcare Center Staffed?
CMS rates ORCHARD HILL REHABILITATION AND HEALTHCARE CENTER's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 58%, which is 12 percentage points above the Maryland average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at Orchard Hill Rehabilitation And Healthcare Center?
State health inspectors documented 92 deficiencies at ORCHARD HILL REHABILITATION AND HEALTHCARE CENTER during 2018 to 2025. These included: 1 that caused actual resident harm, 90 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Orchard Hill Rehabilitation And Healthcare Center?
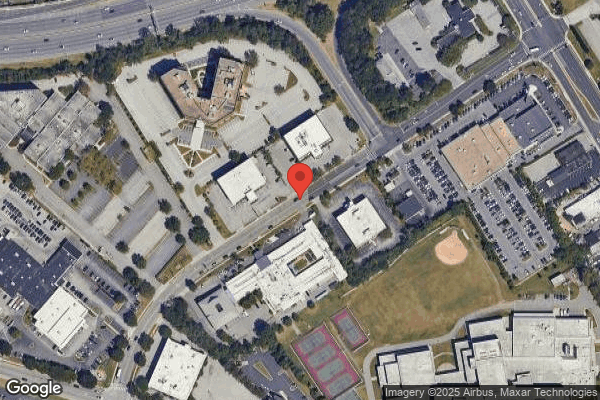
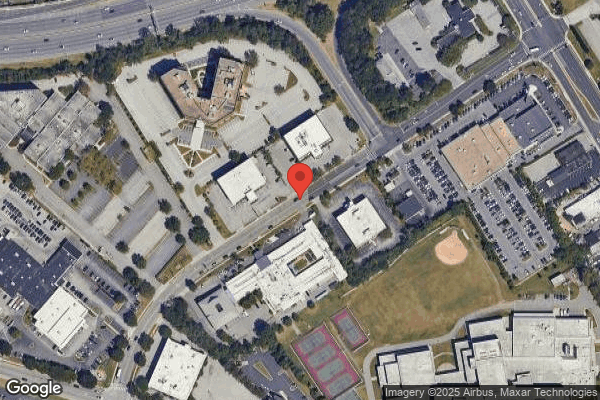
ORCHARD HILL REHABILITATION AND HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by MARQUIS HEALTH SERVICES, a chain that manages multiple nursing homes. With 139 certified beds and approximately 117 residents (about 84% occupancy), it is a mid-sized facility located in TOWSON, Maryland.
How Does Orchard Hill Rehabilitation And Healthcare Center Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, ORCHARD HILL REHABILITATION AND HEALTHCARE CENTER's overall rating (2 stars) is below the state average of 3.0, staff turnover (58%) is significantly higher than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Orchard Hill Rehabilitation And Healthcare Center?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the substantiated abuse finding on record, the facility's high staff turnover rate, and the below-average staffing rating.
Is Orchard Hill Rehabilitation And Healthcare Center Safe?
Based on CMS inspection data, ORCHARD HILL REHABILITATION AND HEALTHCARE CENTER has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Maryland. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Orchard Hill Rehabilitation And Healthcare Center Stick Around?
Staff turnover at ORCHARD HILL REHABILITATION AND HEALTHCARE CENTER is high. At 58%, the facility is 12 percentage points above the Maryland average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Orchard Hill Rehabilitation And Healthcare Center Ever Fined?
ORCHARD HILL REHABILITATION AND HEALTHCARE CENTER has been fined $75,840 across 1 penalty action. This is above the Maryland average of $33,837. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Orchard Hill Rehabilitation And Healthcare Center on Any Federal Watch List?
ORCHARD HILL REHABILITATION AND HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.