ATLEE HILL HEALTH AND REHAB CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Atlee Hill Health and Rehab Center has received a Trust Grade of F, indicating significant concerns about the facility and its care. It ranks #181 out of 219 nursing homes in Maryland, placing it in the bottom half, and #8 out of 10 in Carroll County, meaning there are only two local options considered better. While the facility has shown improvement in issues, decreasing from 21 in 2023 to 10 in 2025, there are still serious concerns, including a resident receiving the wrong medication, which led to hospitalization. On the positive side, staffing is a strength with a 4 out of 5-star rating, although the turnover rate is 45%, which is average. However, the facility has incurred fines totaling $14,888, higher than 76% of Maryland facilities, suggesting ongoing compliance issues, and the RN coverage is only average, which may limit oversight of resident care.
- Trust Score
- F
- In Maryland
- #181/219
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 45% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $14,888 in fines. Higher than 66% of Maryland facilities. Some compliance issues.
- Skilled Nurses ✓ Good
- Each resident gets 42 minutes of Registered Nurse (RN) attention daily — more than average for Maryland. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 80 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, fire safety.
The Bad
Below Maryland average (3.0)
Significant quality concerns identified by CMS
Near Maryland avg (46%)
Higher turnover may affect care consistency
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 80 deficiencies on record
Aug 2025
10 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review and staff interviews, it was determined that the facility failed to notify an attending physician when there were documented changes in a Resident's condition. This was evident ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0628
(Tag F0628)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, it was determined that the facility failed to 1) ensure appropriate information was commu...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, it was determined that the facility failed to provide residents/representatives with a co...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, it was determined that the facility failed to ensure that a resident who required assista...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interviews, it was determined that the facility failed to ensure that care was provided in ac...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record review and staff interviews, it was determined that the facility failed to ensure a resident received their medication according to the attending physician's order. This was evident fo...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
Based on record review, observations, and interviews, it was determined that the facility failed to ensure that residents were served meals according to a predetermined menu that incorporated their pr...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, it was determined that the facility failed to report allegations of abuse in a timely man...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
Based on medical record review and interviews, it was determined that the facility failed to develop comprehensive person-centered care plans for residents. This was found to be evident for 3 ( #48, #...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected most or all residents
Based on review of the facility's abuse policy and interview it was determine that the facility failed to ensure the abuse policy addressed all the required components. This was found to be evident fo...
Read full inspector narrative →
Dec 2023
21 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0760
(Tag F0760)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, it was determined that the facility failed to ensure residents did not receive medicatio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with staff it was determined the facility staff failed to inform and provide written information to all residents concerning the right to formulate at the ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on medical record review related to a complaint and interviews with the facility staff and family, it was determined that the facility failed to report an unobserved fall with injury to the Offi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3) On 12/18/2023 at 11:00AM, a review of Resident #29's electronic medical record revealed that the resident was transferred to ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) A Bed Hold is the act of holding or reserving a resident's bed while the resident is absent from the facility for therapeutic...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
On 12/12/2023 at 12:21 PM, during a review of Resident #29's record, the Surveyor discovered a Post Fall Evaluation note dated 5/8/2022 at 1:46PM which stated that the resident had an unwitnessed fall...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and staff interview it was determined the facility staff failed to ensure the resident's env...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, review of the medical record and interview with staff it was determined the facility staff failed to provi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on medical record review and interview with facility staff and resident representatives, it was determined that the facility failed to have a process in place to implement and determine the comp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on review of the facility's Controlled Drug Count Verification sheets and interview with staff it was determined that the facility failed to ensure that an account of all controlled drugs were c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview with staff, it was determined that the facility failed to 1) have a system in place to ensu...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review it was determined the facility failed to ensure adequate indication for use, identify resident sp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on medical record review, interview and observations completed during medication pass, the calculated medication error rate during the annual survey for medication pass was determined to be 7.4%...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations and staff interviews it was determined that the facility failed to maintain a safe and effective system fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, it was determined that the facility failed to ensure that Geriatric Nursing Assistants (...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview with staff it was determined the facility staff failed to develop and implement a b...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview with staff it was determined the facility staff failed to develop plans of care tha...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** According to the Centers of Disease Control and Prevention Transmission-Based Precautions are the second tier of basic infection...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview with staff, it was determined that the facility failed to store food and equipment in a manner that maintains professional standards of food service safety. This pra...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation and interviews with staff, it was determined that the facility failed to properly contain and cover waste in dumpsters. This was evident for 2 of 3 dumpsters in the outdoor garbag...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0577
(Tag F0577)
Minor procedural issue · This affected most or all residents
Based on surveyor observation and interview it was determined the facility failed to post the results of the most recent surveys in a place readily accessible to residents, families, and visitors. Thi...
Read full inspector narrative →
Apr 2019
27 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, it was determined that the facility staff failed to treat each resident in a dignified manner by failing to knock on a resident's door to request permission before entering. This...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
2) Record review for Resident #37 between 4/15/19 and 4/19/19, revealed a skin tear to left hip sustained on 1/23/19. The left hip wound was classified as a full thickness wound, per the Assistant Dir...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observations, medical record review and staff interview, it was determined the facility failed to implement an ongoing resident centered activities program designed to meet the interests and ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation and interview with facility staff, it was determined that the facility failed to ensure that a resident receiving oxygen therapy had orders that did not conflict and that were bei...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, the facility staff failed to document a review of the care, the resident's current condition, progress and problems in maintaining or improving thei...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on review of the medical record and interview with facility staff, it was determined the facility staff failed to ensure irregularities reported to the attending physician by the pharmacist were...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on medical record review, It was determined that the facility failed to ensure that a resident's medication regimen was free from an unnecessary psychotropic medication by 1) failing to ensure t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on medication administration observation, medical record review and staff interview, it was determined the facility staff failed to ensure a medication error rate of less than 5 percent for 2 (#...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on surveyor observation and interview with facility staff, it was determined that the facility staff 1) failed to ensure that inhalation medication and prescribed topical creams were secured in ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
Based on observation, resident and staff interviews, and medical record review, it was determined that the facility failed to provide dental services within a reasonable time frame following a complai...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
Based on observation, it was determined that the facility failed to ensure that food was stored in a sanitary way. This was evident for 1 of 2 kitchen observations performed during the survey.
The fi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on record review and staff interview, the facility failed to 1) document in the medical record that the Flu and Pneumonia vaccine was offered and administered to 1 (resident #36) of 5 residents ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
Based on observation, medical record review and staff interview, it was determined that the facility staff failed to ensure that Minimum Data Set (MDS) assessments were accurately coded. This was evid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and resident and staff interview, it was determined that the facility 1) failed to develop a base...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and resident/staff interview, it was determined that the facility failed to develop and implement...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
4) Review of the medical record for Resident #37 between 4/15/19 and 4/19/19, failed to reveal that the weekly skin assessments were completed by the nursing staff. The last documented assessment was ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on review of Geriatric Nursing Assistant (GNA) personnel files and staff interview, it was determined the facility failed to conduct yearly performance reviews and review with the GNAs at least ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected multiple residents
Based on observations, medical record review and staff interview, it was determined that the facility failed to assess a resident's blood pressure as prescribed prior to the administration of an oral ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on medical record review and staff interview, it was determined the facility failed to have complete and accurate medical records. This was evident for 1 (#37) of 32 residents reviewed during th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, record review, staff and resident interview, it was determined that the facility staff failed to follow infection control practices and guidelines to prevent the development and ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected most or all residents
6) Observation of Resident #12 on 4/15/19 at 8:45 AM, revealed several teeth that were broken off on the front, bottom gum line.
Review of Resident #12's care plans on 4/16/19 at 9:30 AM, failed to re...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on surveyor observation, interviews with staff and review of resident and facility records, it was determined that the facility failed to have an effective quality assessment and assurance progr...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0582
(Tag F0582)
Minor procedural issue · This affected multiple residents
Based on medical record review and staff interview, it was determined that the facility failed to provide residents or resident representatives with the Skilled Nursing Facility (SNF) Advanced Benefic...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Transfer Notice
(Tag F0623)
Minor procedural issue · This affected multiple residents
2) On 4/18/19 at 10:27 AM, review of Resident #38's medical record revealed documentation that Resident #38 was sent to an acute care facility on 3/1/19. On 3/1/19 at 12:00 PM, in a progress note, the...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0624
(Tag F0624)
Minor procedural issue · This affected multiple residents
Based on medical record review and staff interview it was determined the facility failed to document what preparation and orientation was given to a resident to ensure an orderly transfer to an acute ...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0625
(Tag F0625)
Minor procedural issue · This affected multiple residents
Based on medical record review and staff interview it was determined the facility failed to notify the resident/resident representative in writing of the bed-hold policy upon transfer of a resident to...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected multiple residents
Based on observations and staff interview, it was determined that the facility failed to maintain the daily past nurse staffing data for a minimum of 18 months.
The findings include:
Observations of ...
Read full inspector narrative →
Nov 2017
22 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0272
(Tag F0272)
Could have caused harm · This affected 1 resident
Based on review of medical record documentation, observation and staff interview, it was determined that facility staff failed to ensure that Minimum Data Set (MDS) assessments were accurately coded. ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0278
(Tag F0278)
Could have caused harm · This affected 1 resident
2) On 11/15/17 at 9:00 AM, a review of Resident #75's medical record revealed that, on 9/11/17, the Nurse Practitioner (NP) documented in a progress note that Resident #75 had diagnoses that included,...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0387
(Tag F0387)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility failed to develop and implement an effective system to ensure residents are seen by a physician for a required f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0428
(Tag F0428)
Could have caused harm · This affected 1 resident
2) The pharmacist failed to identify and report medication irregularities related to a resident's use of an antipsychotic medication.
Resident #75's medical record was reviewed on 11/15/17 at 9:00 AM....
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0441
(Tag F0441)
Could have caused harm · This affected 1 resident
Based on observation, it was determined that facility staff failed to follow standard hand hygiene practices to prevent the spread of infections and prevent cross-contamination. This was evident for 1...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0502
(Tag F0502)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined that the facility staff failed to provide laboratory services to meet the need of its residents. This was evident for 1 (#75) of 5...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0155
(Tag F0155)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined the facility staff failed to follow a resident's MOLST for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0157
(Tag F0157)
Could have caused harm · This affected multiple residents
2) Failed to notify a resident when there was a change in a resident's treatment related to medication.
a) On 11/14/17 at 1:03 PM a review of Resident #77's medical record was conducted. Review Resid...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0241
(Tag F0241)
Could have caused harm · This affected multiple residents
Based on observation, it was determined the facility failed to treat residents in a dignified manner as evidenced by 1) failing to serve all residents at the same table at the same time during a dinin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0248
(Tag F0248)
Could have caused harm · This affected multiple residents
2) On 11/13/17 at 10:11 AM, during an interview, when asked Do you participate in the activity programs here?, Resident #77 stated that he/she was never asked to attend an activity. The resident state...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0253
(Tag F0253)
Could have caused harm · This affected multiple residents
Based on surveyor observation, it was determined that the facility staff failed to provide services necessary to maintain a sanitary, orderly and comfortable interior by failing to maintain 1) a soap ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0279
(Tag F0279)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5) On 11/14/17 a review of Resident #77's medical record revealed Resident #77 was admitted to facility in late September, 2017....
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0280
(Tag F0280)
Could have caused harm · This affected multiple residents
4) On 11/15/17, a review of Resident #75's medical record was conducted. Review of Resident #75's care plans included, but was not limited to, a care plan that stated Resident #75 is on diuretic (medi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0282
(Tag F0282)
Could have caused harm · This affected multiple residents
4) A review of Resident #70's record, on 11/15/17 at 7:55 AM, revealed an activity care plan. The care plan goal was Resident will attend at least 2 activities weekly. The interventions, which were in...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0309
(Tag F0309)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4) On 11/13/17, at 10:12 AM, Resident #77 was observed lying in bed. During an interview, when asked Do you get out of bed? Resi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0329
(Tag F0329)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined that the facility failed to ensure that a residents' medic...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0371
(Tag F0371)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor observation and interview with staff, it was determined that the facility staff failed to properly label and d...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0386
(Tag F0386)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview, it was determined that the physician/nurse practitioner failed to write a pr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0431
(Tag F0431)
Could have caused harm · This affected multiple residents
Based on observation and staff interview, it was determined the facility failed to properly store medications as evidenced by failing to lock a medication cart when unattended. This was evident on 1 o...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0514
(Tag F0514)
Could have caused harm · This affected multiple residents
8) On 11/13/17, at 10:12 AM, Resident #77 was observed lying in bed. During an interview, when asked Do you get out of bed? Resident #77 stated no, except when my husband or sister come and we go out ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0167
(Tag F0167)
Minor procedural issue · This affected most or all residents
Based on surveyor observation and interview with facility staff, it was determined that the facility failed to post the results of the most recent standard survey and approved plan of correction in a ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0247
(Tag F0247)
Minor procedural issue · This affected most or all residents
Based on interview with the resident and facility staff and review of the medical record, it was determined that the facility failed to ensure that each resident is treated with respect and dignity by...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • 80 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $14,888 in fines. Above average for Maryland. Some compliance problems on record.
- • Grade F (33/100). Below average facility with significant concerns.
About This Facility
What is Atlee Hill Health And Rehab Center's CMS Rating?
CMS assigns ATLEE HILL HEALTH AND REHAB CENTER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Atlee Hill Health And Rehab Center Staffed?
CMS rates ATLEE HILL HEALTH AND REHAB CENTER's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 45%, compared to the Maryland average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Atlee Hill Health And Rehab Center?
State health inspectors documented 80 deficiencies at ATLEE HILL HEALTH AND REHAB CENTER during 2017 to 2025. These included: 1 that caused actual resident harm, 71 with potential for harm, and 8 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
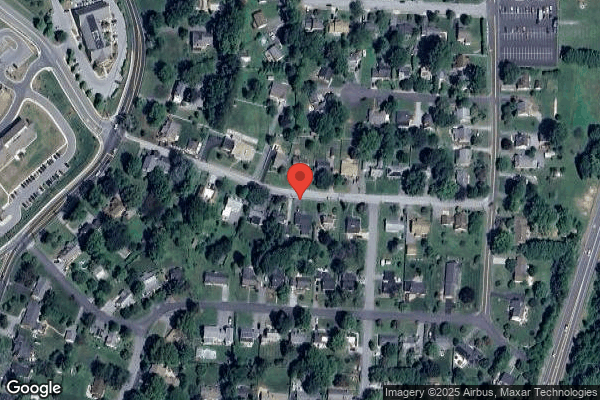
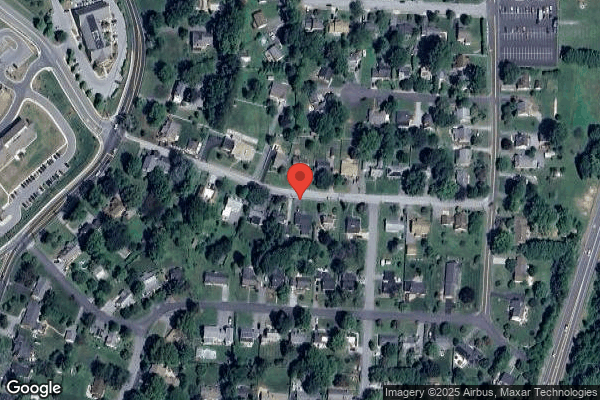
Who Owns and Operates Atlee Hill Health And Rehab Center?
ATLEE HILL HEALTH AND REHAB CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by FUTURE CARE/LIFEBRIDGE HEALTH, a chain that manages multiple nursing homes. With 60 certified beds and approximately 55 residents (about 92% occupancy), it is a smaller facility located in WESTMINSTER, Maryland.
How Does Atlee Hill Health And Rehab Center Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, ATLEE HILL HEALTH AND REHAB CENTER's overall rating (1 stars) is below the state average of 3.0, staff turnover (45%) is near the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Atlee Hill Health And Rehab Center?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Atlee Hill Health And Rehab Center Safe?
Based on CMS inspection data, ATLEE HILL HEALTH AND REHAB CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Maryland. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Atlee Hill Health And Rehab Center Stick Around?
ATLEE HILL HEALTH AND REHAB CENTER has a staff turnover rate of 45%, which is about average for Maryland nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Atlee Hill Health And Rehab Center Ever Fined?
ATLEE HILL HEALTH AND REHAB CENTER has been fined $14,888 across 1 penalty action. This is below the Maryland average of $33,228. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Atlee Hill Health And Rehab Center on Any Federal Watch List?
ATLEE HILL HEALTH AND REHAB CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.