WESTMINSTER HEALTHCARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Westminster Healthcare Center has received a Trust Grade of F, indicating significant concerns and overall poor performance. Ranking #179 out of 219 facilities in Maryland places it in the bottom half, and at #7 out of 10 in Carroll County, only two local options are worse. Although the facility is showing improvement, reducing issues from 34 in 2024 to 8 in 2025, it still has a troubling history. Staffing is rated average with a turnover rate of 50%, which is concerning as it suggests a lack of stability among caregivers. The facility also faces substantial fines totaling $48,789, higher than 78% of Maryland facilities, indicating ongoing compliance issues. Specific incidents include a serious failure to prevent intimidation of a resident following an allegation of sexual abuse, as well as concerns about inadequate food safety procedures in the kitchen, which could affect the health of all residents. Overall, while there are some areas of improvement, the facility's weaknesses raise significant red flags for prospective residents and their families.
- Trust Score
- F
- In Maryland
- #179/219
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 50% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $48,789 in fines. Lower than most Maryland facilities. Relatively clean record.
- Skilled Nurses ✓ Good
- Each resident gets 43 minutes of Registered Nurse (RN) attention daily — more than average for Maryland. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 68 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Maryland average (3.0)
Below average - review inspection findings carefully
Near Maryland avg (46%)
Higher turnover may affect care consistency
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 68 deficiencies on record
Aug 2025
7 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Based on observation, medical record review, facility documentation review and interview, it was determined the facility staff failed to prevent intimidation of a resident after the resident alleged s...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on medical record review, facility documentation review and interview it was determined the facility failed to maintain an effective grievance system as evidenced by the failure to resolve a com...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on review of facility reported incidents and staff interview, it was determined the facility failed to provide documentation that allegations of misappropriation of property were thoroughly inve...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on record review and staff interview it was determined that the facility failed to meet professional standards of practice as evidenced by licensed nursing staff signing off that a medication wa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interviews, it was determined that the medical provider failed to review the pain medication ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview, it was determined the facility failed to provide physician ordered medications timely to meet the needs of the residents. This was evident for 1 (#1...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on medical record review and interview, it was determined the facility failed to maintain complete and accurate medical records in accordance with accepted professional standards. This was evide...
Read full inspector narrative →
Feb 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review, interview, and facility policy review, the facility failed to follow the physician's orders for 1 (Resident #1) of 3 residents reviewed for medications. Specifically, the facil...
Read full inspector narrative →
Oct 2024
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0569
(Tag F0569)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview it was determined that the facility staff failed to notify the family of a deceased residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor observation and interview with staff, it was determined that the facility staff failed to protect the privacy ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on review of facility-reported investigation records and interview with staff, it was determined the facility staff failed to report an allegation of suspected resident abuse to the state agency...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined that the facility staff failed to complete a thorough investigation of an allegation of misappropriation of property and failed to investigation ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on interviews with residents, review of medical records, and interview with facility staff, it was determined that the facility failed to provide a baseline care plan summary to residents. This ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined that the facility staff failed to initiate person centered care plan for mobility and wound care. This deficient practice was evidenced in 1 (#67...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on interviews, observations, and medical records reviews, it was determined that the facility failed to: 1.) perform and/or document that appropriate revisions to care plan goals and interventio...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
6. During a narcotic observation review and reconciliation on 10/16/2024 at 09:45 AM on the first floor, surveyor observed LPN# 24 during a medication administration pass. The surveyor reviewed the Co...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on medical record reviews and interviews it was determined that the facility failed to ensure that a dependent resident's personal hygiene needs were adequately met. This was evident for 1 (Resi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on surveyor observation and interview with staff, it was determined the facility staff failed to ensure medications were s...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interviews it was determined that the facility staff failed to maintain infection control practices as ...
Read full inspector narrative →
Apr 2024
23 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined that the facility failed to treat residents with respect and dignity. This was evident for 1 facility reported incident (MD00204591) of 7 facilit...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on medical record review and interviews with facility staff, it was determined that the facility failed to inform the residents of their right to establish an advance directive and provide assis...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on a complaint, reviews of medical records, and staff interview, it was determined that facility staff failed to notify a resident's representative party and physician when a resident had a chan...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on review of facility records and interview with facility staff, it was determined that facility staff failed to ensure that all allegations of abuse were thoroughly investigated. This was evide...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interviews, it was determined that the facility failed to notify the resident/resident representative in writing of the reserve bed payment policy upon a resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on record review and interview it was determined that the facility failed to ensure care plans were comprehensive. This was evident for 1 resident (Resident #26) of 2 residents reviewed for pres...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on record reviews and interviews it was determined that the facility failed to ensure that resident care was provided in a safe manner. This was evident for 1 facility reported incident (MD00204...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interviews, it was determined that the facility failed to have a system to monitor and respond to changes in residents' weights and notify the physician when w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
Based on observations, record reviews, and resident and staff interviews, it was determined that the facility failed to evaluate residents' pain. This was evident for one Resident (# 354) of two resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on a review of employee files and interviews, it was determined that the facility failed to put a system in place to ensure Geriatric Nursing Assistant (GNAs) were competent with their skill set...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record review and staff interviews, it was determined that the facility failed to follow recommended parameters prescribed by the physician when administering blood pressure and pain medicati...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review it was determined that the facility failed to provide dental services to meet residents' needs. This was evident for 1 of 2 (Resident #17) reviewed fo...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0801
(Tag F0801)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview it was determined the facility failed to ensure overall supervisory responsibilities for the facility's kitchen was assigned to a qualified dietetic ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and interviews, it was determined the facility failed to: 1) adequately document certifications of incapacity and ensure accuracy of the Maryland Medical orders for life sustain...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interviews, it was determined that the facility failed to: 1) revise and update a compr...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, staff interviews and a complaint, it was determined that the facility failed to: 1) have a proce...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and staff interview it was determined that the physician/Certified Registered Nurse Practitioner ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0838
(Tag F0838)
Could have caused harm · This affected multiple residents
Based on record review and interview it was determined that the facility failed to include dietary staffing as part of the facility assessment. This was evident during review of the facility's assessm...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0802
(Tag F0802)
Could have caused harm · This affected most or all residents
Based on interview and record review it was determined the facility failed to ensure the kitchen maintained adequate staffing levels. This deficient practice affects all residents.
The findings inclu...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations of the facility's kitchen, review of kitchen records and interviews of dietary staff, it was determined that the facility failed to: 1.) ensure the monitoring and oversight of fo...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Social Worker
(Tag F0850)
Could have caused harm · This affected most or all residents
Based on record review and interviews it was determined that the facility failed to employ a qualified social worker on a full-time basis. This was evident during the recertification survey and had th...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected most or all residents
Based on record reviews and staff interviews, it was determined that the facility failed to meet at least quarterly to conduct required Quality Assurance and Performance Improvement (QAPI) activities....
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Deficiency F0577
(Tag F0577)
Minor procedural issue · This affected most or all residents
Based on observations and interview with staff it was determined the facility staff failed to ensure the results from the last annual survey were posted in a place readily accessible to residents and ...
Read full inspector narrative →
Sept 2023
26 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0551
(Tag F0551)
Could have caused harm · This affected 1 resident
Based on medical record review and interview of facility staff it was determined the facility failed to identify the responsible party of a resident. This was evident for one (Resident #144) out of th...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
2) On 8/31/23 at 1:28 PM, a review of the facility's investigation file for the facility reported incident MD00186429 revealed that Resident #62 had reported that there was a delay in his/her care on ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Based on record review and staff interviews, it was determined that the facility failed to protect a resident's right to be free from misappropriation and/or exploitation. This was evident for 1 (#78)...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined the facility staff failed to notify the resident/resident representative in writing of a transfer/discharge of a resident along wit...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews it was determined that the facility failed to develop and implement a compr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2) On 9/14/23 at 3:12 PM review of a facility reported incident MD00195946 revealed that License Practical Nurse (LPN) #25 a cha...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
Based on medical record review and interview it was determined the facility failed to ensure residents' bathing preference for showers. This was evident for 1 (Resident #142) out of 2 residents review...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review and interview of facility staff it was determined the facility failed to: 1) ensure a resident re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observations, record review, and interview of facility staff it was determined the facility failed to implement the resident's care plan for a resident at risk for falls. This was evident for...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0711
(Tag F0711)
Could have caused harm · This affected 1 resident
Based on medical record review and staff interview it was determined the physician progress notes were not placed timely in the resident medical records. This was evident for 3 (#13, #93, and #131) of...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
2) On 8/29/23 at 11:30 AM a review of the Controlled Drug Administration Records (CDAR) located on the first-floor medication cart revealed some discrepancies with documentation of the removal times. ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on review of the medical record and interview with staff it was determined the facility staff failed to ensure that the attending physician documented in the medical record that drug irregularit...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
2) Review of Resident #34's Medication Administration Records (MAR) on 8/30/23 at 1:00 PM revealed an order, Morphine Sulphate (concentrate) oral solution 100mg/5ml, give 0.5mg sublingually every 6 ho...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
2) On 8/16/23 at 12:28 PM, Resident #62 told the surveyor in an interview that s/he has been asking to see an oral surgeon for a tooth pull since January 2023 but has only seen the dental hygienist.
A...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined that the facility failed to monitor and track antibiotic usage and resistance data. This was evident for 1 (Resident #159) out of 3 residents' a...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
6) On 9/07/23 at 12:51 PM a review of facility self-report #MD00186322 revealed that Resident #22 was found with blisters/burns on his/her neck and chest. Although the self-report indicated that the i...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
8) On 8/17/23 at 1:34 PM a review of the facility self-report MD00185460 was conducted. The report stated that Resident #66's roommate reported that he/she observed an unidentified male Geriatric Nurs...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record review, and interviews, it was determined that the facility staff failed to ensure Minimum Data Se...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 8). On 8/18/23 at 10:17 AM a review of the medical record revealed that Resident #66 was admitted to the facility on [DATE] afte...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4) On 9/18/23 at 9:42AM, the surveyor reviewed the medical record for Resident #2 which revealed a nurse's note dated 3/17/23 do...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident, family and staff interview, documentation review, observation, and review of Resident Council meeting minutes...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on record review and interviews it was determined that the facility failed to assure that all nursing staff had competency evaluations. This was evident for 5 (RN #42, GNA #43, GNA #57, GNA #58,...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on review of Geriatric Nursing Assistant (GNA) employee records and staff interview, it was determined the facility failed to conduct yearly performance reviews at least every 12 months. This wa...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 5) On 8/16/23 at 12:02PM the surveyor observed Resident #91 in their bed with only one floor mat in place next to their bed. On ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected multiple residents
Based on interview and documentation review, it was determined the facility failed to ensure that staff received training regarding abuse, neglect, exploitation, misappropriation of resident property....
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected most or all residents
Based on interviews, observation, and record review, it was determined that the facility administration failed to provide adequate oversight activities for the facility to ensure that resources were u...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 1 harm violation(s), $48,789 in fines. Review inspection reports carefully.
- • 68 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • $48,789 in fines. Higher than 94% of Maryland facilities, suggesting repeated compliance issues.
- • Grade F (25/100). Below average facility with significant concerns.
About This Facility
What is Westminster Healthcare Center's CMS Rating?
CMS assigns WESTMINSTER HEALTHCARE CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Maryland, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Westminster Healthcare Center Staffed?
CMS rates WESTMINSTER HEALTHCARE CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 50%, compared to the Maryland average of 46%. RN turnover specifically is 59%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Westminster Healthcare Center?
State health inspectors documented 68 deficiencies at WESTMINSTER HEALTHCARE CENTER during 2023 to 2025. These included: 1 that caused actual resident harm, 66 with potential for harm, and 1 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Westminster Healthcare Center?
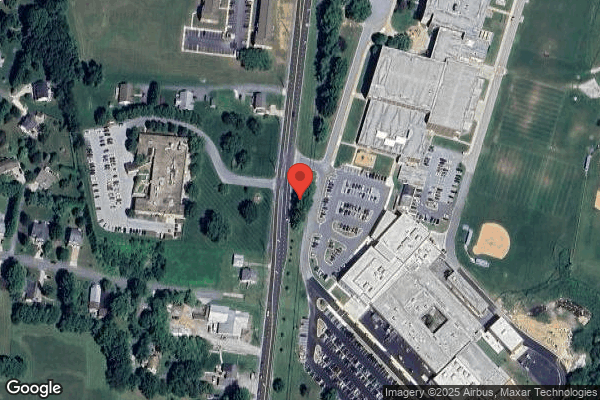
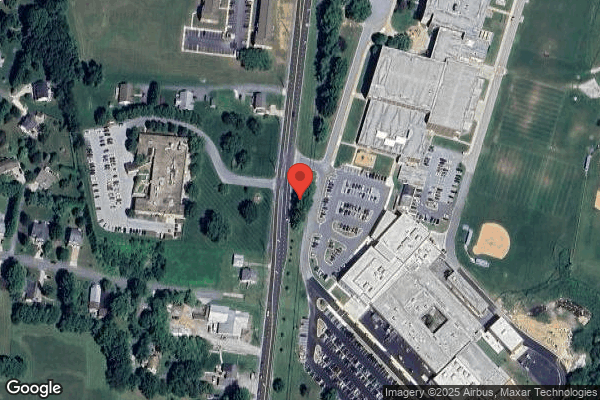
WESTMINSTER HEALTHCARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by COMMUNICARE HEALTH, a chain that manages multiple nursing homes. With 170 certified beds and approximately 115 residents (about 68% occupancy), it is a mid-sized facility located in WESTMINSTER, Maryland.
How Does Westminster Healthcare Center Compare to Other Maryland Nursing Homes?
Compared to the 100 nursing homes in Maryland, WESTMINSTER HEALTHCARE CENTER's overall rating (2 stars) is below the state average of 3.0, staff turnover (50%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Westminster Healthcare Center?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the substantiated abuse finding on record.
Is Westminster Healthcare Center Safe?
Based on CMS inspection data, WESTMINSTER HEALTHCARE CENTER has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Maryland. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Westminster Healthcare Center Stick Around?
WESTMINSTER HEALTHCARE CENTER has a staff turnover rate of 50%, which is about average for Maryland nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Westminster Healthcare Center Ever Fined?
WESTMINSTER HEALTHCARE CENTER has been fined $48,789 across 1 penalty action. The Maryland average is $33,567. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Westminster Healthcare Center on Any Federal Watch List?
WESTMINSTER HEALTHCARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.