LIFE CARE CENTER OF AUBURN




Inspected within the last 6 months. Data reflects current conditions.
Life Care Center of Auburn has received a Trust Grade of D, which indicates below-average performance and some concerns. Ranking #161 out of 338 facilities in Massachusetts places it in the top half, while its county rank of #24 out of 50 suggests that only a few local options are better. The facility is improving, with issues decreasing from 10 in 2024 to 7 in 2025, though it still has a high number of deficiencies, totaling 35. Staffing is a relative strength here, with a turnover rate of 28%, which is well below the state's average, and average RN coverage ensures basic medical needs are met. However, there are serious concerns, such as failing to manage a resident's pressure ulcer properly and neglecting to provide timely pain medication during a dressing change, indicating potential gaps in care.
- Trust Score
- D
- In Massachusetts
- #161/338
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ✓ Good
- 28% annual turnover. Excellent stability, 20 points below Massachusetts's 48% average. Staff who stay learn residents' needs.
- Penalties ⚠ Watch
- $32,988 in fines. Higher than 83% of Massachusetts facilities, suggesting repeated compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 29 minutes of Registered Nurse (RN) attention daily — below average for Massachusetts. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 35 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Low Staff Turnover (28%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (28%)
20 points below Massachusetts average of 48%
Facility shows strength in quality measures, staff retention, fire safety.
The Bad
Near Massachusetts average (2.9)
Meets federal standards, typical of most facilities
Below median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 35 deficiencies on record
Jun 2025
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on interviews, and record reviews, the facility failed to notify the state mental health authority (Pre-admission Screening and Resident Review [PASRR] Office) promptly of the need for Resident ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to identify a change in condition relative to bilater...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews, and interviews, the facility failed to adhere to infection control standards of practice ...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Assessment Accuracy
(Tag F0641)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews, and interviews, the facility failed to complete Comprehensive Minimum Data Set (MDS) Assessments that a...
Read full inspector narrative →
Jan 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on interviews and records reviewed, for two of five sampled residents (Residents #2 and #3), the Facility failed to ensure staff implemented and followed the Facility Abuse Prohibition Policy, w...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interviews and records reviewed, for two of five sampled residents (Residents #1 and #4), the Facility failed to ensure they reported allegations of abuse by Housekeeper #1 to the Department ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interviews and records reviewed, for two of five sampled residents (Resident #1 and #4), the Facility failed to ensure that after being made aware of allegations of potential sexual abuse by ...
Read full inspector narrative →
Apr 2024
10 deficiencies
2 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record and policy review, the facility failed to provide care consistent with professional stan...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
Based on observation, interview and record review, the facility failed to provide pain management that was consistent with professional standards of practice for one Resident (#18) out of a total samp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide treatment, services and care that met professional standards of quality for one Resident (#18) out of a total sample ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide services and to assist with obtaining a specialist consultation for one Resident (#102), out of a total sample of 25 ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record reviewed the facility failed to provide sufficient nursing staff with the appropriate competencies and skills sets to provide nursing and related services t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected 1 resident
1b. On 4/8/24 at 7:50 A.M., the surveyor observed the following during the follow-up visit to the main kitchen:
-Dietary Staff #2 prepared food items on the service line with an improperly placed hair...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected multiple residents
Based on interview, record and policy review, the facility failed to notify the Physician/Non Physician Practitioner (NPP: Nurse Practitioner) of a significant change in physical status for one Reside...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
Based on observation, interview, record and policy review, the facility failed to provide nutrition care and services for one Resident (#102) out of a total sample of 25 residents, with a history of w...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
2. Resident #95 was admitted to the facility in August 2023 with diagnoses including Pressure Ulcer of Left Heel, Pressure Ulcer of Right Heel, Pressure Ulcer of Unspecified Part of Back, and Pressure...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
MDS Data Transmission
(Tag F0640)
Minor procedural issue · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to accurately complete, encode and transmit Minimum Data Set (MDS) Ass...
Read full inspector narrative →
Dec 2022
18 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and policy review, the facility failed to ensure its staff provided dignity and privacy for one Resident (#30), out of a total sample of 29 residents, relative to pl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to ensure its staff provided notification of a change in condition for one Resident (#30), out of 29 sampled residents. Specifically, failure...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
3. Resident #35 was admitted to the facility April 2019.
Review of the facility policy titled Comprehensive Care Plans and Revisions, reviewed 8/17/22, indicated the following:
-A comprehensive care p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record review, the facility failed to ensure its staff provided activities designed to support the physical, mental, and psychosocial well-being for one Resident...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and record review, the facility failed to ensure its staff provided timely care and treatment for a chronic ulcer (open area) located on one Resident (#104)'s lower e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure its staff provided appropriate treatment and...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record review, the facility failed to ensure its staff assessed the safety of one Resident (#42), out of 29 sampled residents, to self-administer Albuterol (a me...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #128 the facility staff failed to ensure the Resident had appropriate orders for the care and services of a urin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record review, the facility failed to ensure its staff provided appropriate care and services relative to respiratory care for one Resident (#42), out of 29 samp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure that its staff provided comprehensive behavior...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure its staff obtained orders for a PRN (as needed) antipsychotic medication (medication used to manage psychotic disorders) that were l...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure its staff maintained accurate documentation for one Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure its staff maintained a record that contained the most recent plan of care from Hospice and Hospice documentation that could be utili...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on interviews and record review, the facility failed to ensure its staff maintained a medical record that included documentation that residents were offered, received or declined the pneumococca...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record reviews, the facility failed to ensure its staff provided a Notice of Transfer and Discharge to t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, record reviews, and policy review, the facility failed to ensure its staff provided the Resident and/or the...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record reviews, the facility failed to ensure its staff: 1) implemented recommendations for infection control and prevention relative to the use of personal prot...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Assessment Accuracy
(Tag F0641)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, the facility failed to ensure Minimum Data Set (MDS) Assessments were coded accurately f...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 28% annual turnover. Excellent stability, 20 points below Massachusetts's 48% average. Staff who stay learn residents' needs.
- • Multiple safety concerns identified: 2 harm violation(s), $32,988 in fines, Payment denial on record. Review inspection reports carefully.
- • 35 deficiencies on record, including 2 serious (caused harm) violations. Ask about corrective actions taken.
- • $32,988 in fines. Higher than 94% of Massachusetts facilities, suggesting repeated compliance issues.
- • Grade D (48/100). Below average facility with significant concerns.
About This Facility
What is Life Of Auburn's CMS Rating?
CMS assigns LIFE CARE CENTER OF AUBURN an overall rating of 3 out of 5 stars, which is considered average nationally. Within Massachusetts, this rating places the facility higher than 99% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Life Of Auburn Staffed?
CMS rates LIFE CARE CENTER OF AUBURN's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 28%, compared to the Massachusetts average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Life Of Auburn?
State health inspectors documented 35 deficiencies at LIFE CARE CENTER OF AUBURN during 2022 to 2025. These included: 2 that caused actual resident harm, 30 with potential for harm, and 3 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
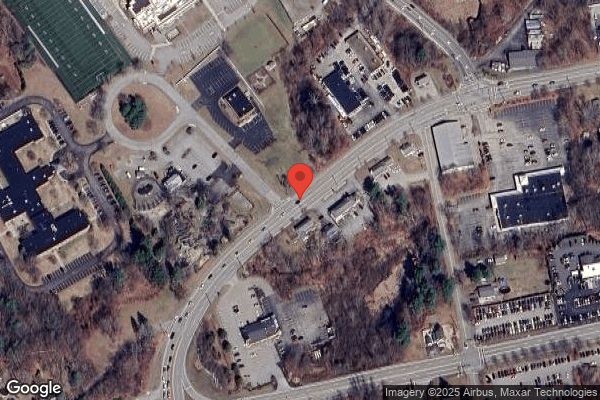
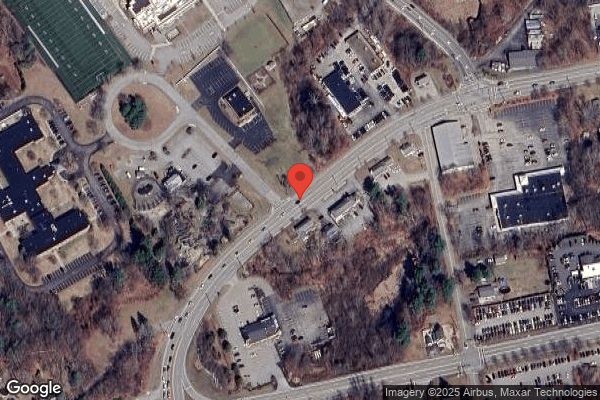
Who Owns and Operates Life Of Auburn?
LIFE CARE CENTER OF AUBURN is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by LIFE CARE CENTERS OF AMERICA, a chain that manages multiple nursing homes. With 154 certified beds and approximately 141 residents (about 92% occupancy), it is a mid-sized facility located in AUBURN, Massachusetts.
How Does Life Of Auburn Compare to Other Massachusetts Nursing Homes?
Compared to the 100 nursing homes in Massachusetts, LIFE CARE CENTER OF AUBURN's overall rating (3 stars) is above the state average of 2.9, staff turnover (28%) is significantly lower than the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Life Of Auburn?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Life Of Auburn Safe?
Based on CMS inspection data, LIFE CARE CENTER OF AUBURN has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in Massachusetts. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Life Of Auburn Stick Around?
Staff at LIFE CARE CENTER OF AUBURN tend to stick around. With a turnover rate of 28%, the facility is 18 percentage points below the Massachusetts average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly.
Was Life Of Auburn Ever Fined?
LIFE CARE CENTER OF AUBURN has been fined $32,988 across 2 penalty actions. This is below the Massachusetts average of $33,409. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Life Of Auburn on Any Federal Watch List?
LIFE CARE CENTER OF AUBURN is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.