PARSONS HILL REHABILITATION & HEALTH CARE CENTER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Parsons Hill Rehabilitation & Health Care Center has a Trust Grade of C, which means it is average-right in the middle of the pack. It ranks #234 out of 338 facilities in Massachusetts, placing it in the bottom half, and #38 out of 50 in Worcester County, indicating that there are better local options available. The facility is showing signs of improvement, as the number of issues decreased from 18 in 2024 to 13 in 2025. Staffing is a relative strength with a 3/5 rating and a low turnover rate of 26%, which is below the state average, suggesting staff stability. However, there were some concerning findings, including a lack of RN coverage for at least eight consecutive hours on one day and failures to conduct timely COVID-19 testing during an outbreak. Additionally, the facility did not provide proper discharge notices for some residents, highlighting areas that need attention. Overall, while there are strengths in staffing and a trend of improvement, there are significant weaknesses in compliance and communication that families should consider.
- Trust Score
- C
- In Massachusetts
- #234/338
- Safety Record
- Low Risk
- Inspections
- Getting Better
- Staff Stability ✓ Good
- 26% annual turnover. Excellent stability, 22 points below Massachusetts's 48% average. Staff who stay learn residents' needs.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Massachusetts facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 27 minutes of Registered Nurse (RN) attention daily — below average for Massachusetts. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 53 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Low Staff Turnover (26%) · Staff stability means consistent care
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover is low (26%)
22 points below Massachusetts average of 48%
Facility shows strength in quality measures, staff retention, fire safety.
The Bad
Below Massachusetts average (2.9)
Below average - review inspection findings carefully
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 53 deficiencies on record
Aug 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0628
(Tag F0628)
Could have caused harm · This affected multiple residents
Based on records reviewed and interviews, for three of four sampled residents (Resident #1, Resident #2, and Resident #4), the Facility failed to ensure that prior to the time of their discharge from ...
Read full inspector narrative →
Apr 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for three of three sampled residents (Resident #1, #2, and #3), as well as interviews ...
Read full inspector narrative →
Mar 2025
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on record review, and interview, the facility failed to ensure that residents and/or their representatives were informed and given necessary information to make health care decisions including t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, and interview, the facility failed to provide a safe and homelike environment for one Resident (#3) out of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and interview, the facility failed to coordinate vision care services for one Resident (#129) out of a t...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide necessary care and services relative to enter...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide respiratory care and services consistent with professional standards of practice for one Resident (#91), out of a tot...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
2. Resident #147 was admitted to the facility in January 2025 with diagnoses including End Stage Renal Disease (ESRD) and Adult Failure to Thrive.
Review of Resident #147's Care Plan for Hemodialysis,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. The Food and Drug Administration (FDA) Highlights of Prescribing Levothyroxine Tablets for Oral Use, dated December 2017, ind...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, and interview, the facility failed to adhere to infection control standards of practice, increasing the risk of contamination and the spread of infection to other residents withi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, and interview, the facility failed to implement an effective pest control program on three Units (Tatnuck,...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0582
(Tag F0582)
Minor procedural issue · This affected multiple residents
Based on interview, and record review, the facility failed to ensure that the Notice of Medicare Non-Coverage (NOMNC: notice issued to a resident who is receiving benefits under Medicare Part A when a...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Assessment Accuracy
(Tag F0641)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of the Centers for Medicare and Medicaid Services (CMS) Long-Term Care Facility Resident Assessment Instrument (RAI) U...
Read full inspector narrative →
Jul 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, the Facility, (who had an in-house census of 148 residents) failed to ensure that the Director of Nurses (DON) did not serve as a charge nurse on a unit, when...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews, for one of three sampled residents (Resident #1) who's Comprehensive Care Plan and Hos...
Read full inspector narrative →
Jan 2024
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0557
(Tag F0557)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure that one Resident (#40) out of a total sample ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on observation, interview, record and policy review, the facility failed to prohibit and prevent abuse and retaliation following the reporting of an alleged violation to law enforcement for two ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to re-submit a Level 1 Preadmission Screening and Resident Review (PASARR- is a federal requirement to help ensure that individuals are not in...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of the facility policy Trauma Informed Care, undated, indicated the following:
-It is the policy of this facility to e...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, the facility failed to provide activities as scheduled, on the Tatnuck Unit and to meet the needs of three Residents (#12, #40, and #248), in a tota...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide proper assistive devices to maintain hearing abilities for ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide adequate nutritional care and services for one...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on interview, policy and record review, the facility failed to ensure that one Resident (#102) out of a total sample of 31 Residents, received dialysis care consistent with professional standard...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on interview, record and policy review, the facility failed to ensure that performance reviews were completed every 12 months and regular in-service education was provided based on the outcome o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
Based on observation, interview, policy and record review, the facility failed to meet the nutritional needs for one resident (Resident #348) out of a total sample of 31 residents.
Specifically, the ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on observation, interview, policy and record review, the facility failed to maintain accurate medical records to reflect the status of the residents for two Residents (#130 and #141) out of a to...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, records reviewed and policy review, the facility failed to ensure that the Pneumococcal Vaccine was offered...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #141 was admitted to the facility in November 2023 with a diagnosis of Retention of Urine (inability to urinate) and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on interview, policy and record review, the facility failed to ensure that three licensed nursing staff (Unit Manager #2, Nurse #5 and Nurse #6), out of a sample of five licensed nursing staff, ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and National Standards reviewed, the facility failed to provide a safe, sanitary environment fo...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to provide coverage as required by a Registered Nurse (RN) for at least eight consecutive hours a day for seven days a week.
Specifically, th...
Read full inspector narrative →
Apr 2023
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on records reviewed and interviews for one of three sampled residents (Resident #1), who required continual supervision wi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on records reviewed and interviews, for one of three sampled residents (Resident #1) who was care planned as being at risk for elopement, had his/her picture in the Elopement Risk Binder which w...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected multiple residents
Based on records reviewed and interviews, the Facility failed to ensure their policy related to Patient/Resident Trust Accounts was implemented and followed when residents reported they did not have a...
Read full inspector narrative →
Feb 2023
2 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on policy review, record review and interview, the facility failed to ensure its staff implemented their policy for annual influenza vaccination for one Resident (#4) out of five applicable samp...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review and interview, the facility failed to ensure its staff conducted COVID-19 outbreak testing...
Read full inspector narrative →
Nov 2022
3 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review, and interview, the facility failed to ensure its staff offered the pneumococcal vaccine t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of the Centers for Disease Control (CDC) Interim Guidelines for Collecting and Handling of Clinical Specimens for COVI...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on policy review, record review, and interview, the facility failed to ensure its staff conducted COVID-19 testing for bot...
Read full inspector narrative →
Jul 2022
14 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record reviews and interviews, the facility failed to ensure that its staff accurately identifed advance directives rel...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on observations, record reviews, and interviews, the facility failed to ensure that its staff: a) notified the Physician/Non Physician Practitioner (NPP) of changes in the condition of two Resid...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interviews, record review, and policy review, the facility failed to ensure that its staff investigated and reported a resident to resident altercation for one Resident (#10) out of a total s...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interviews, the facility failed to ensure that its staff completed: a) a fall evaluation assessment f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure that its staff developed a baseline care plan within 48 hours of admission to the facility for one Resident (#119) out of 30 total s...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0676
(Tag F0676)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews, and record review, the facility failed to ensure its staff assisted one Resident (#133) in obt...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record review, the facility failed to ensure its staff provided appropriate care and services for one Resident (#71), relative to a wound on the Resident's left ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
3. For Resident #91, the facility failed to ensure its staff made certain that the Resident did not smoke cigarettes while wearing a nicotine transdermal patch.
Resident #91 was admitted to the facili...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on observation, interview, record review, and policy review, the facility failed to ensure that its staff provided care consistent with professional standards, related to the changing of oxygen ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #9 was admitted to the facility in June 2021 with the following diagnoses: ESRD and dependence on renal dialysis.
Re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record reviews and interviews, the facility failed to ensure that its staff documented in the medical record that the recommendations from the Pharmacist's drug regimen review had been review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview the facility failed to ensure that its staff implemented the dietary plan of ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0920
(Tag F0920)
Could have caused harm · This affected 1 resident
Based on observations and interviews, the facility failed to ensure that its staff provided adequate space and furnishings for resident dining on one of four units.
Findings include:
Review of the cen...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
MDS Data Transmission
(Tag F0640)
Minor procedural issue · This affected multiple residents
Based on record reviews and interview, the facility failed to ensure that its staff encoded and transmitted discharge Minimum Data Set (MDS) assessments for five Residents (#2, #3, #4, #5, and #46) ou...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No major safety red flags. No abuse findings, life-threatening violations, or SFF status.
- • No fines on record. Clean compliance history, better than most Massachusetts facilities.
- • 26% annual turnover. Excellent stability, 22 points below Massachusetts's 48% average. Staff who stay learn residents' needs.
- • 53 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • Grade C (53/100). Below average facility with significant concerns.
About This Facility
What is Parsons Hill Rehabilitation & Health's CMS Rating?
CMS assigns PARSONS HILL REHABILITATION & HEALTH CARE CENTER an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Massachusetts, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Parsons Hill Rehabilitation & Health Staffed?
CMS rates PARSONS HILL REHABILITATION & HEALTH CARE CENTER's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 26%, compared to the Massachusetts average of 46%. This relatively stable workforce can support continuity of care.
What Have Inspectors Found at Parsons Hill Rehabilitation & Health?
State health inspectors documented 53 deficiencies at PARSONS HILL REHABILITATION & HEALTH CARE CENTER during 2022 to 2025. These included: 50 with potential for harm and 3 minor or isolated issues. While no single deficiency reached the most serious levels, the total volume warrants attention from prospective families.
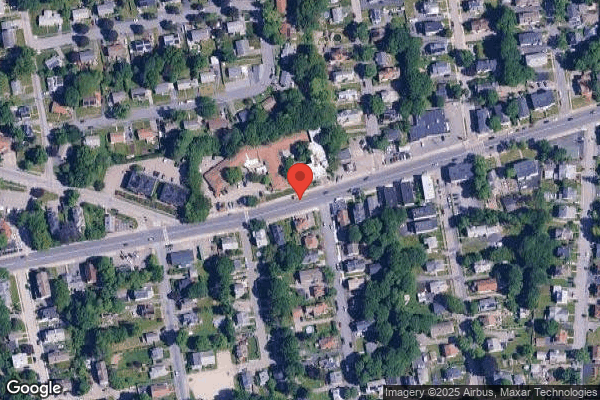
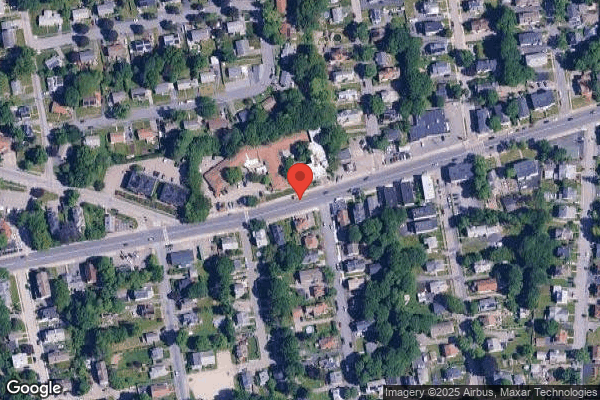
Who Owns and Operates Parsons Hill Rehabilitation & Health?
PARSONS HILL REHABILITATION & HEALTH CARE CENTER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by ATHENA HEALTHCARE SYSTEMS, a chain that manages multiple nursing homes. With 162 certified beds and approximately 150 residents (about 93% occupancy), it is a mid-sized facility located in WORCESTER, Massachusetts.
How Does Parsons Hill Rehabilitation & Health Compare to Other Massachusetts Nursing Homes?
Compared to the 100 nursing homes in Massachusetts, PARSONS HILL REHABILITATION & HEALTH CARE CENTER's overall rating (2 stars) is below the state average of 2.9, staff turnover (26%) is significantly lower than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Parsons Hill Rehabilitation & Health?
Based on this facility's data, families visiting should ask: "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?"
Is Parsons Hill Rehabilitation & Health Safe?
Based on CMS inspection data, PARSONS HILL REHABILITATION & HEALTH CARE CENTER has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Massachusetts. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Parsons Hill Rehabilitation & Health Stick Around?
Staff at PARSONS HILL REHABILITATION & HEALTH CARE CENTER tend to stick around. With a turnover rate of 26%, the facility is 19 percentage points below the Massachusetts average of 46%. Low turnover is a positive sign. It means caregivers have time to learn each resident's needs, medications, and personal preferences. Consistent staff also notice subtle changes in a resident's condition more quickly. Registered Nurse turnover is also low at 29%, meaning experienced RNs are available to handle complex medical needs.
Was Parsons Hill Rehabilitation & Health Ever Fined?
PARSONS HILL REHABILITATION & HEALTH CARE CENTER has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Parsons Hill Rehabilitation & Health on Any Federal Watch List?
PARSONS HILL REHABILITATION & HEALTH CARE CENTER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.