Riverview Health and Rehab Center North




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Riverview Health and Rehab Center North has a Trust Grade of F, indicating significant concerns about the quality of care provided. It ranks #331 out of 422 facilities in Michigan, placing it in the bottom half of nursing homes, and #53 of 63 in Wayne County, suggesting limited local options for improvement. The facility is showing signs of improvement, reducing issues from 28 in 2024 to 5 in 2025, but still has a lot of ground to cover. Staffing is average with a rating of 3 out of 5 stars and a turnover rate of 54%, which is close to the state average. However, there are serious concerns as the center has received $38,471 in fines, indicating compliance issues, and has less RN coverage than 97% of Michigan facilities, meaning there may be less oversight for resident care. Specific incidents raise alarm, such as a resident suffering a fractured pelvis after being dropped during care, which resulted in their eventual death. Additionally, the facility allowed staff with long nails to provide personal care, leading to discomfort and injury to a resident. There were also concerns about food safety practices in the kitchen, with improperly dated food and cleanliness issues that could pose health risks. While there are some strengths, such as an improving trend, the number of serious and critical incidents highlights the need for careful consideration by families looking for care.
- Trust Score
- F
- In Michigan
- #331/422
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 54% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $38,471 in fines. Higher than 57% of Michigan facilities. Some compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 13 minutes of Registered Nurse (RN) attention daily — below average for Michigan. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 39 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Michigan average (3.1)
Below average - review inspection findings carefully
Near Michigan avg (46%)
Higher turnover may affect care consistency
Above median ($33,413)
Moderate penalties - review what triggered them
The Ugly 39 deficiencies on record
Apr 2025
3 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to document and ensure resident's activity preferences w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure meals were served at palatable temperatures fo...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to: 1. Properly date-label food stored in the walk-in freezer and walk-in cooler, 2. Ensure food past the use-by-date was not st...
Read full inspector narrative →
Jan 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake MI00149358.
Based on interview and record review, the facility failed to ensure staff reported ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake MI00149358.
Based on interview, and record review the facility failed to update/revise/review a...
Read full inspector narrative →
Aug 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0559
(Tag F0559)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to notify and discuss a room change with a resident and ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to develop or implement a person-centered behavior care p...
Read full inspector narrative →
Jul 2024
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake MI00145652.
Based on interview and record review the facility failed to review the Plan of Care...
Read full inspector narrative →
May 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Transfer
(Tag F0626)
Could have caused harm · This affected 1 resident
This citation pertains to intake MI00143701.
Based on interview and record review the facility failed to readmit one resident (R609) to the facility upon discharge from a hospital.
Findings include:
...
Read full inspector narrative →
Feb 2024
24 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** DPS #2
Based on observation, interview, and record review, the facility failed to prevent injury when allowing nursing staff to ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide dignified dining for one resident (R17) of on...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure a call light was within reach of one (R92) of ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review the facility failed to provide showers as desired for one resident (R103) of two residents reviewed for choices, resulting in resident dissatisfactio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide a clean and comfortable environment for two re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to file a report with the state of Michigan within a 24-hour period concerning an allegation of staff to resident abuse for one resident (R115)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0645
(Tag F0645)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R89
On 2/13/24 at 2:17 PM, record review revealed R89's last PASARR I (Pre-admission Screening and Annual Resident Review) scree...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide adequate Activities of Daily Living (ADL) care...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide vision services for one of one resident (R120)...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to provide adequate foot care for one resident (R101) out...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to follow therapy recommendations to initiate restorative...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake MI00141655.
Based on observation, interview, and record review the facility failed to ensure th...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to respond to a pharmacy recommendation for one resident (R3) of two residents reviewed for medication and medication regimen, resulting in a l...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to justify the use of three medications for one resident (R3) of two residents reviewed for medication and medication regimen, re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Room Equipment
(Tag F0908)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to maintain medical equipment in safe operating condition.
Findings include:
On 2/11/24 at 8:59 AM an observation of the third fl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R41
On 2/11/24 at 3:34 p.m. R41 was observed resting in bed watching television. The resident presented as alert and oriented to...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** R20
On 02/11/24 at 01:06 PM R20 was observed with a contracted left hand. When asked if he wore a palm protector, R20 nodded yes...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0726
(Tag F0726)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to ensure that five out of five (FF, MM, NN, OO, and PP ) certified nurse aides (CNA) whose in-service files were reviewed, had the required a...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected multiple residents
Based on interview and record review the facility failed to ensure certified nurse aides (CNAs) fulfilled the requirement to complete 12 hours of in-service education annually for five of five certifi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** DPS#3
Based on observation, interview, and record review the facility failed to ensure (1) a tub was cleaned/sanitized and (2) e...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview the facility failed to ensure hand sinks were in good repair to be easily cleaned and sanitiz...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0563
(Tag F0563)
Could have caused harm · This affected most or all residents
R120
On 2/11/24 at 3:12 p.m. during the resident representative (family member) interview for R120, the family expressed being angry following the resident's most recent fall which resulted in being t...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to: 1. Maintain food service equipment in a clean and sanitary manner; 2. Ensure walls in areas where food was prepared were cle...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected most or all residents
Based on interview and record review the facility failed to ensure that the Medical Director (MD) attended the Quality Assurance and Performance Improvement (QAPI-program aimed on improving processes ...
Read full inspector narrative →
Jan 2023
6 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to accurately transcribe a physician's medication order a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to intake MI0027872.
Based on observation, interview and record review, the facility failed to ensure fre...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure they consistently offered and administered influenza and pne...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to consistently utilize the services of a Registered Nurse (RN) for eight consecutive hours per day, seven days per week, affecting all reside...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to ensure the Infection Preventionist completed specialized training in infection prevention and control, resulting in the potential for knowl...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to implement their COVID-19 policy and demonstrate they had screened fo...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s), 1 harm violation(s), $38,471 in fines, Payment denial on record. Review inspection reports carefully.
- • 39 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $38,471 in fines. Higher than 94% of Michigan facilities, suggesting repeated compliance issues.
- • Grade F (28/100). Below average facility with significant concerns.
About This Facility
What is Riverview Health And Rehab Center North's CMS Rating?
CMS assigns Riverview Health and Rehab Center North an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Michigan, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Riverview Health And Rehab Center North Staffed?
CMS rates Riverview Health and Rehab Center North's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 54%, compared to the Michigan average of 46%.
What Have Inspectors Found at Riverview Health And Rehab Center North?
State health inspectors documented 39 deficiencies at Riverview Health and Rehab Center North during 2023 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 1 that caused actual resident harm, and 37 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Riverview Health And Rehab Center North?
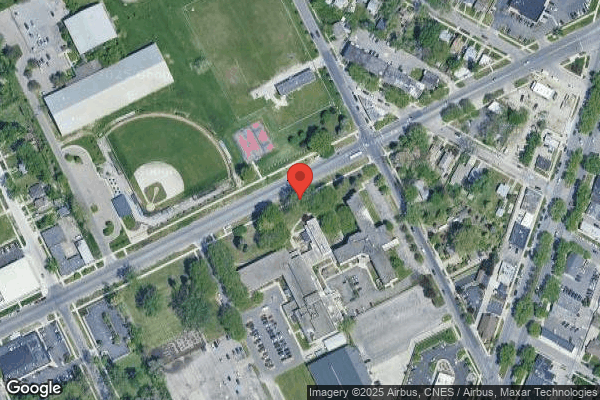
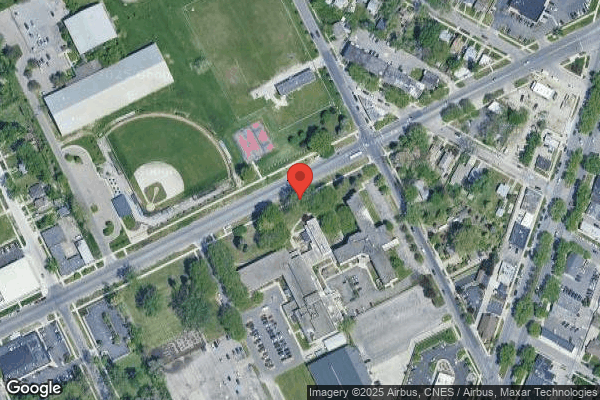
Riverview Health and Rehab Center North is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 180 certified beds and approximately 133 residents (about 74% occupancy), it is a mid-sized facility located in Detroit, Michigan.
How Does Riverview Health And Rehab Center North Compare to Other Michigan Nursing Homes?
Compared to the 100 nursing homes in Michigan, Riverview Health and Rehab Center North's overall rating (2 stars) is below the state average of 3.1, staff turnover (54%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Riverview Health And Rehab Center North?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Riverview Health And Rehab Center North Safe?
Based on CMS inspection data, Riverview Health and Rehab Center North has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Michigan. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Riverview Health And Rehab Center North Stick Around?
Riverview Health and Rehab Center North has a staff turnover rate of 54%, which is 8 percentage points above the Michigan average of 46%. Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Riverview Health And Rehab Center North Ever Fined?
Riverview Health and Rehab Center North has been fined $38,471 across 4 penalty actions. The Michigan average is $33,464. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Riverview Health And Rehab Center North on Any Federal Watch List?
Riverview Health and Rehab Center North is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.