CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0573
(Tag F0573)
Could have caused harm · This affected 1 resident
This citation pertains to Intake # MI00135264.
Based on interview and record review, the facility failed to respond timely to a request for medical records in 1 resident (Resident #38) of 1 resident r...
Read full inspector narrative →
This citation pertains to Intake # MI00135264.
Based on interview and record review, the facility failed to respond timely to a request for medical records in 1 resident (Resident #38) of 1 resident reviewed for medical record requests, resulting in delayed access to a resident's medical records and dissatisfaction with the services provided.
Findings include:
Review of the policy/procedure Preparing for Release, dated 2017, revealed .To protect the individual's right to privacy by releasing confidential information only to authorized persons/entities, and only in accordance with Facility policy, federal and state laws .Procedure .Require request to be in writing .Facility must provide access to resident the requested records for inspection within 24 hours excluding holidays and weekends .If family member is the legal representative, follow the same process as requested from the resident .
Resident #38
Review of an admission Record revealed Resident #38 was a female, with pertinent diagnoses which included Alzheimer's disease, arthritis, depression, and high blood pressure. Noted Family Member V was identified as Resident #38's responsible party.
Review of a Minimum Data Set (MDS) assessment, with a reference date of 2/10/23, revealed Resident #38 had severe cognitive impairment with behaviors that included inattention and disorganized thinking.
Review of a Care Plan for Resident #38 revealed the focus .Resident representative, (Family Member V), involved in care planning . initiated 12/13/21.
In an interview on 6/13/23 at 9:39 a.m., Family Member V reported they submitted a written request for Resident #38's medical records in March 2023. Family Member V reported these records have not been provided by the facility.
Review of an Authorization for Use or Disclosure of Protected Health Information form for Resident #38, revealed Family Member V submitted a written request for medical records on 3/24/23. The section For Office Use Only was incomplete, with no information noted as to whether or not the request was fulfilled.
In an interview on 6/14/23 at 2:26 p.m., Administrator A reported Family Member V submitted a request for Resident #38's medical records. Administrator A unable to provide documentation that this request was fulfilled in a timely manner prior to survey exit.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
Resident #6
Review of an admission Record revealed Resident #6 was a female with pertinent diagnoses which included bipolar disorder, PTSD (post-traumatic stress disorder), chronic pain syndrome, mild...
Read full inspector narrative →
Resident #6
Review of an admission Record revealed Resident #6 was a female with pertinent diagnoses which included bipolar disorder, PTSD (post-traumatic stress disorder), chronic pain syndrome, mild cognitive impairment, sleep disorder, muscle weakness, and diverticulitis (inflammation/infection in one or more small pouches of the digestive tract) of large intestine with perforation and abscess.
Review of Nurses' Notes for Resident #6, dated 1/22/2023 at 03:38 AM, revealed .Resident c/o (complained of) abdominal pain since shift started, On-call NP (nurse practitioner) ordered Simethicone x1 time, after giving it resident has emesis x1 undigested food noted. VS (vital signs) temp (temperature) 97.4, PR (pulse rate) 64, RR (respiratory rate) 18, BP (blood pressure) 116/70 noted P.Ox (pulse oximetry) 96% in room air. reposition resident after an hour, rechecked and still could not sleep, c/o lower back pain and uncomfortable in abdomen again, writer notified NP at 3:23 am and notified again resident, could not sleep, worry and nervous then request to go to hospital, order to send her to hospital, LG (Legal Guardian) (Name of Guardian) notified at 3:35am. DON (Director of Nursing) notified. called (Ambulance Service Name) .and transfer resident to (Hospital Name) at 3:52 AM .
Review of Resident #6's medical record revealed no documentation to indicate that a written transfer notice was provided upon her transfer to the hospital on 1/22/23.
Resident #23
Review of an admission Record revealed Resident #23 was a female with pertinent diagnoses which included leukemia of B-Cell, Alzheimer's disease, diabetes, adult failure to thrive, pain, stroke, and anemia.
Review of Nurses' Notes for Resident #23, dated 1/14/2023 at 03:43 AM, revealed .Lab called at approx (approximately 3:35 a.m.) with a critical hemoglobin of 5.7 for this (resident) NP (Nurse Practitioner) on call (Given name of NP) gave the order to send (resident) to the hospital .residents daughter/POA (power of attorney) was called and a message was left for her. I also called (resident's) substitute decision maker (resident's) granddaughter (Given name) who answered and requested (resident) be taken to (Hospital Name). (Ambulance Service Name) picked (resident) up at (3:45 a.m.) and assisted (resident) via stretcher to (Hospital Name). vitals remained wnl (within normal limits) though resident did appear pale. Resident was alert at baseline prior to leaving. DON .notified .
Review of Resident #23's medical record revealed no documentation to indicate that a written transfer notice was provided upon her transfer to the hospital on 1/14/23.
In an interview on 6/13/23 at 2:43 PM, Medical Records (MR) F reported there was a packet in a green folder kept at the nurse's station and this was given to the resident when they were taken out to the hospital. Nurses were to have them sign they received the documents (transfer notice and bed hold policy) and resident representatives were contacted to come and sign they received the transfer notice and bed hold information.
This citation pertains to Intake # MI00135264.
Based on interview and record review, the facility failed to notify the resident and/or the resident's representative in writing of the reason for a transfer to the hospital in 3 of 5 residents (Resident #38, #6, & #23) reviewed for transfer and discharge requirements, resulting in the potential for residents and/or their representatives to not be fully informed of the reason for a hospital transfer and their rights in regard to an appeal hearing.
Findings include:
Review of the policy/procedure Transfer and Discharge, dated 1/1/22, revealed .It is the policy of this facility to permit each resident to remain in the facility, and not transfer or discharge the resident from the facility except in limited situations when the health and safety of the individual or other residents are endangered .Emergency Transfers/Discharges - initiated by the facility for medical reasons, or for the immediate safety and welfare of a resident (nursing responsibilities unless otherwise specified) .Complete and send with the resident (or provide as soon as practicable) a Transfer Form which documents .Resident status, including baseline and current mental, behavioral and functional status and recent vital signs .Current diagnosis, allergies and reasons for transfer/discharge .The original copies of the transfer form and Advance Directive accompany the resident. Copies are retained in the medical record .Provide orientation for transfer or discharge to minimize anxiety and to ensure safe and orderly transfer or discharge, in a form and manner that the resident can understand .Provide transfer notice as soon as practicable to resident and representative .
Resident #38
Review of an admission Record revealed Resident #38 was a female, with pertinent diagnoses which included Alzheimer's disease, arthritis, depression, and high blood pressure. Noted Family Member V was identified as Resident #38's responsible party.
Review of a Minimum Data Set (MDS) assessment, with a reference date of 2/10/23, revealed Resident #38 had severe cognitive impairment with behaviors that included inattention and disorganized thinking.
Review of a Care Plan for Resident #38 revealed the focus .Resident representative, (Family Member V), involved in care planning . initiated 12/13/21.
Review of a Progress Note for Resident #38, dated 3/16/23 at 12:54 a.m., revealed .Lab notified facility of critical Sodium level of 164. (Nurse Practitioner) on call notified. Stated to call (Family Member V) to see what he wanted. Called (Family Member V) and explained situation and critical lab. (Family Member V) stated to send resident to (Hospital Name). (Ambulance Service) notified. Paramedic spoke with (Family Member V) after assessing resident. A copy of the DNR (Do-Not-Resuscitate Order) was sent with paramedic. Resident transferred to (Hospital Name). DON (Director of Nursing) notified .
Review of Resident #38's medical record revealed no documentation to indicate that a written transfer notice was provided to Resident #38's representative upon her transfer to the hospital on 3/16/23.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
Resident #6
Review of an admission Record revealed Resident #6 was a female with pertinent diagnoses which included bipolar disorder, PTSD (post-traumatic stress disorder), chronic pain syndrome, mild...
Read full inspector narrative →
Resident #6
Review of an admission Record revealed Resident #6 was a female with pertinent diagnoses which included bipolar disorder, PTSD (post-traumatic stress disorder), chronic pain syndrome, mild cognitive impairment, sleep disorder, muscle weakness, and diverticulitis (inflammation/infection in one or more small pouches of the digestive tract) of large intestine with perforation and abscess.
Review of Nurses' Notes for Resident #6, dated 1/22/2023 at 03:38 AM, revealed .Resident c/o (complained of) abdominal pain since shift started, On-call NP (nurse practitioner) ordered Simethicone x1 time, after giving it resident has emesis x1 undigested food noted. VS (vital signs) temp (temperature) 97.4, PR (pulse rate) 64, RR (respiratory rate) 18, BP (blood pressure) 116/70 noted P.Ox (pulse oximetry) 96% in room air. reposition resident after an hour, rechecked and still could not sleep, c/o lower back pain and uncomfortable in abdomen again, writer notified NP at 3:23 am and notified again resident, could not sleep, worry and nervous then request to go to hospital, order to send her to hospital, LG (Legal Guardian) (Name of Guardian) notified at 3:35am. DON (Director of Nursing) notified. called (Ambulance Service Name) .and transfer resident to (Hospital Name) at 3:52 AM .
Review of Resident #6's medical record revealed no documentation to indicate that a written bed-hold notice was provided to Resident #6's representative within 24 hours of her transfer to the hospital on 1/22/23. No signed/dated copy of the bed-hold notice information was noted in Resident #6's medical record.
In an interview on 6/14/23 at 10:44 AM, Administrator A reported the facility was not able to locate documentation that the bed-hold policy information was provided to Resident #6's representative after her transfer to the hospital on 1/22/23.
Resident #23
Review of an admission Record revealed Resident #23 was a female with pertinent diagnoses which included leukemia of B-Cell, Alzheimer's disease, diabetes, adult failure to thrive, pain, stroke, and anemia.
Review of Nurses' Notes for Resident #23, dated 1/14/2023 at 03:43 AM, revealed .Lab called at approx (approximately 3:35 a.m.) with a critical hemoglobin of 5.7 for this (resident) NP (Nurse Practitioner) on call (Given name of NP) gave the order to send (resident) to the hospital .residents daughter/POA (power of attorney) was called and a message was left for her. I also called (resident's) substitute decision maker (resident's) granddaughter (Given name) who answered and requested (resident) be taken to (Hospital Name). (Ambulance Service Name) picked (resident) up at (3:45 a.m.) and assisted (resident) via stretcher to (Hospital Name). vitals remained wnl (within normal limits) though resident did appear pale. Resident was alert at baseline prior to leaving. DON .notified .
Review of Resident #23's medical record revealed no documentation to indicate that a written bed-hold notice was provided to Resident #23's representative within 24 hours of her transfer to the hospital on 1/14/23. No signed/dated copy of the bed-hold notice information was noted in Resident #23's medical record.
In an interview on 6/14/23 at 10:44 AM, Administrator A reported the facility was not able to locate documentation that the bed-hold policy information was provided to Resident #23's representative after her transfer to the hospital on 1/14/23.
In an interview on 6/13/23 at 2:43 PM, Medical Records (MR) F reported there was a packet in a green folder kept at the nurse's station and this was given to the resident when they were taken out to the hospital. Nurses were to have them sign they received the documents (transfer notice and bed hold policy) and resident representatives were contacted to come and sign they received the transfer notice and bed hold information.
This citation pertains to Intake # MI00135264.
Based on interview and record review, the facility failed to provide written notification of the bed hold policy upon transfer to the hospital in 3 of 5 residents (Resident #38, #6, & #23) reviewed for transfer and discharge requirements, resulting in the potential for residents and/or their representatives to be unaware of their rights in regard to facility bed holds.
Findings include:
Review of the policy/procedure Bed Hold Notice Upon Transfer, dated 2/1/22, revealed .At the time of transfer for hospitalization or therapeutic leave, the facility will provide to the resident and/or the resident representative written notice which specifies the duration of the bed-hold policy and addresses information explaining the return of the resident to the next available bed .Before a resident is transferred to the hospital or goes on therapeutic leave, the facility will provide to the resident and/or the resident representative written information that specifies .The duration of the state bed-hold policy, if any, during which the resident is permitted to return and resume residence in the nursing facility .The reserve bed payment policy in the state plan policy, if any .The facility policies regarding bed-hold periods to include allowing a resident to return to the next available bed .Conditions upon which the resident would return to the facility .In the event of an emergency transfers of a resident, the facility will provide within 24 hours written notice of the facility's bed-hold policies, as stipulated in the State's plan .The facility will keep a signed and dated copy of the bed-hold notice information given to the resident and/or resident representative in the resident's file .
Resident #38
Review of an admission Record revealed Resident #38 was a female, with pertinent diagnoses which included Alzheimer's disease, arthritis, depression, and high blood pressure. Noted Family Member V was identified as Resident #38's responsible party.
Review of a Minimum Data Set (MDS) assessment, with a reference date of 2/10/23, revealed Resident #38 had severe cognitive impairment with behaviors that included inattention and disorganized thinking.
Review of a Care Plan for Resident #38 revealed the focus .Resident representative, (Family Member V), involved in care planning . initiated 12/13/21.
Review of a Progress Note for Resident #38, dated 3/16/23 at 12:54 a.m., revealed .Lab notified facility of critical Sodium level of 164. (Nurse Practitioner) on call notified. Stated to call (Family Member V) to see what he wanted. Called (Family Member V) and explained situation and critical lab. (Family Member V) stated to send resident to (Hospital Name). (Ambulance Service) notified. Paramedic spoke with (Family Member V) after assessing resident. A copy of the DNR (Do-Not-Resuscitate Order) was sent with paramedic. Resident transferred to (Hospital Name). DON (Director of Nursing) notified .
Review of Resident #38's medical record revealed no documentation to indicate that a written bed-hold notice was provided to Resident #38's representative within 24 hours of her transfer to the hospital on 3/16/23. No signed/dated copy of the bed-hold notice information was noted in Resident #38's medical record.
In an interview on 6/14/23 at 2:26 p.m., Administrator A reported the facility was not able to locate documentation that the bed-hold policy information was provided to Resident #38's representative after her transfer to the hospital on 3/16/23. Administrator A reported the bed-hold policy should be reviewed with the resident and/or resident representative upon transfer to the hospital. Administrator A reported a copy of the signed bed-hold notice should be uploaded to the medical record.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to Intake # MI00130822.
Based on observation, interview, and record review the facility failed to develop...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to Intake # MI00130822.
Based on observation, interview, and record review the facility failed to develop and implement person centered care plans for 3 of 12 residents (Resident #15, Resident #27 and Resident #21) reviewed for care plans, resulting in the potential for staff to not know how to care for resident conditions or follow resident care interventions.
Findings include:
Review of the Long-Term Care Facility Resident Assessment Instrument 3.0 User's Manual, v1.16, Chapter 4: Care Area Assessment (CAA) Process and Care Planning, revealed .the comprehensive care plan is an interdisciplinary communication tool. It must include measurable objectives and time frames and must describe the services that are to be furnished to attain or maintain the resident's highest practicable physical, mental, and psychosocial well-being.
Resident #15
Review of an admission Record dated 9/29/17 revealed Resident #15 was admitted to the facility with the following pertinent diagnoses: Alzheimer's Disease (disease characterized by progressive mental deterioration), muscle weakness, cognitive communication deficit, other symptoms and signs involving cognitive functions and awareness, Type 2 Diabetes Mellitus (chronic disease characterized elevated blood sugar levels which leads to damage to blood vessels), Major Depressive Disorder and Osteoarthritis (degeneration of joint cartilage and bone causing stiffness and pain).
Review of a Minimum Data Set (MDS) assessment dated [DATE], Section C revealed Resident #15 was severely impaired (never/rarely made decisions) for daily decision making, continuously had difficulty focusing her attention, and continuously presented with disorganized thinking. Section G of the MDS revealed Resident #15 was dependent for bed mobility (how the Resident moves to and from lying position, turns side to side, and positions body while in bed or alternate sleep furniture). Section J revealed Resident #15 had not displayed indicators of pain in the previous 5 days leading up to the time of the assessment. Section M revealed Resident #15 had no pressure ulcers/injuries at the time of assessment but was at risk for developing pressure ulcers.
Review of a wound assessment dated [DATE] revealed Resident #15 had a stage 2 pressure ulcer on the right heel. The pressure ulcer was labeled as status new-age unknown.
Review of a Care Plan for Resident #15, dated 6/12/23 revealed focus/goal/interventions that stated: The Resident has the actual impairment to skin integrity right heel r/t (related to) fragile skin-pressure, Goal: Resident will develop intact skin .Interventions: float heels .air pressure mattress .yellow dot program: turn and reposition every 2 hours (initiated on 4/17/21) .
Review of task documentation labeled Turn and Reposition per Care Plan dated 5/15/23-6/13/23 revealed Resident #15 had been repositioned every 2 hours during 0 of 30 days listed.
During an observation on 6/13/23 at 10:31 a.m., Resident #15 was sleeping in bed, lying on her back.
During an observation on 6/13/23 at 12:29 p.m., Resident #15 was sleeping in bed, lying on her back.
During an observation and interview on 6/13/23 at 12:54 p.m., Licensed Practical Nurse (LPN) G completed wound care to Resident #15's right heel. LPN G reported the pressure ulcer wound was unstageable because it was scabbed over. Resident #15 stated It's burning while LPN G cleaned the wound. LPN G confirmed that Resident #15 was in the yellow dot program and should be repositioned every two hours. Resident #15 remained on her back, lying in bed during and after the wound care.
During an observation on 6/13/23 at 1:39 p.m., Resident #15 was awake, lying on her back when Certified Nursing Assistant (CENA) D entered the room and provided incontinence care. Following the care, Resident #15 was observed still lying on her back in bed.
During an observation on 6/13/23 at 2:30 p.m., Resident #15 was lying on her back in bed, talking to self.
During an observation on 6/13/23 at 3:33 p.m., Resident #15 was lying on her back in bed, talking loudly with an urgent tone, and stated Ok, right here, right here!.
In an interview on 6/14/23 at 8:39 a.m., CENA Q reported Resident #15 was on the yellow dot program which indicated the resident should be turned/repositioned every two hours to protect her skin integrity. CENA Q reported staff knew when a resident is on that program because a yellow dot is placed on their name plaque by their room door.
During an observation on 6/14/23 at 8:44 a.m., a yellow dot sticker was present by Resident #15's name plaque outside her room.
During an observation on 6/14/23 at 11:06 a.m., Resident #15 was awake, sitting up in her wheelchair near the nurse's station.
During an observation on 6/14/23 at 12:21 p.m., Resident #15 was seated in her wheelchair at a table in the dining room, awake and talking quietly to herself.
During an observation on 6/14/23 at 1:22 p.m., Resident #15 was awake, remained sitting up in her wheelchair, was now in her room alone, yelling Help me, help me, come here. Resident #15 rubbed her right thigh and stated, Oh God, help me, facial grimace and furrowed eyebrows noted at that time. Resident #15 attempted to change the position of her right leg but could not do so.
In an interview with Director of Nursing (DON) B on 6/14/23 at 1:38 p.m., it was revealed that all interventions for prevention and treatment of pressure ulcers should be person centered and carried out by staff as outlined in the plan of care, including repositioning of residents who are dependent for mobility. DON B agreed that Resident #15 should be repositioned every two hours as outlined in her plan of care.
Resident #27
Review of an admission Record dated 1/28/23 revealed Resident #27 was admitted to the facility with the following pertinent diagnoses: Senile Degeneration of the Brain (loss of intellectual ability associated with old age), Depression, Unspecified Dementia (progressive loss of intellectual functioning), Adult Failure to Thrive (state of decline that is multifactorial).
Review of a Minimum Data Set (MDS) assessment for Resident #27, dated 4/13/23, revealed a Brief Interview for Mental Status (BIMS) score of 9 indicating the Resident had a moderate level of cognitive impairment (difficulty with problem solving, remembering details, learning new things). Section V of the MDS indicated Resident #27 had a 3-point decrease in from a BIMS completed on 2/2/23. The MDS also indicated Residents #27 had continuous presence of disorganized thinking, was dependent for transfers (moving from one surface to another) and had a life expectancy of 6 months or less.
Review of a Care Plan for Resident #27, dated 4/24/23, revealed focus/goal/ interventions as follows: Focus: Resident exhibits behaviors r/t (related to) dementia .emotional discomfort .Goal: will have no increase in symptoms .Interventions: administer medications .assist Resident to develop more appropriate methods of coping .
During an observation on 6/12/23 at 10:13 a.m., Resident #27 was lying in his bed and could be heard from the nurse's station, approximately thirty feet from his doorway, yelling Hello, hello, hello.
During an observation on 6/12/23 at 2:39 p.m., Resident #27 was sitting in a recliner chair in his room yelling Dad .Dad .[NAME] .hello, hello?
During an observation on 6/13/23 at 3:32 p.m., Resident #27 was lying in his bed yelling Hello, hello ! and could be heard from the hallway, approximately twenty feet from his doorway.
During an observation on 6/14/23 at 11:06 a.m., Resident #27 was sitting in a recliner chair near the nurse's station, when greeted Resident #27 stated Everybody is out and about and it's a nice day. Resident #27 appeared calm, smiled during the interaction.
In an interview on 6/14/23 at 8:39 a.m. Certified Nursing Assistant (CENA) Q reported Resident #27 called out frequently. CENA Q described Resident #27 as a very social person and reported the staff that knew him well help reduce his behaviors by bringing him to the nurse's station area where he can visit with others, giving him his favorite drink (vegetable juice), helping him call his wife and assisting him to the Movies & Popcorn activity. CENA Q reported she learned this information about Resident #27 by interacting with him. These interventions were not present in Resident #27's care plan.
In an interview on 6/14/23 at 9:07 a.m., Activities Director (AD) S reported that Resident #27 sometimes appeared to enjoy group activities. AD S reported Resident #27 enjoyed chatting with others, people watching and reminiscing about owning a restaurant chain. AD S also reported Resident #27 enjoyed drinking vegetable juice. These interventions were not reflected in Resident #27's care plan.
Resident #21
Review of an admission Record revealed Resident #21 was a male with pertinent diagnoses which included stroke, fluency disorder following a stroke, sleep disorder, repeated falls, muscle weakness, reduced mobility, diabetes, anxiety, cognitive communication deficit, chronic pain, senile degeneration of brain, epilepsy, mood disorder, fracture of right acetabulum, fracture of upper end of right humerus, and lower urinary tract symptoms.
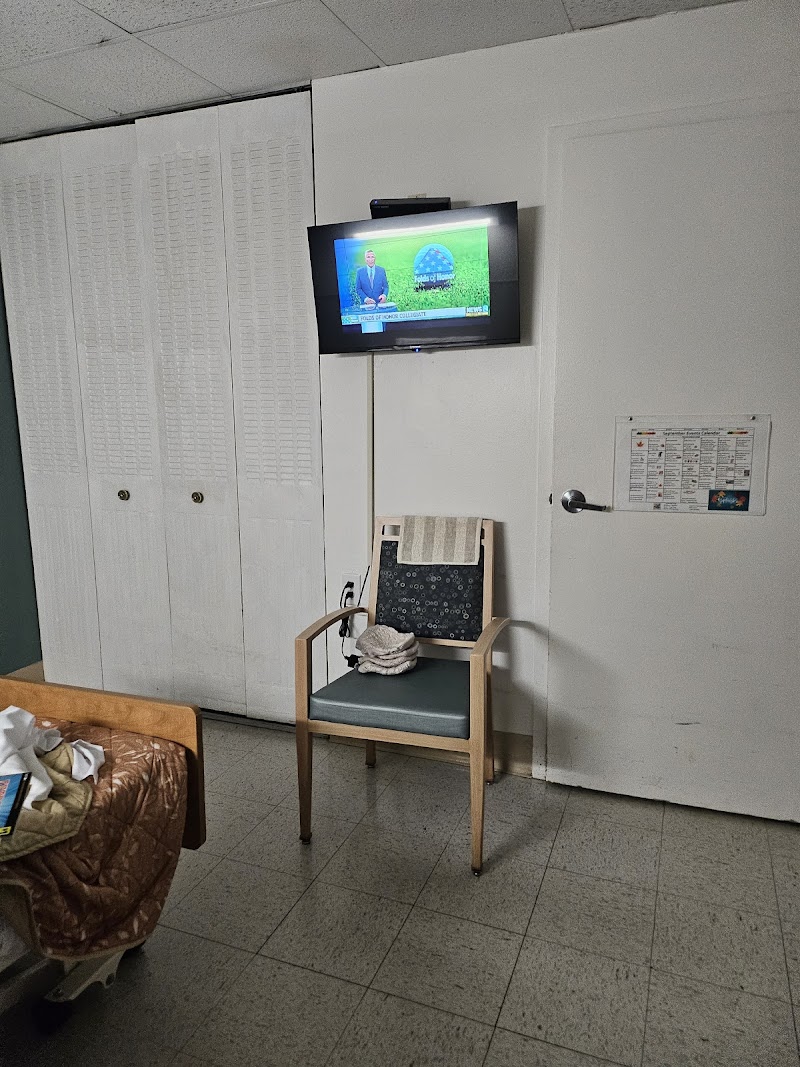
Review of a current Care Plan for Resident #21, revised on 3/20/23, revealed the focus .Resident structures his leisure time independently thru own independent activities. Strong preference to stay in his room; can be difficult to engage in activity groups. Prefers nicknames . with the interventions .CD player with Cuban music, enjoys snacks delivered to room .Favorite activities include snacks delivered to his room (cookies and coffee and his ethnic snacks), TV, social with others often initiating conversations independently. *ordered him Cuban CDs; also provided resident with CD player. Staff offer room visits as tolerated .
Review of a current Care Plan for Resident #21, revised on 3/23/23, revealed the focus .The resident is a risk for falls related to, history of falls, reduced mobility, abnormalities of gait and mobility, muscle weakness, poor communication/comprehension, and dementia unaware of safety needs . with the intervention .Broda to be locked at bedside at all times .Recliner to be placed in the near vicinity of bed for easy access .Keep bed in low position .
In an observation on 06/12/23 at 10:51 AM, Resident #21 was observed lying in his bed, facing the window in the room. Resident #21's bed was not in the low position, Broda chair was not locked at the bedside, and recliner was placed approximately 6 feet away from the bed. If the resident were to self-ambulate, it was not placed for easy access. Noted no Cuban music playing, and the TV was not on. CD player was located on a stand next to the recliner.
In an observation on 06/12/23 at 10:55 AM, Licensed Practical Nurse (LPN) G and Certified Nursing Assistant (CNA) O did not check in on Resident #21 in his room when leaving Resident #23's room. Noted no Cuban music playing, and the TV was not on. CD player was located on a stand next to the recliner.
In an observation on 06/13/23 at 09:44 AM, Resident #21 was observed seated in his bed, bed was not in the low position, and the head of the bed was approximately 80 degrees. Resident #21 was noted to not have on socks or shoes. Resident #21's Broda chair was placed along the wall over by the entry way to the room not locked at the bedside. Resident #21's recliner was not placed for easy access from the bed if resident were to attempt to self-ambulate to the chair. It was placed approximately 6 feet away from bed. LPN G offered Resident #21 his water from his rolling bedside table, which was not in his reach, and he drank the full cup of water. Noted no Cuban music playing, and the TV was not on. CD player was located on a stand next to the recliner.
In an observation on 06/13/23 at 01:51 PM, Resident #21 was in his room yelling, hollering out. Note: No staff proceeded to provide interventions. Resident #21's bed was not in the low position, Broda chair was not locked at the bedside, and recliner was placed approximately 6 feet away from the bed. If the resident were to self-ambulate, it was not placed for easy access. Noted no Cuban music playing, and the TV was not on. CD player was located on a stand next to the recliner.
In an interview on 06/14/23 at 10:14 AM, CNA D reported the CNA's have access to the [NAME] with the resident's care plan interventions via the computer or tablets. CNA D reported she would go to the EMR (electronic medical record) if she was unsure what interventions the resident required for behaviors, ADL (activities of daily living) care/preferences, or other needs for the resident.
In an interview on 06/13/23 at 02:18 PM, Director of Nursing (DON) B reported the expectation would be the nursing staff would assist with the residents' participation in activities, including to go to residents and promote participation in activities. DON B reported she depends on the unit managers and floor nurses to ensure the staff were observing what occurred on the units, by their daily notes, 24-hour reports, and review of documentation would be how she would ensure the care plan interventions were implemented. DON B reported the care plan should have individualized interventions to address residents' behaviors and with dementia care. DON B reported staff are to supervise the residents to ensure those who wander have time to rest, or were safe during ambulation.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to Intake # MI00130822.
Based on observation, interview, and record review the facility failed to prevent...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** This citation pertains to Intake # MI00130822.
Based on observation, interview, and record review the facility failed to prevent the development of an avoidable pressure ulcer for 1 of 12 sampled residents (Resident #15) resulting in the development of a pressure ulcer and the potential for delayed wound healing, pain, infection and overall deterioration in health status.
Findings include:
Review of a facility policy titled Pressure Injury Prevent and Management, dated 1/2/22, revealed the facility definition of an avoidable pressure ulcer as: Avoidable means that the resident developed a pressure ulcer/injury and that the facility did not do one or more of the following: evaluate the resident's clinical condition and risk factors; define and implement interventions that are consistent with resident needs, resident goals, and professional standards of practice; monitor and evaluate the impact of the interventions; or revise the interventions as appropriate. Section 4 of the policy (Interventions for Prevention and to Promote Healing) states: Evidence-based interventions for prevention will be implemented for all residents who are assessed at risk or who have a pressure injury present. Basic or routine care interventions could include, but are not limited to: i Redistribute pressure (such as repositioning .)
Resident #15
Review of an admission Record dated 9/29/17 revealed Resident #15 was admitted to the facility with the following pertinent diagnoses: Alzheimer's Disease (disease characterized by progressive mental deterioration), muscle weakness, cognitive communication deficit, other symptoms and signs involving cognitive functions and awareness, Type 2 Diabetes Mellitus (chronic disease characterized elevated blood sugar levels which leads to damage to blood vessels), Osteoarthritis (deterioration of cartilage and bone resulting in stiffness and decreased mobility) and Major Depressive Disorder.
Review of a Minimum Data Set (MDS) assessment dated [DATE], section C revealed Resident #15 was severely impaired (never/rarely made decisions) for daily decision making, continuously had difficulty focusing her attention, and continuously presented with disorganized thinking. Section E of the MDS revealed Resident #15 did not reject care. Section G revealed Resident #15 was dependent for bed mobility (how the Resident moves to and from lying position, turns side to side, and positions body while in bed or alternate sleep furniture). Section J revealed Resident #15 had not displayed indicators of pain in the previous 5 days leading up to the time of the assessment. Section M revealed Resident #15 had no pressure ulcers/injuries at the time of assessment but was at risk for developing pressure ulcers.
Review of a wound assessment dated [DATE] revealed Resident #15 had a stage 2 pressure ulcer on the right heel. The pressure ulcer was labeled as status new-age unknown.
Review of a wound assessment dated [DATE] revealed Resident #15's wound to the right heel was labeled In-House Acquired.
Review of a Care Plan for Resident #15, dated 6/12/23, revealed focus/goal/interventions that stated: The Resident has the actual impairment to skin integrity right heel r/t (related to) fragile skin-pressure, Goal: Resident will develop intact skin .Interventions: float heels .air pressure mattress .yellow dot program: turn and reposition every 2 hours (initiated on 4/17/21) .
Review of task documentation labeled Turn and Reposition per Care Plan dated 5/15/23-6/13/23 revealed Resident #15 had been repositioned every 2 hours 0 of 30 days listed.
During an observation on 6/13/23 at 10:31 a.m., Resident #15 was sleeping in bed, lying on her back.
During an observation on 6/13/23 at 12:29 p.m., Resident #15 was sleeping in bed, lying on her back.
During an observation and interview on 6/13/23 at 12:54 p.m., Licensed Practical Nurse (LPN) G completed wound care to Resident #15's right heel. LPN G reported the pressure ulcer wound was unstageable because it was scabbed over. Resident #15 stated It's burning while LPN G cleaned the wound. LPN G confirmed that Resident #15 was in the yellow dot program and should be repositioned every two hours. Resident #15 remained on her back, lying in bed after the wound care.
During an observation on 6/13/23 at 1:39 p.m., Resident #15 was awake, lying on her back when Certified Nursing Assistant (CENA) D entered the room and provided incontinence care. Following the care, Resident #15 was observed still lying on her back in bed.
During an observation on 6/13/23 at 2:30 p.m., Resident #15 was lying on her back in bed, talking to self.
During an observation on 6/13/23 at 3:33 p.m., Resident #15 was lying on her back in bed, talking loudly with an urgent tone, and stated Ok, right here, right here!.
In an interview on 6/14/23 at 8:39 a.m., CENA Q reported Resident #15 was on the yellow dot program which indicated the Resident should be turned/repositioned every two hours to protect her skin integrity. CENA Q reported staff knew when a resident is on that program because a yellow dot is placed on their name plaque by their room door.
During an observation on 6/14/23 at 8:44 a.m., a yellow dot sticker was present by Resident #15's name plaque outside her room.
During an observation on 6/14/23 at 11:06 a.m., Resident #15 was awake, sitting up in her wheelchair, sitting near the nurse's station.
During an observation on 6/14/23 at 12:21 p.m., Resident #15 was seated in her wheelchair at a table in the dining room, awake and talking quietly to herself.
During an observation on 6/14/23 at 1:22 p.m., Resident #15 was awake, remained sitting up in her wheelchair, was now in her room alone, yelling Help me, help me, come here. Resident #15 rubbed her right thigh and stated, Oh God, help me, facial grimace and furrowed eyebrows noted at that time. Resident #15 attempted to change the position of her right leg but could not do so.
In an interview with Director of Nursing (DON) B on 6/14/23 at 1:38 p.m., it was revealed that all interventions for prevention and treatment of pressure ulcers should be person centered and carried out by staff as outlined in the plan of care, including repositioning of residents who are dependent for mobility. DON B agreed that Resident #15 should be repositioned every two hours as outlined in her plan of care.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide supervision according to the standards of car...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide supervision according to the standards of care and consistently implement adequate and effective interventions to prevent further falls in 1 of 7 residents (Resident #22) reviewed for safety, resulting in the potential for wandering into other residents' rooms, accidents/hazards with the potential for injury and/or resident to resident altercations.
Findings include:
.One of the biggest safety challenges is preventing falls .3 of every 4 nursing center residents fall each year .Nursing staff must have the knowledge and skills to prevent injury from falls .Previous falls, diminished strength, gait and balance impairments, medications, Alzheimer's disease or dementia, vision impairment and environmental risk factors .Staffing and organization of care. Inadequate staffing may leave residents who are likely to fall without proper supervision . https://www.ahrq.gov/patient-safety/settings/long-term-care/resource/facilities/ltc/mod3sess3.html
Resident #22
Review of an admission Record revealed Resident #22 was a male with pertinent diagnoses which included Alzheimer's disease, early onset, muscle weakness, reduced mobility, cognitive communication deficit, psychotic disorder with delusions, unsteadiness on feet, and abnormalities of gait and mobility.
Review of a Minimum Data Set (MDS) assessment for Resident #22, dated 3/14/23, revealed .Documented behaviors included physical behaviors towards staff and also wandering with attempts to leave thru doors .Physical towards staff during care. No patterns with wandering as it occurs throughout the day .Early onset dementia with depression and anxiety; see medical record .Agitation with care .Dx (diagnosis) of early onset Alzheimer's .Section E: Behavior: Wandering impact .A. Does the wandering place the resident at significant risk of getting to a potentially dangerous place .Yes .E1100. Change in Behavior of Other Symptoms .How does the resident's current behavior status, care rejection, or wandering compare to prior assessment? .2. Worse . Section F: Customary Routine and Activities: Resident #22 finds it important to listen to music he likes, be around animals, do things with groups of people, do favorite activities, and go outside.
Review of a current Care Plan for Resident #22, revised on 5/11/23, revealed the focus .(Resident #22) is at risk for falls related to Alzheimer's, Dementia, Seizures, unsteadiness on feet, abnormalities of gait and mobility, history of falls . with the intervention .Staff to encourage resident to not sit on chairs/walker improperly. Redirect from this (12/15/2022) .Ensure walkway is free of clutter leaving no obstruction and well lit (5/11/2023) .
Review of a SOC (Standards of Care) -Fall assessment for Resident #22, dated 12/15/22 at 9:36 AM, revealed .Date and time of fall: 12/13/22 at 1:45 PM .Resident tried to sit on a different resident's walker and fell to a sitting position. Resident got himself back up off the floor with no complaints of pain or visible injury .Resident continues to be a risk for fall due to his cognitive status and lack of safety awareness .
Review of a SOC - Fall assessment for Resident #22, dated 12/27/22 at 9:24 AM, revealed .Date and time of fall: 12/23/22 at 2:15 PM .Staff observed resident sitting on floor in front of recliner in peer's room. Unable to verbalize what happened but appears as he attempted to sit in the chair and ended up on the floor .Review of ortho (orthostatic) BP's (blood pressures) does not indicate a concern. Goal will be to prevent injury as resident has significant cognitive impairment, no safety awareness and is independently ambulatory and wanders .Goal to ensure resident is safe/prevent injury .
Review of Nurses' Notes for Resident #22, dated 12/23/22 at 6:04 PM, revealed .Resident was previously in other residents room in her bed, staff were assisting female resident back to her room when they observed this resident laying in her bed, they assisted male resident out of her bed as she was yelling at him to get out of her room, male resident started walking down hallway not understanding the situation, short while later female resident came out into hallway grabbed residents arms and was hold them behind him when he was trying to get away he turned around and with a closed fist made contact with female resident's chest . Note: Requested incidents to include this time frame and no incident report provided for this incident.
Review of a SOC - Fall assessment for Resident #22, dated 2/27/23 at 10:50 AM, revealed .Date and time of fall: 2/26/23 at 2:46 PM .Resident was observed in another resident's room sitting on his bottom in front of her recliner. Appearing as though he slid from the recliner to hit (sic) bottom. No apparent injury noted; neuro and vitals WNL (within normal limits) for resident. When resident sits in chairs he is noted to slid (sic) down and is slouching .
Review of a Fall - Initial assessment for Resident #22, dated 2/26/23 at 2:55 PM, revealed .What was resident doing prior to fall? Resident was walking the hall within minutes of being found on the floor .
Requested incident reports for Resident #22 and did not receive for this incident dated 2/26/23.
Review of Nurses' Notes for Resident #22, dated 5/4/223 at 9:13 PM, revealed .Staff called this nurse to memory care unit as they observed blood coming from scalp nearest his forehead. The resident was not In distress, no behaviors were observed. The resident was pacing the hall, which was free of clutter and debris. This writer applied pressure to abrasion, to stop bleeding. Cleaned blood from forehead and hair with warm washcloths. Assessed area. No openings observed. Left OTA (open to air), as a bandage would not adhere due to location of injury. DON (Director of Nursing) notified .
Requested incident reports for Resident #22 and did not receive for this incident dated 5/4/23.
Review of Nurses' Notes for Resident #22, dated 5/6/2023 at 05:57 AM, revealed .resident found on floor in room. no apparent injuries noted .
Review of a SOC Fall assessment for Resident #22, dated 5/6/23, revealed .Resident was found on the floor in his bedroom on his bottom near his bed and the roommate's Broda chair in the early morning hours as he was getting up for the day on his own accord .He is unable to tell the staff what happened and upon assessment there were no injuries observed, vital signs were within normal limits .(Resident #22) has significant cognitive decline and displays no safety awareness. He walks up and down the corridor throughout the day which seems to bring him contentment .His most recent falls have occurred r/t (related to) trying to sit on furniture not on the seat, but the arm of the chair .Staff thought related to the size and positioning of the Broda chair that it may have obstructed the pathway and (Resident #22) typically walks with his head down and may have been unaware that the Broda was blocking his path. He had also just roused from sleep and may have been drowsy adding to the incident .Roommate's Broda chair to be placed outside of room at night to allow more functional space for resident care .
Review of a Fall Initial assessment for Resident #22, dated 5/6/23, revealed .Describe other intervention(s): Remove resident's roommate's w/c (wheelchair) when not in use. Resident's w/c (wheelchair) belongs to is bedridden and only gets up with hoyer (dependent lift) .
Review of a NP/PA (Nurse Practitioner/Physician Assistant) Progress Note for Resident #22, dated 5/9/2023 at 09:50 AM, revealed .being seen for follow up after the nursing staff found pt (patient) on the floor on 5/6/23- there appeared to be no noted injuries at that time-pt appears to be at his baseline today- he is up and walking the memory care unit without any problems-pt walks in the hallways without any type of assistive device- he does walk with his head bent down .pt speaks very few words at this time .Integumentary: Warm, Pink, pt does have a small scab on the left top of his scalp just back in his hair line- there area is closed .Documentation reviewed: Case discussed with: spoke with the nursing staff on the unit today .Condition: Guarded .Impression and Plan .Diagnosis: Fall at nursing home .pt has very poor safety awareness d/t (due to) his advanced dementia-when pt is up and walking he always appears to have good shoe support-no injuries noted from the fall-nursing staff to continue to monitor and report changes .
Requested incident reports for Resident #22 and did not receive for this incident dated 5/6/23.
Review of an Incident Report for Resident #22, dated 5/26/23 at 1:15 PM, revealed .While standing near (memory care unit) entrance door RN (Registered Nurse) heard what sounded like a chair scooting across the floor and someone yelling whoa. Upon entering the (memory care unit) the resident was sitting in the day room, on the floor, in front of the lounge chair .
Review of a NP/PA Progress Note for Resident #22, dated 6/1/23 at 12:47 PM, revealed .seen per the request of the staff at the nursing home that pt appears more agitated and he is not sleeping well at night .Pt has advanced dementia and at this time is unable to make his needs known for the most part .Pt walks in the hallways without any type of assistive device-he does walk with his head bent down .I suspect there are other pt's on the memory care unit that might get pt a bit worked up also .Nursing staff will continue to monitor and report changes .
In an observation on 06/12/23 at 10:39 AM, Resident #22 was observed in the hallway on the memory care unit walking from one end to the other end. Pacing back and forth down the hallway.
In an observation on 06/12/23 at 11:25 AM, Resident #22's roommate's Broda chair was observed to be placed on Resident #22's side of the room blocking his path for safe ambulation in his room.
In an observation on 06/12/23 at 11:27 AM, Resident #22 went into Resident #21's room exited and entered Resident #12's room who was lying in her bed. Resident #12 was looking at Resident #22 as he stood over her at the right side of the bed where her upper body was. Resident #22 was observed to be side stepping down the right side of Resident #12's bed, to the foot of her bed, along the foot board of her bed, then along the wall and to far right corner of her room.
In an observation on 06/12/23 at 11:29 AM, Resident #22 exited Resident #12's room and went to Resident #21's room and proceeded to seat himself sideways in the resident's recliner.
In an observation on 06/12/23 at 11:32 AM, Resident #22 exited Resident #22's room and stood in the doorway of Resident #12's room. Resident #22 proceeded to turn around and then stood in the doorway of Resident #21's room, then leaned on the door frame and looked down the hallway. No staff were present on the hallway to intervene or determine if Resident #22 was tired and needed to rest.
In an observation on 06/12/23 at 11:33 AM, Resident #22 proceeded to enter Resident #12's room and stood at the foot of her bed. Resident #12 was holding up her baby doll and showing it to Resident #22. Resident #22 exited her room and then proceeded back to Resident #21's room. No staff came to intervene during his time entering other resident's rooms. No staff were observed on the hallway.
In an observation on 06/12/23 at 11:34 AM, Resident #22 walked up to Resident #21's bed while he was lying in it. There was a fall mat on the left side of the bed, the right side was against the wall. Resident #22 attempted to step up on the fall mat to walk along the side of Resident #21's bed. Resident #22 was unable to step on the mat and walked across the corner of it over to the recliner in Resident #21's room then proceeded out of the room and ambulated down the hallway towards the main entrance of the unit. Resident #12 moved herself to the side of the bed, still in a lying position, leaned over and grabbed the wheelchair which was about 3 feet away and pulled it to the right side of her bed. No staff came to intervene during Resident #22's time entering other resident's rooms. No staff were observed on the hallway.
In an observation on 06/12/23 at 11:36 AM, Resident #22 proceeded to enter his room then exited and proceeded to stand in the doorway of Resident #12's room. Resident #12 was touching the wheelchair and Resident #22 walked over to the foot of her bed, and she pushed the wheelchair away from the side of her bed out of her reach all the while she was looking at Resident #22 as he stood in the far-right corner of her room. Resident #22 exited her room and stood outside of Resident #21's room and then proceeded to ambulate down the hallway. No staff came to intervene during Resident #22's time entering other resident's rooms. No staff were observed on the hallway.
In an observation on 06/12/23 at 02:32 PM, Resident #22 was standing just inside the doorway to Resident #21's room by his chair by the door. Resident #21 was on his side facing away from the wall and he had his head covered. Resident #22 was walking towards Resident #21's bed and was positioned at the head of his bed, looked down at the fall mat. Resident #22 waved his hand in the air, made some nonsensical statements, and proceeded to step on the fall mat with his right foot, it moved some as he was unable to raise his foot high enough to step on it, proceeded to walk over the corner of the fall mat while he mumbled and stepped towards the recliner and sat down in Resident #21's recliner. No staff intervened while Resident #22 had entered another resident's room.
In an observation on 06/12/23 at 02:38 PM, Resident #22 was observed seated on Resident #21's recliner sideways on his left hip, hanging on to the table with his right hand while mumbling to himself. Resident #22 proceeded to remove his hand from the table but did not sit back in the recliner with his back against the back of the chair. No staff intervened while Resident #22 had entered another resident's room.
In an interview on 06/12/23 at 02:48 PM, Registered Nurse (RN) C reported Resident #22 liked recliners and he would go to the other residents' rooms with recliners and would sit in them.
In an observation on 06/13/23 at 01:41 PM, Resident #22 exited the dining/day room and entered Resident #8's room. Resident #22 stood at the foot of her bed, walked along the side of the bed, went to the other side of the room and was touching the wall, looking at items on her rolling table, exited to her room, came over to this writer, looked at the computer, made a nonsensical statement, and turned and headed down the hallway.
In an observation on 06/13/23 at 01:53 PM, Resident #22 was observed standing at the back door looking out the back door windows. Resident #22 was walking back down the hallway. Resident #26 repeatedly stated Resident #22 stinks and he was dirty as he passed her in the hallway. As he proceeded back down the hallway, Resident #26 was yelling at him to go home, he wasn't coming with them. Resident #22 walked past her with his head down and he tensed up his body inward as he passed her. Resident #26 reached out to grab him and she stopped as she saw this writer looking at her and continued yelling at him and continued down the hallway with her rant about Resident #22. Note: No staff came to the hallway to observe or intervene in this situation.
In an interview on 06/13/23 at 01:58 PM, Licensed Practical Nurse (LPN) P reported the facility was aware Resident #22 was going into other resident's room and some residents requested to have the stop sign banner placed over their door entry way to prevent him from entering their room. LPN P reported interventions for him were to check on him frequently when he was wandering.
In an interview on 06/14/23 at 09:09 AM, Staff Development (SD) I reported if a CNA observed a behavior, they could review Alert charting, or create a Stop and Watch to document in the record. SD I reported if there was verbal aggression between two residents the staff would introduce redirection and separation of the residents. SD I reported staff could try different interventions to interrupt the behavior or stop the behavior. When presented with the fact Resident #22 liked recliners, SD I expressed questioning of why the facility had not tried a recliner in the resident's room to prevent the wandering. SD I reported this was the resident's home and the facility should do things to make it a good place to live and .do anything to make it comfortable for our residents .
In an interview on 06/14/23 at 01:19 PM, Certified Nursing Assistant (CNA) Z reported the CNA's review the [NAME] in the electronic medical record (EMR) for what interventions were in place for the resident. They would also review the alert charting in the EMR which would alert them to changes in the resident's condition, observations of residents to be aware of, etc.
In an interview on 06/13/23 at 02:18 PM, Director of Nursing (DON) B reported the expectation would be the nursing staff would assist with the residents' participation in activities, including to go to residents and promote participation in activities. DON B reported she depends on the unit managers and floor nurses to ensure the staff were observing what occurred on the units, but their daily notes, 24-hour reports, and review of documentation would be how she would ensure the care plan interventions were implemented. DON B reported the care plan should have individualized interventions to address residents' behaviors and with dementia care. DON B reported staff are to supervise the residents to ensure those who wander are rested or were safe during ambulation.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0744
(Tag F0744)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Review of The Needs of Older People with Dementia in Residential Care, Woods & [NAME] (2006), published in the International Jou...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Review of The Needs of Older People with Dementia in Residential Care, Woods & [NAME] (2006), published in the International Journal of Geriatric Psychiatry revealed Determining which activities have high degree of meaningfulness can aide recreation staff in creating programs more likely to promote health and wellness for persons with dementia.
Review of Activity Involvement and Quality of Life of People at Different Stages of Dementia in Long Term Care Facilities, [NAME] & Twist (2015), published in Aging Mental Health, revealed Despite a Resident's cognitive status, their activity involvement was significantly related to better scores on care relationships, positive affect, restless tense behavior, social relations and having something to do.
Resident #15
Review of an admission Record dated 9/29/17 revealed Resident #15 was admitted to the facility with the following pertinent diagnoses: Alzheimer's Disease (disease characterized by progressive mental deterioration), muscle weakness, cognitive communication deficit, other symptoms and signs involving cognitive functions and awareness, and Major Depressive Disorder.
Review of a Minimum Data Set (MDS) assessment dated [DATE], Section C revealed Resident #15 was severely impaired (never/rarely made decisions) for daily decision making, continuously had difficulty focusing her attention, and continuously presented with disorganized thinking. Section D revealed Resident #15 had trouble concentrating on things, such as reading the newspaper or watching television. Section E revealed Resident #15 experienced hallucinations (perceptual experiences in the absence of real external sensory stimuli). Section F identified the following activities were assessed as being very important to Resident #15: listening to music, doing things with groups of people, doing favorite activities, and participating in religious services. Section G indicated Resident #15 was dependent for mobility in her wheelchair and could not walk.
Review of an Activities Evaluation of Resident #15 dated 4/26/23, revealed the resident preferred to be addressed by a nickname, was born in (State Name), spoke Italian and English and described her former occupation as taking care of my kids. Resident #15 preferred to be up in the morning for breakfast then nap between meals if tired. Family members provided the information for the assessment and described Resident #15 as a social person who was usually cheerful.
In an interview with Activities Director (AD) S on 6/15/23 at 9:14 a.m., revealed activity programming for residents with dementia should include a predictable routine each day with activities tailored to their interests and abilities. AD S also reported that an important part of activity programming to meet the needs of residents with dementia was providing regular sensory stimulation activities. AD S reported two activity calendars were developed each month at the facility. One activity calendar was tailored to the residents in memory care, and the other calendar outlined activities for the residents in the main area of the building, where Resident #15 resides. Residents were not brought from the main area of the building to pursue activities in the memory care program.
Review of the Activity Calendars (for the area of the building in which Resident #15 resides) dated 4/23-6/23 revealed sensory stimulation was scheduled one time per week and 1:1 room visits were scheduled twice a week.
Review of a Planned Activity attendance record for Resident #15 dated 5/15-6/13/23 revealed Resident #15 attended a total of 5 group activities in a month (a social activity, one table game, one session of sensory stimulation, one gardening activity, a religious activity and had in-room visits). Resident #15's response to activity involvement, modifications made to accommodate the resident's abilities/needs, progress toward goals, alleviation of distress was not documented.
Review of a Care Plan for Resident #15, dated 4/26/23, revealed conflicting information about the name resident preferred to be called, her preference to be up in the morning for breakfast, her occupation, and a lack of personalized interventions to reduce her emotional distress/behaviors of calling out.
Review of The Unmet Needs Model, [NAME]-[NAME] and [NAME] (1995), revealed that those with Dementia develop problem behaviors from an imbalance in the interaction between life-long habits and personality, current physical and mental states and less than optimal environmental conditions.
Review of Alert Notes dated 3/6/23-6/13/23 revealed seven occurrences of Resident #15 getting no relief from interventions following episodes of behaviors.
In an interview on 6/14/23 at 8:39 a.m., Certified Nursing Assistant (CENA) Q reported Resident #15 often called out for help, yelled nonsensical statements, and spent most of her time in her room alone. When asked what interventions were helpful in reducing Resident #15's distress, CENA Q said I don't really know, she likes snacks. CENA Q reported the staff were instructed to only get Resident #15 out of bed every other day due to her pressure ulcer.
Review of Physician Orders dated 6/13/23 revealed no order for Resident #15 to remain in bed every other day.
In an interview on 6/13/23 at 10:33 a.m., another resident (Resident #19 who was cognitively intact and who's room was adjacent to Resident #15's) reported he heard Resident #15 calling out much of the day and night. Resident #19 reported he felt sorry for Resident #15 because she was upset so often.
During an observation on 6/13/23 at 2:30 p.m., Resident #15 was lying on her back in bed, talking to self. The television in Resident #15's room was on but she appeared unaware of it.
During an observation on 6/13/23 at 3:33 p.m., Resident #15 was lying on her back in bed, talking loudly with an urgent tone, and stated Ok, right here, right here!.
During an observation on 6/14/23 at 11:06 a.m., Resident #15 was awake, sitting up in her wheelchair, sitting near the nurse's station. Resident #15 appeared calm, was not calling out and was noted to watch others walking by.
During an observation on 6/14/23 at 12:21 p.m., Resident #15 was seated in her wheelchair at a table in the dining room, awake and talking quietly to herself.
During an observation on 6/14/23 at 1:22 p.m., Resident #15 was awake, in her wheelchair alone in her room, yelling Help me, help me, come here. Resident #15 rubbed her right thigh and stated, Oh God, help me.
Resident #27
Review of an admission Record dated 1/28/23 revealed Resident #27 was admitted to the facility with the following pertinent diagnoses: Senile Degeneration of the Brain (loss of intellectual ability associated with old age), Depression, Unspecified Dementia (progressive loss of intellectual functioning), Adult Failure to Thrive (state of decline that is multifactorial) and low back pain.
Review of a Minimum Data Set (MDS) assessment for Resident #27, dated 4/13/23, revealed a Brief Interview for Mental Status (BIMS) score of 9 indicating the Resident was moderately cognitively impaired (difficulty with problem solving, remembering details, learning new things). Section V of the MDS indicated Resident #27 had a 3-point decrease in score from a BIMS completed on 2/2/23. The MDS also indicated Residents #27 had continuous presence of disorganized thinking, was dependent for transfers (moving from one surface to another) and had a life expectancy of 6 months or less.
Review of a Care Plan for Resident #27, dated 4/24/23, revealed a focus/goal and interventions as follows: Focus: Resident exhibits behaviors r/t (related to) dementia .emotional discomfort .Goal: will have no increase in symptoms .Interventions: administer medications .assist Resident to develop more appropriate methods of coping .
In an interview on 6/14/23 at 8:39 a.m., Certified Nursing Assistant (CENA) Q reported Resident #27 called out frequently. CENA Q described Resident #27 as a very social person and reported the staff who knew him well often brought him to the nurse's station area where he could socialize with others, gave him his favorite drink (vegetable juice), helped him call his wife and assisted him to the Movies & Popcorn activity. CENA Q reported she learned this information about Resident #27 by interacting with him, and the interventions seemed to reduce his episodes of calling out. These interventions were not present in Resident #27's care plan.
In an interview on 6/14/23 at 9:07 a.m., Activities Director (AD) S reported that Resident #27 sometimes appeared to enjoy group activities, but was care planned for independent leisure involvement because he had voiced a desire to leave group activities in the past. AD S reported Resident #27 responded well to some interventions, including chatting with others in common areas of the building, people watching and reminiscing about owning a restaurant chain. AD S also reported Resident #27 enjoyed drinking vegetable juice. These interventions were not reflected in Resident #27's care plan.
During an observation on 6/12/23 at 10:13 a.m., Resident #27 was alone in his room, lying in bed and could be heard from the nurse's station, approximately thirty feet from his doorway, yelling Hello, hello, hello.
During an observation on 6/12/23 at 2:39 p.m., Resident #27 was alone in his room, sitting in a recliner chair yelling Dad .Dad .[NAME] .hello, hello?.
During an observation on 6/12/23 at 2:40 p.m., Certified Nursing Assistant (CENA) J and Licensed Practical Nurse (LPN) K stood at the nurse's station, giggled as Resident #27 continued to yell [NAME], hello, hello?. CENA J turned to the surveyor, who had just left Resident #27's room, and asked Did you help him find [NAME]?, then giggled and commented to coworker about the resident yelling. CENA J then went to Resident #27's room briefly, returned to the nurse's station and Resident #27 continued to call out.
During an observation on 6/13/23 at 3:32 p.m., Resident #27 was in his room alone, lying in bed yelling Hello, hello! and could be heard from the hallway, approximately twenty feet from his doorway.
During an observation on 6/14/23 at 11:06 a.m., Resident #27 was sitting in a recliner chair near the nurse's station, when greeted Resident #27 stated Everybody is out and about and it's a nice day. Resident #27 appeared calm, smiled during the interaction. No episodes of calling out were noted while Resident #27 was in a common area.
Review of a Target Behavior record dated 5/16/23-6/13/23 revealed Resident #27 had 26 occurrences of behavioral symptoms and 15 occurrences in which interventions were not effective in providing the Resident relief.
Review of The Unmet Needs Model, [NAME]-[NAME] and [NAME] (1995), revealed that those with Dementia develop problem behaviors from an imbalance in the interaction between life-long habits and personality, current physical and mental states and less than optimal environmental conditions.
Based on observation, interview, and record review the facility failed to engage and enrich the residents' quality of life by failing to develop person centered individualized care plan interventions and to provide meaningful preferred activities for 10 residents (Resident #22, #21, #16, #8, #12, #20, #26, #28, #15, and #27) of 10 residents reviewed for dementia care, resulting in the potential for increased behaviors such as wandering, physical and verbal aggression, agitation, and increased potential for adverse outcomes due to cognitive impairment in order to maintain their highest practicable physical, mental, and psychosocial well-being.
Findings include:
Resident #22
Review of an admission Record revealed Resident #22 was a male with pertinent diagnoses which included Alzheimer's disease, early onset, muscle weakness, reduced mobility, cognitive communication deficit, psychotic disorder with delusions, unsteadiness on feet, and abnormalities of gait and mobility.
Review of a Minimum Data Set (MDS) assessment for Resident #22, dated 3/14/23, revealed .Documented behaviors included physical behaviors towards staff and also wandering with attempts to leave thru doors .Physical towards staff during care. No patterns with wandering as it occurs throughout the day .Early onset dementia with depression and anxiety; see medical record .Agitation with care .Dx (diagnosis) of early onset Alzheimer's .Section E: Behavior: Wandering impact .A. Does the wandering place the resident at significant risk of getting to a potentially dangerous place .Yes .E1100. Change in Behavior of Other Symptoms .How does the resident's current behavior status, care rejection, or wandering compare to prior assessment? .2. Worse .Section F: Customary Routine and Activities: (Resident #22) finds it important to listen to music - he likes rock and roll and loves to dance, be around animals - always had dogs, enjoys snacks of any kind, gravitates towards where people are on the unit, enjoys taking his walks and sometimes runs, do favorite activities such as hunting, fishing, trucks, and motorcycles, and enjoys going outside .
Review of the Care Plan for Resident #22, revised on 8/10/21, revealed, the focus .(Resident #22) has altered thought processes and cognitive changes related to Alzheimer's . with the intervention .Ask yes/no questions in order to determine the resident's needs .Communicate with the resident/guardian/caregivers regarding resident's capabilities and needs .Cue, reorient, and supervise as needed .
Review of the Care Plan for Resident #22, revised on 8/10/21, revealed, the focus .The resident is dependent on staff for meeting emotional, intellectual, physical, and social needs r/t (related to) cognitive deficits secondary to dementia . with the intervention .Converse with resident while providing care .ensure the activities the resident is attending are: compatible with physical and mental capabilities, compatible with know interests and preferences; Adapted as needed; compatible with individual needs and abilities .Observe for verbal and nonverbal response .review resident's activity needs .The resident needs assistance with ADLs (Activities of Daily Living) as required during the activity .The resident needs assistance/escort to activity functions .The resident's preferred activities are: music (80s rock), enjoys taking walks/touring unit, snacks (juice/coffee & cookies), socializing with other residents & staff during his walks, busy hands, special events, coffee hour (hx (history) of outdoors/hunting, trucks, crossword puzzles & construction) .When experiencing agitation take for a walk, offer snack/drink, allow to vent feelings, offer rest period after lunch .When asking direct questions during activity, phrase questions for a yes or no response. Allow ample response time .
Review of an Activities Evaluation dated 3/14/23, revealed .Interested in life/activities 2. Interested .Activities: Beauty/Barber, Cultural events/news, Exercise/Sports, Family/Friend visits, Gardening/Outdoor, Walking, Parties/Social events, Pet events, Music/Talk radio, Other - Motorcycles, Trucks .Attitude: Cooperative, Active, and Social person .Special Considerations: Wanderer, Pain management, and Task segmentation .
In an observation on 06/12/23 at 10:39 AM, Resident #22 was observed in the hallway on the memory care unit walking from one end to the other end. Pacing back and forth down the hallway.
Review of Nurses' Notes dated 12/23/22 at 6:04 PM, revealed .Resident was previously in other residents room in her bed, staff were assisting female resident back to her room when they observed this resident laying in her bed, they assisted male resident out of her bed as she was yelling at him to get out of her room, male resident started walking down hallway not understanding the situation, short while later female resident came out into hallway grabbed residents arms and was hold them behind him when he was trying to get away he turned around and with a closed fist made contact with female resident's chest . Note: Requested incidents and no incident report provided for this incident.
Review of NP/PA (Nurse Practitioner/Physician Assistant) Progress Note dated 6/1/23 at 12:47 PM, revealed .being seen per the request of the staff at the nursing home that pt (patient) appears more agitated and he is not sleeping well at night .Pt has advanced dementia and at this time is unable to make his needs known for the most part .Pt walks in the hallways without any type of assistive device-he does walk with his head bent down .I suspect there are other pt's on the memory care unit that might get pt a bit worked up also .Nursing staff will continue to monitor and report changes .
Resident #12
Review of an admission Record revealed Resident #12 was a female with pertinent diagnoses which included dementia, anemia, pain, and a tendency to fall.
In an observation on 06/12/23 at 11:27 AM, Resident #22 went into Resident #21's room exited and entered Resident #12's room who was lying in her bed. Resident #12 was looking at Resident #22 as he stood over her at the right side of the bed where her upper body was. Resident #22 was observed to be side stepping down the right side of Resident #12's bed, to the foot of her bed, along the foot board of her bed, then along the wall and to far right corner of her room. At 11:29 AM, Resident #22 exited Resident #12's room and went to Resident #21's room and proceeded to seat himself sideways in the resident's recliner.
Resident #26
Review of an admission Record revealed Resident #26 was a female with pertinent diagnoses which included Alzheimer's disease, dementia, heart failure, depression, back pain, and obstructive lung disease.
In an observation on 06/12/23 at 10:44 AM, observed Resident #26 was angrily raising her voice and was aggressively telling Resident #22 he was stinky and had dandruff. Resident #26 told this writer to not let Resident #22 .get close to the computer otherwise the screen would be covered in dandruff . Staff who were present did not intervene or provide redirection for Resident #26 to remove her from Resident #22's path while he walked in the hallway by the dayroom. Resident #22 proceeded around her and went on down the hallway.
In an observation on 06/12/23 at 11:20 AM, Resident #22 was walking in the hallway down by the dayroom headed down to the end of the hallway. Resident #26 was walking in the other direction reporting that Resident #22 stunk, and the staff needed to use .the spray . to get rid of his smell and continued to focus on his smell and how to get rid of it as he continued to walk down the hallway. No staff intervened or provided intervention or redirection to Resident #26 or to assist Resident #22 with an alternative activity.
In an observation on 06/12/23 at 11:32 AM, Resident #22 exited his room and stood in the doorway of Resident #12's room. Resident #22 proceeded to turn around and then stood in the doorway of Resident #21's room, then leaned on the door frame and looked down the hallway. No staff were present on the hallway to intervene or determine if Resident #22 was tired and needed to rest.
In an observation on 06/12/23 at 11:33 AM, Resident #22 proceeded to enter Resident #12's room and stood at the foot of her bed. Resident #12 was holding up her baby doll and showing it to Resident #22. Resident #22 exited her room and then proceeded back to Resident #21's room. No staff came to intervene during his time entering other resident's rooms. No staff were observed on the hallway.
In an observation on 06/12/23 at 11:34 AM, Resident #22 walked up to Resident #21's bed while he was lying in it. There was a fall mat on the left side of the bed, the right side was against the wall. Resident #22 attempted to step up on the fall mat to walk along the side of Resident #21's bed. Resident #22 was unable to step on the mat and walked across the corner of it over to the recliner in Resident #21's room then proceeded out of the room and ambulated down the hallway towards the main entrance of the unit. Resident #12 moved herself to the side of the bed, still in a lying position, leaned over and grabbed the wheelchair which was about 3 feet away and pulled it to the right side of her bed. No staff came to intervene during Resident #22's time entering other resident's rooms. No staff were observed on the hallway.
In an observation on 06/12/23 at 11:36 AM, Resident #22 proceeded to enter Resident #21's room, then exited and proceeded to stand in the doorway of Resident #12's room. Resident #12 was touching the wheelchair and Resident #22 walked over to the foot of her bed, and she pushed the wheelchair away from the side of her bed out of her reach all the while she was looking at Resident #22 as he stood in the far right corner of her room. Resident #22 exited her room and stood outside of Resident #21's room and then proceeded to ambulate down the hallway. No staff came to intervene during his time entering other resident's rooms. No staff were observed on the hallway.
Resident #20
Review of an admission Record revealed Resident #20 was a female with pertinent diagnoses which included Alzheimer's disease, anxiety, depression, obstructive lung disease, osteoarthritis, adult failure to thrive, and pain.
Resident #28
Review of an admission Record revealed Resident #28 was a male with pertinent diagnoses which included dementia, diabetes, UTI (urinary tract infection), anxiety, neuropathy (nerve damage), arthritis, and dysphagia.
In an observation on 06/12/23 11:47 AM, Resident #26, Resident #20, and Resident #28 were in the day room. Resident #20 had a fidget mat on her lap as her eyes were closed and she was not interacting with the mat. Activities Aide (AA) EE was observed seated at the table talking with Resident #26.
In an observation on 06/12/23 at 02:31 PM, Resident #22 was observed walking out of Resident #12's room and into Resident #21's room. The Certified Nursing Assistant (CNA) staff on the unit were providing report to the second shift staff and no staff intervened or redirected Resident #22 away from entering another resident's room.
In an observation on 06/12/23 at 02:32 PM Resident #22 was standing just inside the doorway to Resident #21's room by his chair by the door. Resident #21 was on his side facing away from the wall and he had his head covered. Resident #22 was walking towards Resident #21's bed and was positioned at the head of his bed, looked down at the fall mat. Resident #22 waved his hand in the air, made some nonsensical statements, and proceeded to step on the fall mat with his right foot, it moved some as he was unable to raise his foot high enough to step on it, proceeded to walk over the corner of the fall mat while he mumbled and stepped towards the recliner and sat down in Resident #21's recliner. No staff intervened when Resident #22 entered another resident's room.
In an observation on 06/12/23 at 02:38 PM, Resident #22 was observed seated on Resident #21's recliner sideways on his left hip, hanging on to the table with his right hand while mumbling to himself. Resident #22 proceeded to remove his hand from the table but did not sit back in the recliner with his back against the back of the chair.
In an observation on 06/12/23 at 02:43 PM, CNA H observed Resident #22 and proceeded to assist him with the use of a gait belt to help him up out of the recliner as he was talking to them. Resident #22 was observed leaning forward with his forearms on his knees.
In an interview on 06/12/23 at 02:48 PM, Registered Nurse (RN) C reported Resident #22 liked recliners and he would go to the other residents' rooms with recliners and would sit in them.
Resident #8
Review of an admission Record revealed Resident #8 was a female with pertinent diagnoses which included dementia, diabetes, stroke, obstructive lung disease, dysphagia, and cataracts.
In an observation on 06/12/23 at 02:59 PM, Resident #28, Resident #22, Resident #26, and Resident #8 were observed in the day room with the Activities Director S doing some folding of washcloths. Resident #22 observed sitting there, not folding the washcloths. He did not appear happy based on his facial expressions and was mumbling to himself.
In an observation on 06/13/23 at 10:06 AM, Resident #22's room had a nightstand, with a 3-drawer plastic dresser next to it along the wall in his room. There were no noted pictures, magazines/books, CD player or other items related to his interests and no noted personal items in his room.
In an observation on 06/13/23 at 01:20 PM, Resident #22 was observed seated at a table with his left hand on his face with his elbow on the arm rest, and his eyes were closed. Resident #20 was lying in her Broda chair, eyes closed, had her legs drawn up to her body and was covered with a couple blankets. Resident #26 started to raise her voice at Resident #21 about how loud he was and told him to .Shut up . then continued to talk nonsensically. Note: At this time Activities Director S was the only staff on the unit.
In an observation on 06/13/23 at 01:35 PM, Resident #26 was seated at the table by the door and was talking to herself about her father, poison oak, and doctor's appointment. Resident #22 got up to walk out of the door and Activities Director (AD) S stopped him as he was close to the exit of the room and redirected him back into the room. Resident #26 started focusing on Resident #22 and began saying he doesn't shampoo his hair, he stinks, and he wasn't going with them to her destination she was talking about. Resident #22 proceeded towards the back part of the room and Resident #26 continued to raise her voice to him and say those statements. AD S walked over to the Styrofoam cups and got Resident #22 a cup to get him a drink.
In an observation on 06/13/23 at 01:41 PM, Resident #22 exited the dining/day room and entered Resident #8's room. Resident #22 stood at the foot of her bed, walked along the side of the bed, went to the other side of the room and was touching the wall and looking at items on her rolling table. Resident #22 then exited to Resident #8's room, came over to this surveyor, looked at the computer and made a nonsensical statement, and turned and ambulated down the hallway.
In an observation on 06/13/23 at 01:53 PM, Resident #22 was observed standing at the back door looking out the back door windows. As Resident #22 walked back down the hallway, Resident #26 repeatedly stated Resident #22 stinks and he was dirty as he passed her in the hallway. As he proceeded back down the hallway, Resident #26 yelled at him to go home, he wasn't coming with them. Resident #22 walked past her with his head down and he tensed up his body inward as he passed her. Resident #26 reached out to grab him and she stopped as she saw this writer looking at her and continued yelling at him and continued down the hallway with her rant about Resident #22. Note: No staff came to the hallway to observe or intervene in this situation.
In an interview on 06/13/23 at 01:58 PM, Licensed Practical Nurse (LPN) P reported the facility was aware Resident #22 was going into other resident's rooms and some residents requested to have the stop sign banner placed over their door entry way to prevent him from entering their room. LPN P reported interventions for him were to check on him frequently when he was wandering, there was also the activity busy hands which has the different locks, knobs and other fidget items, and there were the popper items.
Resident #21
Review of an admission Record revealed Resident #21 was a male with pertinent diagnoses which included stroke, fluency disorder following a stroke, sleep disorder, repeated falls, muscle weakness, reduced mobility, diabetes, anxiety, cognitive communication deficit, chronic pain, senile degeneration of brain, epilepsy, mood disorder, fracture of right acetabulum, fracture of upper end of right humerus, and lower urinary tract symptoms.
Review of a current Care Plan for Resident #21, revised on 9/29/21, revealed the focus .The resident has vascular dementia with behavioral disturbance . with the interventions .Administer medications as ordered .use preferred name, identify yourself with each interaction, face the resident when speaking, make eye contact, provide with necessary cues. Stop and return if agitated .Cue, reorient, and supervise as needed .Present just one thought, idea, question or command at a time .
Review of a current Care Plan for Resident #21, revised on 3/20/23, revealed the focus .Resident structures his leisure time independently thru own independent activities. Strong preference to stay in his room; can be difficult to engage in activity groups. Prefers nicknames . with the intervention .Resident will continue to make activity preferences/choices .Resident will continue to structure their leisure time independently at the center .Ensure resident has the supplies needed to participate in activities in their room independently. CD player with Cuban music, enjoys snacks delivered to room .Favorite activities include snacks delivered to his room (cookies and coffee and his ethnic snacks), TV, social with others often initiating conversations independently. *ordered him Cuban CDs; also provided resident with CD player. Staff offer room visits as tolerated .
Review of an Alert Note dated 2/16/2023 at 3:26 PM, revealed .Behavior occurred - interventions ineffective .
Review of an Alert Note dated 2/21/2023 at 6:53 PM, revealed .Behavior occurred - interventions ineffective .behaviors continue/treatments in place .
Review of Nurse's Note dated 2/22/23 at 5:48 AM, revealed, .Resistant to CENA care, nurse went in and talked to res and gave snack, res. Calmed down.
Review of an Alert Note dated 3/6/2023 at 3:00 PM, revealed .no change in behaviors, all treatments are in place .
Review of Nurse's Note dated 3/7/23 at 11:32 PM, revealed, .res yelling out and swatting at CENA during routine HS care .res now resting comfortably with eyes closed .
Review of an Alert Note dated 3/12/2023 00:46 AM, revealed .behavior continues, all interventions are in place .
Review of an Alert Note dated 3/12/2023 00:48 AM, revealed .behavior continues, all interventions are in place .resident refusing to bathe at this time .
Review of Nurse's Note dated 3/17/23 at 1:53 AM, revealed, .resident yelling out .
Review of Nurse's Note dated 3/20/23 at 6:28 AM, revealed, .Behavior occurred - interventions ineffective .
Review of an Alert Note dated 3/21/2023 05:39 A[TRUNCATED]