MARSHFIELD CARE CENTER FOR REHAB AND HEALTHCARE




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Marshfield Care Center for Rehab and Healthcare has received a Trust Grade of F, indicating significant concerns about the facility's quality of care. Ranking #419 out of 479 in Missouri places it in the bottom half of nursing homes, and it is the lowest-ranked facility in Webster County. Unfortunately, the facility's situation is worsening, with issues increasing from 7 in 2024 to 8 in 2025. Staffing is a major concern, with a low rating of 1 out of 5 and a high turnover rate of 83%, significantly above the state average. While there are no fines on record, which is a positive aspect, the facility has faced serious deficiencies, including failing to provide proper wound care for a resident, leading to wound deterioration and infection. Additionally, there have been concerns about food safety practices, such as improper food storage and contamination risks. Overall, families should weigh these significant weaknesses against the few strengths when considering this facility for their loved ones.
- Trust Score
- F
- In Missouri
- #419/479
- Safety Record
- Moderate
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 83% turnover. Very high, 35 points above average. Constant new faces learning your loved one's needs.
- Penalties ✓ Good
- No fines on record. Clean compliance history, better than most Missouri facilities.
- Skilled Nurses ⚠ Watch
- Each resident gets only 12 minutes of Registered Nurse (RN) attention daily — below average for Missouri. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 45 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Missouri average (2.5)
Significant quality concerns identified by CMS
37pts above Missouri avg (46%)
Frequent staff changes - ask about care continuity
Part of a multi-facility chain
Ask about local staffing decisions and management
35 points above Missouri average of 48%
The Ugly 45 deficiencies on record
Sept 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to provide pharmacy services to meet the needs of each r...
Read full inspector narrative →
Jul 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
May 2025
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to provide care per professional standards related to pressure ulcers ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility staff failed to maintain $4,000.00 cash for one resident (Resident #1) when s...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to implement and maintain an effective infection control...
Read full inspector narrative →
Mar 2025
1 deficiency
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review, the facility failed to store, prepare, distribute, and serve food in accordance with professional standards that protected food from possible contam...
Read full inspector narrative →
Jan 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure all allegations of abuse and neglect were reported immediate...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to document a timely and thorough investigation of verbal abuse when staff did not begin an immediate investigation into an allegation of staf...
Read full inspector narrative →
Aug 2024
7 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure all resident's drug regimens were free from unnecessary drugs when staff failed to provide adequate monitoring related to the admini...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility staff failed to ensure all residents were free from significant medication errors when staff failed to prime (removing the air from the...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain an effective pest control program to control...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of Resident #30's face sheet showed the following information:
-admission date of 07/31/21;
-Diagnoses included COPD, ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Review of Resident #30's face sheet showed the following information:
-admission date of 07/31/21;
-Diagnoses included COPD, ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility staff failed to ensure the facility was maintained in a sanitary and comfortable fashion when light fixtures in the kitchen and dining ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, record review, and interview, the facility failed to keep food safe from potential contamination when staff stacked clean dishware inside one another instead of air drying, which...
Read full inspector narrative →
Feb 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record review, the facility failed to protect the resident's right to be free from verbal and physical abuse by staff when one staff member (Certified Nursing As...
Read full inspector narrative →
Dec 2022
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
This deficiency is uncorrected. For previous examples, please refer to the Statement of Deficiencies dated 11/10/2022.
1. Please refer to event ID ID4122, exit date 12/27/2022 for details.
MO00211485
...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 1. Please refer to event ID ID4122, exit date 12/27/2022 for details.
MO00211485
Based on record review and interview, the facil...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0776
(Tag F0776)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 1. Please refer to event ID ID4122, exit date 12/27/2022 for details.
MO00211485
Based on interview and record review, the facil...
Read full inspector narrative →
Nov 2022
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to ensure medication was administered per standards of practice and per physician's orders when a certified nurse aide (CNA) administered anot...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0776
(Tag F0776)
Could have caused harm · This affected 1 resident
Deficiency Text Not Available
Read full inspector narrative →
Oct 2022
11 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Based on interviews and record reviews, the facility failed to ensure that all allegations of possible abuse were thoroughly and timely investigated when staff failed to document investigations of all...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
This deficiency is uncorrected. For previous examples, please refer to the Statement of Deficiencies dated 11/10/2022.
Based on record review and interview, the facility failed to provide care and ser...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure staff consistently documented urine output as ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
Based on record review, and interview, the facility failed to have a physician's order indicating where and when the resident was to go to dialysis (a process of cleaning the blood by a special machin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide laboratory services as ordered by the physician, when staff...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0776
(Tag F0776)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to obtain radiology services timely to meet the needs of two residents...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
Based on interviews and record reviews, the facility failed to ensure all allegations of possible abuse were reported immediately to management and within two hours to the state licensing agency (Depa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to obtain physicians' orders for bed rails and failed to...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on interview and record review, the facility failed to maintain an effective system of records of receipt and disposition of controlled medications when the facility did not maintain pharmacy re...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to maintain completed and accurate records when staff fa...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on interview and record review, the facility failed to maintain an effective infection control program for all residents when the facility failed to have a program in place for the prevention of...
Read full inspector narrative →
Nov 2019
12 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to inform two additional residents (Residents #27 and #49) when changes were made to his/her Medicare coverage prior to the end of service dat...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to follow their restraint policy for one of 15 sampled residents (Resident #14), when staff did not obtain specific physician's o...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interviews, the facility failed to assure they provided care and treatment in accordance...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to implement measures to treat and prevent pressure u...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observations, interviews and record reviews, the facility failed to provide care to prevent urinary tract infections (UTIs) for a resident with an indwelling catheter when staff failed to fol...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on observations, interview and record review, the facility failed to ensure they documented the administration of their controlled substances to ensure the narcotic count and the Controlled Subs...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observation, interview and record review, the facility failed to provide a safe and effective medication administration system that was free of significant medication errors for one out of 13...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to document a complete and accurate Minimum Data Set (MDS) assessment ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure staff administered medications with a medication error rate of less than 5 percent (%). Facility staff made three medic...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to ensure staff destroyed and did not store an expired bottle of liquid Ativan (often used at end of life and to treat anxiety), ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure staff provided care in a manner to prevent infe...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to implement, follow, and monitor a facility-wide antibiotic stewardship program. The facility census was 52.
1. Review of the f...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • No fines on record. Clean compliance history, better than most Missouri facilities.
- • 45 deficiencies on record, including 1 serious (caused harm) violation. Ask about corrective actions taken.
- • Grade F (25/100). Below average facility with significant concerns.
- • 83% turnover. Very high, 35 points above average. Constant new faces learning your loved one's needs.
About This Facility
What is Marshfield For Rehab And Healthcare's CMS Rating?
CMS assigns MARSHFIELD CARE CENTER FOR REHAB AND HEALTHCARE an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Missouri, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Marshfield For Rehab And Healthcare Staffed?
CMS rates MARSHFIELD CARE CENTER FOR REHAB AND HEALTHCARE's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 83%, which is 37 percentage points above the Missouri average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 86%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Marshfield For Rehab And Healthcare?
State health inspectors documented 45 deficiencies at MARSHFIELD CARE CENTER FOR REHAB AND HEALTHCARE during 2019 to 2025. These included: 1 that caused actual resident harm and 44 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Marshfield For Rehab And Healthcare?
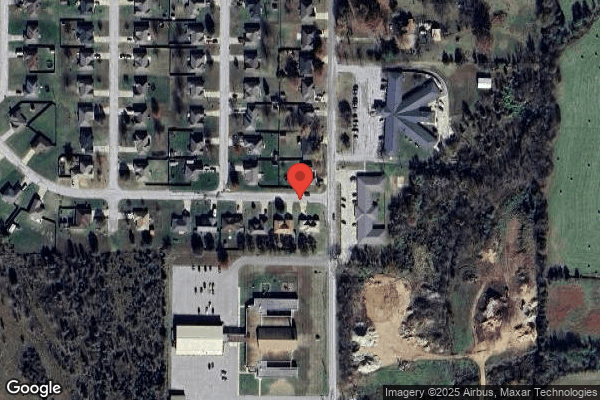
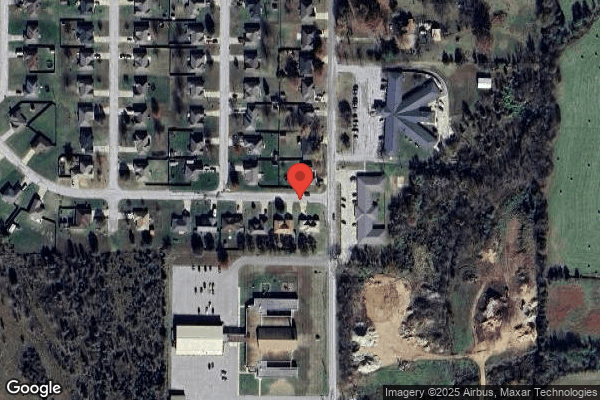
MARSHFIELD CARE CENTER FOR REHAB AND HEALTHCARE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PRIME HEALTHCARE MANAGEMENT, a chain that manages multiple nursing homes. With 74 certified beds and approximately 54 residents (about 73% occupancy), it is a smaller facility located in MARSHFIELD, Missouri.
How Does Marshfield For Rehab And Healthcare Compare to Other Missouri Nursing Homes?
Compared to the 100 nursing homes in Missouri, MARSHFIELD CARE CENTER FOR REHAB AND HEALTHCARE's overall rating (1 stars) is below the state average of 2.5, staff turnover (83%) is significantly higher than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Marshfield For Rehab And Healthcare?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's high staff turnover rate and the below-average staffing rating.
Is Marshfield For Rehab And Healthcare Safe?
Based on CMS inspection data, MARSHFIELD CARE CENTER FOR REHAB AND HEALTHCARE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Missouri. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Marshfield For Rehab And Healthcare Stick Around?
Staff turnover at MARSHFIELD CARE CENTER FOR REHAB AND HEALTHCARE is high. At 83%, the facility is 37 percentage points above the Missouri average of 46%. Registered Nurse turnover is particularly concerning at 86%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Marshfield For Rehab And Healthcare Ever Fined?
MARSHFIELD CARE CENTER FOR REHAB AND HEALTHCARE has no federal fines on record. CMS issues fines when nursing homes fail to meet care standards or don't correct problems found during inspections. The absence of fines suggests the facility has either maintained compliance or corrected any issues before penalties were assessed. This is a positive indicator, though families should still review recent inspection reports for the full picture.
Is Marshfield For Rehab And Healthcare on Any Federal Watch List?
MARSHFIELD CARE CENTER FOR REHAB AND HEALTHCARE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.