Prestige Care Center of Nebraska City




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Prestige Care Center of Nebraska City has received a Trust Grade of F, indicating significant concerns about the facility's care quality and management. Ranked #94 out of 177 nursing homes in Nebraska, this places it in the bottom half of the state, and it is the least favorable option in Otoe County. Although the facility shows an improving trend, with issues decreasing from five in 2024 to three in 2025, it still faces serious deficiencies, including failing to implement critical medication orders and not adequately managing a resident’s pressure ulcer, which could lead to further health complications. Staffing is a concern, with a below-average rating of 2 out of 5 and a high turnover rate of 64%, suggesting that many staff do not remain long enough to build relationships with residents. Additionally, the facility has incurred fines totaling $15,625, which is higher than 83% of similar facilities in Nebraska, raising alarms about ongoing compliance issues.
- Trust Score
- F
- In Nebraska
- #94/177
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 64% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $15,625 in fines. Lower than most Nebraska facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 29 minutes of Registered Nurse (RN) attention daily — below average for Nebraska. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 33 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Near Nebraska average (2.9)
Meets federal standards, typical of most facilities
18pts above Nebraska avg (46%)
Frequent staff changes - ask about care continuity
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
16 points above Nebraska average of 48%
The Ugly 33 deficiencies on record
Sept 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
Licensure Reference Number 175 NAC 12-006.02(H)Based on interview and record review, the facility failed to complete a thorough investigation for an allegation of abuse for 1 (Resident 1) of 3 sampled...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0628
(Tag F0628)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to provide federally required transfer documentation to the receiving health care institution for 2 (Resident 1 & 2) of 3 sampled residents. T...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Licensure Reference Number 175 NAC 12-006.09(I)Based on observation, interview, and record review, the facility failed to implement interventions to prevent potential falls for 1 (Resident 2) of 3 sam...
Read full inspector narrative →
Nov 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** LICENSURE REFERENCE NUMBER 175 NAC 12-006.09(J)(i)(1
Based on record review and interviews, the facility failed to initiate inte...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Licensure Reference Number 175 NAC 12-006.09
Based on observation, record review and interview, the facility failed to provide a...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Licensure Reference Number 175 NAC 12-006.18
Based on observation, interview and record review, the facility failed to maintain ...
Read full inspector narrative →
Sept 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Licensure Reference Number 175 NAC 12-006.04(F)(i)
Based on interview and record review, the facility staff failed to ensure pra...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Licensure Reference Number 175 NAC 12-006.04(F)(i)(5)
Based on record review and interview, the facility staff failed to notify ...
Read full inspector narrative →
Sept 2023
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Licensure Reference Number 12-006.09 D7a
Based on observation, record review and interview, the facility failed to ensure that c...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Licensure Reference Number 12-006-18 B
Based on observation, interview and record review; the facility failed to maintain the cleanliness and condition of ventilation systems, fixtures and floors in 7...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0727
(Tag F0727)
Could have caused harm · This affected most or all residents
Licensure Reference Number NAC 12-006.04C2
Based on record review and interview, the facility failed to ensure a Registered Nurse was present in the facility for a continuous period of 8 hours a day, ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Licensure Reference Number 12-006-11 E
Based on observations, interviews and record reviews; the facility failed to utilize proper hand hygiene practices during the preparation and serving of food to ...
Read full inspector narrative →
Jun 2022
21 deficiencies
3 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** LICENSURE REFERENCE NUMBER 175 NAC 12-006.09D2b
Based on observation, record review and interview; the facility staff failed to ...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0697
(Tag F0697)
A resident was harmed · This affected 1 resident
Licensure Reference Number 175 NAC 12-006.09
Based on observation, interview, and record review, the facility failed to implement a pain management program for 1 sampled resident (Resident 40). The fa...
Read full inspector narrative →
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Deficiency F0760
(Tag F0760)
A resident was harmed · This affected 1 resident
Licensure Reference Number 175 NAC 12-006.10D
Based on observation, interview, and record review, the facility failed to clarify and implement a medication for the treatment of COVID-19 for 1 (Residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility staff failed to issue the Advanced Beneficiary Notice (ABN) to 1 (Resident 39) of 3 sampled residents which did not give the resident/resident repres...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** LICENSURE REFERENCE NUMBER 175 NAC 12-006.02(8)
Based on record review and interview; the facility staff failed to submit a inve...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Licensure Reference Number 175 NAC 12-006.09D6(7)
Based on observation, interview, and record review, the facility failed to obt...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility staff failed to evaluate and obtain treatment for Depression (a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
LICENSURE REFERENCE NUMBER 175 NAC 12-006.10D
Based on observations, record review and interview; the facility staff failed to ensure a medication error rate of less than 5%. Observations of 25 medica...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0565
(Tag F0565)
Could have caused harm · This affected multiple residents
Licensure Reference Number 175 NAC 12-006.05(17)
Based on observation, interview, and record review, the facility failed to address Resident Council grievances (complaint or protest) regarding houseke...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Licensure Reference Number 175 NAC 12-006.18
Based on observation, interview and record review; the facility failed to ensure th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
B. Record Revied of the undated Office of the Long-Term Care Ombudsman (an official appointed to investigate resident's complaints) Facility Initiated Transfer and Discharge Notice Checklist revealed ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** LICENSURE REFERENCE NUMBER 175 NAC 12-006.09
Based on observations, record review and interview; the facility staff failed to ev...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** D. An observation on 06/01/2022 at 09:22 AM revealed Resident 20 was sitting alone in a wheelchair in the room with a plate of u...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
Licensure Reference Number 175 NAC 12-006.09D
Based on record review and interview; the facility failed to implement non pharmacological interventions prior to the administration of antianxiety medica...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected multiple residents
Licensure Reference Number 175 NAC 12-006.11D
Based on observation and interview, the facility staff failed to ensure that food was being served at temperatures to prevent foodborne illness. The facil...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0917
(Tag F0917)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Licensure Reference Number 175 NAC 12-007.03I5
Based on observation and interview, the facility failed to ensure each resident i...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected most or all residents
C. Observation of Resident 13's room revealed; 3 rugs on the floor, sharp metal clamps on the end of the bed, a moving dolly in the closet, tools in a toolbox including screwdrivers and pliers. A tele...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Administration
(Tag F0835)
Could have caused harm · This affected most or all residents
LICENSURE REFERENCE NUMBER 175 NAC 12-006.02
Based on observations, record reviews and interview; the facility management failed to utilize its resources to attain or maintain the highest practicable ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Licensure Reference Number 175 NAC 12-006.17A(2)
Licensure Reference Number 175 NAC 12-006.17B
Based on observation, interview, and record review, the facility failed to ensure staff and visitors' COV...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0886
(Tag F0886)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Licensure Reference Number 175 NAC 12-006.17
Based on observation, interview, and record review, the facility failed to prevent ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0888
(Tag F0888)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and record review; the facility failed to fully implement the facility COVID-19 Contingency Plan for staff with exemptions. Less than 25% of staff were unvaccinated....
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 4 harm violation(s). Review inspection reports carefully.
- • 33 deficiencies on record, including 4 serious (caused harm) violations. Ask about corrective actions taken.
- • $15,625 in fines. Above average for Nebraska. Some compliance problems on record.
- • Grade F (33/100). Below average facility with significant concerns.
About This Facility
What is Prestige Care Center Of Nebraska City's CMS Rating?
CMS assigns Prestige Care Center of Nebraska City an overall rating of 3 out of 5 stars, which is considered average nationally. Within Nebraska, this rating places the facility higher than 99% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Prestige Care Center Of Nebraska City Staffed?
CMS rates Prestige Care Center of Nebraska City's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 64%, which is 18 percentage points above the Nebraska average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at Prestige Care Center Of Nebraska City?
State health inspectors documented 33 deficiencies at Prestige Care Center of Nebraska City during 2022 to 2025. These included: 4 that caused actual resident harm and 29 with potential for harm. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
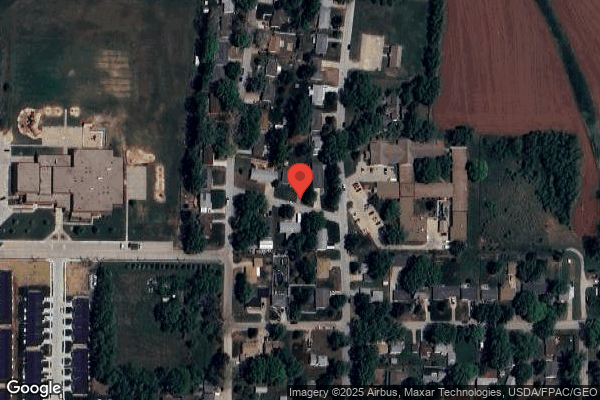
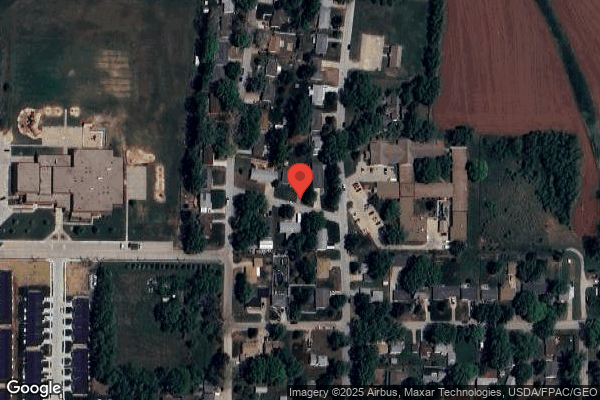
Who Owns and Operates Prestige Care Center Of Nebraska City?
Prestige Care Center of Nebraska City is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by PRESTIGE CARE CENTER, a chain that manages multiple nursing homes. With 64 certified beds and approximately 41 residents (about 64% occupancy), it is a smaller facility located in Nebraska City, Nebraska.
How Does Prestige Care Center Of Nebraska City Compare to Other Nebraska Nursing Homes?
Compared to the 100 nursing homes in Nebraska, Prestige Care Center of Nebraska City's overall rating (3 stars) is above the state average of 2.9, staff turnover (64%) is significantly higher than the state average of 46%, and health inspection rating (3 stars) is at the national benchmark.
What Should Families Ask When Visiting Prestige Care Center Of Nebraska City?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's high staff turnover rate and the below-average staffing rating.
Is Prestige Care Center Of Nebraska City Safe?
Based on CMS inspection data, Prestige Care Center of Nebraska City has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in Nebraska. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Prestige Care Center Of Nebraska City Stick Around?
Staff turnover at Prestige Care Center of Nebraska City is high. At 64%, the facility is 18 percentage points above the Nebraska average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Prestige Care Center Of Nebraska City Ever Fined?
Prestige Care Center of Nebraska City has been fined $15,625 across 1 penalty action. This is below the Nebraska average of $33,235. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Prestige Care Center Of Nebraska City on Any Federal Watch List?
Prestige Care Center of Nebraska City is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.