Bear Canyon Rehabilitation Center




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Bear Canyon Rehabilitation Center currently holds a Trust Grade of F, indicating significant concerns about the quality of care provided, placing it in the bottom tier of facilities. It ranks #40 out of 67 nursing homes in New Mexico and #13 of 18 in Bernalillo County, meaning there are many better options available nearby. The facility's situation is worsening, with the number of issues increasing from 5 in 2024 to 16 in 2025. Staffing is a concern, with a 68% turnover rate that exceeds the state average, and the overall staffing rating is only 2 out of 5 stars. Additionally, the facility has accumulated $167,434 in fines, which is higher than 82% of similar facilities in New Mexico, suggesting ongoing compliance problems. Specific incidents highlight serious care deficiencies, such as failing to monitor a resident for signs of stroke and not administering prescribed blood-thinning medication, which could lead to severe health risks. Another critical finding involved inadequate oversight of skin care, which could result in new pressure injuries for residents. While there is some RN coverage, it remains at an average level and may not sufficiently address the care deficiencies observed. Overall, families should weigh these significant weaknesses against any potential strengths when considering this facility for their loved ones.
- Trust Score
- F
- In New Mexico
- #40/67
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 68% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ⚠ Watch
- $167,434 in fines. Higher than 82% of New Mexico facilities, suggesting repeated compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 32 minutes of Registered Nurse (RN) attention daily — about average for New Mexico. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 68 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below New Mexico average (2.9)
Below average - review inspection findings carefully
22pts above New Mexico avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
20 points above New Mexico average of 48%
The Ugly 68 deficiencies on record
Jul 2025
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
Based on a record review and interviews, the facility failed to update physician's orders for 1 (R #1) of 1 (R #1) resident who received supplemental oxygen, when the resident required a greater oxyge...
Read full inspector narrative →
Apr 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide activities of daily living (ADL; activities related to pers...
Read full inspector narrative →
Apr 2025
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interviews, the facility failed to maintain proper infection prevention practices, when staff did not a...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure the facility was free of accident hazards for 19 (R #1-19) of 19 (R #1-19) when the facility failed to ensure no sprinkler above the g...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to maintain proper infection prevention measures by havi...
Read full inspector narrative →
Feb 2025
11 deficiencies
2 IJ (2 affecting multiple)
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Quality of Care
(Tag F0684)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure residents received treatment and care in accordance with pro...
Read full inspector narrative →
CRITICAL
(K)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0760
(Tag F0760)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to administer clopidogrel (blood thinning medication used to prevent h...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure residents or their guardians were aware of what medications they received and understood the reasons, risks, and benefits of the med...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure the resident's current advance directive (a document which p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure accuracy of the Minimum Data Set (MDS; a federally mandated ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to create an accurate Baseline Care Plan (minimum healthcare information necessary to properly care for a resident immediately upon their admi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to complete staff competencies for 2 (Certified Nursing Assistants (CNA) #6, and CNA #7) of 5 (CNA #4, CNA #5, CNA #6, CNA #7, and CNA #8) CNA...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure the resident's medication regimen was free from unnecessary medications for 1 (R #104) of 1 (R #104) residents, when the attending p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure the resident medication regimen was free from unnecessary medications for 1 (R #104) of 1 (R #104) resident, when R #104's hospice p...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observations, interviews, and record review, the facility failed to ensure nurses and Certified Medication Aids (CMAs) dated opened insulin glargine (a medication prescribed to help the body ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to ensure Certified Nurse Aides (CNAs) received the required in-service training of at least 12 hours per year for 4 (CNAs #4, #5, #6, and #7)...
Read full inspector narrative →
Dec 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide activities of daily living (ADL; activities related to pers...
Read full inspector narrative →
Oct 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to provide quality of care for 1 (R #5) of 3 (R #5, 6, and 7) residents...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to notify the family member/Power of Attorney (POA; a power of attorney grants, in writing, a particular agent the power to make healthcare de...
Read full inspector narrative →
Jan 2024
1 deficiency
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Pressure Ulcer Prevention
(Tag F0686)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to:
1. Provide oversight of shower sheets to identify wounds,
2. Accur...
Read full inspector narrative →
Jan 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview the facility failed to provide adequate supervision for 1 (R #1) of 3 (R #1-3...
Read full inspector narrative →
Dec 2023
3 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, observation, and record review, the facility failed to develop a comprehensive care plan for 2 (R #3 and R #...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to meet professional standards of quality by not maintaining accurate ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview the facility failed provide quality care for Foley Catheters (a flexible tube...
Read full inspector narrative →
Oct 2023
22 deficiencies
1 IJ
CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide the required supervision for 1 (R #74) of 3 (R...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation and interview the facility failed to ensure for 1 (R #104) of 1 (R #104) resident reviewed for dignity was not shaved as frequently as R #104 would like. This deficient practice c...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to notify facility management (Center Executive Director (CED) and Director of Nursing (DON)), the facility physician, and the representative/P...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to provide a safe, functional, and comfortable environment for 1 (R #118) of 1 (R #118) resident, as identified by the facility census provided ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to:
1. Administer medications as ordered by a physician and;
2. Notify...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to provide an ongoing activity program to meet the resident's interests and support residents' psychosocial well-being for 1 (R ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to provide quality care for 1 (R #6) of 1 (R #6) resident due to the facility not fixing or replacing the resident's wheelchair. This deficien...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to effectively manage pain for 1 (R #87) of 1 (R #87) residents review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure that residents have the right to make treatment decisions based on their individuals needs and understanding for 2 (R #35 and R # 87...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected multiple residents
G. On 10/11/23 at 11:53 am, during an observation of R #15's room revealed one bottle of Nystatin powder on his bedside table.
H. On 10/11/23 at 11:55 am, during an interview, R #15 revealed staff lef...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, the facility failed to promote resident self determination through support of resident choice for 9 (R #s 2, 3, 20, 58, 85, 86, 94, 98, and 139) of 9...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on record review and interview, the facility failed to:
1. Update the EHR (Electronic Health Record) to match MOST forms ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to develop an accurate and implement a comprehensive person-centered c...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide care plan meetings on a quarterly basis for 2 (R #39 and R ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to meet professional standards of care for 2 (R #15 and R #118) of 3 (R #15 and R #118) residents reviewed for respiratory care ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to inquire about daily meal preferences for 6 (R #'s 2, 18, 26, 32, 68, and 85) of 6 (R #'s 2, 18, 26, 32, 68, and 85) residents...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
.
Based on observation, record review, and interview, the facility failed to provide sufficient nursing staff to:
1. Assist residents in getting dressed to go eat in the dining room;
2. Assist resid...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected most or all residents
Based on observations and interviews the facility failed to:
1. Ensure that opened and accessed (has been opened and used) insulin flex pens were dated as to when they were initially opened by nursing...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to:
1. Discard fresh produce that was older than seven (7) days;
2. Document a date on prepared food;
3. Place a splash guard on the bottom shel...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on observation, record review and interview, the facility failed to maintain proper infection prevention measures by:
1. Performing hand hygiene between residents.
This deficient practice could...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected most or all residents
Based on interview, the facility failed to ensure staff implemented a comprehensive antibiotic stewardship program (The effort to measure and improve how antibiotics are prescribed by clinicians and u...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0882
(Tag F0882)
Could have caused harm · This affected most or all residents
Based on interview the facility failed to have a qualified, trained, or Certified Infection Preventionist. This deficient practice could likely to affect all 144 residents identified on the census pro...
Read full inspector narrative →
Apr 2023
4 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure that residents are free from neglect for 1 (R #10) of 3 (R #...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure that residents received appropriate and safe transfer assistance for 1 (R #15) of 1 (R #15) resident reviewed for accidents. This de...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure that medical records/medication administration record (MAR) were complete and accurate for 1 (R #10) of 1 (R #10) resident reviewed ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected multiple residents
Based on record review and interview, the facility failed to obtain and administer medications to 2 (R #12 and 15) of 2 (R #12 and 15) residents reviewed for medication errors. This deficient practice...
Read full inspector narrative →
Aug 2022
18 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on record review, observation, and interview the facility failed to ensure a resident was treated with respect and dignity for 1 (R #118) of 1 (R #118) resident reviewed for dignity by not dress...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Requirements
(Tag F0622)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review the facility failed to document in the resident record for 1 (R #120) of 1 (R #120) residen...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to develop a baseline care plan within 48 hours that would provide inf...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on interview and record review, the facility failed to change the urine collection bag as required for 1 (R #37) of 1 (R #37) resident reviewed for incontinence care was noted to be incontinent ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
Based on interview and record review the facility failed to follow through with a needed dental appointment for 1 (R #13) of 1 ( R #13) resident reviewed for dental care. This deficient practice could...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0561
(Tag F0561)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure that a resident was getting in and out of bed according to his preferences for 1 (R #113) of 1 (R #113) resident revie...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to revise the care plans for 2 (R #33 and 39) of 4 (R #33, 39, 66, and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Findings for #113
I. Record review of R #113's face sheet revealed R #113 is diagnosed with the following conditions: paraneopla...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation, and interview the facility failed to ensure treatment or services that met that resident's ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Findings for R #8:
L. On 07/27/22 at 10:30 am, during an interview, R #8 stated I misplaced my glasses. I need glasses.
M. Reco...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to monitor and treat pressure ulcers (areas of damaged skin caused by ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure that resident's received restorative [a nursin...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Findings for R #89:
J. A record review of R #89's face sheet revealed the following diagnoses: muscle weakness (generalized) and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and interview the facility failed to provide all care needed to prevent complications with use of Gastrosto...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0712
(Tag F0712)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to maintain a process that would allow each resident the opportunity t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interview, the facility failed to ensure the medication error rate did not exceed 5% by...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to adhere to a process that would allow residents the ability to communicate for 1 [R #8] of 3 [R #'s 2, 8, and 80] residents re...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to store and serve food under sanitary conditions by not ensuring:
1. Food items stored in facilities refrigerators were labeled and dated,
2. ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 4 life-threatening violation(s), 2 harm violation(s), $167,434 in fines. Review inspection reports carefully.
- • 68 deficiencies on record, including 4 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $167,434 in fines. Extremely high, among the most fined facilities in New Mexico. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Bear Canyon Rehabilitation Center's CMS Rating?
CMS assigns Bear Canyon Rehabilitation Center an overall rating of 2 out of 5 stars, which is considered below average nationally. Within New Mexico, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Bear Canyon Rehabilitation Center Staffed?
CMS rates Bear Canyon Rehabilitation Center's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 68%, which is 22 percentage points above the New Mexico average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs. RN turnover specifically is 76%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Bear Canyon Rehabilitation Center?
State health inspectors documented 68 deficiencies at Bear Canyon Rehabilitation Center during 2022 to 2025. These included: 4 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 2 that caused actual resident harm, and 62 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Bear Canyon Rehabilitation Center?
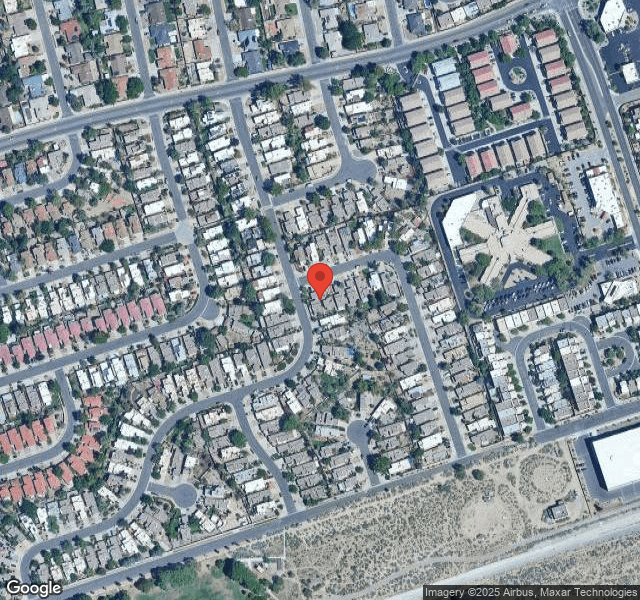
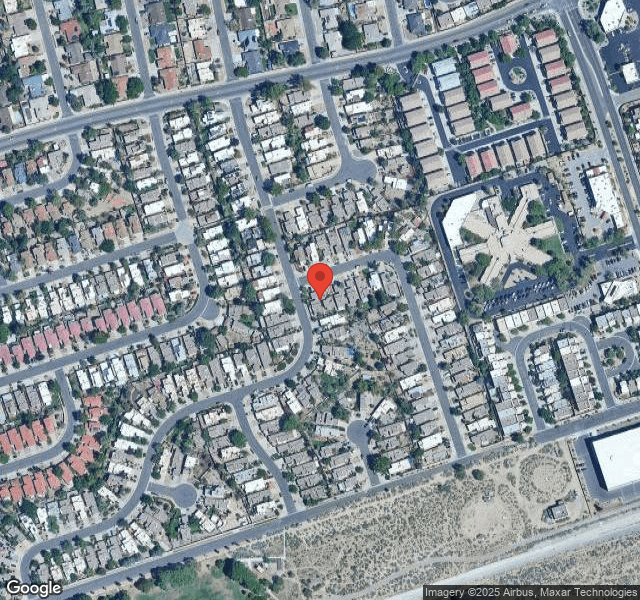
Bear Canyon Rehabilitation Center is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by GENESIS HEALTHCARE, a chain that manages multiple nursing homes. With 178 certified beds and approximately 116 residents (about 65% occupancy), it is a mid-sized facility located in Albuquerque, New Mexico.
How Does Bear Canyon Rehabilitation Center Compare to Other New Mexico Nursing Homes?
Compared to the 100 nursing homes in New Mexico, Bear Canyon Rehabilitation Center's overall rating (2 stars) is below the state average of 2.9, staff turnover (68%) is significantly higher than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Bear Canyon Rehabilitation Center?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the facility's high staff turnover rate, and the below-average staffing rating.
Is Bear Canyon Rehabilitation Center Safe?
Based on CMS inspection data, Bear Canyon Rehabilitation Center has documented safety concerns. Inspectors have issued 4 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in New Mexico. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Bear Canyon Rehabilitation Center Stick Around?
Staff turnover at Bear Canyon Rehabilitation Center is high. At 68%, the facility is 22 percentage points above the New Mexico average of 46%. Registered Nurse turnover is particularly concerning at 76%. RNs handle complex medical decisions and coordinate care — frequent RN changes can directly impact care quality. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Bear Canyon Rehabilitation Center Ever Fined?
Bear Canyon Rehabilitation Center has been fined $167,434 across 5 penalty actions. This is 4.8x the New Mexico average of $34,753. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Bear Canyon Rehabilitation Center on Any Federal Watch List?
Bear Canyon Rehabilitation Center is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.