CONTINUING HEALTHCARE AT BECKETT HOUSE




Inspected within the last 6 months. Data reflects current conditions.
Continuing Healthcare at Beckett House has received a Trust Grade of F, indicating significant concerns about the quality of care provided. It ranks #641 out of 913 nursing homes in Ohio, placing it in the bottom half of facilities statewide, and #3 out of 7 in Muskingum County, meaning only two local options are better. While the facility is improving, having reduced issues from 22 in 2024 to 8 in 2025, it still reported serious deficiencies, including a resident who developed sepsis from an untreated urinary tract infection and another who suffered a fractured hip due to insufficient assistance during a transfer. Staffing has a 2 out of 5 stars rating but shows a turnover rate of 39%, which is better than the state average. However, the facility has been fined $44,060, which is concerning and suggests ongoing compliance problems. Overall, while there are some strengths in staffing stability, the serious incidents and Trust Grade indicate considerable weaknesses that families should consider carefully.
- Trust Score
- F
- In Ohio
- #641/913
- Safety Record
- Moderate
- Inspections
- Getting Better
- Staff Stability ○ Average
- 39% turnover. Near Ohio's 48% average. Typical for the industry.
- Penalties ○ Average
- $44,060 in fines. Higher than 70% of Ohio facilities. Some compliance issues.
- Skilled Nurses ⚠ Watch
- Each resident gets only 27 minutes of Registered Nurse (RN) attention daily — below average for Ohio. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 51 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
-
Staff turnover below average (39%)
9 points below Ohio average of 48%
Facility shows strength in quality measures, fire safety.
The Bad
Below Ohio average (3.2)
Below average - review inspection findings carefully
Near Ohio avg (46%)
Typical for the industry
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 51 deficiencies on record
Jun 2025
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0605
(Tag F0605)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interview, the facility failed to ensure a psychotropic medication had a 14 day stop date. This affected one resident (#14) of five residents reviewed for un...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to clean a dependent resident's eyeglasses. This affected one resident (#23) of four residents reviewed for activities of daily ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility pharmacist failed to identify a psychotropic medication needed a 14 day stop date. This affected one resident (#14) of five residents reviewed for un...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, and staff interview, the facility failed to ensure accurate documentation in the me...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation of medication administration, and staff interview , the facility failed to ensure proper hand washing was completed during medication administration. This affected two residents (...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
2. Observation on 06/09/25 at 12:13 P.M. of Resident #42 and #224's room revealed a dark yellow orange stain in front of toilet, two broken linoleum with a raised uneven floor by Resident #42's chair ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
Based on the interview and resident council meeting minute review the facility failed to provide preferred resident activities including community outings to residents in the facility. This affected t...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0680
(Tag F0680)
Minor procedural issue · This affected most or all residents
Based on the review of the facility job description, personnel record review and staff interview, the facility failed to ensure the Activities Director was qualified for the position. This had the pot...
Read full inspector narrative →
Dec 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review, and interview, the facility failed to maintain a clean and safe living environment ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, medical record review, and policy review, the facility failed to provide adequate incontinence ...
Read full inspector narrative →
Jun 2024
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure residents received showers per their preferences. This affec...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and policy review the facility failed to maintain residents' personal living space in a comfortable, homelike manner. This affected two residents (Resident #4 and #62...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review, review of glucometer manufacturer information, policy review, and interview, the fa...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected most or all residents
Based on observations, interviews, and interviews, the facility failed to ensure the windows were kept in good repair. This had the potential to affect all residents residing in the facility. The cens...
Read full inspector narrative →
Mar 2024
16 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Incontinence Care
(Tag F0690)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, hospital record review, and interviews, the facility failed to ensure Resident #23 received adequate car...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure residents were properly assessed for restraints...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Record review revealed Resident #26 was admitted to the facility on [DATE] with diagnoses including epilepsy, major depressio...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Record review revealed Resident #15 was admitted to the facility on [DATE] with diagnoses including multiple sclerosis, anemi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview, the facility failed to ensure Residents #15, #26, and #46 had quarterly care ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Record review revealed Resident #27 was admitted to the facility on [DATE] with diagnoses including atherosclerotic heart dis...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, hospital record review, observation, and interview the facility failed to ensure wounds were properly id...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide Resident #15 with an optometry consult. This affected one r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, interviews, and policy review the facility failed to ensure pressure relieving inte...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, and interviews the facility failed to ensure foot care was provided for a resident. This af...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to provide range of motion services for residents. This affected two r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, interview, and policy review the facility failed to ensure
appropriate storage of ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0790
(Tag F0790)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, facility failed to provide dental services to residents. This affected two residents (#26,...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Dental Services
(Tag F0791)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Record review revealed Resident #15 was admitted to the facility on [DATE] with diagnoses including multiple sclerosis, anemi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, McGreer's criteria review, and interview, the facility failed to ensure the criteria was met prior to an...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and interview, the facility failed to store and prepare food under sanitary conditions. This had the potential to affect 56 of 57 residents who received food from the facility. Th...
Read full inspector narrative →
Jan 2023
7 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
Based on record review, interview, and policy review the facility failed to ensure a resident's physician was contacted when an antibiotic medication was not available to start. This affected one Resi...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on record review, policy review, and interview, the facility failed to complete a post-fall risk assessment. This affected one (Resident #10) of three residents reviewed for falls. The facility ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, record review, interview, and policy review the facility failed to ensure treatment and care was provided to residents with indwelling urinary catheters in the treatment and prev...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, policy review, and interview, the facility failed to ensure a medical record was complete regarding a re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Antibiotic Stewardship
(Tag F0881)
Could have caused harm · This affected 1 resident
Based on record review, interview, and policy review the facility failed to ensure a resident met the requirement for an antibiotic medication prior to initiation. This affected one Resident (#38) of ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected most or all residents
Based on record review, policy review, and interview, the facility failed to ensure the call light system was properly functioning and not purposefully disabled by staff, to allow the residents to cal...
Read full inspector narrative →
MINOR
(C)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Minor Issue - procedural, no safety impact
Staffing Information
(Tag F0732)
Minor procedural issue · This affected most or all residents
Based on observation and interview the facility failed to ensure daily staffing levels were posted for three consecutive days. This had the potential to affect all 55 residents in the facility.
Findin...
Read full inspector narrative →
May 2022
14 deficiencies
1 Harm
SERIOUS
(G)
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review and interview the facility failed to ensure Resident #48 was provided adequate assistance du...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview the facility failed to ensure Resident #253 and Resident #254 received and signed the...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected 1 resident
Based on record review, review of a facility Self-Reported Incident (SRI), facility policy and procedure review and interview the facility failed to prevent the misappropriation of the anti-anxiety me...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, review of Pre-admission Screening and Resident Review (PASARR) documentation and interview the facility ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview the facility failed to ensure Resident #5, who was assessed to require staff assistance for activities of daily living (ADL) care received adequate an...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Review of Resident #202's medical record revealed the resident was admitted to the facility on [DATE] with diagnoses includin...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on record review, review of facility policy and procedure and interview the facility failed to properly assess Resident #48's skin upon admission, timely identify a pressure area and implement a...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to provide supplements as ordered to Resident #44 who had experienced w...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, facility policy and procedure review and interview the facility failed to ensure Resident #...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview the facility failed to complete pre-dialysis and post-dialysis assessments for Resident #44...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record review, facility policy and procedure review and interview the facility failed to discontinue the medication Acidophilus for Resident #46 timely after a pharmacy recommendation/physici...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to ensure adequate justification for the increase in the medication Depakote prescribed for Resident #51 for agitation related to bipolar disor...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, record review, facility policy and procedure review and interview the facility failed to maintain Resident...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, review of the facility timeline for positive COVID-19 residents and staff, review of resident vaccination ...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • 39% turnover. Below Ohio's 48% average. Good staff retention means consistent care.
- • 51 deficiencies on record, including 2 serious (caused harm) violations. Ask about corrective actions taken.
- • $44,060 in fines. Higher than 94% of Ohio facilities, suggesting repeated compliance issues.
- • Grade F (35/100). Below average facility with significant concerns.
About This Facility
What is Continuing Healthcare At Beckett House's CMS Rating?
CMS assigns CONTINUING HEALTHCARE AT BECKETT HOUSE an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Ohio, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Continuing Healthcare At Beckett House Staffed?
CMS rates CONTINUING HEALTHCARE AT BECKETT HOUSE's staffing level at 2 out of 5 stars, which is below average compared to other nursing homes. Staff turnover is 39%, compared to the Ohio average of 46%. This relatively stable workforce can support continuity of care. RN turnover specifically is 56%, which is notably high. RNs provide skilled clinical oversight, so turnover in this role can affect medical care quality.
What Have Inspectors Found at Continuing Healthcare At Beckett House?
State health inspectors documented 51 deficiencies at CONTINUING HEALTHCARE AT BECKETT HOUSE during 2022 to 2025. These included: 2 that caused actual resident harm, 47 with potential for harm, and 2 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates Continuing Healthcare At Beckett House?
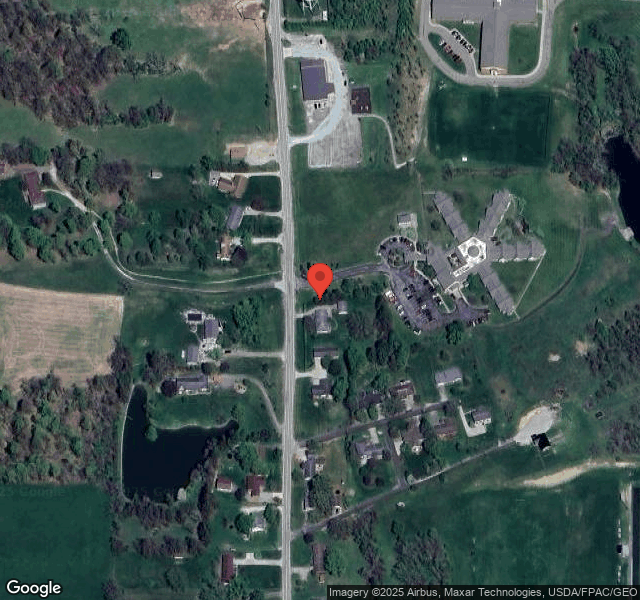
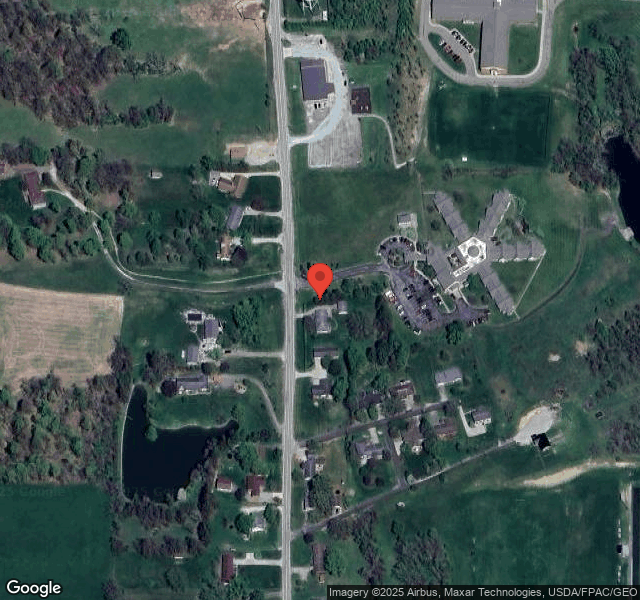
CONTINUING HEALTHCARE AT BECKETT HOUSE is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by CERTUS HEALTHCARE, a chain that manages multiple nursing homes. With 85 certified beds and approximately 72 residents (about 85% occupancy), it is a smaller facility located in NEW CONCORD, Ohio.
How Does Continuing Healthcare At Beckett House Compare to Other Ohio Nursing Homes?
Compared to the 100 nursing homes in Ohio, CONTINUING HEALTHCARE AT BECKETT HOUSE's overall rating (2 stars) is below the state average of 3.2, staff turnover (39%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Continuing Healthcare At Beckett House?
Based on this facility's data, families visiting should ask: "Can you walk me through typical staffing levels on day, evening, and night shifts?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the below-average staffing rating.
Is Continuing Healthcare At Beckett House Safe?
Based on CMS inspection data, CONTINUING HEALTHCARE AT BECKETT HOUSE has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Ohio. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at Continuing Healthcare At Beckett House Stick Around?
CONTINUING HEALTHCARE AT BECKETT HOUSE has a staff turnover rate of 39%, which is about average for Ohio nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Continuing Healthcare At Beckett House Ever Fined?
CONTINUING HEALTHCARE AT BECKETT HOUSE has been fined $44,060 across 1 penalty action. The Ohio average is $33,519. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Continuing Healthcare At Beckett House on Any Federal Watch List?
CONTINUING HEALTHCARE AT BECKETT HOUSE is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.