LAFAYETTE MANOR, INC




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Lafayette Manor, Inc. has a Trust Grade of F, which indicates significant concerns and places it in the poor category. It ranks #448 out of 653 nursing homes in Pennsylvania, putting it in the bottom half of facilities statewide, and #4 out of 7 in Fayette County, meaning only three local options are worse. While the facility's trend is improving, with issues decreasing from 21 in 2024 to 3 in 2025, it still faces serious challenges. Staffing is average with a 3 out of 5 star rating, but the turnover rate is concerning at 59%, higher than the Pennsylvania average. Families should note that the facility has had incidents, such as failing to check the dish machine temperature which could lead to foodborne illness, and not following proper infection control practices during dressing changes. Overall, while there are some signs of improvement, potential residents and their families should weigh these concerns carefully.
- Trust Score
- F
- In Pennsylvania
- #448/653
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 59% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ○ Average
- $11,536 in fines. Higher than 71% of Pennsylvania facilities. Some compliance issues.
- Skilled Nurses ○ Average
- Each resident gets 36 minutes of Registered Nurse (RN) attention daily — about average for Pennsylvania. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 33 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in fire safety.
The Bad
Below Pennsylvania average (3.0)
Below average - review inspection findings carefully
13pts above Pennsylvania avg (46%)
Frequent staff changes - ask about care continuity
Below median ($33,413)
Minor penalties assessed
11 points above Pennsylvania average of 48%
The Ugly 33 deficiencies on record
Aug 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observations, review of clinical records, and staff interview it was determined that the facility failed to provide reasonable accommodation of needs for five of 25 residents reviewed (Reside...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observations, review of facility policy, resident, and staff interviews, it was determined that the facility failed to provide a safe, clean, comfortable, and homelike environment on two of t...
Read full inspector narrative →
Jun 2025
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
Based on the review of facility policy, observations, clinical records, and staff interviews, it was determined that the facility failed to accurately document meal consumption for six of seven reside...
Read full inspector narrative →
Sept 2024
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff interview, and observation, it was determined that the facility failed to provide an envi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0947
(Tag F0947)
Could have caused harm · This affected 1 resident
Based on review of facility policy, staff education records, and staff interview, it was determined that the facility failed to conduct at least 12 hours of in-service education, within 12 months of t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected multiple residents
Based on a review of facility policy, clinical records, and incident investigation documents, it was determined that the facility failed to ensure that residents are free from misappropriation of prop...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected multiple residents
Based on a review of resident chosen menus, observations, resident council minutes and meeting and resident and staff interview it was determined that the facility failed to follow resident food prefe...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0865
(Tag F0865)
Could have caused harm · This affected multiple residents
Based on review of facility documentation, review of cited deficiencies from the facility's abbreviated survey of 5/24/24, and staff interview, it was determined that the facility's Quality assurance ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected multiple residents
Based on review of facility policy and documents, and staff interview, it was determined that the facility failed to provide training on Abuse, Neglect, and Exploitation for five of ten staff members ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0945
(Tag F0945)
Could have caused harm · This affected multiple residents
Based on review of facility documents and staff interview, it was determined that the facility failed to provide training on infection control for six of ten staff members (Employees E8, E12, E14, E15...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on a review of facility policies, observations and staff interviews it was determined that the facility failed to verify the washing temperature of the dish machine in the main kitchen, which cr...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
Based on review of facility policy, observations and staff interviews, it was determined that the facility failed to maintain infection control practices to prevent the potential for cross contaminati...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Transfer Notice
(Tag F0623)
Minor procedural issue · This affected multiple residents
Based on a review of federal regulation and staff interview, it was determined that the facility failed to provide transfer notices to representatives of the Office of the Long-Term Care Ombudsman Div...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0726
(Tag F0726)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of facility policy, nursing staff personnel records, nurse training documentation and staff interview, it was de...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0730
(Tag F0730)
Minor procedural issue · This affected multiple residents
Based on review of facility policy, personnel records, and staff interview it was determined that the facility failed to complete annual performance evaluations for five out of five nurse aides (NA Em...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0941
(Tag F0941)
Minor procedural issue · This affected multiple residents
Based on review of facility documents and staff interview, it was determined that the facility failed to provide Communication training to five of ten direct care facility staff reviewed (Employees E1...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0942
(Tag F0942)
Minor procedural issue · This affected multiple residents
Based on review of facility documents and staff interview, it was determined that the facility failed to provide training on resident rights for six of ten staff members (Employees E8, E12, E14, E15, ...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0944
(Tag F0944)
Minor procedural issue · This affected multiple residents
Based on review of facility documents and staff interview, it was determined that the facility failed to provide Quality Assurance and Performance Improvement (QAPI) training to five of ten facility s...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0946
(Tag F0946)
Minor procedural issue · This affected multiple residents
Based on review of facility policy and documents, and staff interview, it was determined that the facility failed to provide training on compliance and ethics for six of ten staff members (Employees E...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Deficiency F0949
(Tag F0949)
Minor procedural issue · This affected multiple residents
Based on review of facility documents and staff interview, it was determined that the facility failed to provide training on behavioral health for ten of ten staff members (Employees E8, E9, E10, E11,...
Read full inspector narrative →
May 2024
4 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of facility policy, clinical record review, and resident and staff interview, it was determined that the facilit...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on a review of CDC (U.S. Centers for Disease Control and Prevention) documents, facility policy, clinical record review, o...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0602
(Tag F0602)
Could have caused harm · This affected multiple residents
Based on a review of facility policy, clinical records, and incident investigation documents, it was determined that the facility failed to ensure that residents are free from misappropriation of prop...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on review of facility policy, resident observations, resident interviews and confidential staff interviews, and grievance review, it was determined that the facility failed to have sufficient nu...
Read full inspector narrative →
Oct 2023
5 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the facility policy, clinical record and staff interview, it was determined that the facility failed to devel...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0742
(Tag F0742)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical records and facility policy review, and staff interview, it was determined that the facility failed to ensure ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review and staff interview, it was determined that the facility failed to ensure a medication regime wa...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on the review of facility policy, clinical records and staff interviews, it was determined that the facility failed to mai...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of facility policies, clinical records,facility submitted documents, facility investigation information and staf...
Read full inspector narrative →
Oct 2022
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of facility policy, clinical records, facility documents, and staff interview, it was determined that the facili...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on review of facility policy, clinical record review, and resident and staff interviews, it was determined that facility staff failed to make certain physician orders were followed for one of se...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on observations, interview and facility policy, the facility failed to ensure medications were given according to manufacturer's guidelines resulting in a significant medication error for one of...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and review of facility policy, the facility failed to store medications according to manufacture...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What safeguards are in place to prevent abuse and neglect?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding. Review inspection reports carefully.
- • 33 deficiencies on record. Higher than average. Multiple issues found across inspections.
- • $11,536 in fines. Above average for Pennsylvania. Some compliance problems on record.
- • Grade F (28/100). Below average facility with significant concerns.
About This Facility
What is Lafayette Manor, Inc's CMS Rating?
CMS assigns LAFAYETTE MANOR, INC an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Pennsylvania, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Lafayette Manor, Inc Staffed?
CMS rates LAFAYETTE MANOR, INC's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 59%, which is 13 percentage points above the Pennsylvania average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at Lafayette Manor, Inc?
State health inspectors documented 33 deficiencies at LAFAYETTE MANOR, INC during 2022 to 2025. These included: 25 with potential for harm and 8 minor or isolated issues.
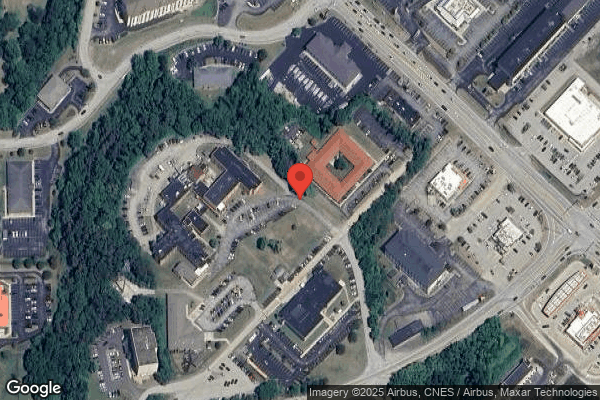
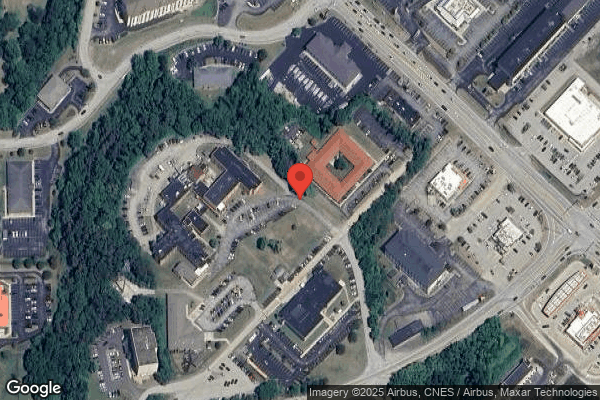
Who Owns and Operates Lafayette Manor, Inc?
LAFAYETTE MANOR, INC is owned by a non-profit organization. Non-profit facilities reinvest revenue into operations rather than distributing to shareholders. The facility operates independently rather than as part of a larger chain. With 98 certified beds and approximately 81 residents (about 83% occupancy), it is a smaller facility located in UNIONTOWN, Pennsylvania.
How Does Lafayette Manor, Inc Compare to Other Pennsylvania Nursing Homes?
Compared to the 100 nursing homes in Pennsylvania, LAFAYETTE MANOR, INC's overall rating (2 stars) is below the state average of 3.0, staff turnover (59%) is significantly higher than the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Lafayette Manor, Inc?
Based on this facility's data, families visiting should ask: "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the substantiated abuse finding on record and the facility's high staff turnover rate.
Is Lafayette Manor, Inc Safe?
Based on CMS inspection data, LAFAYETTE MANOR, INC has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Pennsylvania. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Lafayette Manor, Inc Stick Around?
Staff turnover at LAFAYETTE MANOR, INC is high. At 59%, the facility is 13 percentage points above the Pennsylvania average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Lafayette Manor, Inc Ever Fined?
LAFAYETTE MANOR, INC has been fined $11,536 across 2 penalty actions. This is below the Pennsylvania average of $33,194. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Lafayette Manor, Inc on Any Federal Watch List?
LAFAYETTE MANOR, INC is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.