CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure that each resident received adequate supervi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure that each resident received adequate supervision to prevent accidents for one (Resident #1) of 1 resident reviewed for supervision.
The facility failed to ensure Resident #1 received adequate supervision while Resident #1 was unaccounted for approximately 15 minutes from 6:00 PM to 6:15 PM on 10/07/24 before a 3rd party called to notify the facility that Resident #1 was walking through a field adjacent to the facility.
On 10/18/24 at 2:27 PM, an Immediate Jeopardy (IJ) was identified. While the IJ was removed on 10/19/24 at 1:25 PM, the facility remained out of compliance at a scope of isolated and a severity level of no actual harm with potential for more than minimal harm that was not immediate jeopardy due to the facility's continuing to monitor the implementation and evaluate the effectiveness of their Plan of Removal.
This failure could place residents requiring supervision at risk for injury and accidents with potential for more than minimal harm.
Findings included:
Record review of Resident #1's face sheet revealed an [AGE] year-old male with an original admission date of 10/15/22 and a current admission date of 05/28/24. Pertinent diagnoses included Alzheimer's disease, Dementia, and Unsteadiness on Feet.
Record review of Resident #1's Comprehensive MDS assessment section C, cognitive patterns, dated 10/01/24 revealed a BIMS score of 3 (severe impairment).
Record review of Resident #1's care plan revealed the focus Resident is at risk for falls D/T CONFUSION initiated on 10/15/22 and revised on 10/17/22. Interventions listed for this focus included:
Assist with ADLs as needed initiated on 10/15/22.
Call light within reach initiated on 10/15/22.
Complete fall risk assessment initiated on 10/15/22.
Orient resident to room initiated on 10/15/22.
Provide adaptive equipment or devices as needed initiated on 10/17/22.
Pt evaluate and treat as ordered or PRN initiated on 10/17/22.
SIDE RAILS: quarter rails up as ordered initiated on 10/17/22 and revised on 10/17/22
Further record review of Resident #1's care plan revealed the focus The resident has had an actual fall with no injury, d/t poor balance initiated on 05/18/24 and revised on 05/20/24. Interventions listed for this focus included:
For no apparent acute injury, determine and address causative factors of the fall initiated on 05/18/24 and revised on 05/20/24.
Neuro-checks as per protocol initiated on 05/18/24 and revised on 05/20/24.
Observe/report PRN x 72h to MD for s/sx: Pain, bruises, change in mental status, new onset: confusion, sleepiness, inability to maintain posture, agitation initiated on 05/18/24 and revised on 05/20/24.
Physician ordered UA&C/S for resident initiated on 05/18/24.
Resident education on using his cane for support initiated on 05/18/24 and revised on 05/20/24.
Record review revealed Resident #1's elopement risk assessment dated [DATE] indicated he was not a risk for elopement at that time. Further record review revealed Resident #1's elopement risk assessment dated [DATE] indicated he was a risk for elopement at that time.
Record review of the provider investigation report dated 10/11/24 revealed the following narrative:
Resident was seen by charge nurse a few minutes before 6pm walking from dining room down the hallway. At 615pm Charge nurse received a call from a woman stating there was an elderly man looking like a patient of ours walking in the back field towards the fire station all in brown and was he ours? Charge nurse [LVN K] asked the 2nd charge nurse if she was missing anyone and both nurses started looking at their residents. As the staff kept looking [LVN K] quickly got in her car and drove down the street and a fireman and the lady were sitting with the resident unharmed and he stated that he was looking for his work. [LVN K] brought him safely back. Resident was in the facility at 643pm. [QAPI] and CP updated for Elopement. Elopement audit for all residents. Code change for doors and ambulance door change to lobby door. 1x1 [one to one monitoring of the resident by facility staff].
Further review of the provider investigation report revealed a witness statement written as follows by LVN C on 10/08/24:
330pm- [Resident #1] came to nurses station to ask for coffee, we told him it was not ready yet and he left the nursing area.
Approx 615pm- I was coming up from the 300hall and [LVN K] told me a lady just called and said she saw a man wearing brown walking through the grassy area by our building. Went down my hall to look for all my residents, I looked out the back door and I did not see anything. Spoke with [CNA L] and he stated the alarm had sounded but he did not notice anything unusual, thought it was a family member. I went back to nurses station and saw [Unknown CNA] come back from the dining room and then we went to go look outside the facility at this time. We did not notice any residents in the surrounding area. I came back in and notified [LVN K] I did not have any missing residents and I didn't see anyone outside.
Further review of the provider investigation report revealed a witness statement written as follows by LVN K on 10/08/24:
Approx 6pm I saw [Resident #1] coming up 400 hall.
Approx 615pm I answered the phone and it was a lady stating she saw an older gentlemen walking through the grassy area by our building wearing brown.
We started checking the building for any missing residents. I took off in my vehicle to go drive around and look for him. I found him down [local road] with some fire fighters right passed the fire station. Resident was placed back in my vehicle and returned to facility. I assessed the resident from head to toe and notified all proper channels.
Further review of the provider investigation report revealed in-services covering Missing Residents/Actual Elopement Event were conducted for 65 staff members between 10/07/24 and 10/09/24 by the ADON.
In an interview with the DON on 10/27/24 at 2:25 PM, the DON stated Resident #1 had no history of exit seeking behavior prior to the elopement incident. The DON stated Resident #1 did not typically go outside. The DON stated Resident #1 was not allowed to go outside unsupervised. The DON stated LVN K called her after she had already found Resident #1 by the first station. The DON stated she did not know which exit Resident #1 used to leave the facility but was most likely the 100 hall exit door. The DON stated the alarm sounded on the 100 hall exit door around the time of the elopement. The DON stated she did not know who called the facility to report the elopement. The DON stated nobody in the facility was aware Resident #1 was missing until the facility was notified by the caller. The DON stated all exit doors in the facility had an electronic lock that required a code to exit. The DON stated since the incident the staff had been told not to use any of the exit doors at the rend of any residential halls. The DON stated they had an elopement drill on 10/08/24 at around 10:00 AM and they will continue to do them weekly for the next 4 weeks. The DON stated the emergency code for a missing resident was purple. The DON stated if purple was called, the charge nurse split up the staff with half of them searching outside the facility and the other half searching inside. The DON stated if they did not find the resident in a timely manner, they would notify the police. The DON stated all staff take part in the search for the missing resident. The DON stated there would be 25 to 30 staff members at the facility during the day and about 6 at night. The DON stated only staff should know the codes to the exit doors. The DON stated the last fall risk assessment performed on Resident #1 before the elopement was on 10/07/24 and received a score of 16. The DON stated a score of 10 or higher meant interventions should be initiated for the resident related to falls.
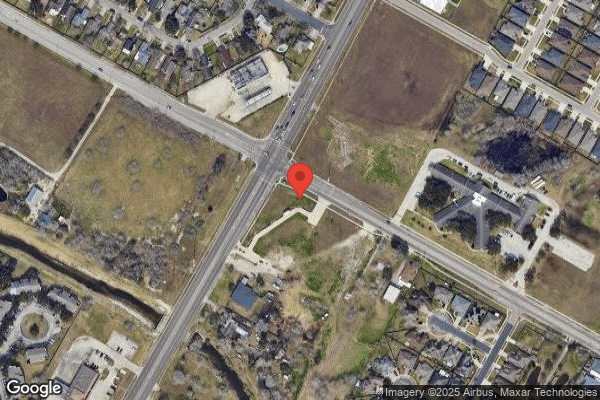
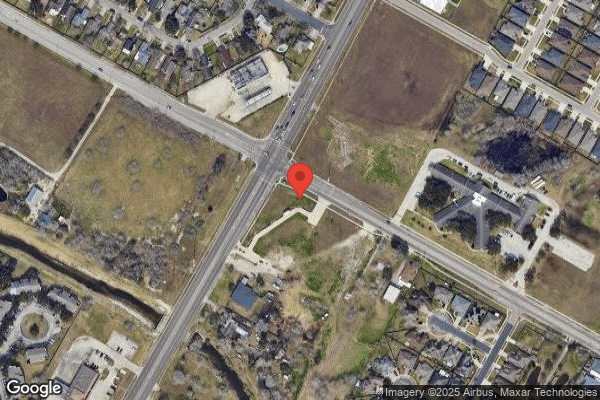
During an observation on 10/17/24 at 3:00 PM, this state surveyor walked from the 100 hall exit door to the local fire station where the missing resident was located. The distance across the field just outside the 100 hall was approximately 650 feet to a residential road, and then another 350 feet after crossing the road to the fire station.
In an interview with LVN C on 10/17/24 at 3:36 PM, LVN C stated the emergency color code for a missing resident was pink. LVN C stated a code pink indicated the staff should start looking everywhere for the missing resident. LVN C stated she would go through the rooms to see who was there or not. LVN C stated one of the nurses would delegate some people to go outside and others to stay inside. LVN C stated she would notify the police immediately after the resident was missing. LVN C stated she had not been part of an elopement drill since she had been working at the facility for 2 years. LVN C stated it had been weeks since her last in-service on elopements.
In an interview with HK L on 10/17/24 at 3:40 PM, HK L stated he had never taken from in an elopement drill at the facility. HK L stated he had an in-service 2 days ago covering elopement. HK L stated someone goes outside to look for the resident while others stay inside. HK L stated someone needed to notify the administrator and nurse. HK L stated the emergency color code for an elopement was silver.
In an interview with CNA M on 10/17/24 at 3:43 PM, CNA M stated the emergency color code for a missing resident was grey. CNA M stated a code grey indicated to all staff they needed to start looking for a missing resident. CNA M stated she would look in the rooms in her hall first. CNA M stated the charge nurse would be in charge during the elopement. CNA M stated some staff would search inside while others searched outside. CNA M stated she received an in-service 2 or 3 days ago covering elopements. CNA M stated she took part in an elopement drill 3 days ago.
In an interview with the AD on 10/17/24 at 3:43pm, the AD stated the code called overhead for a missing resident was Code Purple, and if it was called, all staff were to meet at the nurse's station where the DON or the ADM would let everyone know who they were looking for and assign tasks. The AD stated if the resident was not found within 25 minutes, the police department was to be called, and the resident reported missing. The AD stated the last drill and in-service were done last Thursday or Friday (10/10/24 or 10/11/24). The AD stated for the drill, the van driver went and hid, a code purple was called overhead, and everyone was assigned a task/area to look. The van driver was found outside hiding behind a bush.
In an interview with the SW on 10/17/24 at 3:49 PM, the SW stated she had only had one elopement drill since she had been working at the facility starting on 12/01/10. The SW stated when it first occurred, someone would get over the intercom and call out a code purple. The SW stated someone would go out the door that alarmed and look for the resident. The SW stated the administrator and RP were to be notified. The SW stated all the door codes had recently been changed and staff were no longer to use the exit doors on the resident's halls.
In an interview with RN N on 10/17/24 at 3:50, RN N stated the emergency color code for a missing resident was purple. RN N stated they would check outside while combing the patients inside and inform the DON. RN N stated whoever found out the resident was missing would be the one to take charge. RN N stated they would search inside and outside the facility at the same time. RN N stated if they could not find the resident within 10 minutes they would notify the police. RN N stated she received an elopement in-service 2 days ago. RN N stated it had been a few months since her last elopement drill.
In an interview with the MS on 10/17/24 at 3:53 PM, the MS stated he had worked at the facility for 19 years and that he had always conducted an elopement drill once every 3 months. The MS stated he conducted an elopement drill on 10/08/24 with all staff who were present on shift at 10:35 AM. The MS stated he had no records of ever conducting an elopement drill during night shift. The MS stated he checked the door locks and alarms weekly on all exit doors. The MS stated during door checks he pressed on the push bar from the inside for 15 seconds to ensure the alarm sounded and that the door would open. The MS stated after the door opened, he closed it back and entered the code to shut off the alarm. The MS stated he did not check the door functionality from the outside. The MS stated he was aware the door could be held open indefinitely without the alarm sounding if no one touched the push bar after the code was input.
In an interview with the ADM on 10/17/24 at 3:55 PM, the ADM stated they conducted an elopement in-service with 100% staff over the course of 10/07/24 and 10/08/24 right after the elopement occurred. The ADM stated she conducted another in-service with staff on 10/15/24. The ADM stated when an alarm went off, staff were supposed to go outside and check to make sure no residents went out. The ADM stated staff should notify the charge nurse the alarm went off to initiate a head count. The ADM stated she had the alarm codes changed after the incident, along with an elopement assessment conducted on every resident in the facility. The ADM stated the elopement assessment was changed to immediately notify them if it triggered. The ADM stated the most recent elopement drills were done on 10/08/24, 09/18/24 and 06/26/24. The ADM stated she did not know the last time night shift had an elopement drill. The ADM stated the emergency code for an elopement was purple. The ADM stated Resident #1 was put on a 1 to 1 a few months ago because he talked about wanted to leave for work. The ADM stated during that time Resident #1 never attempted to leave the facility or went near an exit door. The ADM stated it turned out Resident #1 had a urinary tract infection at that time, and once it was cleared up his behaviors improved and was taken off the 1 to 1. The ADM stated she did everything she could to prevent an immediate jeopardy situation.
In an interview with LVN Y on 10/18/24 at 9:45 AM, LVN Y stated resident elopement assessments were completed on entry, re-entry, after an event, quarterly, and annually. LVN Y stated the charge nurse on the floor should conduct the elopement risk assessment. LVN Y stated if the resident was overdue for an elopement risk assessment the nurse would see it in their chart as red indicating it was overdue.
In an interview with CNA L on 10/18/24 at 10:50 AM, CNA L stated he was in room [ROOM NUMBER] at the end of the hall when the alarm for the exit door on hall 100 sounded at approximately 6:00 PM on 10/07/24. CNA L stated he saw a family member at the other end of the hall and assumed they opened the door but came back inside. CNA L stated he did not recognize the visitor and never spoke to them. CNA L stated he did not look outside at that time. CNA L stated he received an in-service on elopements on 10/08/24. CNA L stated he did not know the emergency color code for a missing resident. CNA L stated he had not taken part in any elopement drills at the facility. CNA L stated the alarm was going off for about 10 minutes before he turned it off around 6:10 PM. CNA L stated he was not aware of anyone else checking on the alarm. CNA L stated LVN K saw him turn the alarm off. CNA L stated he did not know the elopement policy and he did not know Resident #1 was missing until LVN K had already brought him back in the building.
In an interview with LVN K on 10/18/24 at 3:40 PM, LVN K stated she was sitting at her computer in the nurse's station when she saw Resident #1 walking towards his room on the 200 hall. LVN K stated she received a call from a lady driving by the facility that stated she saw a male wearing all brown walking in the field adjacent to the facility. LVN K stated she remembered the alarm going off on the 100 hall but could not remember the time it occurred. LVN K stated the alarm went off 5 to 10 minutes before she received the phone call. LVN K stated the alarm sounded for a 1 to 2 minutes at the most. LVN K stated she observed CNA L go towards the 100 hall exit door, turned off the alarm and looked out the window. LVN K stated she did not speak to CNA L at that time. LVN K stated once she was informed that a resident was missing, CNA L and LVN C looked around the rooms while other staff started looking in common areas. LVN K stated no one went outside to look for Resident #1 at that time. LVN K stated since Resident #1 liked to wander into other resident's rooms they began looking for him there. LVN K stated Resident #1 had not been known to try to go outside or display exit seeking behaviors. LVN K stated after they could not find Resident #1 in the facility, she got in her personal vehicle and drove around the facility. LVN K stated she found the resident at a local fire station near the facility talking to firemen about trying to get to work. LVN K stated she thought someone might have let Resident #1 out a back door since family and visitors would use those exit doors on the halls. LVN K stated it took a while to get back to the facility because there was a lot of traffic at the time. LVN K stated she performed a head-to-toe assessment on Resident #1 once she got back to the facility and noted bruising to the left side of his head and bruising to his left elbow due to a fall earlier in the day. LVN K stated the bruising on Resident #1 did not look brand new. LVN K stated a code purple was not called during this incident because staff were around the nurse's station when the call came in and were aware Resident #1 was missing. LVN K stated she believed RN A did the assessment on Resident #1 after his fall earlier in the morning. LVN K stated she believed she had seen the bruise to Resident #1's head earlier in the day.
In an interview with RN A on 10/18/24 at 3:54 PM, RN A stated he did the head-to-toe assessment on Resident #1 after his fall earlier in the day on 10/07/24. RN A stated he did not find any injuries on Resident #1 during his assessment.
Record review of the facility policy Missing Resident/Actual Elopement Event revised on 04/05/23 and reviewed on 04/03/24 revealed the following:
1. A facility head count should be conducted whenever the following occurs;
a. When a door alarm has sounded, but there was no witness to the reason for the sounding of the alarm.
b. When the fire alarm goes into alarm to verify that all residents are accounted for.
c. Anytime the alarm system for the doors is not operational
2. If during a facility head count a resident is unaccounted for, proceed to step 4
3. If staff cannon account for the whereabouts of a resident, during the course of the day proceed to step 4.
4. The sign out log should be reviewed to determine if the resident or resident representative has signed out of the facility.
5. The time and location the resident was last seen and the clothing the resident was wearing should be determined.
6. The Executive Director or representative and all department heads are notified that the resident cannot be located. The executive Director may need to initiate a facility lockdown if determined it is needed by the Executive Director.
7. The charge nurse will assign staff to begin a coordinated search of the facility and facility grounds. Search the facility's grounds for the resident. If necessary, distribute copies of the resident's photograph to the staff searching the grounds. Keep a record of the areas searched.
8. Staff will be assigned to remain on the unit(s) and to utilize the roster/census sheet to establish the unit census and confirm the whereabouts of all other residents.
9. If the resident cannot be located, the charge nurses or designee will notify law enforcement immediately. Law enforcement personnel will then coordinate the search efforts.
10. The charge nurse or designee will notify the responsible party, the physician, and the medical director that the resident is missing.
Record review of the facility policy Unsafe Wandering and Elopement Prevention revised on 08/22/22 and reviewed on 09/25/24 revealed the following:
1. Accurate and thorough assessment of the resident is fundamental in determining indicators for unsafe wandering and elopement. Not all resident exhibit unsafe wandering behaviors or verbalize the desire to leave the facility unplanned.
a. A situation in which a resident with decision-making capacity leaves the facility intentionally would generally not be considered an elopement unless the facility is unaware of the resident's departure and/or whereabouts.
Record review of the undated facility policy Emergency Code Words revealed the following:
Code Purple - Missing Resident
An Immediate Jeopardy was identified on 10/18/24 at 2:27 PM. The IJ template was presented to the ADM, and a plan of removal was requested.
This was determined to be an Immediate Jeopardy (IJ) on 10/18/24 at 2:27 PM. The Administrator was notified. The IJ template was presented to the ADM on 10/18/24 at 2:27 PM. The following Plan of Removal was submitted by the facility and was accepted on 10/18/24 at 4:27 PM.
PLAN OF REMOVAL FOR IMMEDIATE JEOPARDY
Plan of Removal:
Regarding: IJ 10/18/2024
F 689 Free of Accidents / Hazards / Supervision
Failure: The facility failed to ensure the safety of Resident #1 by not providing supervision to prevent Resident #1 from eloping from the facility. On 10/7/2024 Resident #1 exited from the facility and was found near the fire department
Corrective action for those found to be affected by the alleged deficient practice:
o
Identified resident was discharged to a secured unit on 10/9/2024.
o
Clinical assessment of the resident after return to the unit was completed.
o
Completed incident report within the PCC system
o
Notified Medical Director and family of event.
o
Ensured all residents are present and in the building
o
Completed/ updated elopement assessment for resident that exited facility and updated his care plan.
Identification of others residents having the potential to be affected:
o
Elopement risk assessments were completed for all residents in the building.
Measures/Systemic Changes to ensure the deficient practice does not recur:
o
Complete elopement assessments for all residents that reside in the facility today, quarterly, significant change and new admissions to the facility.
o
Elopement drill was completed on 10/8/202 and will be completed weekly.
o
Obtained statements from staff members that were present during the incident
o
The following in-services were completed for staff on 10/7/24, 10/8/2024 and 10/15/2024
-Residents at risk for elopement
-What to do if a resident elopes
-Door security-with alarms, how to ensure door alarms are in place, how often to monitor door alarms, ensuring alarms are turned back on after turning off and exiting and ensuring doors are secure.
-Reporting guidelines with elopement
-Completing elopement assessments and updating care plans
o
A list of residents with potential for elopement will be placed at the nurse's station and reception desk, pictures of residents and information will be placed in that book to identify who is at risk. This will be updated quarterly and PRN
o
AD-hoc QAPI completed by DON-ED and Medical Director
o
Check all exterior doors to ensure alarms are functioning properly and document. This will be complete weekly and as needed.
o
Elopement drill to be completed weekly to include all 3 shifts.
o
Complete elopement assessments for all residents that reside in the facility quarterly, significant change and new admissions to the facility.
o
Door codes were changed on all exit doors.
o
Doors at the end of hallways are no longer used.
o
Further education initiated on 10/18/2024 to include Policy on unsafe wandering and Elopement Prevention.
o
Elopement drill completed on night shift 10/17/2024.
On going monitoring:
o
Elopement drills will be reviewed in monthly QAPI.
o
Elopement assessments will be reviewed 2-3 times per week in morning meeting.
o
All components of this plan of correction will be submitted to the facility QAPI committee meeting and additional recommendations will be made until substantial compliance has been achieved.
Verification of Plan of Removal
Interviews were conducted with RN O, CNA P, HK Q, CNA R, LVN J, RN A, RN S, CNA T, CNA U, CNA H, CNA G, CNA V, CNA W, DA X on 10/19/24 from 10:00 AM through 12:00 PM. All staff were able to identify the proper emergency color code for a missing resident. All staff stated the proper procedures if they responded to an elopement. All staff were knowledgeable on the changes implemented in the plan of removal.
In an interview with the MS on 10/19/24 at 12:03 PM, the MS stated all shifts were getting elopement drills once a week until all staff were knowledgeable, and administration felt all staff were competent on elopement procedures.
In an interview with the DON on 10/19/24 at 12:08 PM, the DON stated elopement drills were being conducted once per week for all 3 shifts. The DON stated elopement assessments were reviewed 2 to 3 times per week in the morning meetings to verify elopement drills were done and staff were knowledgeable on all elopement procedures. The DON stated the elopement procedures and implementation of training had been added to QAPI for review.
Record review and verification of the accepted POR:
Identified resident was discharged to a secured unit on 10/09/24 - Verified by record review through discharge list and interview with DON on 10/18/24.
Clinical assessment of the resident after return to the unit was completed - Verified by record review of progress notes and nurse assessments on 10/18/24.
Completed incident report within the PCC system - Verified by record review of incident reports on 10/18/24.
Notified Medical Director and family of event - Verified by record review of progress notes and interview with DON on 10/18/24.
Ensured all residents are present and, in the building - Verified by observation of all residents on a walkthrough of the facility on 10/18/24.
Completed/updated elopement assessment for resident that exited facility and updated his care plan - Verified by record review of Resident #1's elopement assessment and interview with DON on 10/18/24.
Identification of other residents having the potential to be affected - Verified by interview with DON on 10/18/24.
Elopement risk assessments were completed for all residents in the building - Verified by interview with DON on 10/18/24.
Measures/Systemic Changes to ensure the deficient practice does not recur - Verified by interview with DON on 10/18/24.
Complete elopement assessments for all residents that reside in the facility today, quarterly, significant change and new admissions to the facility - Verified by interview with DON on 10/18/24.
Elopement drill was completed on 10/18/24 and will be completed weekly - Verified by record review of elopement drill documentation sheet and interview with MS on 10/18/24.
Obtained statements from staff members that were present during the incident - Verified by record review of provider investigation and interviews of relevant staff on 10/18/24.
The following in-services were completed for staff on 10/7/24, 10/08/24, 10/15/24, and 10/18/24 - Verified by record review of in-service sign-in sheets and interviews with staff on 10/18/24 and 10/19/24:
What to do if a Resident Elopes
Door Security
Reporting Guidelines with Elopement
Complete Elopement Assessments and Updating Care Plans
Employees given a quiz beginning on 10/18/24 on Elopement Procedures - Verified by record review of the quiz and interview with ADM on 10/19/24.
A list of residents with potential for elopement will be placed at the nurse's station and reception desk, pictures of residents and information will be placed in that book to identify who is at risk. This will be updated quarterly, and PRN - Verified by observation of the new binder on 10/19/24.
Emergency QAPI was completed with Medical Director - Verified by record review of the QAPI minutes on 10/19/24.
Checking of all exterior doors to ensure alarms are functioning properly and document. This will be complete weekly and as needed - Verified by record review of the maintenance logs and interview with MS on 10/18/24 and 10/19/24.
Elopement drills to be completed weekly to include all 3 shifts - Verified by interview with MS on 10/19/24.
Complete elopement assessments for all residents that reside in the facility quarterly, significant change and new admissions to the facility - Verified by interview with DON on 10/18/24.
Door codes were changed on all exit doors. Verified by observation of input of old door codes and interview with MS on 10/18/24.
Doors at the end of hallways were no longer used. Verified by interviews with DON and ADM on 10/18/24.
Elopement drill completed on night shift 10/17/24 - Verified by record review of elopement drill documentation sheet and interview with MS on 10/18/24.
On going monitoring - Verified by interviews with DON and ADM on 10/19/24
Elopement drills will be reviewed monthly in QAPI - Verified by interview with DON on 10/19/24.
Elopement assessments will be reviewed 2-3 times per week in morning meetings - Verified by interviews with DON and ADON on 10/18/24.
All components of this plan of correction will be submitted to the facility QAPI committee meeting and additional recommendations will be made until substantial co[TRUNCATED]
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews, and interviews, the facility failed to ensure residents were treated with respect and dig...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, record reviews, and interviews, the facility failed to ensure residents were treated with respect and dignity and care for each resident in a manner and in an environment, that promoted maintenance or enhancement of his or her quality of life, for one (Resident #3) of five reviewed for dignity issues.
Resident #3's foley catheter drainage bag did not have a privacy bag, leaving the urine in the bag visually exposed to visitors, staff, and other residents.
This failure could place residents at risk of feeling uncomfortable and disrespected which could decrease residents' self-esteem and/or quality of life.
Findings were:
Record review of Resident #3's Face Sheet dated 10/12/2024 revealed Resident #3 was an [AGE] year-old male who was admitted on [DATE] with diagnoses of sepsis (infection), bacteremia (blood infection), and personal history of malignant neoplasm (cancer) of rectum (buttock).
Record review of Resident #3's Care Plan date initiated 09/09/2024 revealed the resident has an Indwelling Catheter. Goal: Will have no complications related to indwelling catheter use. Interventions: Catheter care every shift.
Record review of Resident #3's admission MDS dated [DATE] revealed a BIMS score of 14 and coded for an indwelling catheter. The MDS also revealed Resident #3 was dependent of staff for toileting hygiene, and partially dependent of staff for other activities of daily living.
During an observation on 10/12/2024 at 2:04PM and 2:28PM, Resident #3's room door was open and upon immediate observation there was visible urine in his urinary catheter. Upon further inspection there was a visibly full chamber of yellow urine with no privacy veil. Additionally, staff members, residents, and resident family members were observed to be walking pass Resident #3's room.
During an interview on 10/12/2024 at 2:32PM Resident #3 was asked the reasoning for his foley catheter and was additionally asked if he knew the foley urinary bag was visible from the hallway to which Resident #3 responded with incoherent sentences. Multiple attempts were made to interview Resident #3 with no success.
During an interview on 10/12/2024 at 2:35PM CNA B stated Resident #3 was not cognitively aware and had frequent moments of confusion. CNA B stated Resident #3 can feed himself independently but does need substantial assistance with majority of all other activities of daily living including toileting. CNA B stated Resident #3 frequently forgets the topic of his conversations. CNA B stated Resident #3 has a foley. CNA B stated she has worked at the facility since May 2024 and was still learning the facility's policy and procedures. CNA B stated Resident #3 has moments of agitation and confusion but was redirectable. CNA B stated she was unaware that Resident #3 was missing a privacy bag on his foley catheter, and continued by stating she does not regularly work on Resident #3's hallway CNA B stated she was aware that privacy bags for foley catheters were required and could not definitively state why Resident #3's foley urinary catheter did not have a privacy bag. When asked how Resident #3's psychosocial well-being could be impacted, CNA B did not verbalize a response. CNA B stated she was under the understanding that privacy bags were implemented by the nurses, and continued by stating privacy bags were used to maintain a resident's right to privacy. CNA B stated she could not recall attending any recent in-service regarding urinary catheter privacy bags.
During an interview on 10/12/2024 at 2:47PM RN A stated Resident #3 had a foley catheter placed during his previous hospitalization date unknown. RN A stated the foley catheter was placed due to urinary complications of urinary retention. RN A stated Resident #3 was very forgetful and was alert to self. RN A stated the CNAs will empty Resident #3's catheter of urine and report the numerical value to him while also documenting it in the resident's electronic health record. RN A stated while directly looking into Resident #3's room that he would place a privacy bag over Resident #3's foley catheter to maintain Resident#3's right to privacy. RN A stated Resident #3's foley catheter needed a privacy bags, and stated privacy bags were utilized to maintain a resident's right to privacy. RN A stated he tried to maintain privacy for all his patients. RN A stated by not utilizing a catheter privacy bag, Resident #3 could have potentially been affected negatively. RN A stated privacy bags were kept in their supply closet and it was the responsibility of the nurse to put them on the resident. RN A stated he will get the privacy bag and apply it right away. RN A stated he attended an educational in-service regarding catheter care, privacy bags within the past 2-3months and stated these in-services were done frequently.
During an interview on 10/14/2024 at 5:44PM the DON and the Administrator stated all resident foley catheters must have a privacy bag. Both stated Resident #3 has been in the facility for over a month. Both stated Resident #3 was sent out initially to the hospital for urinary complications date unknown and returned to the facility a month ago. The DON stated upon Resident #3's return, the clinical staff should have placed a privacy bag over Resident #3's urinary foley catheter. Both stated by the clinical staff failing to implement a privacy cover on Resident #3's foley urinary catheter, Resident #3's dignity may have been compromised, could have affected him negatively, and could have compromised his psychosocial well-being. Both stated they will conduct an impromptu privacy bag in-service to the nurses.
Record review of the facility's Resident Rights policy and procedure, within the Resident admission Agreement, review dated 2002, 2016, 2018, 2022, 2024 documented [NAME] of Rights 1. The resident has a right to a dignified existence .
43. The resident has a right to personal privacy and confidentiality of their personal and medical records.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure that residents received treatment and care in accordance wit...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure that residents received treatment and care in accordance with professional standards of practice and the comprehensive person-centered care plan for one (Resident #12) of five residents reviewed for quality of care.
The facility failed to present consistent accurate and detailed assessments of Resident #12's progressive injuries on 07/09/2024 after an unwitnessed fall, as an effort to ensure appropriate treatment was developed. There was no documented progress note, or skin assessments in Resident #12's electronic health record, detailing the injuries mentioned in Resident #12's 07/09/2024 emergency room transfer form, or incident report.
This failure could place residents at risk of not receiving appropriate and timely medical interventions which could result in a decline in resident's condition, the need for hospitalization, or death.
The findings included:
Record review of Resident #12's admission record dated 10/14/2024 revealed Resident #12 was initially admitted on [DATE] and was an [AGE] year-old female with medical diagnoses of: displaced fracture of first cervical vertebra, subsequent encounter for fracture with routine healing, difficulty in walking, and muscle weakness.
Record review of Resident #12's Quarterly MDS dated [DATE] revealed Resident #12 had a BIMS score of 13 which indicated she was cognitively aware and was independent with toilet hygiene. Additionally, Resident #12 was coded for needing supervision or touching assistance for other activities of daily living.
Record review of Resident #12's care plan date initiated 07/15/2024 revealed, Resident was at risk for falls D/T recent fall with C1 fracture and laceration to back of head. Goal: The resident will not sustain serious injury requiring hospitalization through the review date. Interventions: anticipate and meet the resident's needs, assist with ADLs as needed, call light within reach, complete fall risk assessment, educate the resident/family/caregivers about safety reminders and what to do if a fall occurs, orient resident to room, provide adaptive equipment or devices as needed, Physical therapy evaluate and treat as ordered or PRN, and side rails: quarter rails up as ordered.
Record review of Resident #12's incident report dated 07/09/2024 at 2:24PM prepared by LVN J revealed, Nursing description: This nurse was notified by CNA that a patient was sitting on the floor by their bed. Resident description: Patient stated that she was getting out of bed and made a turn when she slipped on the floor and fell to floor. Patient stated she hit her right elbow against the bed rail. Injuries Observed at time of Incident: Injury Type: Fracture, and Hematoma (back of head). Other Info: Resident got out of bed and lost her balance and fell. Resident reported hitting her right arm. X-ray ordered STAT with no dislocations or fractures noted. Sent to ER for evaluation of bump to head.
Record review of Resident #12's progress notes dated 07/09/2024 at 2:23PM LVN J documented This nurse was notified by CNA that patient was sitting on floor bed. Patient stated that she was getting out of bed & made a turn when she slipped on floor & fell to floor. patient stated she hit her right elbow against bed rail. Head to toe assessment done & VS assessed. Notified [clinician] & STAT x-ray to be ordered. New order for Tramadol 50mg Q6hrs if Tylenol 325mg does not help with pain. plan of care continues.
Record review of Resident #12's Interact Nursing Home to Hospital Transfer form dated 07/09/2024 at 4:32PM filled out by LVN C revealed, Resident #12 was being transferred to the emergency room for fall during dayshift (7AM-3PM), hit right humerus to right shoulder with x ray orders, this shift a Quarter-size bump with dry blood to back of head on left side, resident denied LOC, HA, blurred vision, or dizziness, reached out to NP-send out to eval and treat as needed.
Record review of X-ray on Wheels imaging dated 07/09/2024 documented, Impression: The bones are osteoporotic. There is no dislocation or fracture. The humeral head defect is visualized, likely due to prior injury or avascular necrosis. The moderate to severe gleno-humeral osteoarthritis is visualized and indeterminate of age.
Record review of the emergency room notes date of service: 07/09/2024: patient reports that she tripped, falling backwards and hitting the back of her head approximately 3 hours prior to arrival.initially did not think she needed to be seen in the ER, however changed her mind after finding a goose egg on the back of her head. Upon reviewing the emergency room records, the documentation did not suggest any immediacy/urgency with emergent interventions.
During an interview on 10/12/2024 at 10:53AM, LVN J stated she normally worked the 7AM-3PM shift. LVN J stated around 2:30pm ON 07/09/2024, a CNA notified her that Resident #12 was on the floor in her room. LVN J stated Resident #12 was independent for toilet assistance and did not regularly use the call light system. LVN J stated Resident #12 stated she twisted and hit her right arm and proceeded to conduct a full head to toe assessment documented within the incident report dated 07/09/2024. LVN J stated while conducting her head-to-toe assessment she felt everything but did not notice any skin irregularities. LVN J stated while notifying Resident #12's primary care physician, the physician ordered a STAT X-Ray on 07/09/2024 (the same day). LVN J stated she notified LVN C (3PM-11PM shift) about the ordered STAT X-Ray while conducting shift switch report. LVN J stated LVN C was the one that observed a hematoma on Resident #12. LVN J stated hematomas could occur minutes to hours later, after any injury. LVN J stated she never saw blood or any skin irregularities. when on the floor the hematoma could have happened after. LVN J reiterated she observed no bruising on Resident #12's arm. LVN J stated once she left at 3pm, LVN C could have found Resident #12's skin irregularities. LVN J stated any skin irregularity, including bruising, lacerations, and hematomas, would necessitate a full head to toe assessment documented on a Skin Assessment form, which would include descriptive details of the skin irregularity and measurements if possible. LVN J stated if there was a quarter size skin irregularity/hematoma, she did not definitively answer how nurses would monitor its' progression daily and stated the wound care/treatment nurse would assess skin irregularities weekly but not daily. When LVN J was asked how would details and measurements of the skin irregularity/hematoma benefit the nursing staff, LVN J did not verbalize a response. LVN J reiterated, on 07/09/2024 she did not observe any skin irregularity on Resident #12, and if a skin irregularity was observed, it was after her shift. When LVN J was asked how a resident could be affected when details of the skin irregularities were not detailed appropriately, LVN J did not verbalize a response. When LVN J was asked about the last Wound/Skin irregularity in-service she attended, she stated she could not recall.
During an interview on 10/12/2024 at 11:25AM LVN C stated she normally worked the 3-11PM shift. LVN C stated she does recall being notified of Resident #12's fall on 07/09/2024, and stated LVN J notified her of the unwitnessed fall but did not recall any specific descriptive details given by LVN J. LVN C stated she went into Resident #12's room shortly after her shift began, as a CNA notified her of dry blood observed to the back of Resident #12's head. LVN C stated when she assessed Resident #12, she observed a quarter size bump on the left, back side of Resident #12's head, a massive bruise to Resident #12's right arm, and dried blood also to the back of Resident #12's head. LVN C stated the blood looked like it was there for a while and an injury sustained from the same unwitnessed fall. LVN C stated at the time, she believed LVN J properly documented the skin irregularities, but did not answer the question if she reviewed LVN J's Skin Assessment documentation. LVN C stated she was told by LVN J that Resident #12 was to be transferred to the emergency room for evaluation and did not believe she needed to further document her own findings. LVN C stated she documented in the emergency room transfer form dated 07/09/2024 of the reasoning Resident #12 was being sent to the emergency room but did not document the skin irregularities in the facility's Skin Assessment Form, in Resident #12's electronic health record. LVN C stated she was under the impression that LVN J completed the Skin Assessment efficiently. LVN C stated she did not recall LVN J notifying her of the details of Resident #12's injuries and recalled just being notified of the unwitnessed fall. LVN C stated it was LVN J's responsibility to conduct a thorough head-to-toe assessment followed by documenting them. LVN C stated the dried blood she found on Resident #12's back of head, should have been noticed by LVN C as the appearance of the dried blood was indicative of a fresh injury. LVN C did not verbalize a response when asked: how do nurses monitor skin irregularities daily to ensure injuries i.e., bruising and hematomas, do not progress in size, or progressively get worse. LVN C stated it would be beneficial to know details including measurements of skin irregularities and continued by stating the wound care nurse did conduct weekly Skin Assessments for all residents but did not verbalize a response as to her reasoning of not documenting the observed skin irregularities for Resident #12 in her electronic health record. LVN C stated a resident could be affected negatively if injuries were not descriptively details, as the hematoma could get bigger and affect not only skin tissue but more delicately, the neurological system. LVN C stated she does not recall the last Wound/Skin Assessment in-service she attended.
During an interview on 10/11/2024 at 3:56PM the DON stated Resident #12 was sent out to the emergency room on [DATE] with the complaint of arm pain. When the DON was asked for a description about Resident #12's hematoma, she reviewed Resident #12's electronic health record, the DON stated she did not have that information available. The DON stated after reviewing Resident #12's record, it would be best practice for nurses to document the description of all skin irregularities, and should have documented all of the nurses findings in the Skin Assessment form, or within the incident report. The DON clarified that the incident report for Resident #12 was later updated once they were made aware of the emergency room findings on 07/09/2024. The DON stated measurements of Resident #12's hematoma and bruises, would be ideal but reiterated that documentation was not in Resident #12's electronic health record. The DON stated she could see how measurements would be important, and especially Resident #12's hematoma should have been descriptively detailed to monitor the healing process. The DON stated if a hematoma got bigger, it could negatively impact a patient's health and wellbeing. The DON stated currently, the wound care/treatment nurse did weekly skin assessments and that was how the facility monitor skin irregularities. The DON was asked if the treatment nurse only assessed skin weekly, how would nurse monitor daily for potential negative skin irregularity changes, to which the DON did not provide a definitive answer. The DON stated without the measurements of Resident #12's hematoma or bruise, there would be no way to track for negative progress of the skin irregularities. The DON stated, going forward the expectation would be for nurses to measure and descriptively detail any hematoma, or skin irregularities as an effective way to monitor for negative declination or positive improvement. The DON stated skin irregularities were any break in the skin, skin tear, lacerations, anything that required a treatment. The DON stated she was unaware of any dried blood found on Resident #12, and while reviewing Resident #12's 07/09/2024 emergency room Transfer form, she read LVN C documented reason of transfer was for bump to head and dried blood. The DON stated LVN C's documented reasoning should have been documented in the resident electronic health record, with descriptive detail and in a more observable place in the record. The DON stated she will be conducting an impromptu Wound/Skin Assessment Documentation in-service starting 10/11/2024 and will rectify the situation.
Record review of the facility's Area of Focus: Basic Skin Management review dated 11/29/2023 documented,
2. All residents have a head-to-toe skin inspection upon admission/readmission, then completed weekly and as needed by nursing. It is documented in PCC: NRSG: Weekly Skin. Review PCC UDA for assignments.
4. If any new skin alteration/wound is identified, it is the responsibility of the nurse to perform and document an assessment/observation, obtain treatment orders, and notify MD and responsible party.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to provide a safe, functional, sanitary, and comforta...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record reviews, the facility failed to provide a safe, functional, sanitary, and comfortable environment for residents, staff, and the public in one of one central supply rooms reviewed for environment in that:
The central supply room door on the 200 hall was propped open with a large roll of plastic, allowing easy access to potentially harmful supplies such as razors and lancets.
There were 9 full boxes of disposable razors on the shelves within reach and easily accessible.
There was a full case of deodorant that expired on [DATE].
There were 33 cases of lancets (a sharp, spring-loaded pointed tool used to check blood sugars (finger sticks) accessible.
These failures could place residents, staff, and visitors at risk of receiving incorrect care and cause health complications with subsequent illnesses, and injury.
Findings were:
Observation of the facility ' s central supply room on [DATE] at 9:15 am revealed the door was propped open with a large roll of plastic, allowing easy access to potentially harmful supplies such as razors and lancets. Expired deodorant was also found. The boxes of lancets and razors on the shelves were within reach and easily accessible. The full case of deodorant expired on [DATE].
In an interview with the DON on [DATE] at 9:15 am, she stated the door of the central supply room should not have been propped open. She said there were hazardous supplies on the shelves that residents could have gotten into. She said the razors and lancets were sharp objects and they could harm anyone with misuse, such as a resident who did not know how to handle them properly. She said she was unaware the deodorant had expiration dates. She said the CS was responsible for maintaining the central supply room including ordering supplies and making sure there was nothing expired.
In an interview with the CS on [DATE] at 3:02 pm, she said she was responsible for the central supply room and its contents. She said her responsibility included ordering supplies, not storing anything on the ground, nothing could be expired, and she had to keep it stocked. She said the door was supposed to be closed and locked at all times. She said she has had the issue of the door being propped open with a large roll of plastic. She said she was getting rid of the roll of plastic. She said she did not know who or when someone was going in and out of the door enough to prop it open. She said she assumed the CNAs probably propped the door open when they were re-stocking their areas. She said they only had one cart to assist with taking bulky items such as briefs out of central supply. She said she thought she should order another cart to prevent staff from having to prop the door open. She said her other job in the facility was staffing and she spent 90% of her time on that and she could not check the central supply door very often. She said she did not delegate to anyone to check the door for her. She said there were hazardous materials in the central supply room such as razors, lancets, nail clippers, and syringes. She said the residents would have easy access to those items and staff would probably not know they were in there because the central supply room was at the end of the 200 hall. She said she kept her main stock in the medication room. She said she highlighted expiration dates so she could keep up with items that were about to expire. She said she was unaware of the expired deodorant.
In an interview with the DON and ADON on [DATE] at 3:10 pm, they said the facility did not have a specific policy on general supplies. They both said the only policy they could find was Storage of Chemicals and they would look for something more appropriate for storage of supplies. They said the policies they had were from corporate.
In an interview with the DON on [DATE] at 3:35 pm, she presented another facility policy titled, Licensure and Compliance with Federal, State, Local Laws, and Professional Standards. She stated she did not understand the difference between a facility policy and Federal Regulations.
In an interview with the RCNS on [DATE]/ at 3:50 pm, she stated, The facility did not have their own policies, that under the definition of the policy on what they had, implied what the facility was compliant with regulations. The RCNS then provided an eleven-page document from Lippincott procedures titled, Indwelling urinary catheter (Foley) insertion, assigned male at birth. She stated, We just don ' t have policies.
Record review of the facility policy titled; Storage of Chemicals reviewed [DATE] revealed it quoted Federal regulations F689 483.25 (d) Accidents. The facility must ensure that- 483.25(d)(1) The resident environment remains as free of accident hazards as is possible. F584 483.10(i) Safe Environment .the physical layout of the facility does not pose a safety risk. Under Policy, the facility will store chemicals in accordance with manufacturer guidelines while maintaining supervision while in use.
Record review of the facility policy titled; Licensure and compliance with Federal, State, Local Laws, and Professional Standards reviewed [DATE] revealed it quoted Federal regulations F836 483.70(b) Compliance with Federal, State, and Local Laws and Professional Standards. Under Policy, the facility will provide services in compliance with all applicable Federal, State, and local laws, regulations, and codes, and with accepted professional standards and principles that apply to any professional providing services in the facility, whether temporary or permanent.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on observation, interview, and record review, the facility failed to maintain an infection prevention and control program...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY**
Based on observation, interview, and record review, the facility failed to maintain an infection prevention and control program, including hand hygiene, designed to provide a safe, sanitary, and comfortable environment, and to help prevent the development and transmission of communicable diseases and infections for one (Resident #2) of three residents, one of one Central Supply Rooms, and one of twelve rooms on the 400 hall reviewed for infection control.
1.) The facility failed to ensure resident briefs were properly stored and out of reach from other residents, staff, and visitors to prevent possible cross-contamination.
2.) The facility failed to ensure Resident #2 was placed on transmission-based precautions when her urine culture result was positive for Klebsiella pneumoniae (a bacteria).
3.) There were 4 boxes of sterile urinary catheters containing 12 each, that were expired in the Central Supply room.
This failure could place residents that require assistance with personal care at risk for healthcare associated cross-contamination and infections.
The Findings included:
1.) During an observation on [DATE] at 9:58 pm this state surveyor observed resident briefs in open packages on the CNA linen cart and two loose briefs on top of a plastic three drawer infection control storage bin outside a room on the 400 hall.
During an observation on [DATE] at 4:07 pm this state surveyor observed an open package of resident briefs on the CNA linen cart on the 400 hall.
In an interview on [DATE] at 3:15pm the DON stated she did not think resident briefs should be left open on the CNA linen carts or the infection control three drawer cart. The DON stated open briefs should not be left out on carts due to infection control and possible cross-contamination. The DON stated she was going to in-service staff on infection control immediately.
In an interview on [DATE] at 3:33pm LVN C stated she had been working since 7:00 am that morning and stated she did see the briefs on the CNA linen carts but got distracted and did not put them away. LVN C stated resident briefs should not be left out on the CNA linen carts because she felt it would be infection control issue. LVN C stated she had just started working the day shift and had not really seen resident briefs on the CNA linen carts but when she did, she had not reported it to anyone because she was not sure if it was ok to have briefs out or not. LVN C could not state when the last infection control in-service was.
In an interview on [DATE] at 3:44pm CNA D stated resident briefs should not be on the carts due to cross-contamination and infection control reasons. CNA D stated when she arrived on shift at 2:00pm that day, she saw the resident briefs and started to put them away. CNA D Stated she threw away the loose briefs that were left on the plastic 3 drawer infection control bin. CNA D stated the last in-service on infection control was about a week ago.
2.) Record review of Resident #2's admission record reflected at [AGE] year-old female initially admitted to the facility on [DATE] and readmitted on [DATE]. Her diagnoses included non-traumatic brain hemorrhage (brain bleed not caused by a head injury), left hemiplegia and hemiparesis (weakness and paralysis) following cerebral infarction (brain bleed), essential (primary) hypertension (high blood pressure), unspecified dementia, and cognitive communication deficit.
Record review of Resident #2's quarterly MDS dated [DATE] reflected Resident #2 had a BIMS score of 15 which indicated she was cognitively intact.
Record review of Resident #2's laboratory results reflected Resident #2 had a urine culture collected on [DATE] and resulted on [DATE] that showed that Resident #2 had Klebsiella pneumoniae bacteria in her urine.
Observation of Resident #2's room on [DATE] at 3:45pm reflected no TBP (transmission-based precaution) signage on the door or wall next to the door and no PPE (personal protective equipment) outside the room.
Observation of Resident #2's room on [DATE] at 1:54pm reflected no TBP signage on the door or wall next to the door and no PPE outside the room.
In an interview on [DATE] at 1:26pm, LVN I stated she knew that someone was supposed to be on TBP by diagnoses, lab results, and report. LVN I stated if a resident was supposed to be on TBP, the nurse would put an order in the computer that usually came from a telephone order from the provider. LVN I stated they would get the signage to place on the door and the PPE cart to place in the hall outside the door. LVN I stated if someone was supposed to be on TBP but was not, it could potentially cause the spread of whatever bacteria or virus that resident had which could lead to hospitalization or worse for the other residents.
In an interview on [DATE] at 2:43pm RN A stated, We know if someone was supposed to be on isolation by looking for the isolation cart or go into the computer and look for the order for isolation. The order was entered by the nurse or the provider from information from the sending entity (if the resident is coming from another facility or hospital) or from lab results. RN A stated the provider was the one to make the decision on TBP. RN A stated if someone was not on isolation that should have been, infection could be spread to other residents, family or visitors which could result in illness or death. RN A stated he knew Resident #2 recently had a UTI, but did not know what the organism was. After RN A was informed it was Klebsiella pneumoniae, he stated that she should have been on contact precautions, and he did not know why she was not.
In an interview on [DATE] at 3:35pm LVN E stated that they knew by the signage on the door that a resident was on transmission-based precautions and what type. LVN E stated if a resident was supposed to be on contact precautions but was not, it could spread the bacteria to other residents which could cause an outbreak resulting in hospitalization or death.
In an interview on [DATE] at 4:09pm the MD stated for any infection, the resident should be put on standard contact precautions. The MD stated, I thought it was standard (automatic) for residents to be put on contact precautions for any type of infection. I did not think I would need to give orders for that. In reference to Resident #2's Klebsiella pneumoniae in her urine, the MD stated, I wouldn't have necessarily treated this particular UTI with antibiotics because the bacteria count was under 100,000.
In an interview on [DATE] at 4:59pm, the IP stated a resident would be placed on contact precautions for ESBL (Extended Spectrum Beta-Lactamase. An enzyme produced by some bacteria that makes them resistant to many antibiotics) in the urine if they were incontinent without a foley and if they had a foley they would be on EBP (Enhanced Barrier Precautions). The IP stated once the physician put a resident on antibiotics it would trigger her to look at cultures. The IP stated some physicians did not want to prescribe an antibiotic if it was under 10,000 CFUs (Colony Forming Units) on the culture. In reference to Resident #2, the IP stated, With her klebsiella pneumoniae, I did not put her on contact precautions until I talked to the MD to see if she wanted to put her on EBP -vs- contact precautions. I also just do not want to fight with the family member because she got very mad when we put the resident on c diff precautions while testing for it. It came back negative, so we took her off precautions, but the family member was upset that she was on precautions in the first place. The IP stated in general, if a resident had positive urine or blood cultures they would be put on some type of precautions. The IP stated if a resident was put on precautions, the facility had batch orders to put in the computer and then it would go on her surveillance. The IP stated if someone needed to be on contact precautions but was not, infection could spread.
3.) Four full boxes of sterile urinary catheters in different sizes were expired in the Central Supply room. One box of 22fr urinary catheters had an expiration date of [DATE]. One box of 26fr urinary catheters expired on [DATE]. Two boxes of 24fr urinary catheters expired on [DATE].
In an interview with the DON on [DATE] at 9:15 am, she stated she was unaware of the expired urinary catheters. She said the catheters were sterile and should have been discarded. She said the catheters were not safe to use after the expiration date because they were most likely no longer sterile.
In an interview with the CS on [DATE] at 3:02 pm, she said she was responsible for the central supply room and its contents. She said her responsibility included ordering supplies, not storing anything on the ground, nothing could be expired, and she had to keep it stocked. She said the door was supposed to be closed and locked at all times. She said she was unaware of the expired catheters. She said she did not know what could happen to the residents if sterile catheters were used to replace per doctor orders.
In an interview with the DON and ADON on [DATE] at 3:10 pm, they said the facility did not have a specific policy on general supplies. They both said the only policy they could find was Storage of Chemicals and they would look for something more appropriate for storage of supplies. They said the policies they had were from corporate.
In an interview with the RCNS on [DATE]/ at 3:50 pm, she stated, The facility did not have their own policies, that under the definition of the policy on what they had, implied what the facility was compliant with regulations. The RCNS then provided an eleven-page document from Lippincott procedures titled, Indwelling urinary catheter (Foley) insertion, assigned male at birth. She stated, We just don ' t have policies.
Record review of the facility policy titled; Licensure and compliance with Federal, State, Local Laws, and Professional Standards reviewed [DATE] revealed it quoted Federal regulations F836 483.70(b) Compliance with Federal, State, and Local Laws and Professional Standards. Under Policy, the facility will provide services in compliance with all applicable Federal, State, and local laws, regulations, and codes, and with accepted professional standards and principles that apply to any professional providing services in the facility, whether temporary or permanent.
Record review of the facility's Infection Prevention and Control Program (IPCP) and Plan policy dated [DATE] and revised on [DATE] stated:
The facility has systems for the prevention, identification, reporting, investigating and control of infections and communicable disease of residents, staff, and visitors. This system includes an ongoing system of surveillance designed to identify possible communicable diseases and infections before they can spread to other persons in the facility and procedures for reporting possible incidents of communicable disease or infections.
Establishing Priorities and Setting Goals
5. Examples of goals might include the following:
a. Decreasing the risk of infection spreading
b. Enhancing hand hygiene
c. Minimizing the risk of transmitting infections associated with the use of procedures, medical equipment, and medical devices
Implementing Strategies to Achieve the Goals
4. Methods to reduce the risks associated with procedures, medical equipment, and medical devices, including the following:
a. Appropriate storage, cleaning, disinfection, and/or disposal of supplies and equipment.
5. Applicable precautions, as appropriate, based on the following:
a. The potential for transmission
b. The mechanism of transmission
c. The care, treatment, and services setting
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to maintain clinical records on each resident that were complete and ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to maintain clinical records on each resident that were complete and accurately documented, in accordance with accepted professional standards and practices for 7 (Resident #2, Resident #4, Resident #5, Resident #7, Resident #8, Resident #9, and Resident #10) of 7 residents reviewed for clinical records.
1a. The facility failed to ensure that RN A documented Resident #2's blood pressure on the MAR (medication administration record) or in the vital signs when Resident #2 was given medication that would decrease her blood pressure in 5 of 16 opportunities reviewed for medication administration.
1b. The facility failed to ensure that LVN E documented Resident #2's blood pressure on the MAR when Resident #2's medication that would decrease her blood pressure was not given due to her vital signs being outside of parameters for blood pressure medication administration in 4 of 38 opportunities reviewed for medication administration.
1c. The facility failed to ensure that RN J documented Resident #2's blood pressure on the MAR or in the vital signs when Resident #2 was given medication that would decrease her blood pressure in 1 of 1 opportunity reviewed for medication administration.
2a. The facility failed to ensure that RN A documented Resident #4's blood pressure and/or pulse on the MAR or in the vital signs when Resident #4 was given medication that would decrease her blood pressure and/or pulse in 44 of 61 opportunities reviewed for medication administration.
2b. The facility failed to ensure that LVN E documented Resident #4's blood pressure and/or pulse on the MAR or in the vital signs when Resident #4 was given medication that would decrease her blood pressure and/or pulse in 81 of 132 opportunities reviewed for medication administration.
2c. The facility failed to ensure that RN J documented Resident #4's blood pressure and/or pulse on the MAR or in the vital signs when Resident #4 was given medication that would decrease her blood pressure and/or pulse in 2 of 2 opportunities reviewed for medication administration.
3a. The facility failed to ensure that RN A documented Resident #5's blood pressure in the vital signs when Resident #5 was given medication that would decrease his blood pressure in 14 of 17 opportunities reviewed for medication administration.
3b. The facility failed to ensure that LVN E documented Resident #5's blood pressure in the vital signs when Resident #5 was given medication that would decrease his blood pressure in 1 of 35 opportunities reviewed for medication administration.
3c. The facility failed to ensure that RN J documented Resident #5's blood pressure in the vital signs when Resident #5 was given medication that would decrease his blood pressure in 1 of 1 opportunity reviewed for medication administration.
3d. The facility failed to ensure that LVN C documented Resident #5's blood pressure in the vital signs when Resident #5 was given medication that would decrease his blood pressure in 1 of 1 opportunity reviewed for medication administration.
4a. The facility failed to ensure that RN A documented Resident #7's blood pressure in the vital signs when Resident #7 was given medication that would decrease her blood pressure in 22 of 35 opportunities reviewed for medication administration.
4b. The facility failed to ensure that LVN F documented Resident #7's blood pressure in the vital signs when Resident #7 was given medication that would decrease her blood pressure in 12 of 12 opportunities reviewed for medication administration.
4c. The facility failed to ensure that LVN E documented Resident #7's blood pressure in the vital signs when Resident #7 was given medication that would decrease her blood pressure in 2 of 69 opportunities reviewed for medication administration.
4d. The facility failed to ensure that LVN E documented Resident #7's blood pressure in the vital signs when Resident #7's medication that would decrease her blood pressure was not given due to her vital signs being outside of parameters for blood pressure medication administration.
4e. The facility failed to ensure that LVN L documented Resident #7's blood pressure in the vital signs when Resident #7 was given medication that would decrease her blood pressure in 1 of 1 opportunity reviewed for medication administration.
5. The facility failed to ensure that RN A documented Resident #8's blood pressure and pulse on the MAR or in the vital signs when Resident #8 was given medication that would decrease her blood pressure and pulse in 6 of 16 opportunities reviewed for medication administration.
6a. The facility failed to ensure that RN A documented Resident #9's blood pressure in the vital signs when Resident #9 was given medication that would decrease his blood pressure in 14 of 15 opportunities reviewed for medication administration.
6b. The facility The facility failed to ensure that LVN E documented Resident #9's blood pressure in the vital signs when Resident #9 was given medication that would decrease his blood pressure in 4 of 38 opportunities reviewed for medication administration.
6c. The facility The facility failed to ensure that LVN C documented Resident #9's blood pressure in the vital signs when Resident #9 was given medication that would decrease his blood pressure in 1 of 1 opportunity reviewed for medication administration.
6d. The facility The facility failed to ensure that RN J documented Resident #9's blood pressure in the vital signs when Resident #9 was given medication that would decrease his blood pressure in 1 of 1 opportunity reviewed for medication administration.
7a. The facility failed to ensure that RN A documented Resident #10's blood pressure and pulse in the vital signs when Resident #10 was given medication that would decrease her blood pressure and pulse in 14 of 16 opportunities reviewed for medication administration.
7b. The facility failed to ensure that LVN E documented Resident #10's blood pressure and pulse in the vital signs when Resident #10 was given medication that would decrease her blood pressure and pulse in 1 of 37 opportunities reviewed for medication administration.
7c. The facility failed to ensure that LVN C documented Resident #10's blood pressure and pulse in the vital signs when Resident #10 was given medication that would decrease her blood pressure and pulse in 1 of 1 opportunity reviewed for medication administration.
7d. The facility failed to ensure that RN J documented Resident #10's blood pressure and pulse in the vital signs when Resident #10 was given medication that would decrease her blood pressure and pulse in 1 of 1 opportunity reviewed for medication administration.
This deficient practice could affect residents whose records are maintained by the facility and could place them at risk for errors in care and treatment.
The findings included:
1. Record review of Resident #2's admission record reflected at [AGE] year-old female initially admitted to the facility on [DATE] and readmitted on [DATE]. Her diagnoses included non-traumatic brain hemorrhage (brain bleed not caused by a head injury), left hemiplegia and hemiparesis (weakness and paralysis) following cerebral infarction (brain bleed), essential (primary) hypertension (high blood pressure), unspecified dementia, and cognitive communication deficit.
Record review of Resident #2's quarterly MDS dated [DATE] reflected Resident #2 had a BIMS score of 15 which indicated she was cognitively intact.
Record review of Resident #2's provider order summary report reflected the following orders for medications that would decrease blood pressure:
Amlodipine Besylate tablet 10mg. Give 1 tablet PO (by mouth) one time a day for HTN (high blood pressure). Hold for BP (blood pressure) < (under)120/60. (No space to document blood pressure on the MAR)
Lisinopril tablet 20mg. Give 1 tablet PO one time a day for HTN. Hold for BP <120/60. (There was a space to document blood pressure on the MAR)
Record review of Resident #2's vital signs in the September 2024 and October 2024 MARs reflected the following:
RN A documented NA in the space where Resident #2's blood pressure was supposed to be documented when Lisinopril was administered on 9/4/24, 9/22/24, 10/10/24, and 10/16/24.
LVN E documented an x in the space where Resident #2's blood pressure was supposed to be documented when Lisinopril was not administered due to her vital signs being outside of parameters for blood pressure medication administration on 9/24/24, 10/2/24, 10/7/24 and 10/20/24.
RN J documented NA in the space where Resident #2's blood pressure was supposed to be documented when Lisinopril was administered on 9/10/24.
Record review of Resident #2's September 2024 and October 2024 vital signs in the EHR reflected the following:
RN A did not document Resident #2's blood pressures on 9/4/24, 9/22/24, 10/10/24 and 10/16/24.
LVN E documented Resident #2's blood pressures on 9/24/24, 10/2/24, 10/7/24 and 10/20/24.
RN J did not document Resident #2's blood pressure on 9/10/24.
2. Record Review of Resident #4's admission record reflected a [AGE] year-old female admitted to the facility on [DATE]. Her diagnoses included chronic systolic (congestive) heart failure (the heart does not pump blood effectively and causes fluid build up in the lungs), atrial fibrillation (the upper chambers of the heart beat out of coordination with the lower chambers and causes poor blood flow), unspecified dementia, and essential (primary) hypertension (high blood pressure).
Record review of Resident #4's quarterly MDS dated [DATE] reflected Resident #4 had a BIMS score of 13 which indicated she was cognitively intact.
Record review of Resident #4's provider order summary report reflected the following orders for medications that would decrease blood pressure and/or pulse:
Amiodarone Hcl tablet 100mg. Give 1 tablet PO one time a day for arrhythmia (irregular heartbeat). Hold for HR <60. (No space to document HR on the MAR)
Carvedilol tablet 3.125mg. Give 1 tablet PO BID (2 times a day) for HTN. Hold for BP <120/60, HR <50. (No space to document BP or HR on the MAR)
Digoxin tablet 125mcg. Give 1 tablet PO in the morning every other day for CHF. Check pulse and hold for HR <60. (No space to document HR on the MAR)
Losartan Potassium tablet 100mg. Give 1 tablet PO HS (at bedtime) for HTN. Hold for BP <120/60, HR <50. (There was space to document the BP and HR on the MAR).
Record review of Resident #4's vital signs in the September 2024 and October 2024 MARs reflected the following:
RN A documented NA in the space where Resident #4's blood pressure and pulse were supposed to be documented when Losartan was administered on 9/11/24, 9/29/24, 10/4/24, 10/9/24, and 10/16/24. (1 medication = 5 of 12 opportunities)
Record review of Resident #4's vital signs in the EHR for September 2024 and October 2024 reflected the following:
RN A did not document Resident #4's blood pressure with the morning administration of blood pressure decreasing medications on 9/4/24, 9/5/24, 9/11/24, 9/22/24, 9/23/24, 9/28/24, 9/29/24, 10/3/24, 10/4/24, 10/8/24, 10/10/24, 10/16/24, 10/17/24, and 10/22/24. (1 medication = 14 of 15 opportunities)
RN A did not document Resident #4's heart rate with the morning administration of heart rate decreasing medications on 9/4/24, 9/5/24, 9/11/24, 9/22/24, 9/23/24, 9/28/24, 9/29/24, 10/4/24, 10/5/24, 10/8/24, 10/10/24, 10/16/24, 10/17/24, and 10/22/24. (3 medications = 18 of 18 opportunities)
RN A did not document Resident #4's blood pressure with the bedtime administration of blood pressure decreasing medications on 9/11/24, 9/29/24, 10/4/24, 10/9/24, and 10/16/24. (2 medications = 6 of 16 opportunities)
LVN E did not document Resident #4's blood pressure with the morning administration of blood pressure decreasing medications on 9/1/24, 9/2/24, 9/3/24, 9/7/24, 9/8/24, 9/9/24, 9/12/24, 9/13/24, 9/14/24, 9/15/24, 9/16/24, 9/17/24, 9/18/24, 9/19/24, 9/20/24, 9/21/24,9/24/24, 9/25/24, 9/26/24, 9/27/24, 9/30/24/24, 10/1/24, 10/2/24, 10/3/24, 10/6/24, 10/7/24, 10/9/24, 10/11/24, 10/12/24, 10/13/24, 10/14/24, 10/15/24, 10/18/24, and 10/24/24. (1 medication = 34 of 37 opportunities)
LVN E did not document Resident #4's heart rate with the morning administration of heart rate decreasing medications on 9/1/24, 9/2/24, 9/3/24, 9/7/24, 9/8/24, 9/9/24, 9/12/24, 9/13/24, 9/14/24, 9/15/24, 9/16/24, 9/17/24, 9/18/24, 9/19/24, 9/20/24, 9/21/24, 9/24/24, 9/25/24,9/26/24, 9/27/24, 9/30/24, 10/2/24, 10/3/24, 10/6/24, 10/7/24, 10/9/24, 10/12/24, 10/13/24, 10/14/24, 10/15/24, 10/18/24, 10/19/24, 10/22/24, and 10/24/24. (3 medications = 105 of 108 opportunities)
LVN E did not document Resident #4's heart rate when heart rate decreasing medications were not administered in the morning due to her vital signs being outside of parameters for heart rate decreasing medication administration on 9/27/24, 10/1/24 and 10/11/24. (1 medication = 3 of 7 opportunities)
LVN F did not document Resident #4's blood pressure with the morning administration of blood pressure decreasing medications on 9/6/24. (1 medication = 1 of 1 opportunity)
LVN F did not document Resident #4's heart rate with the morning administration of heart rate decreasing medications on 9/6/24. (2 medications = 2 of 2 opportunities)
RN J did not document Resident #4's blood pressure with the morning administration of blood pressure decreasing medications on 9/10/24. (1 medication = 1 of 1 opportunity)
RN J did not document Resident #4's heart rate with the morning administration of heart rate decreasing medications on 9/10/24. (2 medications = 2 of 2 opportunities)
LVN K did not document Resident #4's blood pressure with the morning administration of blood pressure decreasing medications on 9/19/24. (1 medication = 1 of 1 opportunity)
LVN K did not document Resident #4's heart rate with morning administration of heart rate decreasing medications on 9/19/24. (3 medications = 3 of 3 opportunities)
3. Record review of Resident #5's admission record reflected a [AGE] year-old male that was originally admitted to the facility on [DATE] an re-admitted on [DATE]. Resident #5's diagnoses included atrial fibrillation, essential (primary) hypertension, and dementia.
Record review of Resident #5's quarterly MDS dated 10.4.24 reflected Resident #5 had a BIMS score of 11 which indicated moderate cognitive impairment.
Record review of Resident #5's provider order summary report reflected the following order for a medication that would decrease blood pressure:
Metoprolol Tartrate tablet 25mg. Give 1 tablet PO one time a day for HTN. Hold for BP<120/60.
Record review of Resident #5's vital signs in the EHR for September 2024 and October 2024 reflected:
RN A did not document Resident #5's blood pressure with the morning administration of a blood pressure decreasing medication on 9/4/24, 9/5/24, 9/11/24, 9/22/24, 9/23/24, 9/28/24, 9/29/24, 10/4/24, 10/5/24, 10/8/24, 10/10/24, 10/16/24, 10/17/24 and 10/23/24. (1 medication = 14 of 17 opportunities)
LVN E did not document Resident #5's blood pressure with the morning administration of a blood pressure decreasing medication on 9/1/24. (1 medication = 1 of 35 opportunities)
RN J did not document Resident #5's blood pressure with the administration of a blood pressure decreasing medication on 9/10/24. (1 medication = 1 of 1 opportunity)
LVN C did not document Resident #5's blood pressure with the morning administration of a blood pressure decreasing medication on 10/22/24. (1 medication = 1 of 1 opportunity)
4. Record review of Resident #7's admission record reflected a [AGE] year-old female who was admitted to the facility on [DATE]. Resident #7's diagnoses included persistent atrial fibrillation and chronic kidney disease stage 4.
Record review of Resident #7's admission MDS reflected Resident #7 had a BIMS score of 15 which indicated she was cognitively intact.
Record review of Resident #7's provider order summary report reflected the following orders for medications that would decrease blood pressure and pulse:
Isosorbide Mononitrate Extended Release 24 hour tablet 30mg. Give 1 tablet PO one time a day for HTN. (No hold parameters indicated. No place to document BP or HR on the MAR. Discontinued 9/28/24)
Metoprolol Tartrate tablet. Give 12.5mg PO BID for HTN. (No hold parameters indicated. No place to document BP or HR on the MAR.)
Record review of Resident #7's September 2024 and October 2024 vital signs in the EHR reflected:
RN A did not document Resident #7's blood pressure and heart rate with the morning administration of blood pressure and heart rate decreasing medications on 9/22/24, 9/23/24, 10/4/24, 10/8/24, 10/10/24, 10/16/24, 10/17/24, 10/22/24, and 10/23/24. (2 medications = 11 of 19 opportunities)
RN A did not document Resident #7's blood pressure and heart rate with the evening administration of a blood pressure and heart rate decreasing medication on 9/8/24, 9/10/24, 9/11/24, 9/20/24, 9/23/24, and 10/4/24, 10/5/24(BP), 10/6/24(HR), 10/11/24, 10/16/24, 10/17/24, 10/19/24, 10/22/24, and 10/24/24. (1 medication = 14 of 18 opportunities)
LVN E did not document Resident #7's blood pressure and heart rate with the evening administration of a blood pressure and heart rate decreasing medication on 10/1/24 and 10/23/24. (1 medication = 2 of 10 opportunities)
LVN E did not document Resident #7's blood pressure and heart rate in the evening when a heart rate and blood pressure decreasing medication was documented as not given due to her vital signs being outside of parameters for blood pressure and heart rate decreasing medication administration on 10/12/24 and 10/23/24. (1 medication = 2 of 8 opportunities)
LVN F did not document Resident #7's blood pressure and heart rate with the evening administration of a blood pressure and heart rate decreasing medication on 9/14/24, 9/15/24, 9/17/24, 9/26/24, 9/27/24, 10/2/24, 10/3/24, 10/8/24, 10/14/24, 10/15/24, 10/20/24, and 10/21/24. (1 medication = 12 of 12 opportunities)
5. Record review of Resident #8's admission record reflected a [AGE] year-old female who was admitted to the facility on [DATE]. Resident #8's diagnoses included essential (primary) hypertension, occlusion (blockage) and stenosis (hardening) of unspecified carotid artery (artery in the neck that helps supply the brain with blood) and unspecified heart failure.
Record review of Resident #8's annual MDS dated [DATE] reflected that Resident #8 had a BIMS score of 5 which indicated she had severe cognitive impairment.
Record review of Resident #8's provider order summary report reflected the following orders for blood pressure and heart rate decreasing medications:
Digoxin tablet 125mcg. Give 1 tablet PO one time a day for heart failure. Hold for HR <60. (No place to document HR on the MAR)
Metoprolol Tartrate tablet 50mg. Give 1 tablet PO one time a day for HTN. Hold for BP <120/60 or HR <60. (There are places to document the BP and HR on the MAR)
Lisinopril tablet 20mg. Give 1 tablet PO one time a day for HTN. Hold for BP <120/60. (No place to document BP on the MAR)
Record review of Resident #8's September 2024 and October 2024 MARs reflected the following:
RN A documented NA in the space for BP and NA in the space for HR on the MARs with the morning administration of a blood pressure and heart rate decreasing medication on 9/4/24, 9/22/24, 9/29/24, 10/10/24, and 10/26/24. (1 medication = 5 of 15 opportunities)
RN J documented NA in the space for BP and NA in the space for HR on the MARs with the morning administration of a blood pressure and heart rate decreasing medication on 10/10/24. (1 medication = 1 of 1 opportunity)
Record review of Resident #8's September 2024 and October 2024 vital signs in the EHR reflected:
RN A did not document Resident #8's blood pressure and heart rate with the morning administration of blood pressure and heart rate decreasing medications on 9/4/24, 9/22/24, 9/29/24, 10/10/24, and 10/16/24. (3 medications = 15 of 45 opportunities)
RN J did not document Resident #8's blood pressure and heart rate with the morning administration of blood pressure and heart rate decreasing medications on 9/10/24. (3 medications = 3 of 3 opportunities)
6. Record review of Resident #9's admission record reflected a [AGE] year-old male who was admitted to the facility on [DATE]. Resident #9's diagnoses included essential (primary) hypertension, dementia, and chronic kidney disease.
Record review of Resident #9's quarterly MDS dated [DATE] reflected Resident #9 had a BIMS score of 13 which indicated he was cognitively intact.
Record review of Resident #9's provider order summary report reflected an order for the following blood pressure decreasing medication:
Lisinopril oral tablet 20mg. Give 20mg PO one time a day for HTN. Hold for BP <110/50. (No place to document BP on the MAR)
Record review of Resident #9's September 2024 and October 2024 vital signs in the EHR and September 2024 and October 2024 MARs reflected the following:
RN A did not document Resident #9's blood pressure with the morning administration of a blood pressure decreasing medication on 9/4/24, 9/5/24, 9/11/24, 9/22/24, 9/23/24, 9/28/24, 9/29/24, 10/4/24, 10/5/24, 10/8/24, 10/10/24, 10/16/24, 10/17/24, and 10/23/24. (1 medication = 15 of 16 opportunities)
LVN E did not document Resident #9's blood pressure with the morning administration of a blood pressure decreasing medication on 9/25/24 and 10/14/24, 10/21/24, and 10/25/24. (1 medication = 4 of 38 opportunities)
RN J did not document Resident #9's blood pressure with the morning administration of a blood pressure decreasing medication on 9/10/24. (1 medication = 1 of 1 opportunity)
LVN C did not document Resident #9's blood pressure with the morning administration of a blood pressure decreasing medication on 10/22/24. (1 medication = 1 of 1 opportunity)
7. Record review of Resident #10's admission record reflected a [AGE] year-old female who was admitted to the facility on [DATE]. Resident #10's diagnoses included chronic systolic (congestive) heart failure, essential (primary) hypertension, and dementia.
Record review of Resident #10's quarterly MDS reflected Resident #10 had a BIMS score of 6 which indicated she had severe cognitive impairment.
Record review of Resident #10's provider order summary report reflected an order for the following blood pressure and heart rate decreasing medication:
Metoprolol Tartrate tablet 25mg. Give 1 tablet PO one time a day for HTN. Hold for BP <120/60, HR <50. (There were no places to document the BP or HR on the MAR)
Record review of Resident #10's September 2024 and October 2024 vital signs in the EHR and September 2024 and October 2024 MARs reflected the following:
RN A did not document Resident #10's blood pressure and heart rate with the morning administration of a blood pressure and heart rate decreasing medication on 9/4/24, 9/5/24, 9/11/24, 9/22/24, 9/23/24, 9/28/24, 9/29/24, 10/4/24, 10/5/24, 10/8/24, 10/10/24, 10/16/24, 10/17/24, 10/19/24(HR), and 10/23/24. (1 medication = 15 of 16 opportunities)
LVN E did not document Resident #10's blood pressure and heart rate with the morning administration of a blood pressure and heart rate decreasing medication on 10/24/24. (1 medication = 1 of 37 opportunities)
RN J did not document Resident #10's blood pressure and heart rate with the morning administration of a blood pressure and heart rate decreasing medication on 9/10/24. (1 medication = 1 of 1 opportunity)
LVN C did not document Resident #10's blood pressure and heart rate with the morning administration of a blood pressure and heart rate decreasing medication on 10/22/24. (1 medication = 1 of 1 opportunity)
In an interview on 10/18/24 at 1:26pm LVN I stated vital signs were done by whoever was passing the medications and they were usually in the morning from 7am to 9am. LVN I stated, On the long-term residents sometimes you get all the blood pressures first, document, and then give the medications. Medications are documented as they are given. LVN I stated if the BP was not checked before giving a BP medication and the resident's BP was low, it could cause the resident to have hypotension (low blood pressure), which could lead to distress or hospitalization. LVN I stated it was important to document accurately and timely so that they would know what information to give the provider if something happened to the resident. LVN I stated if things were not documented accurately, it could lead to inaccurate information being passed along.
In an interview on 10/18/24 at 2:43pm RN A stated he checked vital signs before he gave medications to make sure they were within the parameters to be given. RN A stated he would check vital signs as he went along, document them (the vital signs) as soon as they were done, give the med, then document the med right after it was given. RN A stated if a BP was not checked before a BP med was given, it could drop the pressure too low and the resident could have an adverse reaction such as syncope (fainting), falls, or dizziness. RN A stated if he found a resident with a BP too low, he would assess the resident and notify the provider. RN A stated if vital signs or medications were not documented correctly, another nurse might medicate the resident again. RN A stated, On 10/10 and 10/16 I know I took a bp before I gave the meds. I don't know if I clicked something that made it show NA and not record the bp, but I know that I took them because otherwise I wouldn't know if it was ok to give the BP meds. I will make sure from now on that it is documented correctly. RN A stated occasionally if the resident was not in the room (out to an appt or something) then the vital signs and the medication administration might get documented later on when the resident returned.
In an interview on 10/18/24 at 3:35pm LVN E stated blood pressures were checked right before he gave the medications, and the blood pressure was usually documented when he put it in the computer after he gave the medication. LVN E stated he could not think of any reason why the BP and meds would be documented at a later time. LVN E stated if a medication had 8:00am, it could be given between 7am and 9am. LVN E stated if he did not check a blood pressure before giving a blood pressure med, it could cause the resident to become hypotensive which could lead to dizziness, falls, hospitalization or even death if the blood pressure got too low. LVN E stated it was important to document accurately and timely so that something was not forgotten and so that another nurse did not medicate a resident again because it appeared they had not been medicated. LVN E stated, I don't dispute the documented times on 10/11-10/15 for Resident #2's blood pressures. I documented the blood pressures once I got all the meds passed and had a chance to sit down and put the information in the computer. LVN E further stated, I have about 60 (or more) residents to medicate in a 2 hour time span. I start medicating at 6:15am and usually finish around 11:00am and that's just medicating- that's not documenting. I don't document the actual times I checked BPs, I just put them in when I get the chance to document. I've told administration that there's no way to get that many residents medicated in that amount of time.
In an interview on 10/17/24 at 4:13pm, the DON stated the person giving the medication checked the BP and pulse and was supposed to document the BP and pulse at the same time the medication was given and documented.
In a follow up interview on 10/25/24 at 12:42pm, the DON stated there were 2 primary people who did medication pass- RN A and LVN E and that only 1 medication aide was scheduled at a time. The DON stated the medication aide passed medications to all of the residents except the ones with G tubes because the floor nurses did those. The DON stated on average the medication aide passed medications to 58 residents. RN A and LVN E usually worked 6am to 10pm. LVN F usually worked evening shift, 2pm to 10pm, as a medication aide or 3p to 11p as a nurse. When asked about the medication aide having to pass medications to approximately 58 residents in a 2 hour time span the DON stated, I think that it CAN be done. It looks like what they are doing is signing off after medications were done. The DON further stated, I talked to my corporate nurse and we are looking at ways to change 2 of the halls to a 9am medication pass so the medication aides have a little better time frame to pass medications. The DON stated it was very important to check and document blood pressures and pulses when giving certain cardiac medications because if the med aide or nurse did not check blood pressures and/or pulses prior to medication administration, it could lower the resident's BP or HR to a dangerous level. The DON further stated when blood pressures and heart rates were checked, they should have been documented in the vitals and on the MAR. The DON stated if the vital signs were not documented where they were supposed to be, the next nurse would not know what the most recent vital signs were. The DON stated, The 3 primary medication aides were probably last in[T