CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure each resident received adequate supervision to...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure each resident received adequate supervision to prevent accidents for one of five residents (Resident #38) reviewed for accidents and hazards in that:
1. The facility failed to ensure Resident #38 did not elope after he was identified to be of high risk for elopement. Resident #38 eloped on 06/09/23 through his window.
2. The facility failed to put alarms on all unit windows after the elopement as indicated in the PIR. 3 windows were missing alarms. 2 of 3 windows had screws to keep them permanently closed.
3. The facility failed to establish a system to monitor alarms.
4. The facility failed to have sufficient staff to safely monitor residents on the secured unit.
These failures resulted in the identification of an Immediate Jeopardy (IJ) on 07/10/23 at 03:59 PM. While the IJ was removed on 07/11/23 at 2:59 PM, the facility remained out of compliance at a scope of isolated and a severity level of potential for more than minimal harm that is not immediate jeopardy due to the facility's need to evaluate the effectiveness of the corrective systems.
This deficient practice could place the residents at risk for harm, serious injury, or death.
Findings included:
Record review of Resident #38's undated face sheet indicated he was a [AGE] year-old male, admitted to the facility on [DATE]. He had diagnoses that included Alzheimer's disease (a progressive disease that destroys memory and other important mental functions) and depression (a mental health disorder characterized by persistently depressed mood or loss of interest in activities, causing significant impairment in daily life).
Record review of Resident #38's admission MDS, dated [DATE], indicated he had a BIMS score of 05, which indicated severe cognitive impairment. Resident #38 was independent in bed mobility and transfers. He required supervision assistance for walking and locomotion on unit, dressing, toileting, eating, and personal hygiene. He received antipsychotics, antidepressants, and anticoagulants 7 of 7 days of the assessment window.
Record review of Resident #38's physician's orders, dated 07/11/23, indicated he had this order:
*Admit to secured unit related to wandering / elopement risk. The start date was 05/15/23.
Record review of Resident #38's care plan, with a review date of 06/09/23, indicated a focus of elopement risk as evidenced by elopement on 06/09/23. The interventions included staff will monitor resident's location frequently and to monitor and record behavior when it occurs.
Record review of Resident #38's progress notes, dated 06/09/23 through 06/30/23, indicated Resident #38 eloped on 06/09/23, and was later found 25-30 minutes later down the street. The progress notes further indicated that on 06/17/23 the alarm in Resident #38's room had been removed from the window and was reapplied by facility staff.
Record review of Resident #38's elopement/wandering observation, dated 05/16/23, indicated he was a high risk for wandering. The assessment further indicated that Resident #38 had a history of elopement, exhibited wandering behavior, has shown exit seeking behavior, is likely to follow someone through a facility exit, and resident was physically able to exit on foot or by wheelchair.
Record review of Resident #38's elopement/wandering observation, dated 06/09/23, indicated he was a high risk for wandering. The assessment further indicated that Resident #38 had a history of elopement, exhibited wandering behavior, had shown exit seeking behavior, is likely to follow someone through a facility exit, had verbalized the need and/or desire to go home or to another location and had the ability to act on that verbalization, and resident was physically able to exit on foot or by wheelchair.
Record review of Resident #38's elopement incident report, dated 06/09/23, indicated he was found at 10:05 AM on 06/09/23.
Record review of the Provider Investigation Report, dated 06/15/23, indicated Resident #38 was noted missing from the facility on 06/09/23 at approximately 9:30 AM. Facility staff searched the facility and were unable to locate him internally. The facility expanded their search outside and Resident #38 was found at an EZ Mart gas station down the street. The report indicated that the facility staff estimated Resident #38 was out of the facility for an estimated 20-25 minutes. The PIR indicated the facility had taken action by placing alarms on all occupied resident room windows.
Record review of Resident #38's vital signs after his elopement indicated his vital signs were taken on 06/09/23 at 10:24AM and his blood pressure was 125/81 and his pulse was 99 beats per minute. No temperature reading was found. No respiration reading was found.
During an observation and interview on 07/10/23 at 10:57 AM, Resident #38 was observed walking out of his room [ROOM NUMBER] in the secured unit. He was independently able to open and close his bedroom door and ambulate throughout the unit. He said he remembered leaving the unit and said he was trying to go visit his mom and dad.
During an observation on 07/10/23 at 10:59 AM, room [ROOM NUMBER], at the end of the unit, was observed with the door open. Residents wandering in the unit had open access to this room. The window alarm for the window in this room was not attached to the window and was laying in the windowsill. This surveyor was able to open the window fully and the alarm did not make any noise.
During an observation and interview on 07/10/23 at 11:06 AM, CNA E said she was not working the day Resident #38 eloped. She said she was familiar with him and she monitors him if he started fidgeting or exit seeking. She said she tries to keep him occupied. She took this surveyor into Resident #38's room ( room [ROOM NUMBER]) and the window had a screw in the frame so it could not be opened. It did not have an alarm attached.
During an interview on 07/10/23 at 11:14 AM, RN F said she was taking care of Resident #38 that day. She said she was not working the day he eloped. She said when he starts exit seeking, she attempts to distract him by talking to him or having him call his daughter.
During an interview on 07/10/23 at 11:18 AM, the Social Worker said she was in her office on the day Resident #38 eloped when she noticed staff were looking for him so she went outside to help. She said she was unable to find him in the facility so she jumped into her car to assist looking for him. She had looked around the neighborhood and they had already found him when she came back to the facility. She said the staff gave him water and assessed him. She said it was warm outside, and he had a sweater on. She said he looked tired and hot. She said she did not talk to him directly. She said the Marketing, business office, and medical records staff found Resident #38 and brought him back.
During an interview on 07/10/23 at 11:30AM, CNA G said she was the CNA that noticed Resident #38 was not in his room. She said she was not assigned to the unit that day. She said she was weighing residents around the facility that day. She said she was trying to go get Resident #38 to weigh him and was unable to locate him in his room. She said she told the nurse Resident #38 was not in his room or in the unit. She said she then left the unit to weigh another resident. After this she came back to the unit to assist the nurse in finding Resident #38. She said her and the nurse looked around the unit and then notified the DON. Then the facility staff searched the facility for Resident #38 and were unable to locate him. She said they eventually found him near a busy roadway at a gas station about 0.8 miles away from the facility. She said he was gone from the facility about an hour. She said when he returned he was wearing a sweater and he was hot and sweaty. She said he eloped from the unit through the window in his room. She said this was the first time that she recalls Resident #38 eloping from the facility. She said there was only typically one staff member assigned to the unit. She said there was only a nurse assigned to the unit on the day Resident #38 eloped. She said the Marketing Director brought Resident #38 back to the facility. She said the facility put window alarms in place to keep the unit residents from eloping and Resident #38 likes to take the alarms off the windows.
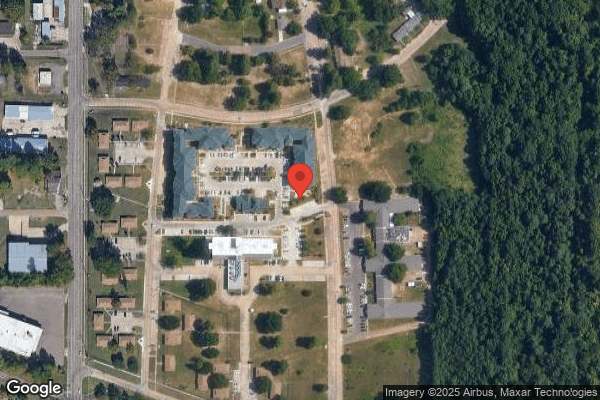
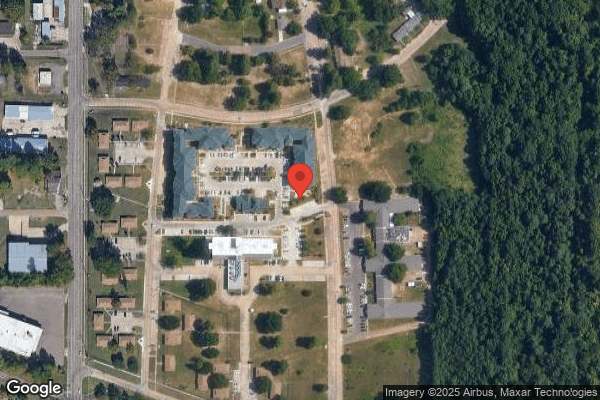
During an observation on 07/10/23 at 11:47AM, the Super Bingo and the EZ Mart were both located off of N [NAME] Road, approximately 0.6 to 0.8 miles from the facility. The speed limit was 35 miles per hour. It was a busy 4 lane street. The EZ mart was on the opposite side of the street and Resident #38 would have crossed the street to reach the EZ mart.
During an interview on 07/10/23 at 12:05PM, LVN D said she was assigned to the unit the day Resident #38 eloped. She said she was in the middle of medication pass. She said she was giving the resident next door to Resident #38 and noticed Resident #38 had walked down the hallway and entered his room. She said a CNA came to get Resident #38's weight and said he was not in his room. She said she immediately stopped medication pass and searched for Resident #38. She said she could not find him in the dining area and the MDS coordinator came to help. She said had not heard any alarms. She said her and the MDS coordinator searched all over the unit. She said she noticed the screen in Resident #38's room window appeared to be bent. She said she was unable to open the window. She then notified the DON and they searched all over the facility. She said eventually other facility staff found Resident #38 offsite. She assessed him and he was hot and sweaty. She said he was found first at the EZ Mart and then they finally picked him up at the Super Bingo hall. She said she obtained his vitals and he had a sweat shirt on and long pants. She said they got him some ice water because he was tired and sweaty. She said it was hot outside. She said Resident #38 had no bruises or injuries. She said Resident #38 told the staff he wanted to go walking. She said He has not eloped at this facility but he has eloped before at another facility before he came to this one. She said they put alarms on the windows to ensure the residents do not escape through the windows. She said she checks the windows at least once a shift, but she was not told by administration how often she should check them. She said she works back in the unit by herself most of the time. She said she has only had another staff member assigned with her about 5-6 times since she started working there in February of 2023. She said she does her nursing duties as well as the CNA duties when she was the only staff assigned to the unit. She said she performed incontinent care when she was back there alone. She said she tries to do as many baths as possible and will notify the next shift when she was not able to complete all the baths. She said there were typically around 9 residents back in the unit. She said she saw Resident #38 about 10 mins before anyone noticed he was missing.
During an interview on 07/10/23 at 12:21PM, the Marketing Director said she went out front to help the Social Worker look for Resident #38. After they searched the facility she and the Business Office Manager jumped into her car to look for Resident #38. She said they found him at a bingo hall near a busy roadway. She said Resident #38 was leaning against the telephone pole. He was hot and sweaty and was wearing a sweater. They got him into the car and brought him back to the building and got him some water. They handed him back to the nurse assigned to the unit that day.
During an interview on 07/10/23 at 12:25PM, the Business Office Manager said the DON asked her if she saw Resident #38. She said the staff looked all over the facility for the resident. She said she and the Marketing Director went out the side door to make sure he was not out in the patio. She said they hopped in the Marketing Director's vehicle to look for Resident #38. She said they travelled down a busy roadway and found him near the bingo hall. She said she got out of the vehicle and talked to Resident #38 and he said he was walking. They got him back in the vehicle to take him back to the facility. She said he was wearing a sweater, hat and long pants. She said he was hot and sweaty. They got him back to the facility and used cool rags to cool him off. She said she notified Resident #38's daughter. She said she left him with the nursing staff. She said it was warm outside that day.
During an interview on 07/10/23 at 12:30PM, the Maintenance Supervisor said after Resident #38 eloped they put a screw in Resident #38's room window and the window next door to his room to make the window stay closed. He said he put alarms on all windows in the unit and made sure the alarms on the unit doors were functioning properly. He said he tries to check the window alarms in the unit at least 3 times a week. He said he will also go check on them if he was notified by the CNAs in the unit. He said he did not keep any log or documentation of him checking the alarms.
During an interview on 07/10/23 at 12:36PM, CNA E said she checks the alarms as often as possible. She said she was not told by administration how often to check the alarms. She said she did not keep a log of when she has checked the alarms.
During an interview on 07/10/23 at 12:37PM, RN F said she does not routinely check the alarms. She said she did not keep a log of when they were checked. She said she thought the maintenance director was responsible for checking the alarms routinely.
During an observation on 07/10/23 at 2:15PM, the middle window in the secured unit dining room had no alarm attached to the window. There were residents in the room and they had free access to it. There was a screw in the frame of the window that was supposed to keep it from opening.
During an observation on 07/10/23 at 2:20PM, Resident #38's room [ROOM NUMBER] had no alarm attached to the window. The screw was still in place on the window frame.
During an observation on 07/10/23 at 2:30PM, room [ROOM NUMBER] alarm was still in the windowsill, not attached to the window. This surveyor was able to lift the window open and then close it back.
During an interview on 07/11/23 at 9:45AM, the DON said the facility does not have a policy that addresses supervision of residents. She said they do not have a policy that addresses alarms or monitoring of alarms.
During an interview on 07/11/23 at 02:50PM, Resident #38's Responsible Party said she was not surprised when the facility notified her that Resident #38 had eloped. She said he had eloped before he came to this facility.
During an interview on 07/12/23 at 1:12PM, the ADON said she did not work in this facility when Resident #38 eloped. She said she started working in this facility on 06/20/23. The incident occurred on 06/09/23. She said she was not aware of anyone being assigned to check the alarms routinely before surveyor intervention this week. She said before surveyor intervention this week, they tried to have two staff members assigned to the unit during the day, and only one staff nurse assigned from 10pm-6am. She said she does not think one staff member assigned in the unit was enough staff to properly monitor all the unit residents and keep them from eloping. She said the one staff member would not be able to get their work done, or even leave the unit to go to the bathroom.
During an interview on 07/12/23 at 02:01PM, the DON said after Resident #38 eloped they installed window alarms on occupied rooms and the room next to him. She said they did not put a procedure in place to monitor the alarms. She said the staff would report the alarms missing whenever they saw it. She said they did in-services about the alarms. there were 1 -2 staff members assigned to the unit at times, there was not a specific set schedule of how many people should have been back there at a time. She said she did not have enough staff to assign more staff to the unit. She said there was an average of eight residents back in the unit at a time. She said they did not increase staff immediately after the elopement. She said on 07/05/23 they increased staffing to 2 staff assigned to the unit all the time except for 10PM to 6AM. she said they finally had enough staff then to be able to permanently assign more staff back in the unit. She said she did not feel like one nurse would be able to adequately monitor the residents in the unit while passing medications. She said the nurse that was assigned to the unit was primarily responsible for ensuring the residents did not elope. She said it was ultimately all staff's responsibility to prevent residents from eloping. She said there was risk to all residents if they eloped for serious injury, serious harm, or death.
During an interview on 07/12/23 at 2:20PM, the ADON said if a resident eloped like Resident #38 did there was a potential for serious injury, serious harm, or death.
During an observation on 07/12/23 at 2:44PM, the Administrator said after Resident #38 eloped, they put window alarms on all occupied rooms in the unit. He said they increased rounding and supervision of Resident #38. He said they reported the elopement to the state, notified his family and the doctor. He said the MD director was notified. He said the nurse took an assessment of Resident #38 and they gave him water and made sure he did not suffer heat exhaustion. He said the Administrator, Maintenance and all other staff were responsible for ensuring that the alarms were in place. He said that the Administrator and the other management were constantly replacing window alarms in the unit. He said they did not document that they were checking alarms. He said he was in the unit daily along with maintenance and other staff assigned to the unit, and they were checking the alarms. He said there was no documentation that logged the staff checking the alarms. He did not know without checking the schedule if there was only one staff assigned to the unit at a time before 07/05/23. He said on 7/05/23 they changed the staffing to ensure that 2 staff members were assigned to the unit all the time except for 10pm to 6am. He said after surveyor intervention on 07/10/23 the staffing was changed to ensure 2 staff were assigned to the unit at all times. He said he expected one nurse to be able to take care of 8 residents in the unit while passing meds. He said he expected the nurse to be able to keep the 8 residents from eloping. He said that all staff were responsible for ensuring that the residents do not elope, but the nurse was assigned to take care of the residents in the unit that day. He said a resident that eloped like Resident #38 was at risk for heat stroke, heat exhaustion, a possible vehicle accident, fall, serious harm, serious injury, or death.
The Administrator was notified of an IJ on 07/10/23 at 3:59PM and was given a copy of the IJ template and a Plan of Removal (POR) was requested. The Plan of Removal was accepted on 07/11/23 at 9:45AM and included the following:
7/11/2023
Plan of Removal - F 689
Immediate Action Taken
Resident Specific
*
Resident #38 was located by Business Office Manager and Marketer on 6/9/2023 at 10:02am and returned to the facility.
*
Resident #38 assessed by licensed nurse on 6/9/2023 at 10:15am. Findings documented in Matrix. No injuries or adverse effect noted.
*
Elopement Risk Assessment for Resident #38 completed on 6/9/2023 at 11:13am by RN.
*
Elopement Risk Careplan for Resident #38 updated on 6/9/2023 at 11:30am by RN.
*
NP notified of elopement on 6/9/2023 at 10:15am by LVN. No new orders received.
*
Responsible party notified of elopement on 6/9/2023 at 10:15am by LVN. No concerns voiced.
*
MD notified of the IJ on 7/10/2023 at 4:45pm by Director of Nursing, no new orders received.
*
Resident #38 remains in the Secured Unit and has had no further elopement attempts.
System Changes
*
Elopement Risk Assessments completed for all residents in the facility on 6/9/2023 at 1:40pm by DON and RN.
*
Window alarms placed on windows of all occupied rooms on 6/9/2023 at 12:30pm.
*
Window alarms placed on all secured unit windows on 7/10/23 at 4:45pm.
*
Staff increased in Secured Unit to 1 Licensed Nurse and 1 Nurse Aide, from 6am to 10pm on 7/5/23.
*
Staff increased in Secured Unit to 1 Licensed Nurse and 1 Nurse Aide, 24 hours a day on 7/10/2023.
*
Secured Unit rounds established on 7/10/2023 at 6:00pm. This is to monitor that all windows have alarms, alarms are functioning properly, and all residents are in place.
*
All windows in the Secured Unit secured and raise a minimum of 4 inches, as of 7/11/23 at 6:30am.
*
Elopement policy reviewed on 6/9/23 at 11:30am by Administrator, Regional Nurse, and Director of Nursing. No changes made to policy at this time.
Education
*
Director of Nursing provided education to all staff regarding the Elopement Policy. All staff present in the facility were educated on 7/10/2023, at 5pm. Staff not present for the education will receive the education prior to their next shift.
*
Director of Nursing provided education to nursing staff regarding the Secured Unit Rounds to ensure residents are in place, alarms are on windows, and alarms are functioning properly. All nursing staff present in the facility were educated on 7/10/2023, at 5pm. Staff not present for the education will receive the education prior to their next shift.
*
Director of Nursing provided education to nursing staff regarding the Secured Unit staffing pattern - 2 staff members on all shifts. All nursing staff present in the facility were educated on 7/11/2023, at 8:30am. Staff not present for the education will receive the education prior to their next shift.
Monitoring
*
Administrator/designee to review Secured Unit rounds 5x/week to ensure compliance.
The surveyor verification of the Plan of Removal from 07/11/23 was as follows:
During an observation on 07/11/23 at 7:56AM room [ROOM NUMBER] has an alarm on the window and the screw was removed. Resident #38's room [ROOM NUMBER] had an alarm on the window and the screw was removed.
During an observation on 07/11/23 at 7:59AM, all three unit dining room windows had alarms and the screw in the middle window was removed.
During an observation on 07/11/23 at 08:05AM, two staff members were assigned and working in the unit.
During an observation on 07/11/23 at 10:54AM, it was observed that all windows in the unit had alarms installed and they were turned on.
During interviews conducted from 07/11/23 11:52AM through 3:20PM, 21 of 38 staff (15 from day shift, and 6 from night shift and including CNAs, LVNs, and RNs) were interviewed. All staff said they received education on elopement, rounding on the unit and checking alarms every two hours, and that there will be two staff assigned to the unit at all times.
Record review of in-service training, dated 06/09/23, after the elopement, indicated training related to window alarms in the secured unit was provided to facility staff. The training stated: .Residents on the unit will have window alarms on their windows, please ensure the alarm is on and functioning, if you find one that does not work, please contact Admin/DON/maintenance director. If you hear any alarms going off, you are to respond immediately.
The Weather Underground website, accessed on 07/13/23 at 10:59AM, indicated that the temperature in the city of Texarkana was 82 degrees Fahrenheit on 06/09/23 at 9:53AM. The wind speed was 5 miles per hour with 0 miles per hour wind gusts. There was 0.0 inches of precipitation and the condition was fair. The humidity was 67%.
Record review of facility's policy titled Elopement, effective December 2017, stated:
It is the policy of this home to provide a systematic approach to searching for a resident who may have left the home and/or home grounds.
Procedure
The following steps are to be followed when a resident is noted absent and is not found on initial search of the home. This also includes when a resident leaves the home grounds without staff notification.
Home staff will:
*Search the home and grounds
*Send staff member(s) out to locate the resident
*Notify Administrator or on-call person immediately
*If resident is not located within 30 minutes, call the local police
Charge Nurse will:
*Notify responsible party (this may be done when the search is initiated)
*Notify the resident's physician
*Assess the resident on return to the home
*Document the time resident absence is noted, time of return, assessment of resident, and notification of physician and responsible party
*Complete and incident report in the clinical software
*Follow-up charting for 24 hours if no injuries .
.Administrative / supervisory staff will:
*Determine if elopement is reportable to state regulatory agency
*Interview staff and obtain written statements .
*Establish a monitoring system for resident until flight risk is resolved
*Determine what measures can be taken to prevent it from happening again
On 07/11/23 at 02:59PM, the Administrator was notified the IJ was removed. However, the facility remained out of compliance at a scope of isolated and a severity level of potential for more than minimal harm that is not immediate jeopardy due to the facility's need to evaluate the effectiveness of the corrective systems.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure an accurate MDS assessment was completed for 2 of 20 residen...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure an accurate MDS assessment was completed for 2 of 20 residents reviewed for MDS accuracy. (Resident # 36 and #17)
1.
The facility failed to accurately document Resident #36's significant weight change
2.
The facility failed to accurately document Resident #17's upper extremity contractures.
These failures could place residents at risk for not receiving needed care and services.
Findings included:
1. Review of Resident #36's undated electronic face sheet revealed that she was admitted to the facility on [DATE] with diagnoses of dementia (the loss of cognitive functioning - thinking, remembering, and reasoning - to such an extent that it interferes with a person's daily life and activities), hypothyroidism (a common condition where the thyroid doesn't create and release enough thyroid hormone into your bloodstream), and insomnia (having trouble falling asleep, staying asleep, or getting good quality sleep).
Record review of Resident #36's significant change MDS assessment dated [DATE] revealed a BIMS with a score of 09, which indicated Resident #36 had a moderate cognitive deficit. The MDS also revealed, Resident #36, was independent with set up for eating and had limited range of motion to one side of her upper and lower body. There was no weight loss noted.
Record review of Resident #36's care plan revealed Resident #36 had a significant unplanned/unexpected weight loss as evidence by 4.9% loss in 30 days dated 05/22/2023 with interventions of giving the residents supplements as ordered.
Record review of Resident #36's weight logs revealed Resident #36 had a 16 pound/ 17% weight loss in 30 days. Resident #36's monthly weight for May 2023 was 90 pounds and June 2023 weight was 74 pounds.
2. Review of Resident #17's undated electronic face sheet revealed that she was admitted to the facility on [DATE] with diagnoses of rheumatoid arthritis (an autoimmune and inflammatory disease, which means that your immune system attacks healthy cells in your body by mistake, causing inflammation (painful swelling) in the affected parts of the body), diabetes mellitus type 2 (group of diseases that result in too much sugar in the blood (high blood glucose), and depression ( a common and serious medical illness that negatively affects how you feel, the way you think and how you act).
Record review of Resident #17's quarterly MDS assessment dated [DATE] revealed a BIMS with a score of 15, which indicated resident #17 had no cognitive deficit. The MDS also revealed, Resident #17, required extensive assistance of one staff member for eating and no limited range of motion was noted on the MDS.
Record review of Resident #17's care plan dated 05/24/2023 indicated Resident # 17 had contractures to her bilateral upper extremities which increased her risk for skin breakdown, pain, and injury. The intervention listed for the contracture care plan for Resident #17 was to assist with repositioning often, use positioning devices to maintain proper body alignment and position bilateral upper extremities on pillows for comfort.
During an observation on 07/10/2023 at 8:33 a.m., Resident #17 had bilateral upper extremity contractures to shoulders, elbows, wrists, hands, and fingers.
During an interview on 7/12/2023 at 2:43 p.m., the MDS Nurse stated that she was responsible for completing MDS in the facility. She stated that she was aware that Resident #17 had contractures to her upper extremities and the contractures should have been on the 05/23/2023 MDS. The MDS Nurse stated accuracy of the MDS was important so the care plans would be correct.
During an interview on 07/12/2023 at 3:25 p.m., the DON said she expected the MDS to be accurately coded. She stated that the MDS Nurse was responsible for the accuracy of the MDS. She stated that residents could be placed at risk of not receiving the services they require with an inaccurate MDS.
Record review of CMS Manual provided by the facility as their guidance to MDS updated in October 2019. Chapter 1: Resident Assessment Instrument shows that, Care Area Triggers are specific resident responses for one or a combination of MDS elements. The triggers identify residents who have or at risk for developing specific functional problems and require further assistance. Care Area Assessment is the further investigation of triggered areas, to determine if the care area triggers require interventions and care planning. The key to successfully using the resident assessment instrument is to understand that its structure is designed to enhance resident care, increase a resident's active participation in care, and promote the quality of a resident's life. The resident assessment has multiple regulatory requirements The assessment accurately reflects the resident's status.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide an ongoing program of activities in accordanc...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide an ongoing program of activities in accordance with the comprehensive assessment to meet the interests and the physical, mental, and psychosocial well-being for 2 of 10 residents reviewed for activities. (Residents # 7 and Resident # 36.)
The facility failed to provide Resident # 7 and Resident #36 with consistent, scheduled activities.
This failure could place residents at risk for not having activities to meet their interests or needs and a decline in their physical, mental, and psychosocial well-being.
Findings included:
1. Record review of a face sheet dated 11/07/2023 revealed Resident #7 was a [AGE] year-old female admitted on [DATE] with diagnoses Chronic obstructive pulmonary disease (group of diseases that cause airflow blockage and breathing-related problems), Muscle wasting and atrophy (the wasting or thinning of muscle mass), Dysuria (Discomfort when urinating can have causes that aren't due to underlying disease), Personal history of urinary (tract) infections (An infection in any part of the urinary system, the kidneys, bladder, or urethra) , and Anxiety disorder (persistent and excessive worry that interferes with daily activities.).
Record review of Resident #7's annual MDS dated [DATE] revealed a BIMS with a score of 4, which indicated resident #7 has severely impaired cognition. Revealed that it was very important for Resident # 7 to do her favorite activities. Revealed that Resident #7 required a one-person physical assist for locomotion on unit.
Record review of Resident #71's care plan problem dated 05/04/2023 revealed Resident #7 is dependent on staff for activities, cognitive stimulation, social interaction. The resident needs out of room social, spiritual, and stimulus activities and mental stimulation. Resident will be encouraged to attend participate in activities 3 times per week in group setting through the review date. The resident will maintain involvement in cognitive stimulation, social activities as desired 1:1 and in small group setting through review date. Resident also enjoys playing bingo, listening to gospel music as well as religious services, resident enjoys the outdoors when weather permits as well as visits from family and friends, she enjoys getting her nails done and facetime visit with church members and grandson who serves in military.
2. Record review of a face sheet dated 03/16/2023 revealed Resident #36 was a [AGE] year old female and was admitted on [DATE] with diagnosis including dementia (the loss of cognitive functioning - thinking, remembering, and reasoning - to such an extent that it interferes with a person's daily life and activities), psychotic disturbance (severe mental disorders that cause abnormal thinking and perceptions), hypothyroidism (happens when your thyroid gland doesn't make enough thyroid hormones to meet your body's needs), and muscle wasting and atrophy (wasting or thinning of muscle mass.)
Record review of Resident #36's MDS dated [DATE] revealed Resident # 36 had a BIMS score of 9 which indicated moderate cognitive impairment. Revealed that it was very important for Resident # 36 to do her favorite activities. Revealed that locomotion on the unit did not occur for rResident #36.
Record review of Resident #3627's care plan last reviewed on 03/16/2023 revealed Resident #36 will be provided 1:1 activities when needed. Revealed that resident will attend 3 activities per week.
Record review of a Weekly Calendar for the Month of May 2023 indicated the following 1:1 activities: Monday at 11:15 a.m. Activities to go 1:1 activities. Tuesday at 11:15 a.m. Activities to go 1:1 activities. Wednesday at 11:15 a.m. Activities to go 1:1 activities. Thursday at 11:15 a.m. Activities to go 1:1 activities. Friday at 11:15 a.m.
Record review of a Weekly Calendar for the Month of June 2023 indicated the following 1:1 activities: Monday at 11:15 a.m. Activities to go 1:1 activities. Tuesday at 11:15 a.m. Activities to go 1:1 activities. Wednesday at 11:15 a.m. Activities to go 1:1 activities. Thursday at 11:15 a.m. Activities to go 1:1 activities. Friday at 11:15 a.m.
Record review of a Weekly Calendar for the Month of July 2023 indicated the following 1:1 activities: Monday at 11:15 a.m. Activities to go 1:1 activities. Tuesday at 11:15 a.m. Activities to go 1:1 activities. Wednesday at 11:15 a.m. Activities to go 1:1 activities. Thursday at 11:15 a.m. Activities to go 1:1 activities. Friday at 11:15 a.m.
During an observation on 07/11/2023 at 11:13 a.m., Resident # 7 was not engaged in activities. Resident #7 was laying in bed unengaged. There were no activities ongoing for Resident #7.
During an observation on 07/11/2023 at 11:20 a.m., Resident # 36 was not engaged in activities. Resident # 36 was laying in bed unengaged. There were no activities ongoing for Resident # 36. No staff entered Resident #36's room to provide 1:1 activities.
During an interview on 07/12/2023 at 9:00 a.m., Resident #7 stated that she has not had an activity done in her room. She stated she did not know what activities are available to her and she has never played any games or had anyone do anything fun with her in her room. She stated that she had not had any one-on-one activities in her room with anyone ever.
During an interview on 7/12/23 at 9:20 a.m., Resident # 36 stated that she doesn't do any activities and she just lays in bed most of the day. She stated that it has been like this since March. She stated that there was a woman that came into her room and did activities with her for two or three weeks but no one has done anything with her in a long time.
During an observation on 07/12/2023 at 11:24 a.m., Resident # 7 was not engaged in activities. Resident #7 was laying in bed unengaged. There were no activities ongoing for Resident #7.
During an observation on 07/12/2023 at 11:28 a.m., Resident # 36 was not engaged in activities. Resident # 36 was laying in bed unengaged. There were no activities ongoing for Resident # 36. No staff entered Resident #36's room to provide 1:1 activities.
During an interview on 7/12/2023 at 2:10 p.m. LVN B stated that she has not seen any of the staff complete activities for Resident #7. She stated that residents who are bedfast are supposed to get directed activities in their room however she has not personally witnessed any of the bedfast residents having activities in their room.
During an interview on 7/12/2023 at 2:10 p.m., CNA H stated that the activities director used to do activities with residents down the hall. She stated that since the activities director has been on medical leave no activities are done with the bedfast residents. She stated that it gets busy and they don't always have time to do activities with the bedfast residents. She stated that it is normal for the bedfast residents that can't go to the group activities to not have any planned activities at all.
During an interview on 7/12/2023 at 2:20 p.m., RN C She stated that she has not seen any staff ding activities for Resident # 36. She stated that staff have been filling in to do activities for residents but I have not seen any staff do an activity for Resident #36. She stated that she has no idea who is supposed to be doing one on one activities with the residents that aren't able to participate in the group activities.
During an interview on 7/12/2023 at 1:11 p.m., the ADM stated that their activities director has been out, for approved leave. He stated that they have been assigning department heads to do different activities for residents. He stated that there is also other residents who have taken up leading activities such as a resident led bingo. He stated that he expects that all residents have activities available to them including the residents that are dependent and bedfast. He stated that the activity logs do not go past May for the 1:1 activities is because the activity director has not completed them and the logs do not exist. He stated that there is no policy regarding activities to provide.
During an interview on 7/12/2023 at 1:39 p.m. the DON stated that residents who are dependent and bedfast should have activities brought to their room if they are unable to participate in the group activities. She stated that this includes the 1:1 resident activities. She stated that she does not know why the 1:1 residents are not receiving activities in their room.
Record review of facility observation report for resident activities dated from 5/1/2023 to 6/1/2023 revealed that 1:1 activities were completed for residents. However, there are no activities for 1:1 residents logged past 5/19/2023 as the activities director was out on approved leave and 1:1 activities ceased to be documented afterwards. Shows that both Resident # 7 and Resident # 36 did not have any 1:1 activities past 5/19/2023.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure a resident with pressure ulcers received necess...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to ensure a resident with pressure ulcers received necessary treatment and services, consistent with professional standards of practice, to promote healing, prevent infection and prevent new ulcers from developing for 1 of 4 residents, (Resident #4) reviewed for skin integrity in that:
The facility failed to provide Resident #4 with proper wound care.
This failure could place residents at risk of wound deterioration, increased pain, infection, and a decline in health.
The findings were:
Record review of Resident #4's face sheet dated 7/12/2023 revealed Resident # 4 was a [AGE] year-old-female with an admission date of 03/17/2023 with diagnoses that included quadriplegia (a symptom of paralysis that affects all a person's limbs and body from the neck down), morbid obesity (a complex chronic disease in which a person has a body mass index (BMI) of 40 or higher or a BMI of 35 or higher and is experiencing obesity-related health conditions), and stage 4 sacral pressure ulcer (full-thickness skin loss extending through the fascia with considerable tissue loss).
Record review of Resident #4's most recent quarterly MDS assessment, dated 6/07/2023 revealed the resident had a BIMS of 14, which indicated minimal cognitive impairment. Further review of the quarterly MDS assessment revealed Resident #4 had (1) stage 4 pressure ulcer that was present on admission to the facility. The MDS also revealed (4) unstageable (ulcers covered with slough or eschar) pressure ulcers, not present on admit classified as deep tissue injury ulcers (when a deep pressure injury is suspected but can't be confirmed. The area of skin may look purple or dark red, or there may be a blood-filled blister).
Record review of Resident #4's care plan dated 07/10/2023 revealed the resident had an unstageable pressure ulcer located on the sacrum with an intervention to provide treatment to pressure ulcer per physician's order.
Record review of Resident #4's physician's orders, dated 06/12/2023 revealed the following orders for the following treatments:
1.
Stage 4 sacral pressure ulcers- cleanse wound with wound cleanser, pat dry, pack with dilute sodium hypochlorite (NaClO) solution wet to moist, cover with dry dressing daily.
2.
Stage 4 Right lower buttock- cleanse wound with wound cleanser, pat dry, pack with dilute sodium hypochlorite (NaClO) solution wet to moist, cover with dry dressing daily.
3.
Right 4th toe unstageable, paint with betadine daily
4.
Right 3rd toe unstageable (DTI), paint with betadine daily.
5.
Right Heel unstageable (DTI), with betadine daily.
6.
Left 1st toe stage 3, paint with betadine daily
Record review of last wound care physician consult dated 06/14/2023 indicated no change in Stage 4 pressure ulcer to sacrum or Stage 4 pressure ulcer to R lower buttock and listed the following wounds and treatment recommendations:
1.
Stage 4 pressure ulcer to sacrum, treatment of dilute sodium hypochlorite (NaClO) solution-soaked gauze ¼ strength wet to moist; cover with gauze island dressing with border; apply house barrier cream to peri-wound once daily.
2.
Stage 4 pressure ulcer to right lower buttock-treatment dilute sodium hypochlorite (NaClO) solution-soaked gauze ¼ strength wet to moist; cover with gauze island dressing with border; apply house barrier cream to peri-wound once daily
3.
Right 4th toe unstageable, paint with betadine daily
4.
Right 3rd toe unstageable (DTI), paint with betadine daily.
5.
Right Heel unstageable (DTI), with betadine daily.
6.
Left 1st toe stage 3, paint with betadine daily.
During the observation of wound care for Resident #4, on 07/11/2023 at 11:30 a.m., LVN Q cleaned Resident #4's sacral wound improperly, using a piston syringe to irrigate the wound and touching the tip of the piston syringe to the sides and base of the wound. LVN Q then dressed the wound without using barrier cream to the peri-wound as recommended by the wound care physician. LVN Q proceeded to cleanse Resident #4's stage 4 pressure ulcer to her lower right buttock using the same piston syringe used for the sacral wound and once again touched the tip of the piston syringe to the sides and base of the buttock wound. LVN Q noted an area of skin bleeding around the buttock wound and wiped the blood with the dilute sodium hypochlorite (NaClO) solution-soaked gauze prepared for packing the buttock wound. LVN Q then cut out the area of dilute sodium hypochlorite (NaClO) solution-soaked gauze she wiped the blood with and packed the stage 4 buttock wound with the remainder of the contaminated gauze. LVN Q did not change her gloves before packing the wound and did not use barrier cream to the peri wound as ordered. LVN Q proceeded with the treatments and painted all prescribed areas with betadine as ordered.
During an interview on 07/12/2023 at 11:50 a.m., LVN Q stated the proper technique to cleanse the stage 4 wounds to the sacrum and buttock would have been to spray wound cleanser to the wound and wipe them out gently with gauze. LVN Q stated she did not think about using two separate pistons to irrigate the wounds. LVN Q stated she should have changed gloves between cleaning the wound and applying a fresh dressing and should have gotten another dilute sodium hypochlorite (NaClO) solution-soaked gauze when she wiped the blood up with first one. LVN Q stated she was unaware the wound care doctor's recommendations to apply barrier cream to the peri-wound. LVN Q stated barrier cream would protect the wound edges from the dilute sodium hypochlorite (NaClO) solution. LVN Q stated the treatment nurse was responsible for the reviewing the wound doctor's notes and transcribing them for them to end up on the TAR. LVN Q stated improper wound care treatment of the pressure ulcer could hinder the healing process.
During an interview on 7/8/22 at 9:46 a.m., the DON stated, LVN Q should not have used a piston to irrigate the stage 4 wound to Resident #4's sacrum or buttock. The DON stated LVN Q should have used wound cleanser-soaked gauze and cleansed the wound in a center to outward motion. The DON stated she was unaware the wound care doctor recommended barrier cream to the peri wound for the stage 4 pressure ulcers, but she would call him for clarification. The DON stated changing gloves from dirty to clean was a must to prevent infection. The DON stated using a soiled gauze to pack a wound even if you cut out the soiled part was not acceptable practice for wound care.
At the time of the exit on 07/12/2023, the facility did not provide a policy and procedure for wound care.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure an acceptable parameter of nutritional status ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure an acceptable parameter of nutritional status was maintained for 1 of 20 residents (Resident #36) who was reviewed for nutritional status, in that:
1.
Resident #36 had a significant weight loss of 21.5 pounds, a 22% loss, in less than 180 days. The facility did not follow RD recommendations or provide nutritional supplements as ordered.
This failure could place residents at risk for further weight loss and decline in health due to nutritional needs not being met.
Finding included:
1.Review of Resident #36's undated electronic face sheet revealed that she was admitted to the facility on [DATE] with diagnoses of dementia (the loss of cognitive functioning - thinking, remembering, and reasoning - to such an extent that it interferes with a person's daily life and activities), hypothyroidism (a common condition where the thyroid doesn't create and release enough thyroid hormone into your bloodstream), and insomnia (having trouble falling asleep, staying asleep, or getting good quality sleep).
Record review of Resident #36's significant change MDS assessment dated [DATE] revealed a BIMS with a score of 09, which indicated resident #36 had a moderate cognitive deficit. The MDS also revealed, Resident #36, was independent with set up for eating and had limited range of motion to one side of her upper and lower body. There was no weight loss noted. There was no therapeutic diet noted. There were no behaviors of refusal or signs of depression noted on the MDS for Resident #36.
Record review of Resident #36's care plan revealed it was last updated 05/22/2023. Resident #36 required set up and supervision for eating and had no care plan for limited range of motion. Resident #36 had a significant unplanned/unexpected weight loss as evidence by 4.9% loss in 30 days dated 05/22/2023 with interventions of giving the residents supplements as ordered.
Record review of the weight log for Resident #36 revealed the following weights:
March 2023- 95.6 pounds
April 2023- 94.6 pounds
May 2023- 90 pounds
June 2023- 74 pounds
July 2023- 71.4 pounds
Record review of an RD assessment dated [DATE] indicated Resident #36 weighed 90 pounds. The RD assessment indicated Resident #36 was underweight, was on a regular diet, consumed 26-75% of meals. The RD assessment indicated Resident #36's current intake appeared to be inadequate as evidenced by weight loss. RD assessment revealed the facility would offer nutrition intervention in an attempt to halt weight loss and support weight gain toward a healthy weight range for Resident #36. RD Recommendations were to add fortified foods three times a day with meals for 90 days, house shakes 4 ounces twice daily between meals to add 400 calories and 12 grams of protein for 60 days.
Record review of an RD assessment dated [DATE] at 1:56 p.m., indicated Resident #36 weighted 86.6 pounds, was underweight, and had a 9.4% in 69 days, and her intake was 1-25% of meals. Recommendations for Resident #36 were whole milk with lunch and dinner, ice cream twice daily with lunch and dinner, House shakes daily at bedtime.
Record review of consolidated physician orders revealed Resident #36 had a diet order of regular diet, regular texture, thin liquids dated 03/16/2023. An order for house shakes once a day at bedtime was ordered on 06/22/2023. An order for Remeron (antidepressant with weight gain side effects) 15mg once daily at bedtime was ordered 06/23/2023.
Record review of the history and physical dated 03/23/2023 did not address Resident #36's weight or nutrition status. History and physical dated 05/16/2023 did not address Resident #36's weight or nutritional status. History and physical dated 06/23/2023 was the addressed weight loss with new order for Remeron 15mg once daily at bedtime.
Record review of meal intake dated 06/01/2023 to 07/11/2023 revealed 20 refusals of meals, 38 meals 1-25% consumption, and 1 meal 26-50% consumption.
During an observation and interview on 07/10/2023 at 8:00 a.m., Resident #36 was lying in her bed on her right side with bed in lowest position. Resident #36's breakfast tray was sitting on a rolling overbed table that was in the highest position. Resident #36 stated she could not see or reach what was on her overbed table. Resident #36 stated she was not going to eat her breakfast but did want the milk to drink. No milk was on the tray for Resident #36, only water and coffee.
During an observation and interview on 07/10/2023 at 12:40 p.m., Resident #36 had an untouched lunch tray on her rolling overbed table. No milk, no ice cream, no fortified foods were noted on tray. Resident #36 asked if she could have a drink of milk because the red punch was too sweet and hurt her stomach.
During an observation on 07/11/2023 at 12:38 p.m., Resident #36 had an untouched meal tray on her overbed table. No milk, no ice cream, no fortified food was noted on tray.
During an interview on 07/11/2023 at 12:45 p.m., CNA P stated Resident #36 could feed herself if she felt like eating. CNA P stated Resident #36 had refused almost every meal for the last month. CNA P stated she was unaware Resident #36 should have milk or ice cream on her tray and she had never seen milk or ice cream on her tray unless they had ice cream for dessert.
During an interview on 07/11/2023 at 12:55 p.m., LVN Q stated Resident #36 refused almost every meal. LVN Q stated Resident #36 was on a regular diet with house shake at bedtime. LVN Q stated she was unaware the dietician made recommendations for fortified food, milk twice daily, or ice cream twice daily. LVN Q stated Resident #36 liked milk and ice cream. LVN Q stated it was the DON's responsibility to follow up on all RD recommendations, put them in place, and notify the kitchen of the changes to residents' diet.
During an interview on 07/11/2023 at 2:12 p.m., the DM stated she was unaware of Resident #36 having any changes to her diet. The DM stated normally, the DON or ADON would provide a dietary change slip to the kitchen staff if fortified food or supplements were added. The DM stated she had not received any dietary change slips for Resident #36.
During an interview on 07/12/2023 at 2:15 p.m., the DON stated it was her responsibility to review dietary recommendations and put interventions in place for weight loss. The DON stated she was aware of the weight loss Resident #36 was unsure how the dietary recommendations were overlooked. The DON stated she expected dietary recommendations to be followed even if the resident refused meals. The DON stated Resident #36's family decided to sign her up on hospice because of her refusal to eat.
During an interview on 07/12/2023 at 2:25 p.m., the Administrator stated he expected for dietary recommendations to be followed to promote healthy weights for all residents. The Administrator stated it was the responsibility of the DON to follow up on dietary recommendations and ensure all parties are notified of any changes. The Administrator stated he was aware Resident #36 was refusing most meals and instructed social services to call the physician and family and discuss the next step in intervention for Resident #36.
Review of the facility policy dated 12/2017 indicated the dietician will assess and make recommendations in areas which may include:
a.
Fortified food diet changes
b.
Vitamin/mineral supplementation
c.
Supplements/shakes
d.
Appetite stimulants
e.
Meal assistance
f.
Diet texture
g.
Labs
h.
Weight changes
i.
Alternate means of nutritional support.
The recommendations made by the consultant dietician will be addressed by Director of Nursing or designee within 72 hours, if possible, after exit by the consultant dietician.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0697
(Tag F0697)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure that pain management was provided to residents who require ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews and record review, the facility failed to ensure that pain management was provided to residents who require such services, consistent with professional standards of practice for 1 of 20 residents reviewed for pain management. (Resident #47)
The facility failed to manage Resident #47's pain by not administering an ordered as needed pain medication.
This failure placed residents at risk for increased pain, decline in mobility, functioning, inability to perform activities of daily living and decreased quality of life.
Findings Include:
Record review of a face sheet dated 07/10/23 revealed Resident #47 was [AGE] years old and was admitted on [DATE] with diagnoses including dementia, muscle spasms, and Parkinson's Disease (a disorder of the central nervous system that affects movement, including tremors).
Record review of current physician's orders indicated an open-ended order with a start date of 06/27/23 for Tylenol #3 (an opioid pain medication), 1 tab every 4 hours as needed for pain. The orders indicated an open-ended order with a start date of 10/05/22 for Tramadol (narcotic used to treat moderate to severe pain) 50 milligrams every 6 hours as needed for pain.
Record review of the most recent MDS dated [DATE] indicated Resident #47 was understood and understood others. The MDS indicated a BIMS of 15 indicating no cognitive impairment for Resident #47. The MDS indicated Resident #47 an active diagnosis of unspecified pain. The MDS indicated Resident #47 had received scheduled pain medication and PRN (as needed) pain medication during the 5 previous days. The MDS was electronically signed on 06/06/23 by the MDS Coordinator indicating she had completed the assessment for Section J of the MDS.
Record review of a care plan last revised on 07/09/2023 indicated Resident #47 did not indicate pain as a problem area.
Record review of a Medication Administration History dated 07/01/23 - 07/12/23 indicated a Tylenol #3 had been administered to Resident #47 at 9:15 a.m. There was no indication of a dose being administered at 5:00 a.m. The Medication Administration History indicated Tramadol 50 milligrams was administered at 4:41 p.m. and a stat (immediate) dose was given but did not indicate the time given.
Record review of a Controlled Drug Record dated 06/20/23 - 07/10/23 for Resident #47 indicated a Tramadol 50 milligram was signed out at 10:54 a.m. on 7/10/23. There was no Tramadol signed out at an earlier time on that 07/10/23. The Controlled Drug Record indicated on 7/10/23 a Tylenol #3 was signed out at 5:00 a.m. and 9:15 a.m.
Record review of an Inservice Form dated 05/03/23 indicated, .Staff to provide frequent checks on (Resident #47) . The form was signed by LVN B indicated she had been inserviced.
During an observation and interview on 07/10/23 at 9:00 a.m., Resident #47 said she had been hurting since 5 a.m. She said she was hurting in her back, right arm, and right shoulder. On a pain scale of 1 to 10 with 10 being the worst pain, she rated her pain a 10. The resident was shaking and tearful. She said she told the aide changing her clothes that she was hurting. She said she did get her morning medications, but she was not sure if it was pain medicine or not.
During an interview on 07/10/23 at 9:07 a.m., CNA A said she did tell the nurse that Resident #47 was hurting. She was not sure if anything else had been done. She said, this is normal for her.
During an interview on 07/10/23 at 9:10 a.m., LVN B said Resident #47 had something for pain at 5:00 a.m. She said her pain medicine was just now due and as soon as she was finished with another resident, she will give her the next dose.
During an observation on 07/10/23 at 10:10 a.m., Resident #47 was in bed. LVN B was at bedside. The resident's lips were quivering, and she appeared uncomfortable.
During an observation on 07/10/23 at 10:40 a.m., LVN B said the night nurse reported to her that Resident #47 was administered a Tylenol #3 at 5:00 a.m. She said the Tylenol #3 was not charted on the medication administration record. She said the Tylenol #3 was signed out on the narcotic sign out sheet by the previous nurse. LVN B said she was in the dining room at 7:00 a.m. and did not know Resident #47 was still in pain. She said that was why she had not given standing order for Tramadol.
During an interview 07/10/23 at 11:13 a.m., CNA A said she came into work at 6:00 a.m. She said she reported to LVN B that Resident #47 was in pain and shaking at approximately 7:30 a.m. She said Resident #47 had her good days and her bad days. She said on Resident #47's bad days she was hurting and crying.
During an interview on 07/10/23 at 12:14 p.m., LVN B said she first saw Resident #47 while making her first rounds. She said she saw the resident at approximately 6:30 a.m. She said the resident did not appear to be in pain at that time. She said did not chart a follow up on the Tylenol 3 that was given at 5:00 a.m. because it was not charted on the medication administration record. She said the CNA and the therapist did come and tell her the resident was in pain, but she was not sure what time they told her. She said the resident told her at 9:15 that she was having hip pain and rated the pain 10 out of 10. She said she was given a one-time dose of Tramadol at 10:54 a.m.
During an interview on 07/12/23 at 2:49 p.m., the DON said she would have expected the pain medication that was given on 07/10/23 at 5:00 a.m. to have been marked on the medication administration record and that would have triggered a follow up. She said she would have expected Resident #47's pain to have been treated when it was reported to the nurse by the aide at approximately 7:30 a.m. She said pain not being treated in a timely manner could cause the resident to continue to be in pain.
During an interview on 07/12/23 at 3:15 p.m., the Administrator said he would have expected Resident #47's pain to have been addressed timely. He said no one wants to be in pain and they were there to help ensure that they were not.
Review of a Pain Management facility policy dated 12/2017 indicated, .It is the policy of this home that residents experiencing pain will be assessed and pain management provided to the degree possible to provide comfort and enhance the resident's quality of life .Resident will be re-assessed 30 - 60 minutes after pain management interventions to determine the effectiveness of the intervention .nursing staff will assess how pain is affecting mood, activities of daily living, sleep and the resident's quality of life .Resident's with unrelieved pain will be evaluated by the nurse and the physician notified .
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to maintain an infection prevention and control program d...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review the facility failed to maintain an infection prevention and control program designed to provide a safe, sanitary, and comfortable environment and to help prevent the development and transmission of communicable diseases and infections for 2 of 5 residents (Residents #7, Resident #60) reviewed for infection control practices.
The facility failed to ensure Resident #7 and Resident #60's room was sanitized and free from soiled adult briefs.
These failures placed residents at risk for cross contamination and infection.
Findings included:
1. Record review of a face sheet dated 11/07/2023 revealed Resident #7 was a [AGE] year-old female admitted on [DATE] with diagnoses Chronic obstructive pulmonary disease (group of diseases that cause airflow blockage and breathing-related problems), Muscle wasting and atrophy (the wasting or thinning of muscle mass), Dysuria (Discomfort when urinating can have causes that aren't due to underlying disease), Personal history of urinary (tract) infections (An infection in any part of the urinary system, the kidneys, bladder, or urethra) , and Anxiety disorder (persistent and excessive worry that interferes with daily activities).
Record review of Resident #7's annual MDS dated [DATE] revealed a BIMS with a score of 4, which indicated Resident #7 has severely impaired cognition. The MDS also revealed, Resident #7, required total dependence with hygiene. And extensive assistance with dressing. Resident #7 required one-person physical assistance with dressing and hygiene.
Record review of a care plan dated 05/04/2023 shows that Resident #7 needs assistance with ADLs as required during the activity.
2. Record review of a face sheet dated 01/14/2023 revealed Resident #60 was a [AGE] year-old male admitted on [DATE] with diagnoses including dementia (the loss of cognitive functioning - thinking, remembering, and reasoning - to such an extent that it interferes with a person's daily life and activities), psychotic disturbance (A mental disorder characterized by a disconnection from reality), Psychotic disorder with delusions (Paranoid delusion and delusions of grandeur are two examples of psychotic delusions), Anxiety disorder (persistent and excessive worry that interferes with daily activities), and Cellulitis (common bacterial skin infection that causes redness, swelling, and pain in the infected area of the skin).
Record review of Resident #60's annual MDS dated [DATE] revealed a BIMS with a score of 07, which indicated Resident #60 has severely impaired cognition. The MDS also revealed, Resident #60, required extensive assistance with personal hygiene and required a two person assist.
Record review of a care plan dated 05/23/23, revealed that Resident #60 has the following long-term goal, Will maintain a sense of dignity by being clean, dry, odor free and well-groomed over next 90 days.
During an observation and interview on 07/10/2023 at 7:26 a.m., Resident #7 had soiled briefs on the floor of her bedroom. The room smelled of feces and urine. When asked if it bothered the resident, she did not answer the question and spoke of a different matter.
During an observation and interview on 07/10/2023 at 11:25 a.m., Resident #7 had soiled briefs on the floor of her bedroom.
During an observation and interview on 07/10/2023 at 2:31 p.m., Resident #7 had soiled briefs on the floor of her bedroom.
During an interview and observation on 7/10/2023 at 7:36 a.m., Resident #60 stated that he is being treated well by staff and has no problems. He stated that he urinates in his briefs. He stated that he did not care. He stated that he did not want a nurse to clean him up. Observed that the room had a strong smell of ammonia and urine. Observed used and soiled briefs laying on the tile floor under a sink in the main bedroom. Resident #60 stated that they have been there all night.
During an interview on 07/10/23 at 11:19 a.m., Housekeeper M. She stated that she works 4 days a week Mon through Thursday. She stated that sometimes she takes soiled diapers out of the rooms. She stated that it is the CNAs job to remove the dirty diapers from rooms because she is not supposed to touch anything with bodily fluids on it. She stated that she disposes of soiled diapers when the aides don't do it. She stated that she has scrubbed the floor multiple times in Resident #60's room and she can't get rid of the ammonia and urine smell. She stated that everybody knows that the ammonia and urine smell this bad. She stated that she tries to clean his room the best she can. She stated that Resident #60 urinates on himself because he doesn't want to get up to go urinate in the bathroom. She stated that she has to clean his room every time she goes in there because of the urine. She stated that often times soiled diapers are laying on the floor.
During an interview and observation on 07/11/2023 at 11:57 a.m., Resident #60 stated again that he did not want to be cleaned up. The smell an odor from Resident #60's room carried into the hallway. Resident #60 had soiled briefs laying on the tile floor under a sink in the main bedroom.
During an interview on 07/11/23 at 12:03 p.m., LVN B stated that she works down the hall with Resident #60. She stated that his room always smells like urine and feces. She stated that he refuses care frequently. She stated that he does let staff shower him about once a week with a lot of encouragement. She stated that she hasn't heard any other residents voice concerns about Resident #60. She stated that he usually doesn't start leaving his room until afternoon around 2:00 p.m. or 3:00 p.m. She stated that it is best to not go into his room early because he is more likely to refuse treatment. She stated that his smell is pretty bad. She stated that you can smell him in the hallways. She stated that sometimes you can smell him inside his room from out in the hallway even after staff clean the room. She stated that his room smells like urine and feces. She stated that in his room there are often times soiled adult briefs on the floor. She stated that primarily it is the CNAs responsibility to ensure that soiled briefs are disposed of and not left on the floor but any staff including herself can do that.
During an interview on 7/12/2023 at 1:11 p.m., with the ADM, he stated that he expects that his CNAs dispose of dirty briefs in the rooms of residents. He stated that it is not okay to leave dirty briefs on the tile floor. He stated that there is a potential for infection when a staff leaves dirty briefs on the floor. He stated that any staff that saw the dirty briefs should have disposed of them rather than let them lay on the floor.
During an interview on 7/12/2023 at 1:39 p.m., with the DON, she stated that she expects staff to follow company policy regarding infection control. She stated that she expects staff to not leave dirty briefs on the floor anywhere in the facility. She stated that soiled briefs should be placed in a trash bag in the room and then take them into the soiled linen room where there is a place to dispose of soiled briefs. She stated that residents can be placed at risk for infections if the resident were to touch the brief or touch the floor where the brief was located.
Review of facility policy effective December of 2017 titled, Infection control - Prevent Spread of Infection revealed that the purpose of this policy was to, It is the policy of this home that residents with infectious diseases are isolated appropriately and that employees with communicable diseases or infectious lesions will not perform client care or handle resident food to prevent the spread of infection. The Director of Nursing or Designee will develop, in conjunction with the physician and the Interdisciplinary Care Plan Team, a plan of care to contain the spread of infection, with the least amount of restriction or isolation to the resident.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents had the right to reside and receive ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents had the right to reside and receive services in the facility with reasonable accommodation of resident needs and preferences for 4 of 20 residents (Residents #17, #36, #56, and #15) reviewed for reasonable accommodations.
The facility failed to ensure Residents #17, #36, #56, and #15's call lights were accessible.
This failure could place residents at risk of injuries, health complications and decreased quality of life.
Findings included:
1. Review of Resident #17's undated electronic face sheet revealed she was admitted to the facility on [DATE] with diagnoses of rheumatoid arthritis (an autoimmune and inflammatory disease, which means that your immune system attacks healthy cells in your body by mistake, causing inflammation (painful swelling) in the affected parts of the body), diabetes mellitus type 2 (group of diseases that result in too much sugar in the blood (high blood glucose), and depression (a common and serious medical illness that negatively affects how you feel, the way you think and how you act).
Record review of Resident #17's quarterly MDS assessment dated [DATE] revealed a BIMS with a score of 15, which indicated Resident #17 had no cognitive deficit. The MDS also revealed, Resident #17, required extensive assistance of one staff member for eating and no limited range of motion was noted on the MDS.
Record review of Resident #17's care plan dated 05/24/2023 indicated Resident # 17 had contractures to her bilateral upper extremities which increased her risk for skin breakdown, pain, and injury. The intervention listed for the contracture care plan for Resident #17 was to assist with repositioning often, use positioning devices to maintain proper body alignment and position bilateral upper extremities on pillows for comfort.
During an interview and observation on 07/10/2023 at 08:35 a.m., Resident # 17 had no call light in reach. The touch pad call light was secured to the privacy curtain, approximately 3 feet from Resident #17's bed. A sign was observed above the bed of Resident #17 that read: Ensure (Resident #17) had call light in hand prior to leaving the room. Resident #17 said the CNAs told her they do not have time to answer her call light every hour. Resident #17 said her call light is rarely in her reach because of her contractures. Resident #17 said the call light must be placed on left side for her to reach it. Resident #17 said she does press the call light more than most when it was in reach because she had muscle spasms, and her limbs would start to hang off the bed after a while and she needed to be repositioned or she would fall.
During an observation on 07/10/2023 at 1:55 p.m., Resident # 17 had no call light within reach. Resident #17's call light was pinned to the privacy curtain, approximately 3 feet from Resident #17's bed.
During an observation on 07/10/2023 at 3:40 p.m., Resident #17 was observed had no call light within reach. Resident #17's call light was pinned to the privacy curtain, approximately 3 feet from Resident #17's bed.
2. Review of Resident #36's undated electronic face sheet revealed that she was admitted to the facility on [DATE] with diagnoses of dementia (the loss of cognitive functioning - thinking, remembering, and reasoning - to such an extent that it interferes with a person's daily life and activities), hypothyroidism (a common condition where the thyroid doesn't create and release enough thyroid hormone into your bloodstream), and insomnia (having trouble falling asleep, staying asleep, or getting good quality sleep).
Record review of Resident #36's significant change MDS assessment dated [DATE] revealed a BIMS score of 09, which indicated resident #36 had a moderate cognitive deficit. The MDS also revealed, Resident #36, was independent with set up for eating and had limited range of motion to her upper and lower extremities on one side.
Record review of Resident #36's care plan revealed the last updated was 05/22/2023. Resident #36's ADL care plan revealed she required set up and supervision for eating and had no care plan was initiated for limited range of motion.
During and observation and interview on 07/10/2023 8:20 a.m., Resident #36 was noted to be in bed on her right side. The bed was in lowest position, approximately 6-12 inches from the floor. Resident #36's breakfast tray with cover was on rolling bedside table in high position, approximately 3.5 feet from the floor. Resident #36 was unable to see or reach her tray. Resident #36 was asked if she was going to eat, and she replied she was just thirsty and did not want the food. Resident #36 said she could not reach her drink. Resident #36's call light was not in reach; it was pinned to the privacy divider curtain 4 to 6 feet from resident.
During an observation on 07/11/2023 at 12:38 p.m., Resident #36's call light was pinned to privacy curtain, 4-6 feet from the reach of Resident #36. Resident #36 stated it would be nice to be able to able to reach the call light so she could get someone to help her get a drink when she was thirsty.
3. Review of Resident #56's undated electronic face sheet revealed that she was admitted to the facility on [DATE] with diagnoses of Alzheimer's disease (a gradual decline in memory, thinking, behavior and social skills), major depressive disorder (mental health disorder characterized by persistently depressed mood or loss of interest in activities, causing significant impairment in daily life), psychotic disorder with delusions (person with psychosis will often believe an individual or organization is making plans to hurt or kill them).
Record review of Resident #56's quarterly MDS assessment dated [DATE] revealed a BIMS with a score of 12, which indicated resident #56 had a mild cognitive deficit. The MDS also revealed, Resident #56, was extensive assist of one staff member for eating.
Record review of Resident #56's care plan revealed it was last updated 01/16/2023. Resident #56 had a care plan for fall risk with an intervention of keeping call light within reach.
During an interview and observation on 07/10/2023 at 7:35 a.m., Resident #56's call light was behind headboard on floor. Resident #56 said she needed to be adjusted in bed because her back hurt. Resident #56 said she had been waiting for a while (unable to give exact amount of time) for someone to come along.
During observation on 07/11/2023 at 10:30 a.m., Resident #56's call light was pinned to top of fitted sheet out of the reach of resident.
4. Review of Resident #15's undated electronic face sheet revealed that she was admitted to the facility on [DATE] with diagnoses of dementia (the loss of cognitive functioning - thinking, remembering, and reasoning - to such an extent that it interferes with a person's daily life and activities), hypertension (when the pressure in your blood vessels is too high (140/90 mmHg or higher), and chronic kidney disease (your kidneys are damaged and can't filter blood the way they should).
Resident #15's quarterly MDS assessment dated [DATE] revealed a BIMS with a score of 03, which indicated resident #15 had a severe cognitive deficit. The MDS also revealed, Resident #15, was extensive assist of one staff member for all ADLs except eating. Eating for Resident #15 was coded as supervision of staff member.
Record review of Resident #15's care plan revealed it was last updated 07/05/2023. Resident #15 had a care plan for fall risk with an intervention of keeping call light within reach.
During an observation on 07/10/2023 at 7:38 a.m., Resident #15's call light was pinned on the privacy curtain approximately 6-8 feet from resident's reach.
During observation and interview on 07/11/2023 at 11:00 a.m., Resident #15 was attempting to get out of bed with empty water pitcher in hand. Resident #15 said he was going to get some iced water. Resident #15's call light was pinned on the privacy curtain approximately 6-8 feet from resident's reach.
During an interview on 07/11/2023 at 10:12 a.m., CNA P said she was aware that all residents should have their call lights within reach of the resident. CNA P said call lights were to be in reach so the residents could ask for assistance or signal they had an emergency.
During an interview on 07/11/2023 at 3:45 p.m., CNA R said she worked the 2-10 p.m. shift and worked short 2 out of 4 days per week that she worked. CNA R said there may have been a time or two that she was working so quickly that she failed to put a call light back in the reach of a resident. CNA R said she understood the residents needed to be able to signal for assistance by having a call light in reach.
During an interview on 07/11/2023 at 4:00 p.m., LVN Q said that all residents should always have their call lights within reach. LVN Q said it was important for the residents to be able to call for help in case of an emergency or if they needed assistance with going to the restroom or transferring. LVN Q said she sometimes (maybe once per week) found the call lights out of reach of the residents but would clip them to the resident or the bed when she found them. LVN Q said she would remind the CNAs to be mindful of call light placement.
During an interview on 07/12/2023 at 3:00 p.m., the DON said she expected every resident to have a call light in reach. The DON said she was unaware that Resident #17, #36, #56, and #15's call light was not in reach on multiple observations. The DON said it was important to prevent injury for residents at risk for falls to have their call lights in reach.
During an interview on 07/12/2023 at 3:30 p.m., the Administrator said it was very important for all residents to have access to their call lights. The Administrator said it was his expectation that each resident be able to always call for assistance day and night to prevent accidents and to ensure the residents feel their needs were being met.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide a safe, functional, sanitary, and comfortable...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide a safe, functional, sanitary, and comfortable environment for 3 of 10 residents reviewed for environment. (Resident #60, Resident #57, and Resident #28)
The facility failed to control Resident #60's odor and provide a comfortable environment.
These failures could place residents at risk of an unsafe or uncomfortable environment and a decrease in quality of life and self-worth.
Findings included:
1. Record review of a face sheet dated 01/14/2023 revealed Resident #60 was a [AGE] year-old male admitted on [DATE] with diagnoses including dementia (the loss of cognitive functioning - thinking, remembering, and reasoning - to such an extent that it interferes with a person's daily life and activities), psychotic disturbance (A mental disorder characterized by a disconnection from reality), Psychotic disorder with delusions (Paranoid delusion and delusions of grandeur are two examples of psychotic delusions), Anxiety disorder (persistent and excessive worry that interferes with daily activities), and Cellulitis (common bacterial skin infection that causes redness, swelling, and pain in the infected area of the skin.)
Record review of Resident #60's annual MDS dated [DATE] revealed a BIMS with a score of 07, which indicated resident #60 has severely impaired cognition. The MDS also revealed, Resident #60, required extensive assistance with personal hygiene and required a two person assist.
Record review of a care plan dated 05/23/23, revealed that Resident #60 has the following long-term goal, Will maintain a sense of dignity by being clean, dry, odor free and well-groomed over next 90 days.
2. Record review of a face sheet dated 03/28/2023 revealed Resident #57 was a [AGE] year-old male admitted on [DATE] with diagnoses including Multiple sclerosis (a potentially disabling disease of the brain and spinal cord (central nervous system), Muscle wasting and atrophy (the wasting or thinning of muscle mass), and Anxiety disorder (persistent and excessive worry that interferes with daily activities.)
Record review of Resident #57's annual MDS dated [DATE] revealed a BIMS with a score of 15, which indicated resident #57is cognitively intact.
3. Record review of a face sheet dated 01/09/2023 revealed Resident # 28 was a [AGE] year-old male admitted on [DATE] with diagnoses including diabetes mellitus (a disease of inadequate control of blood levels of glucose), Gastro-esophageal reflux disease (A digestive disease in which stomach acid or bile irritates the food pipe lining), Muscle weakness (commonly due to lack of exercise, ageing, muscle injury or pregnancy), Cognitive communication deficit (difficulty with thinking and how someone uses language.)
Record review of Resident #28's annual MDS dated [DATE] revealed a BIMS with a score of 07, which indicated resident #28 has severely impaired cognition.
During an interview on 07/11/2023 at 11:15 a.m., Resident # 57 stated that Resident #60's smell bothers him. He stated that he thinks that staff should force him to take a shower. He stated that he felt Resident #60 should take a shower or leave the building. He stated that every time he is near Resident #60 the smell is enough to make him vomit. He said that he doesn't want to eat in the dining room because of his terrible smell. He stated that he has complained about it but staff said that he refuses to shower or let anyone clean him or his room. He stated that his smell travels down the hallway and you can smell him even after he passes by. He stated that the smells coming from him made him want to find somewhere else to live.
During an interview on 07/11/2023 at 11:45 a.m., Resident #28 stated that he knows who Resident # 60 is. He stated that he calls him, stinky. He stated that he stinks to High Heaven. He stated that his smell bothers him because he can smell him all the way across the hall. He stated that he also smells him when he is sitting in the lobby area. He stated that he can smell him because he is always going down the hall so he can go outside and smoke. He said the smells are affecting his life at the facility. He said that if Resident #60 was in the lobby he would leave and not go sit and watch outside the window like he prefers to do.
During an attempted interview on 07/11/2023 at 11:57 a.m., Resident # 60, Attempted to speak to resident about showering and cleaning up. He refused to speak.
During an interview on 07/11/23 at 12:01 p.m., Housekeeper M stated that Resident # 60 refuses to do anything about the way he smells or his hygiene. She stated that he gets violent about it when you ask him because he does not want to get up to shower or allow you to change his sheets. She stated that he sometimes is able to be encouraged to shower by giving him extra cigarettes. She stated that he has been like this since he has been here at the facility. She stated that when he refuses all they can do is tell the charge nurse because he has the right to refuse to bathe. She stated that residents down his hall complain about the smell, but you can't get the bad smell out by mopping or cleaning because it is him and his clothes that smell so bad. She stated that usually when he does get up and goes to get a cigarette they will go into his room and try to clean up and change his sheets before he gets back.
During an interview on 07/11/23 at 12:13 p.m., LVN # B stated that she works down the hall with Resident # 60 She stated that his room always smells like urine and feces. She stated that he refuses care frequently including allowing staff to bathe him and to change his sheets and clothes. She stated that he does let them shower him about once a week with a lot of encouragement. She stated that she hasn't heard any other residents voice concerns about Resident #60's odors. She stated that he usually doesn't start leaving his room until afternoon around 2:00 p.m. or 3:00 p.m. She stated that it is best to not go into his room early because he is more likely to refuse treatment. She stated that his smell is pretty bad as you can smell him in the hallways even when he isn't there or after he gone down the hall to smoke. She stated that sometimes you can smell him inside his room from out in the hallway even after they clean the room. She stated that his room smells like urine and feces constantly. She stated that in his room there are often soiled adult briefs on the floor. She stated that it is primarily the CNAs responsibility to ensure that soiled briefs are disposed of and not left on the floor but any staff including herself can do that.
During an interview and observation on 07/11/23 at 12:20 p.m., CNA N. She stated that she works the hall with Resident #60. She stated that Resident #60 has hygiene issues. She stated that she was able last to get him take a shower last Saturday, 7/8/2023. She stated that she has asked him to take a shower before he smokes but he will just refuse. She stated that he got pissed at her when she asked but he needed it really bad. She stated that he refuses to take a shower or let staff clean the room. She stated that he will cuss at staff and fight them to not clean up. She stated that she tried yesterday to clean his sheets and he yelled, Get the F out of here. She stated that he comes down the hall all nasty and dirty wanting cigarettes. She stated that the residents in this hall have complained about the smell. She stated that Resident #28 and Resident # 57 complained to her saying they were offended by the smells. She stated that she gets tired of smelling it too. She stated that she doesn't blame them for smelling. She stated that even after staff clean the room, he smells so bad it gets the room back smelling terrible. Went down hall and tried to get Resident #60 to shower and change bed sheets. Resident #60 refused.
During an interview on 07/12/2023 at 1:39 p.m., the ADM stated that he expects that staff keep odors from residents to a reasonable level and that other residents will not be affected by the odors coming from the room of residents with hygiene issues. The ADM stated that there is no facility policy regarding maintaining a homelike environment or controlling odors.
During an interview on 07/12/2023 at 1:39 p.m., the DON stated that she expects staff to reasonably control odors in the building and prevent offensive odors from effecting the quality of life of other residents. She stated that Resident's rooms should be cleaned, and interventions should be in place to ensure that odors are controlled.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to develop and implement a comprehensive person-centered care plan to...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview, and record review, the facility failed to develop and implement a comprehensive person-centered care plan to meet each resident's medical, nursing, mental and psychosocial needs for 3 of 20 residents reviewed for care plans. (Resident #270, Resident #47, and Resident #36)
The facility failed to develop a comprehensive person-centered care plan including an active problem of diabetes mellitus for Resident #270.
The facility failed to develop a comprehensive person-centered care plan including an active problem of pain for Resident #47.
The facility failed to develop a comprehensive person-centered care plan for a significant change in status for Resident #36.
These failures could place residents at risk of not having individual needs met, a decreased quality of life, and cause residents not to receive needed services
Findings include:
1. Record review of a face sheet dated 03/20/2023 revealed Resident #270 was [AGE] years old female and was admitted on [DATE] with diagnoses including Type 2 diabetes mellitus (problem in the way the body regulates and uses sugar as a fuel), Muscle wasting and atrophy (the wasting or thinning of muscle mass), abnormalities of gait and mobility (General causes of abnormal gait may include: Arthritis of the spine, hip, leg, or foot joints).
Record review of the most recent MDS dated [DATE] indicated Resident #270 was understood and understood others. The MDS indicated a BIMS score of 15 showing that Resident #270 was cognitively intact. Record review shows that Resident #270 MDS section V care area assessment summary was triggered for ADL Functional/Rehabilitation Potential, Urinary Incontinence and Indwelling Catheter, Falls, Nutritional Status, and Pressure Ulcers. Also revealed that Resident #270 had an active diagnosis of Diabetes.
Record review of a care plan dated 03/29/2023 revealed Resident #270 was not care planned for ADL Functional/Rehabilitation Potential, Urinary Incontinence and Indwelling Catheter, Falls, Nutritional Status, Pressure Ulcers, and Diabetes.
During an interview on 7/12/2023 at 1:11 p.m., the ADM stated that he expects that their care plans accurately reflect their resident's needs. He expects that if a resident needed to have their blood sugar checked with a finger stick blood sugar test it would be on their care plan as well as with any other active diagnoses or treatments ordered.
During an interview on 7/12/2023 atn1:39 p.m. the DON stated that she expects that resident's care plans are accurate and up to date. She stated that caregivers who take care of a resident may not know the needs of a resident if all care for that specific resident is not documented in the resident's file. She stated that finger stick blood sugar tests should be care planned and that Resident #270 had a doctor's order for this test to be completed. She stated that all of Resident's care should be documented on their care plan. She stated that she did not know why Resident # 270's care plan had not been fully developed.
Review of facility policy titled, Care Plans, Comprehensive Person-Centered facility policy dated December 2017 indicated, It is the policy of this home that staff must develop a comprehensive care plan to meet the needs of the resident. Review CAA (Care Area Assessment) triggers on the MDS. If the interdisciplinary Team decides to proceed with care planning, list the problem. The specific problem as well as the underlying cause should be listed.
2. Record review of a face sheet dated 07/10/23 revealed Resident #47 was [AGE] years old and was admitted on [DATE] with diagnoses including dementia, muscle spasms, and Parkinson's Disease (a disorder of the central nervous system that affects movement, including tremors).
Record review of current physician's orders indicated an open-ended order with a start date of 06/27/23 for Tylenol #3 (an opioid pain medication), 1 tab every 4 hours as needed for pain. The orders indicated an open-ended order with a start date of 10/05/22 for Tramadol (narcotic used to treat moderate to severe pain) 50 milligrams every 6 hours as needed for pain.
Record review of the most recent MDS dated [DATE] indicated Resident #47 was understood and understood others. The MDS indicated a BIMS of 15 indicating no cognitive impairment for Resident #47. The MDS indicated Resident #47 an active diagnosis of unspecified pain. The MDS indicated Resident #47 had received scheduled pain medication and PRN (as needed) pain medication during the 5 previous days. The MDS was electronically signed on 06/06/23 by the MDS Coordinator indicating she had completed the assessment for Section J of the MDS.
Record review of a care plan last revised on 07/09/2023 indicated Resident #47 did not indicate pain as a problem area.
During an interview on 07/13/23 at 2:17 p.m., the MDS Coordinator she said problems that were triggered on the MDS should have been care planned as soon as the MDS was complete. She said she did not know why Resident #47's pain had not been care-planned. She said 07/10/23 was the first day she knew Resident #47 had a problem with pain. She said the problem had not been reported to her. She said nurses looking at Resident #47 care-plan would not know about the problem. She said the nurses did not look at the care plans. She said a care plan was used to give a plan of care for each resident.
Review of a Pain Management facility policy dated 12/2017 indicated, .A care plan will be completed with goals for pain treatment, pharmacological and non-pharmacological interventions. Plan will be updated appropriately .
3. Review of Resident #36's undated electronic face sheet revealed that she was admitted to the facility on [DATE] with diagnoses of dementia (the loss of cognitive functioning - thinking, remembering, and reasoning - to such an extent that it interferes with a person's daily life and activities), hypothyroidism (a common condition where the thyroid doesn't create and release enough thyroid hormone into your bloodstream), and insomnia (having trouble falling asleep, staying asleep, or getting good quality sleep).
Record review of Resident #36's significant change MDS assessment dated [DATE] revealed a BIMS with a score of 09, which indicated resident #36 had a moderate cognitive deficit. The MDS also revealed, Resident #36, was independent with set up for eating and had limited range of motion to one side of her upper and lower body.
Record review of Resident #36's care plan revealed no care plans were created for Care Area Assessments trigged on 06/22/2023 significant change MDS assessment.
Care Areas Triggered were cognitive status, ADL status, incontinence, nutritional status, pressure ulcers, and psychotropic drug use.
During an interview on 07/12/2023 at 2:45 p.m., the MDS Coordinator stated that a significant change assessment required a new comprehensive care plan to be developed. The MDS Coordinator was unaware that a comprehensive care was not developed for Resident #36. The MDS Coordinator stated the care plan was used as a guide to ensure care specific to each resident was delivered.
During an interview on 07/12/2023 at 3:30 p.m., the DON stated it was the responsibility of the MDS Coordinator to ensure all care plans were developed and current, and it was the responsibility of the interdisciplinary team (social worker, activities director, dietary manager, nursing, therapy) to add resident specific problems and interventions to the care plan once developed. The DON stated care plans were a map to direct specific resident care and needed to be as accurate as possible.
During an interview on 07/12/2023 at 3:45 p.m., the Administrator stated it was the MDS Coordinator's responsibility to initiate MDS triggered care plans. The Administrator stated it was the responsibility of everyone that worked with the resident to ensure the care plans were resident specific. The Administrator stated it was his expectation that the care plans were up to date and resident specific at all times.
Review of a facility policy titled Care Plans dated 12/2017 revealed the resident care plan was used to plan and assign care for all disciplines. The resident care plan must be kept current at all times.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide the necessary services to maintain personal h...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to provide the necessary services to maintain personal hygiene for 5 of 20 residents reviewed for ADLs (Resident #2, Resident #33, Resident #37, Resident #10, and Resident #44).
The facility failed to remove facial hair from female Resident #2 and female resident #37.
The facility failed to clean the fingernails of Resident # 33.
The facility failed to provide scheduled baths/showers for Resident #10 and Resident #44.
These failures could place residents who required assistance from staff for ADLs at risk of not receiving care and services to meet their needs which could result in poor care, risk for skin breakdown, feelings of poor self-esteem, lack of dignity and health.
Findings included:
1. Review of Resident #2's electronic face sheet dated 03/20/2023 revealed that she was admitted to the facility on [DATE] with diagnoses of senile degeneration of brain (severe cortical atrophy and cell loss as well as a high index of dementia as measured by numbers of neurofibrillary tangles (NFT) and neuritic plaques (NP) in neocortex and hippocampus), obsessive-compulsive disorder (chronic, and long-lasting disorder in which a person has uncontrollable, reoccurring thoughts (obsessions) and/or behaviors (compulsions) that he or she feels the urge to repeat over and over), expressive language disorder (trouble using language), severe intellectual disabilities (major delays in development, and individuals often have the ability to understand speech but otherwise have limited communication skills), major depressive disorder (A mental health disorder characterized by persistently depressed mood or loss of interest in activities, causing significant impairment in daily life)
Record review of Resident #2's annual MDS dated [DATE] revealed a BIMS with a score of 5, which indicated resident #12 has severely impaired cognition. The MDS also revealed, Resident #2, required extensive assistance with personal hygiene. Resident #2 required one-person physical assistance with personal hygiene, including shaving.
During an interview and observation on 07/10/2023 at 07:40 AM Resident # 2 had multiple chin hairs approximately 8 that appeared to be one to one and a half inches in length. Resident #2 did not respond to being asked, if it bothered her that she had long chin hairs on her face she continued to yell unintelligible words. Surveyor asked if she would like her face to be shaved and she was unable to answer.
During an observation on 07/11/2023 at 09:05 a.m., Resident # 2 was observed with chin hairs approximately one to one and a half inches in length. There were approximately 8 chin hairs visible to the surveyor.
During an observation on 07/11/2023 at 2:02 p.m., Resident # 2 was observed with chin hairs approximately one to one and a half inches in length. There were approximately 8 chin hairs visible to the surveyor.
During an interview on 07/12/2023 at 1:39 p.m., the ADM stated that he expects that his staff are to shave residents who are dependent of care. He stated that it is a dignity issue that residents who prefer to be clean shaved have facial hair. He stated that staff are to follow all facility policies including their policy on ADLs
During an interview on 07/12/2023 at 1:39 p.m., the DON stated that she expects her staff to follow facility policies regarding ADLs and to ensure that dependent residents are shaved. She stated that residents who would prefer to be shaved but could not do this task for themselves were at risk for feeling low self-esteem and a loss of their dignity.
2. Record review of the face sheet dated 07/12/23 indicated Resident #37 was [AGE] years old and admitted on [DATE] with diagnoses including unsteadiness on feet, muscle wasting, and heart failure.
Record review of the MDS dated [DATE] indicated Resident #37 was understood and understood others. The MDS indicated a BIMS score of 15 which indicated Resident #37 was cognitively intact. The MDS indicated Resident #37 required supervision with personal hygiene.
Record review of a care plan revised on 05/24/23 indicated Resident #37 had an ADL self-care performance deficit. The goal was for Resident #37 to be clean and well-groomed with staff assistance for the next 90 days. There was an intervention for limited assistance with personal hygiene.
Record review of a Point of Care ADL Report for Resident #37 and dated 07/01/23 - 07/12/2023 indicated the resident last received assistance with personal hygiene on 07/10/23 and had last been bathed on 07/09/23. The documentation did not indicate any refusals for personal hygiene or bathing.
Record review of Progress Notes for Resident #37 did not indicate any progress notes for 07/23.
During an observation on 07/10/23 at 9:22 a.m., Resident #37 was sitting on her bed in her room. The resident had many dark hairs and a few gray hairs approximated 0.25 centimeters in length on the chin and many dark hairs on her upper lip.
During an observation on 07/11/23 at 1:14 p.m., Resident #37 was walking in hallway with her walker. The resident had many dark hairs and a few gray hairs approximated 0.25 centimeters in length on the chin and many dark hairs on her upper lip.
During an observation and interview on 07/12/23 at 1:16 p.m., Resident #37 said she did not like when her chin hairs were grown out. She said she had hair to her upper lip too. She said there had been times when she had asked staff for a razor. She said it was embarrassing having facial hair. During the interview the resident was tearful.
3. Record review of the face sheet dated 07/11/23 indicated Resident #33 was [AGE] years old and admitted on [DATE] with diagnoses including dementia, generalized anxiety disorder, and major depressive disorder (a mood disorder that causes a persistent feeling of sadness and loss of interest).
Record review of the MDS dated [DATE] indicated Resident #33 was usually understood and usually understood others. The MDS indicated a BIMS score of 7 which indicated Resident #33 was severely cognitively impaired. The MDS indicated Resident #33 required extensive to total assistance from staff for activities of daily living. Resident #33 was totally dependent for personal hygiene.
Record review of a care plan revised on 06/26/23 indicated Resident #33 had an ADL self-care performance deficit and limited mobility. The care plan indicated Resident #33 required total assistance with bathing.
Record review of a Point of Care ADL Report for Resident #37 and dated 07/01/23 - 07/12/2023 indicated the resident had received assistance with personal hygiene 07/01/23 - 707/12/23 and had received scheduled baths. The documentation did not indicate any refusals for personal hygiene or bathing.
Record review of Progress Notes dated 07/23 for Resident #33 did not indicate any refusals of care or family being notified of a refusal.
During an observation on 07/10/23 at 8:00 a.m., Resident #33 was eating in the dining room with a dark substance under his fingernails on his left hand. When asked what was under his nails he said, probably shit.
During an observation on 07/10/23 at 2:50 p.m., Resident #33 was in bed. There was a dark substance under his fingernails on his left hand.
During an observation and interview on 07/11/23 at 3:36 p.m., Resident #33 was lying in bed. Dark brown substance under fingernails on left hand. He said no one ever cleans under his nails. He said he would like his nails clean and trimmed.
During an interview on 07/12/23 at 1:50 p.m., CNA J said the aides were responsible for removing facial hair from women. She said that was part of providing care. She said anytime she saw facial hair on women she removed the hair. She said she checked fingernails on shower days. She said she offered to cut Resident #33's nails on 07/07/23 and he had refused. She said did not chart the refusal but had reported it to the nurse. She said some days Resident #33 would let you provide care and some days he would not.
During an interview on 07/12/23 at 2:00 p.m., CNA H said aides were responsible for removing facial hair on women. She said if the aides saw facial hair on women, it should be removed if the resident allows. She said refusals were reported to the nurse. She said refusals were then charted in the ADL charting. She said aides were responsible for cleaning under residents' fingernails. She said since Resident #33's nails were dirty an aide should have cleaned them.
During an interview on 07/12/23 at 2:07 p.m., LVN B said nursing staff was responsible for removing facial hair and cleaning out resident's fingernails. She said aides were to report refusals to the nurses. She said the nurses chart any refusals in the progress notes. She said Resident #33 refusing nail care had not been reported to her. She said facial hair should be removed from females as soon as it could be seen. She said any refusals should be noted in the progress notes.
During an interview on 07/12/23 at 2:32 p.m., CNA K said women like to be cute and they should be shaved if they have facial hair. She said the aides were responsible for removing facial hair from the residents. She said if any resident refused, they reported the refusal to the nurse. She said Resident #33 was easy to do and he listened to her. She said she felt like he would let her clean his nails.
During an interview on 07/12/23 at 2:49 p.m., the DON said CNAs were responsible for removing facial hair from female residents. She said as soon as the aide saw the facial hair, the hair should be removed. She said she would have expected for Resident #37's facial hair to have been removed. She said females with facial hair could cause a decrease in their self-esteem and be embarrassed by it. She said CNAs or nurse could clean fingernails. She said nails should be cleaned if they were dirty. She said if the resident refused, staff should re-attempt to clean their nails or get another person to attempt. She said the refusal should have been reported to the nurse. She said if the resident still refused, a family member should be contacted to see if they can help. She said refusals should be charted in the ADL documentation and in the progress notes.
During an interview on 07/12/23 at 3:15 p.m., the Administrator said CNAs were responsible for ADL care, including removing facial hair and nail care. He said his expectation for facial hair on women was for it not to be there. He said he would expect all residents' nails to be kept clean. He said women with facial hair could contribute to less sense of dignity and dirty nails could be an infection control issue.
4. Review of Resident #44's face sheet revealed Resident #44 was an [AGE] year-old female, admitted on [DATE] with the diagnosis of diabetes mellitus type 2 (chronic condition that affects the way the body processes blood sugar (glucose), anxiety (a feeling of fear, dread, and uneasiness), and cellulitis (a common bacterial skin infection that causes redness, swelling, and pain in the infected area of the skin).
Record review of Resident #44's quarterly MDS assessment dated [DATE] indicated Resident #44 had a BIMs of 10, which indicated a moderate memory impairment. The MDS indicated Resident # 44 required extensive assistance of staff member for bathing. No refusals of care were noted.
Record review of Resident #44's care plan dated 07/05/2023 indicated Resident #44 required limited assist of one to two staff members for bathing. Resident #44 had a care plan for incontinence with an intervention to keep skin clean and dry. No refusals of care were care planned.
Record review of the point of care ADL report dated 05/26/2023 to 07/12/2023 indicated, Resident #44 received a bath/shower on 06/05/2023, 06/07/2023, 06/12/2023, and 06/23/2023. No other bath/showers were documented. Resident #44's bath/shower schedule was every Monday, Wednesday, and Friday on the 2-10 shift. Resident #44 missed baths/showers on 05/26/2023, 05/29/2023, 05/31/2023, 06/02/2023, 06/09/2023, 06/14/2023, 06/16/2023, 06/19/2023, 06/21/2023,06/26/2023, 06/28/2023, 06/30/2023, 07/03/2023, 07/05/2023, 07/07/2023, and 07/10/2023.
During an interview on 07/10/2023 at 8:19 a.m., Resident #44 stated she had not received a bath in over one week. Resident #44 stated she admitted in March and had not gotten more than one bath in a week since admission. Resident #44 stated she was incontinent at times and her skin itched from not being bathed regularly and she had cellulitis currently on her lower extremities. Resident #44 stated her husband was her roommate and he kept a calendar of when they received bathes/showers. Resident #44 stated the staff told her they were short staffed an unable to get to all bathes.
5.Review of Resident #10's undated face sheet revealed Resident #10 was an [AGE] year-old male, admitted on [DATE] with the diagnosis of anemia (a condition that develops when your blood produces a lower-than-normal amount of healthy red blood cells), hypertension (when the pressure in your blood vessels is too high (140/90 mmHg or higher), and depression (A group of conditions associated with the elevation or lowering of a person's mood).
Record review of Resident #10's quarterly MDS assessment dated [DATE] indicated Resident #10 had a BIMs of 15, which indicated a no memory impairment. The MDS indicated Resident #10 required extensive assistance of 1 staff member for bathing. The MDS also indicated Resident #10 was occasionally incontinent of bladder and frequently incontinent of bowel. No refusals of care were noted.
Record review of Resident #10's care plan dated 07/05/2023 indicated Resident #10 required limited assist of one to two staff members for bathing. No refusals of care were care planned.
Record review of the point of care ADL report dated 05/26/2023 to 07/12/2023 indicated, Resident #10 received a bath/shower on 05/26/2023, 05/31/2023,06/05/2023, 06/07/2023, 06/12/2023, and 06/23/2023. No other bath/showers were documented. Resident #10's bath/shower schedule was every Monday, Wednesday, and Friday on the 2-10 shift. Resident #10 missed baths/showers on 05/29/2023, 06/02/2023, 06/09/2023, 06/14/2023, 06/16/2023, 06/19/2023, 06/21/2023,06/26/2023, 06/28/2023, 06/30/2023, 07/03/2023, 07/05/2023, 07/07/2023, and 07/10/2023.
During an interview on 07/10/2023 at 8:25 a.m., Resident #10 stated he kept a calendar of the dates that he and his wife (Resident #44) received their bath/shower. Resident #10 stated they were supposed to get a bath every Monday, Wednesday, and Friday on 2-10 shift. Resident #10 stated he received a bath at most once a week. Resident #10 stated there had been weeks when he had not received a bath at all. Resident # 10 stated the staff always used the excuse of being short staffed. Resident #10 stated he felt dirty and as if he smelled like a cow pasture, and the smell embarrassed him.
During an interview on 07/11/2023 at 10:12 a.m., CNA P stated she worked short about half of the time she worked. CNA P stated there were days when the facility was short that it was not possible to feed all meals, get everyone up and down, cleaned, dried, and give all bathes. CNA P stated she reported it to the nurse and the oncoming CNA when she was unable to get to a resident's bath.
During an interview on 07/11/2023 at 3:45 p.m., CNA R stated she worked the 2-10 p.m. shift and worked short 2 out of 4 days per week that she worked. CNA R stated there were days she had to skip giving a bath or two because there was no time to complete the bath with the other tasks, she was responsible for. CNA R stated she tried to give a quick wash off to the residents she could not bath. CNA R described the wash off as wiping the residents face, arm pits and pubic area with a washcloth.
During an interview on 07/12/2023 at 3:30 p.m., the DON stated all residents were scheduled to have assistance with bathing three days per week. The DON stated Resident #44 and Resident #10 were Monday, Wednesday, Friday bathes on the 2-10 p.m. shift. The DON stated she was not aware of Resident #44 and Resident #10 missing bathes. The DON stated bathes are important for skin integrity and self-esteem.
During an interview on 07/12/2023 at 3:45 p.m., the Administrator stated he expected all residents to get a bath at least 3 days per week. The Administrator stated he was unaware Resident #44 and Resident #10 were missing bathes. The Administrator stated Resident #10 usually came to him with any problems he had. The Administrator stated bathes were important for dignity and hygiene.
Review of the facility policy and procedure on care of Activities of Daily Living dated effective December 2017 revealed that the purpose of the policy is that It is the policy of this home to assure residents have their activities of daily living needs met. Encourage resident to apply shave cream or electric pre-shave himself. Use shaving cream dispenser handle if unable to depress valve with hand. Use build-up razor handle or electric razor holder as necessary. Those with arthritic hands or wrists may find this more comfortable. Physical assist - Assistance will be given (with discretion) for those who need help to initiate or complete various portions of tasks.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on observations, interviews, and record review, the facility failed to ensure drugs and biologicals used in the facility were labeled in accordance with currently accepted professional principle...
Read full inspector narrative →
Based on observations, interviews, and record review, the facility failed to ensure drugs and biologicals used in the facility were labeled in accordance with currently accepted professional principles, included the appropriate accessory and cautionary instructions, and the expiration date when applicable for two of three medication carts reviewed for medications storage (A Wing Nurse Medication Cart and C Wing Nurse Medication Cart).
1.
The facility failed to remove expired over the counter medications from the A Wing Nurse Medication Cart.
2.
The facility failed to remove expired over the counter medications from the C Wing Nurse Medication Cart.
These failures could place residents at risk for not receiving the therapeutic benefit of medications or adverse reactions to medications.
Findings included:
During an observation on 07/12/23 at 9:53 AM, this surveyor reviewed the A Wing Nurse Medication Cart with RN C and found these medications:
*1 stool softener docusate sodium 100mg, Expired April 2023
*1 calcium carbonate 500mg, Expired December 2022
*1 nasal spray oxymetazoline HCL 0.05% Nasal decongestant, Expired September 2022
During an interview on 07/12/23 at 09:56 AM, RN C said she was using the A Wing Nurse Cart that day. She said the nurses were responsible for checking the carts to ensure expired medications were removed. She said she was not taught specific times or a routine to check the cart for expired medications. She said she usually checks for expired medications in her free time. She said if residents had received an expired medication the medication could be ineffective, the residents could suffer unexpected side effects, or it could make the residents sick.
During an observation on 07/12/23 at 10:05 AM, this surveyor reviewed the C wing nurse Medication Cart with LVN D and found these medications:
*1 vitamin B12 100 mcg, expired June 2023
*1 bottle of Nutricia pro-stat advanced wound care liquid protein, expired 05/20/23.
During an interview on 07/12/23 at 10:11 AM, LVN D said she was using the C Wing Nurse Medication Cart this day. She said the nurses were supposed to check the carts for expired medications. She said she was not taught by administration on how often she should have checked the medication carts for expired medications. She said she tried to do it at least once a shift. She said if a resident received an expired medication, it could have been ineffective, could make a resident sick, or caused possible side effects.
During an interview on 07/12/23 at 01:12 PM, the ADON said she did not expect the carts to have expired meds. She said started working for the facility on 06/20/23. She said she was going to start checking the carts for expired medications herself. She said she was not sure how often the facility requires the nurses to check the carts for expired medications. She said as a nurse she expected the nurses to check the carts to make sure there was not any expired meds on the cart. She said it was the ADON's responsibility to monitor that the nurses were checking the carts.
During an interview on 07/12/23 at 02:01 PM, the DON said she expected the nurses and medication aides to check the med carts and remove the expired medications. She expected the nurses and medication aides to check the cart at least daily to ensure there were no expired meds on the carts. She said the ADON and DON were responsible for monitoring that the nurses were checking the carts for expired medications. She said if a resident received an expired medication that could cause an adverse reaction or the medication could be ineffective.
During an interview on 07/12/23 at 02:20 PM, the ADON said if a resident received an expired medication it could be contaminated, cause adverse side effects, or the medication could be ineffective.
During an interview on 07/12/23 at 02:44 PM, the Administrator said he did not expect the nurses and medication aides to have expired medications in the medication carts. He said the charge nurses and medication aides were responsible for ensuring the med carts do not have expired medications in them. He said the ADON and DON were responsible for auditing the carts. He said there should have been plenty of opportunity to catch the expired medications. He said residents could have suffered an adverse effect if they took an expired medication.
Record review of the facility's policy, Medication Storage - in the home, effective December 2017, stated:
.12. Outdated, contaminated, or deteriorated medications and those in containers that are cracked, soiled, or without secure closures are immediately removed from stock, disposed of per procedures for medications destruction, and reordered from the pharmacy, if a current order exists .
The policy did not address a routine or how often the medications should be checked.
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide services by sufficient numbers of other nursin...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to provide services by sufficient numbers of other nursing personnel, which included but not limited to nurse aides, on a 24-hour basis to provide nursing care to all residents in accordance with resident care plans for 6 of 20 residents (Residents #38, Resident #33, Resident #37, Resident #44, Resident #10, and #17) reviewed for care and services.
The facility failed to provide sufficient staff on the 6a-2pm, 2pm-10pm,10pm-6am on Friday- Sunday from 04/09/2023 to 07/09/2023 to meet the needs of the residents who required assistance with activities of daily living.
This failure could place residents at risk of injury, skin breakdown, low self-esteem, depression, embarrassment, and psychological harm.
Findings included:
Record review of the PBJ staffing Data Report dated 04/01/2023 to 06/30/2023 indicated the facility triggered for one star staff rating.
Record review of the Facility Assessment Tool updated 04/10/2023 indicated the average daily census was 54 residents and the total minimum number of hours of care per patient day (ppd) would be 3.0 per patient day.
During an interview on 07/10/2023 at 8:38 a.m., the Administrator said the facility attempted to staff 5 CNAs on days shift, 5 CNAs on evening shift, and 3 to 4 CNAs on the night shift. The Administrator said there were 3 nurses on each shift and a medication aide that assisted 100 and 200 hall nurses during the day. The Administrator said that there was just 1 nurse assigned to the secured unit until 07/05/2023, when the census increased and called for a nurse and aide to be on the unit from 6 a.m. to 10 p.m.
Record review of the Staffing Schedule for the weekends (Friday-Sunday) dated 04/09/2023 to 07/09/2023 indicated:
*04/09/23- PPD was 1.86- 5 CNAs on days; 3 CNAs on evenings and 3 CNAs on nights Census was 63 total; 5 on secured unit
*04/14/23- PPD was 2.55- 5 CNAs on days; 4 CNAs on evenings and 3 CNAs on nights Census was 66 total; 6 on secured unit
*04/28/23- PPD was 2.6- 7 CNAs on days; 3 CNAs on evenings and 3 CNAs on nights Census was 69 total; 7 on secured unit
*04/29/23- PPD was 2.37- 6 CNAs on days; 4 CNAs on evenings and 3 CNAs on nights Census was 69 total; 7 on secured unit
*04/30/2023- PPD was 2.34- 4 CNAs on days; 4 CNAs on evenings and 3 CNAs on nights Census was 68 total; 7 on secured unit
*05/05/23- PPD was 2.93- 6 CNAs on days; 4 CNAs on evenings and 3 CNAs on nights Census was 65 total; 7 on secured unit
*05/06/23- PPD was 2.61- 6 CNAs on days; 3 CNAs on evenings and 2 CNAs on nights Census was 64 total; 7 on secured unit
*05/07/23- PPD was 2.10- 6 CNAs on days; 3 CNAs on evenings and 2 CNAs on nights Census was 65 total; 7 on secured unit
*05/12/23- PPD was 2.88- 4 CNAs on days; 3 CNAs on evenings and 3 CNAs on nights Census was 66 total; 6 on secured unit.
*05/13/23- PPD was 2.31- 4 CNAs on days; 2 CNAs on evenings and 2 CNAs on nights Census was 66 total; 6 on secured unit
*05/14/23- PPD was 2.35- 4 CNAs on days; 2 CNAs on evenings and 3 CNAs on nights Census was 66 total; 6 on secured unit
*05/19/23- PPD was 2.27- 4 CNAs on days; 4 CNAs on evenings and 2 CNAs on nights Census was 68 total; 6 on secured unit
*05/20/23- PPD was 2.10- 4.5 CNAs on days; 4 CNAs on evenings and 2 CNAs on nights Census was 67 total; 7 on secured unit
*05/21/23- PPD was 2.10- 5 CNAs on days; 3 CNAs on evenings and 2 CNAs on nights Census was 68 total; 7 on secured unit
*06/09/23- PPD was 2.60- 4 CNAs on days; 3 CNAs on evenings and 4 CNAs on nights Census was 66 total; 8 on secured unit
*06/10/23- PPD was 2.61- 7 CNAs on days; 3 CNAs on evenings and 3 CNAs on nights Census was 66 total; 8 on secured unit
*06/24/23- PPD was 1.90- 3 CNAs on days; 3 CNAs on evenings and 2 CNAs on nights Census was 65 total; 9 on secured unit
*07/01/23- PPD was 2.50- 3 CNAs on days; 4 CNAs on evenings and 2 CNAs on nights Census was 69 total; 11 on secured unit
*07/02/23- PPD was 2.46- 3 CNAs on days; 4 CNAs on evenings and 2 CNAs on nights Census was 68 total; 11 on secured unit
*07/07/23- PPD was 2.88- 4 CNAs on days; 3 CNAs on evenings and 3 CNAs on nights Census was 67 total; 11 on secured unit
*07/08/23- PPD was 2.91- 5 CNAs on days; 3 CNAs on evenings and 3 CNAs on nights Census was 67 total; 11 on secured unit
*07/09/23- PPD was 2.62- 4 CNAs on days; 3 CNAs on evenings and 3 CNAs on nights Census was 67 total; 11 on secured unit
Record review of the CMS 672 dated 07/10/2023 indicated a census of 67 residents with the following:
*30 residents required assist of one or two staff for bathing.
*29 residents were dependent for bathing.
*50 residents required assist of one or two staff for dressing.
*7 residents were dependent for dressing.
*30 residents required assist of one or two staff for transfers.
*16 residents were dependent for transfers.
*26 residents required assist of one or two staff for toilet use.
*23 residents were dependent for toilet use.
*41 residents required assist of one or two staff for eating: and
*3 residents were dependent for eating.
1. Record review of Resident #38's undated face sheet indicated he was a [AGE] year-old male, admitted to the facility on [DATE]. He had diagnoses that included Alzheimer's disease (a progressive disease that destroys memory and other important mental functions) and depression (a mental health disorder characterized by persistently depressed mood or loss of interest in activities, causing significant impairment in daily life).
Record review of Resident #38's admission MDS, dated [DATE], indicated he had a BIMS score of 05, which indicated severe cognitive impairment. Resident #38 was independent in bed mobility and transfers. He required supervision assistance for walking and locomotion on unit, dressing, toileting, eating, and personal hygiene. He received antipsychotics, antidepressants, and anticoagulants 7 of 7 days of the assessment window.
Record review of an incident report dated 06/09/2023 revealed Resident #38 eloped from the secured unit through his bedroom window and was undiscovered for approximately 30-60 minutes.
Record review of staff sign in sheet for 06/09/2023 revealed LVN D was working the secured unit alone.
During an interview on 07/10/23 at 12:05PM, LVN D said she was assigned to the unit the day Resident #38 eloped. She said she was in the middle of medication pass. She said she was giving the resident next door to Resident #38 and noticed Resident #38 had walked down the hallway and entered his room. She said a CNA came to get Resident #38's weight and said he was not in his room. She said she immediately stopped medication pass and searched for Resident #38. She said she works back in the unit by herself most of the time. She said she has only had another staff member assigned with her about 5-6 times since she started working there in February of 2023. She said she does her nursing duties as well as the CNA duties when she was the only staff assigned to the unit. She said she performed incontinent care when she was back there alone. She said she tries to do as many baths as possible and will notify the next shift when she was not able to complete all the baths. She said there were typically around 9 residents back in the unit. She said it was nearly impossible to watch everyone at every moment by herself.
2. 2. Record review of the face sheet dated 07/11/23 indicated Resident #33 was [AGE] years old and admitted on [DATE] with diagnoses including dementia, generalized anxiety disorder, and major depressive disorder (a mood disorder that causes a persistent feeling of sadness and loss of interest).
Record review of the MDS dated [DATE] indicated Resident #33 was usually understood and usually understood others. The MDS indicated a BIMS score of 7 which indicated Resident #33 was severely cognitively impaired. The MDS indicated Resident #33 required extensive to total assistance from staff for activities of daily living. Resident #33 was totally dependent for personal hygiene.
During an interview on 07/12/23 at 1:50 p.m., CNA J said the aides were responsible for providing nail care on shower days. She said she checked fingernails when she could but Resident #33 was hospice and they should be providing the care. She said if hospice did not show up it was her responsibility to care for Resident #33's ADL needs. CNA J said day shift was hectic with two meals to feed, people to get up and bathes to be given. CNA J said honestly there were days not everything got done because there was not enough time with the heavy resident load each section had.
3. Record review of the face sheet dated 07/12/23 indicated Resident #37 was [AGE] years old and admitted on [DATE] with diagnoses including unsteadiness on feet, muscle wasting, and heart failure.
Record review of the MDS dated [DATE] indicated Resident #37 was understood and understood others. The MDS indicated a BIMS score of 15 which indicated Resident #37 was cognitively intact. The MDS indicated Resident #37 required supervision with personal hygiene.
Record review of a care plan revised on 05/24/23 indicated Resident #37 had an ADL self-care performance deficit. The goal was for Resident #37 to be clean and well-groomed with staff assistance for the next 90 days. There was an intervention for limited assistance with personal hygiene.
Record review of a Point of Care ADL Report for Resident #37 and dated 07/01/23 - 07/12/2023 indicated the resident last received assistance with personal hygiene on 07/10/23 and had last been bathed on 07/09/23. The documentation did not indicate any refusals for personal hygiene or bathing.
During an interview on 07/12/23 at 1:50 p.m., CNA J said the aides were responsible for removing facial hair from women. CNA J said she does her best to do all the grooming items when she gives baths but there was only so much time in a day to get everything done and at times, she felt there was not enough to complete every task assigned to her.
4. Review of Resident #44's face sheet revealed Resident #44 was an [AGE] year-old female, admitted on [DATE] with the diagnosis of diabetes mellitus type 2 (chronic condition that affects the way the body processes blood sugar (glucose), anxiety (a feeling of fear, dread, and uneasiness), and cellulitis (a common bacterial skin infection that causes redness, swelling, and pain in the infected area of the skin).
Record review of Resident #44's quarterly MDS assessment dated [DATE] indicated Resident #44 had a BIMs of 10, which indicated a moderate memory impairment. The MDS indicated Resident # 44 required extensive assistance of 1 staff member for bathing. No refusals of care were noted.
Record review of Resident #44's care plan dated 07/05/2023 indicated Resident #44 required limited assist of one to two staff members for bathing. Resident #44 had a care plan for incontinence with an intervention to keep skin clean and dry. No refusals of care were care planned.
Record review of the point of care ADL report dated 05/26/2023 to 07/12/2023 indicated, Resident #44 received a bath/shower on 06/05/2023, 06/07/2023, 06/12/2023, and 06/23/2023. No other bath/showers were documented. Resident #44's bath/shower schedule was every Monday, Wednesday, and Friday on the 2-10 shift. Resident #44 missed baths/showers on 05/26/2023, 05/29/2023, 05/31/2023, 06/02/2023, 06/09/2023, 06/14/2023, 06/16/2023, 06/19/2023, 06/21/2023,06/26/2023, 06/28/2023, 06/30/2023, 07/03/2023, 07/05/2023, 07/07/2023, and 07/10/2023.
5. Review of Resident #10's undated face sheet revealed Resident #10 was an [AGE] year-old male, admitted on [DATE] with the diagnosis of anemia (a condition that develops when your blood produces a lower-than-normal amount of healthy red blood cells), hypertension (when the pressure in your blood vessels is too high (140/90 mmHg or higher), and depression (A group of conditions associated with the elevation or lowering of a person's mood).
Record review of Resident #10's quarterly MDS assessment dated [DATE] indicated Resident #10 had a BIMs of 15, which indicated a no memory impairment. The MDS indicated Resident #10 required extensive assistance of 1 staff member for bathing. The MDS also indicated Resident #10 was occasionally incontinent of bladder and frequently incontinent of bowel. No refusals of care were noted.
Record review of Resident #10's care plan dated 07/05/2023 indicated Resident #10 required limited assist of one to two staff members for bathing. No refusals of care were care planned.
Record review of the point of care ADL report dated 05/26/2023 to 07/12/2023 indicated, Resident #10 received a bath/shower on 05/26/2023, 05/31/2023,06/05/2023, 06/07/2023, 06/12/2023, and 06/23/2023. No other bath/showers were documented. Resident #10's bath/shower schedule was every Monday, Wednesday, and Friday on the 2-10 shift. Resident #10 missed baths/showers on 05/29/2023, 06/02/2023, 06/09/2023, 06/14/2023, 06/16/2023, 06/19/2023, 06/21/2023,06/26/2023, 06/28/2023, 06/30/2023, 07/03/2023, 07/05/2023, 07/07/2023, and 07/10/2023.
During an interview on 07/10/2023 at 8:25 a.m., Resident #10 said he kept a calendar of the dates that he and his wife (Resident #44) received their bath/shower. Resident #10 said they were supposed to get a bath every Monday, Wednesday, and Friday on 2-10 shift. Resident #10 stated he received a bath at most once a week. Resident #10 said there had been weeks when he had not received a bath at all. Resident # 10 said the staff always used the excuse of being short staffed. Resident #10 said he felt dirty and as if he smelled like a cow pasture, and the smell embarrassed him.
During an interview on 07/11/2023 at 10:12 a.m., CNA P said she worked short about half of the time she worked. CNA P said there were days when the facility was short that it was not possible to feed all meals, get everyone up and down, cleaned, dried, and give all bathes. CNA P said she reported it to the nurse and the oncoming CNA when she was unable to get to a resident's bath.
During an interview on 07/11/2023 at 3:45 p.m., CNA R said she worked the 2-10 p.m. shift and worked short 2 out of 4 days per week that she worked. CNA R said there were days she had to skip giving a bath or two because there was no time to complete the bath with the other tasks, she was responsible for. CNA R said she tried to give a quick wash off to the residents she could not bath. CNA R described the wash off as wiping the residents face, arm pits and pubic area with a washcloth.
6.Review of Resident #17's undated electronic face sheet revealed that she was admitted to the facility on [DATE] with diagnoses of rheumatoid arthritis (an autoimmune and inflammatory disease, which means that your immune system attacks healthy cells in your body by mistake, causing inflammation (painful swelling) in the affected parts of the body), diabetes mellitus type 2 (group of diseases that result in too much sugar in the blood (high blood glucose), and depression (a common and serious medical illness that negatively affects how you feel, the way you think and how you act).
Record review of Resident #17's quarterly MDS assessment dated [DATE] revealed a BIMS with a score of 15, which indicated resident #17 had no cognitive deficit. The MDS also revealed, Resident #17, required extensive assistance of one staff member for eating and no limited range of motion was noted on the MDS.
Record review of Resident #17's care plan dated 05/24/2023 indicated Resident # 17 had contractures to her bilateral upper extremities which increased her risk for skin breakdown, pain, and injury. The intervention listed for the contracture care plan for Resident #17 was to assist with repositioning often, use positioning devices to maintain proper body alignment and position bilateral upper extremities on pillows for comfort.
During an observation and interview on 07/10/2023 at 08:35 a.m., Resident # 17 had no call light in reach. The touch pad call light was secured to the privacy curtain, approximately 3 feet from Resident #17's bed. A sign was observed above the bed of Resident #17 that read: Ensure (Resident #17) had call light in hand prior to leaving the room. Resident #17 said the CNAs told her they do not have time to answer her call light every hour. Resident #17 said her call light is rarely in her reach because of her contractures. Resident #17 said the call light must be placed on left side for her to reach it. Resident #17 said she does press the call light more than most when it was in reach because she had muscle spasms, and her limbs would start to hang off the bed after a while and she needed to be repositioned or she would fall.
During an interview on 07/11/2023 at 3:36 p.m., CNA R said Resident #17 used a pad call light because she was unable to move her hands well enough to use a regular call light. CNA R said Resident #17 mashed the call light more than most residents and the staff did not always have time to answer her light 5 and 6 times a shift. CNA R said she knew all call lights were to be in the residents reach at all times.
During an interview on 07/12/2023 at 3:30 p.m., the DON said she was responsible for staffing the building. The DON said she was told by the Administrator to run 4 CNAs on days, 4 on evening shift, and 3 on night shift. The DON said there had been some staffing challenges and they had in the past offered referral bonuses and ran an ad on Indeed looking for CNAs. The DON said she and other department head staff work the floor when there was no one to cover the shift. The DON said shifts had to be covered by department head staff regularly. The DON was unaware the facility assessment indicated a ppd of 3.0 for an average census of 54.
During an interview on 07/12/2023 at 3:45 p.m., the Administrator said the facility attempted to schedule no less than 5 aides on days, 5 on evenings, and 3 on night shift. The Administrator said the facility ran ads on internet employment sites and the facility was going to be short staffed, the department head nurses were assigned to work the spots.
Record review of Appropriate Nurse Staffing Levels for U.S. Nursing Homes (06/29/2020), www.ncbi.nlm.nih.gov/pmc/srticles/PMC7328494 was assessed on 07/12/2023 indicated US nursing homes are required to have sufficient nursing staff with the appropriate competencies to assure resident safety and attain or maintain the highest practicable level of physical, mental, and psychosocial well-being of each resident .nursing homes must take into account the resident acuity to assure they have adequate staff levels to meet the needs of residents .
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and record review the facility failed to store, prepare, distribute, and serve food in accordance with professional standards in 1 of 1 kitchen reviewed for food servi...
Read full inspector narrative →
Based on observation, interview, and record review the facility failed to store, prepare, distribute, and serve food in accordance with professional standards in 1 of 1 kitchen reviewed for food service safety.
The facility failed to ensure cardboard boxes were not stored on the floor.
The facility failed to ensure all food items were labeled and dated in Refrigerator #1, walk-in cooler, Freezer #1 and Freezer #2.
The facility failed ensure all food items were properly stored in Refrigerator #1.
The facility failed to safely thaw meat.
The facility failed to ensure spoiled food items were removed from the pantry and walk-in cooler.
The facility failed to ensure the chlorine test strips for the dishwasher were not expired.
The facility failed to ensure an air conditioner, food carts, and areas of the stove top were clean.
These failures could place residents at risk of foodborne illness and food contamination.
Findings include:
Record review of a blank Daily Cleaning Schedule indicated, .wash & sanitize prep tables/countertops .wash & sanitize beverage table .clean stovetop/grill .clean food carts .
Record review of a blank Weekly Cleaning Schedule indicated, .clean shelves .
During an observation on 07/10/23 at 7:04 a.m., there were 3 boxes of cranberry cocktail and 4 boxes of white foam containers stacked on the floor in the kitchen area.
During an observation on 07/10/23 at 7:06 a.m., in Freezer #1 there were 2 bottles of clear liquid with no date. One was a soda bottle and the other was a water bottle. There were 2 bags of an unknown cube shaped food item with no date or label, 1 bag of unknown breaded food item with no date or label, 1 bag of dark brown round meat with no date or label, and 1 bag of dark brown link shaped food item with no date or label.
During an observation on 07/10/23 at 7:11 a.m., in Refrigerator #1 there was 1 large bag of a yellow food item with no label, 1 package of sliced cheese open to air, and 1 bag of oven roasted turkey with no date.
During an observation on 07/10/23 at 7:14 a.m., in Freezer #2 there was 1 bag of a breaded vegetable with no date, a bag of beige colored stick shaped food item with no date or label, there was a food item wrapped in brown paper and inside a plastic bag with no label, 1 bag of one small brown breaded food item with no date or label, large blue bag with breaded unknown food item with no date or no label and a bag of round beige food item with dark brown chips with no date or label.
During an observation on 07/10/23 at 7:17 a.m., there were 5 unknown pieces of meat out of package soaking in the sink in standing water. The meat was directly in the sink. There was no running water.
During an observation on 07/10/23 at 7:19 a.m., in the pantry there was a bin of potatoes with multiple rotten potatoes and insects flying around inside the bin, on the potatoes, and all areas of the pantry. There was 1 bag of round (cookies) brown food item unlabeled.
During an observation on 07/10/23 at 7:22 a.m., in walk in cooler there was a tray with 5 foam cups with plastic lids with a red liquid inside. There was no date or label. There was a box of bell peppers with 2 peppers with soft spots covered in a black and gray fuzzy substance.
During an observation and interview on 07/10/23 at 7:25 a.m., the chlorine test strips for the dishwasher expired on 3/2023. The Dietary Manager said the man from the company just came to the facility and those were the strips he had left.
During an observation on 07/11/23 at 11:00 a.m., the window unit air conditioner, above the table where purees were being prepared, was on and blowing cool air over the table. The front cover of the air conditioner was covered in fuzzy gray particles.
During an observation on 07/11/23 on 12:00 p.m., during preparation of meal trays there was a cart with six stacks of insulated plate covers sitting at the end of the steam table. The insulated plate covers were being used to cover each plate as it was prepared. The cart had 3 different shelves. The sides of the shelves were covered in a dark substance. The substance felt greasy and sticky. All four legs of the cart had a round rubber piece and each rubber piece was covered in a greasy residue and food splashes. The metal shelf above the burners on the cookstove was dusty and greasy. The metal ledge below the knobs on the stove were dusty and greasy.
During an observation on 07/11/23 at 12:16 p.m., during meal preparation there was a cart sitting next to the steam table holding a bowl of dinner rolls being served. The bottom rail of the cart was covered in a dark greasy residue. All four legs of the cart had a round rubber piece and each rubber piece was covered in a greasy residue and food splashes.
During an interview on 07/12/23 at 10:29 a.m., [NAME] L said everybody was responsible for dating and labeling food items. She said as soon as items come out of the box they should have been dated and labeled. She said then the older foods are placed in the front and the newer foods placed in the back. She said everybody was responsible for keeping boxes off the floor. She said the cook was responsible for removing any spoiled food items. She said spoiled food items should be removed daily. She said she cleaned and washed the equipment she used daily. She said this included the cooktop. She said all staff were responsible for cleaning tables and carts.
During an interview on 07/12/23 at 10:45 a.m., the Dietary Manager said boxes were supposed to be stored off the floor. She said nothing should be stored on the floor at all. She said all staff were responsible for keeping boxes off the floor. She said boxes on the floor could get wet or get bugs in them causing the item inside to be soiled. She said all staff members were responsible for dating and labeling food items. She said staff would need to know what the foods were and how long they had been there. She said new food items should have been dated when they were received. She said undated food items could cause a resident to get sick. She said when a food item was undated you would not know how long it had been there. She said thawing meat should be thawed under running cold water and in a bowl. She said meat not being thawed properly could cause a resident to become sick. She said everyone was supposed to remove any spoiled food items. She said when a staff member saw spoiled foods they should be removed. She said spoiled food items could make residents sick. She said the cooks were responsible for cleaning the stove top. She said everyone was responsible for cleaning carts. She said the stove top should be wiped down everyday. She said the carts should be wiped down every day and deep cleaned twice a week. She said she did have a cleaning schedule. She was not sure what the staff had done with the schedule. She said she would look for the completed schedule. She said all staff were responsible for wiping down the front of the air conditioner. She said the air conditioner should be wiped down daily and as needed. She said since it was over the table it could have food splashes. She said equipment not being properly cleaned could cause something to get into the resident's food and make them sick.
During an interview on 07/12/23 at 11:14 a.m., the Dietary Manager said she could not find a daily or weekly cleaning schedule that had been completed by staff.
During an interview on 07/12/23 at 3:15 p.m., the Administrator said all kitchen staff were responsible for kitchen sanitation. He said not knowing expiration dates on food could cause health issues due to spoiled food. He said improper storage of cardboard boxes could lead to bug infestation and unsanitary storage conditions. He said unsanitary conditions can promote cross contaminations issues and lead to health concerns.
Review of a Food Storage facility policy dated 06/01/19 indicated, .To ensure that all food served by the facility is of good quality and safe for consumption, all food will be stored according to the state, federal and US Food Codes and HACCP guideline .To ensure freshness, store opened and bulk items in tightly covered containers. All containers must be labeled and dated .where possible, leave items in the original cartons placed with the date visible .Use the first-in, first-out rotation method. Date packages and place new items behind existing supplies, so that the older items are used first .Store all items at least 6 (6 inches) above the floor .to protect from overhead pips and other contamination .keep fresh meat, poultry .in the refrigerator at an internal temperature of 41 degrees F or less .Date, label and tightly seal all refrigerated foods using clean, nonabsorbent, covered containers that are approved for food storage .
Review of a General Kitchen Sanitation facility policy dated 04/26/19 indicated, .The facility recognizes that food-borne illness has the potential to harm elderly and frail residents. All Nutrition & Foodservice employees will maintain a clean, sanitary kitchen facilities in accordance with the state and US Food Codes in order to minimize the risk of infection and food borne illness .Clean and sanitize all food preparation areas, food-contact surfaces .After each use, clean and sanitize .food-contact surface of equipment .Keep food-contact surfaces of all cooking equipment free of encrusted grease deposits and other accumulated soil .Clean non-food contact surfaces of equipment at intervals as necessary to keep them free of dust, dirt, and food particles and otherwise in a clean and sanitary condition .