CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident interview, staff interview, facility document review, and clinical record review, the facility st...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident interview, staff interview, facility document review, and clinical record review, the facility staff failed to assess all residents so they could safely and independently leave the facility property specifically for the identified five of 63 residents in the survey sample, Residents #421, #164, #155, #52 and #125. Resident #421 left the facility and was involved in a hit-and-run accident with life-threatening injuries on [NAME] Pike, the four-lane divided highway in front of the facility, which placed this resident in the presence of immediate jeopardy at the time of the accident. The extent of this issue could result in serious injury, harm, impairment, or death, which constituted the determination of Immediate Jeopardy (IJ), as cited at level K. After Immediate Jeopardy was removed, the scope and severity were lowered to a level 3 isolated (G).
The findings include:
1. For Resident #421 (R421), the facility staff failed to assess the resident to safely leave the facility property independently. Resident #421 left the faciity on 9/12/24 and was hit by a car when crossing [NAME] Pike, a four-lane divided highway resulting in life threatening injuries and admission to the local hospital's Intensive Care Unit.
R421 was admitted to the facility with diagnoses that included but were not limited to history of falling, fracture of lumbar vertebra (1), traumatic spondylolisthesis of second cervical vertebra (2), alcohol use and major depressive disorder (3).
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 8/14/24, the resident scored 15 out of 15 on the BIMS (brief interview for mental status) assessment, indicating the resident was cognitively intact for making daily decisions. The assessment further documented functional limitations in range of motion to both lower extremities, normally using a manual wheelchair and able to walk 150 feet in a corridor independently. It documented R421 having an external catheter, being frequently incontinent of bowel, receiving scheduled and as needed pain medication, and having had one fall with minor injury since admission or the previous assessment.
On 10/7/24 a facility synopsis of events for R421 dated 9/13/24 was reviewed. It documented in part, .Describe incident, including location: [Name of R421] who resides in [Room number] and is a [Age and Sex of R421] with a BIMS score of 15, and diagnosis of Alcohol use unspecified with withdrawal, fall resulting in traumatic vertebral fracture, and chronic venous hypertension, Resident was out of the facility on LOA (leave of absence) and nurse supervisor notified by residents sister who confirmed that resident was involved in MVA (motor vehicle accident) and was taken to [Name of hospital] where he was admitted as a result of his injuries. Resident was involved in an MVA that was reported as a possible hit and run. Police initiated an on-going investigation. Ombudsman/APS (adult protective services)/RP (responsible party)/ MD (medical doctor)/ ED (executive director) and DON (director of nursing) notified . A Leave of Absence form dated 9/12/24 for R421 was included in the file which documented the time left as 1:50 p.m. with anticipated return time of 11:00 p.m. The LOA form documented the resident leaving independently. The final investigation summary dated 9/13/24 documented in part, .Nature of Incident: Unusual Occurrence/Collision with MVA while on LOA/Possible hit and run. Staff member: None. Including location: [Name of R421] who resides in [Room number] and is a [Age and Sex of R421] with a BIMS score of 15, and diagnosis of Alcohol use unspecified with withdrawal, fall resulting in traumatic vertebral fracture, and chronic venous hypertension. [Name of R421] signed himself out of the facility on LOA per his normal daily routine in the am, and failed to return to the facility at his signed expected time of return, the nurse supervisor- initiated call inquiry to nearby hospitals and was informed by [Name of hospital] nursing staff that resident was there but were unable to provide facility staff with any information, and advised supervisor to contact resident representative for further information. The facility nurse supervisor placed a call to resident representative (sister), no answer received, a message was left to return call to the facility. Resident sister returned call to the facility and supervisor confirmed admission to [Name of hospital] due to being involved in an MVA that resulted in major injuries and stated that the incident was a possible hit and run. On the following day [Name of R421]'s sister contacted social services to inform of resident in ICU (intensive care unit) pending surgical intervention, and that she would be coming to the facility to pick up residents' personal items due to discharging to the hospital. [Name of county police department] initiated and concluded post confirmation of signed LOA and the unusual occurrence transpired while on LOA .
The physician orders for R421 documented in part,
- May go out on pass with or without meds. Order Date: 5/7/24. End date: 9/13/24.
- Aspen collar (4) on at all times. every shift Document refusal to wear. Order Date: 5/7/24. End date: 9/13/24.
- Wear t shirt underneath the back brace. Monitor skin under the brace for redness or skin irritation. Do not sleep in TLSO (thoracic lumbar sacral orthosis) back brace (5) but keep Aspen collar on every shift. Order Date: 5/7/24. End date: 9/13/24.
A review of the PT (physical therapy) evaluation dated 6/17/24 and the OT (occupational therapy) evaluation dated 5/8/24, progress report dated 5/21/24, and OT Discharge summary dated [DATE] failed to reveal evidence that the resident was assessed for safety outside the building.
Review of the completed Leave of Absence forms for R421 documented the resident leaving the facility independently on 96 occasions between 5/7/24 and 9/12/24.
Review of the progress notes for R421 documented the resident returning from leave of absence intoxicated on 12 dates. Further review of the progress notes documented the police responding to staff calls for R421 being intoxicated at the facility on four dates and the police returning R421 to the facility from the community intoxicated once.
A progress note dated 9/12/24 documented, Late Entry. Note Text: Resident alert and oriented to person, place, time and situation. He signed himself out on LOA from facility at 1:50 pm in an alert and stable condition with expected returned time of 11:00 pm on the same day. Around 9:10 pm, writer was informed that resident was involved in a motor vehicle accident while on LOA and was taken to the hospital via ambulance. [Name of hospital] ER called but writer was not able to get any information regarding resident's current status. ER nurse advised writer to call again later. Call placed to resident's sister, [Name of sister] and was updated about incident. On a follow up call to sister, she confirmed that upon calling the hospital, it was confirmed that resident was hit by a car while outside facility and is now in ICU. Telehealth was called and updated. Nursing staff will continue to follow up.
Further review of the progress notes documented a follow up note dated 9/18/24 which documented, Note Text: Writer followed up on resident at the hospital, per the nurse report resident is still at the ICU intubated and waiting for spine effusion tonight. MD updated.
The comprehensive care plan for R421 documented in part, [Name of R421] has history of falling with injury. At risk for further falling. had a fall with injury Abrasion to right shoulder. Date Initiated: 05/01/2024. Revision on: 08/05/2024.
The emergency provider notes from [Name of hospital] for R421 dated 9/13/24 4:49 a.m. documented in part, . [Name, age and sex of R421] who presents with unknown past medical history presenting with pedestrian strike. EMS (emergency medical services) reports he was witnessed being hit by a jeep wrangler going 35 to 45 mph on the turnpike prompting EMS visit to ED. EMS states patient was in a c-collar (cervical collar) prior to arrival . Critical diagnosis: 1. Contusion of head, subsequent encounter. 2. Trauma shock, initial encounter .
The history and physical for R421 from [Name of hospital] dated 9/12/24 at 10:47 p.m. documented in part, .Patient was a modified trauma activation status post pedestrian struck. In the trauma bay, patient was awake and following commands but confused. He was initially normotensive. He was noted to have facial lacerations, forehead hematoma, bilateral hip bruising and what appeared to be chronic bilateral toe wounds. [NAME] report, patient was noted to have a cervical spine prior to the arrival presumably from recent injury. Patient then became combative and therefore received 4mg of IM (intramuscular) Versed. Soon after, patient became hypotensive and lethargic. At this point, patient was upgraded to a full trauma activation .Given patient's ongoing hypotension, patient received units of whole blood .GI (gastrointestinal): Grade IV liver injury with active subcapsular hematoma and hemoperitoneum. Grade 2 splenic laceration w/subcapsular hematoma, anterior pancreas hematoma .Pt in critical condition .
The discharge summary for R421 from [Name of hospital] dated 10/10/24 documented in part, .Hospital Course: Patient went to the OR for ex-lap (exploratory laparoscopy) and had ileum resection and packing. He was eventually closed and had return of bowel function. NSGY (neurosurgery) was consulted, and patient did not need aspen for dens fx and went for posterior decompression and fusion. He required a TLSO brace when OOB (out of bed). Patient was extubated but required a corpak 2/2 (secondary to) dysphagia. He was able to work with SLP (speech language pathologist) and his diet was advanced to a regular diet. His abdominal staples were removed and there was some superficial wound dehiscence that required iodofoam packing and dressing changes. He was restarted on his home medications. PT/OT worked with patient and recommended SNF (skilled nursing facility). At the time of discharge the patient was afebrile and his vital signs were within normal limits .
On 10/2/24 at 3:49 p.m., ASM (administrative staff member) #5, the regional director of operations, was interviewed. She stated her understanding is that as long as residents have a BIMS score that is high enough, and the residents have been physically assessed as safe, the residents are allowed to sign themselves out on a leave of absence from the facility.
On 10/2/24 at 4:52 p.m., an interview was conducted with ASM #1, the executive director and ASM #3, the regional director of clinical operations. ASM #1 stated that the resident needs an order to go out on LOA, needs to be assessed that they can go out, and typically by nursing, a cognition assessment. He stated that a functionally mobility is done by the IDT (interdisciplinary team). ASM #1 stated therapy is involved in the screening in Section GG on the MDS, when the admission and discharge from therapy assessment are completed. He stated that the MDS staff codes the functional abilities, goals and mobility devices used. ASM #3, the regional director of clinical operations, stated that if a resident wants to go out, the nurse initiates the Leave of Absence Form, and then the resident brings it to the executive director or director of nursing to sign. She stated that any nurse, executive director or director of nursing, could sign off this form. ASM #3 stated that the resident then takes the form to the front desk and gives it to the receptionist, who then logs it into the daily log. She stated that if the resident does not return at the anticipated time, the staff will call the resident or responsible party, then the staff calls 911. ASM #3 stated it is the nurse who monitors when the resident returns.
On 10/2/24 at 5:05 p.m., an interview was conducted with ASM #1, the executive director, ASM #2, the director of nursing, and ASM #5, the regional director of operations. ASM #2 stated the facility uses the BIMS is used to assess a resident's ability to safely leave the facility. ASM #5 stated the BIMS assesses a resident for their ability to process new information and ability to recall. She stated the BIMS does not assess a resident's ability to determine danger from safety.
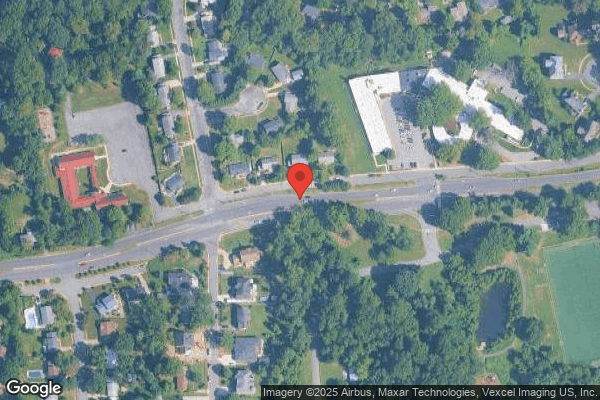
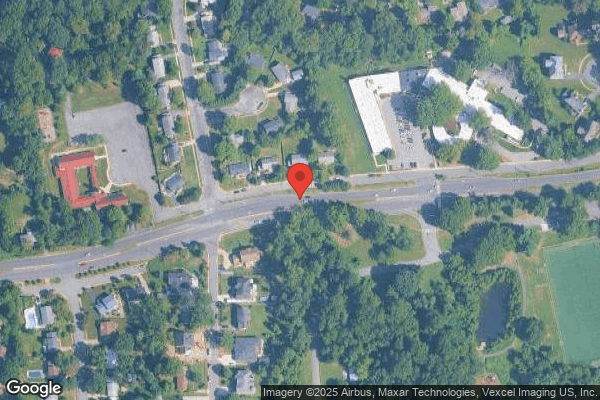
On 10/7/24 at 12:31 p.m., an interview was conducted with ASM #2, the director of nursing. ASM #2 stated that the facility staff had received a report that R421 had been involved in a hit and run and the staff had contacted the sister and the hospital who confirmed the resident was involved. She stated that R421 had signed out on LOA earlier that day and when he did not come back at the expected time, they had started calling around to the local hospitals checking and calling the family. She stated that she was not sure of the exact location of the hit and run other than it was the cross section outside of the facility on [NAME] Pike. She stated that the police had responded and spoken to the executive director and as far as she knew there were no witnesses to the accident. She stated that R421 would catch the bus sometimes when he went out on LOA and used a manual wheelchair.
On 10/7/24 at 12:43 p.m., an interview was conducted with ASM #1, the executive director. ASM #1 stated that the police had come to the facility to ask him if there were any witnesses to the accident involving R421. He stated that there was a former resident of the facility who witnessed the accident, and he was unsure if the police officer questioned them or not. He stated that the hit and run happened on [NAME] Pike in the evening after he had left for the day and staff had called him at home. He stated that R421 would sign out LOA and catch the bus to go shopping or visit family using the manual wheelchair or walking behind it using it as a walker. He stated that no staff witnessed the accident that they knew of. ASM #1 stated that they had previously spoken to the police, VDOT and the county regarding the crosswalk. He stated that VDOT told them that the crosswalk was safe to be used the way it was designed, and the police told them that the residents were not violating any laws so they could not stop them from using it. He stated that the residents had to be in that corner to catch bus and the county told them that the facility could pursue getting a light put in, so they had contacted the North Virginia Emergency Response System however, they said that they did not see a need. He stated that if the resident was in an electric wheelchair or they could walk, there was no way to prohibit them if they were alert and oriented, were care planned, made their own decisions, and they signed themselves out. He stated that if they were to go out and be in a hit and run, they were not able to do anything. He stated that it was difficult due to having authorities tell them that residents were allowed to make bad decisions and as citizens they had rights that could not be taken away.
On 10/7/24 at 2:43 p.m., an interview was conducted with RN (registered nurse) #3, MDS coordinator. RN #3 stated she completes functional abilities and goals assessments based on documentation the CNAs (certified nursing assistants) chart in the clinical record. RN #3 stated the assessments demonstrate what the residents can do in terms of their activities of daily living. RN #3 stated she did not think the assessments determined residents' safety abilities. RN #3 stated maybe the BIMS assessments determined residents' safety abilities but that would be hard to determine because she is not with the residents and does not know what they do when they leave the property.
On 10/7/24 at 2:59 p.m., an interview was conducted with ASM #7, physician. ASM #7 stated that the leave of absence orders for the residents were intended for residents to go out with families for extended periods and then return to the facility. He stated that there were residents at the facility for long term care who had family that wanted to take them home for a long weekend or overnight and the order was intended for them to be able to do that and take their medications with them for the leave of absence.
On 10/7/24 at 3:11 p.m., an interview was conducted with OSM (other staff member) #6, physical therapist. She stated she has never assessed a resident for his or her ability to maneuver safely outside of the facility on a daily basis. She stated she has told residents that attempting to cross the divided highway in front of the facility is not safe, and that she would not attempt it herself. She stated physical therapy assessments are designed to treat a resident with the goal of becoming as functional as possible in the facility, not out outside of it on a day-to-day basis. OSM #6 stated that all assessments and treatments completed for R421 were done in the facility gym or hallways.
On 10/8/24 at 1:51 p.m., an interview was conducted with LPN (licensed practical nurse) #7. LPN #7 stated the executive director was initially signing for residents to go out on LOA but then the nurses were allowed to sign residents out on LOA. LPN #7 stated the nurses write a note that documents the time residents leave the facility then write a note when the residents return. LPN #7 stated there were no assessments completed to determine if residents are physically or mentally safe to leave the property.
On 10/8/24 at 6:05 p.m., an interview was conducted with RN #1. RN #1 stated that another resident (identified as Resident #96) informed him around 9:00 p.m. on 9/12/24 that they thought R421 had been hit by a car outside of the facility. RN #1 stated that he had started calling around to the hospitals in the area and [Name of hospital] had confirmed that R421 was there and had been in an accident but could not give them any other information, so they had called R421's sister. He stated that R421's sister had contacted the hospital and called them back confirming that the resident had been in a hit in run on [NAME] Pike in front of the facility. He stated that he was unsure how the other resident knew that R421 had been hit by the car and he had started calling around because of the report from the other resident. He stated that Resident #96 did not say that R421 had been hit in front of the facility, that he witnessed the accident or how he knew that R421 had been hit by the car. RN #1 stated that he did not go outside or see the accident. He stated that he called and reported the incident to the director of nursing that night.
On 10/9/24 at 7:49 a.m., an interview was conducted with RN #6. RN #6 stated that she was inside the facility and heard the sirens and saw the ambulance across the street on 9/12/24 as it was leaving the scene. She stated that several residents were coming inside the entrance and told her that R421 had been hit by a car crossing the street and was being taken to the hospital. She stated that she had checked the LOA form to see that the resident was actually out of the facility and then she and RN #1 had called the sister who confirmed that the resident was involved in a hit and run while crossing the street from the park bus stop on the opposite side of [NAME] Parkway. She stated that it was around 8:30 p.m. when the residents reported this, and it was dark outside. She stated that they expected the police to come to the facility, but no one ever did. She stated that they had reported the incident to the director of nursing and the physician. She stated that she did not recall the specific residents that reported the incident to her but there were a lot of them all rushing inside the lobby.
On 10/9/24 at 8:25 a.m., an interview was conducted with Resident #96 (R96) in their room. R96 stated that they were sitting outside of the facility at the entrance the evening of 9/12/24 when they witnessed R421 get off the bus on the furthest side of [NAME] Pike and cross the road in the cross walk. R96 stated that R421 was almost across [NAME] Pike and was in the right lane closest to the facility when a car hit him, and he saw the car spin around and then keep going. He stated that he had reported it to multiple nurses but did not know their names and the next day the former social worker came in to speak with him and said that the police may come talk to him, but no one had. Review of the most recent MDS assessment for R96, a quarterly assessment with an ARD of 7/11/24 documented the resident being cognitively intact for making daily decisions.
On 10/9/24 at 8:36 a.m., an interview was conducted with OSM (other staff member) #13, occupational therapist. OSM #13 stated the only time she completes an evaluation to determine if a resident can safely go outside of the building and into the community is if a resident is being discharged home. OSM #13 stated she has not completed any evaluation to determine if R421 can safely and independently go outside and off the facility property.
On 10/9/24 at 10:53 a.m., an interview was conducted with OSM #21, detective. OSM #21 stated that the case involving R421 was still active and not completed at this time. He stated that they could only confirm that R421 was involved in the incident and the other person had left the scene.
Additional interviews with staff identified on the as-worked schedule for 9/12/24 evening shift failed to evidence firsthand witnesses of the hit and run accident involving R421.
Reference:
(1) fracture lumbar vertebra
The spine is made up of 33 bones. The individual bones of the spine are called vertebrae. The spine is divided into three sections: Cervical (upper), Thoracic (midback), Lumbar (lower back). Most spinal fractures occur in the thoracic and lumbar spine, or at the connection of the two (called the thoracolumbar junction). This information was obtained from the website: https://orthoinfo.aaos.org/en/diseases--conditions/fractures-of-the-thoracic-and-lumbar-spine/
(2) traumatic spondylolisthesis of second cervical vertebra
Spondylolisthesis is a condition in which a bone (vertebra) in the spine moves forward out of the proper position onto the bone below it. This information was obtained from the website: https://medlineplus.gov/ency/article/001260.htm
(3) major depressive disorder
Major depression is a mood disorder. It occurs when feelings of sadness, loss, anger, or frustration get in the way of your life over a long period of time. It also changes how your body works. This information was obtained from the website: https://medlineplus.gov/ency/article/000945.htm.
(4) Aspen Collar
A cervical collar provides support and restricts movement in your neck while bones and tissues heal in the area where you had surgery. The Aspen collar is plastic with front and back panels lined with removable padding. It provides comfort and keeps sweat away from your skin. Openings on the front and the back panel of the collar allow your skin to breathe. This information was obtained from the website: https://www.healthsystem.virginia.edu/docs/per/at-home-with-aspen-cervical-collar/handout_view_patient/@@getDocument
(5) TLSO brace
If you have back pain, your physician or physical therapist may prescribe a brace to help control motion of your spine. A special back brace called a thoracic lumbar sacral orthosis (TLSO) may be prescribed for this. A TLSO is a brace that limits movement in your spine from the thoracic area (mid back) to your sacrum (low back). It does allow your neck to move freely. If you have a problem with your back that requires it to be kept in a neutral position while limiting excessive spinal motion, then a TLSO may be an option for you. Knowing what it is and how it is used can help you make an informed decision about using a TLSO. This information was obtained from the website: https://www.verywellhealth.com/thoracic-lumbar-sacral-orthosis-5203250
2. For Resident #164 (R164), the facility staff failed to assess the resident the resident to safely leave the facility property independently. Resident #164 was observed getting off public transportation in a motorized wheelchair onto the pavement linking [NAME] Pike and the [NAME] Pike service road, maneuvering around a van waiting to turn onto [NAME] Pike, meeting another resident in the parking lot and then was observed sitting in the wheelchair in the road on [NAME] Pike Service Road.
R164 was admitted to the facility with diagnoses that included but were not limited to hemiplegia and hemiparesis (1), bipolar disorder (2) and supraventricular tachycardia (3).
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 8/24/24, the resident scored 15 out of 15 on the BIMS (brief interview for mental status) assessment, indicating the resident was cognitively intact for making daily decisions. The assessment further documented functional limitations in range of motion to both lower extremities, normally using a motorized wheelchair and being occasionally incontinent of urine and frequently incontinent of bowel. It further documented R164 receiving as needed pain medication, taking antipsychotic, antidepressant and opioid medications. The assessment documented no falls since the previous assessment.
On 10/2/24 at 3:22 p.m., Resident #164 was observed getting off public transportation in a motorized wheelchair onto the pavement linking [NAME] Pike and the service road, maneuvering around a van waiting to turn onto [NAME] Pike, into the facility parking lot. At 3:35 p.m., R164 was observed sitting in the right lane of [NAME] Pike Service Road on the west side of the facility with another resident.
The physician orders for R164 documented an order dated 11/15/2023 May go out on pass with or without meds.
A review of the PT (physical therapy) Discharge summary dated [DATE] and the OT (occupational therapy) Discharge summary dated [DATE] failed to reveal evidence that the resident was assessed for safety outside the building.
Review of the completed Leave of Absence forms for R164 documented the resident leaving the facility independently on 22 occasions between 9/1/24 and 10/2/24.
The comprehensive care plan for R164 documented in part, Fall: [Name of R164] is at risk for falls Gait/balance problems, Hemiplegia/Hemiparesis. Date Initiated: 02/28/2024.
On 10/2/24 at 3:49 p.m., ASM (administrative staff member) #5, the regional director of operations, was interviewed. She stated her understanding is that as long as residents have a BIMS (brief interview for mental status) score that is high enough, and the residents have been physically assessed as safe, the residents are allowed to sign themselves out on a leave of absence from the facility.
On 10/2/24 at 4:52 p.m., an interview was conducted with ASM #1, the executive director. ASM #1 stated the resident needs an order to go out on LOA, the resident has been assessed that they can go out, and typically by nursing, a cognition assessment. He stated that a functionally mobility is done by the IDT (interdisciplinary team). ASM #1 stated therapy is involved in the screening in Section GG on the MDS, when the admission and discharge from therapy assessment are completed. He stated that the MDS codes the functional abilities, goals and mobility devices used. ASM #3, the regional director of clinical operations, stated, if a resident wants to go out, the nurse initiates the Leave of Absence Form, the resident brings it to the executive director or director of nursing, to sign. She stated that any nurse, executive director or director of nursing, can sign off this form. ASM #3 stated that the resident then takes the form to the front desk and hands it to the receptionist, who then logs it into the daily log. She stated that if the resident does not return at the anticipate time, the staff will call the resident or responsible party, then the staff calls 911. ASM #3 stated it is the nurse who monitors when the resident returns.
On 10/2/24 at 5:05 p.m., ASM #1, the executive director, ASM #2, the director of nursing, and ASM #5 were interviewed. ASM #2 stated the facility uses the BIMS is used to assess a resident's ability to safely leave the facility. ASM #5 stated the BIMS assesses a resident for their ability to process new information and ability to recall. She stated the BIMS does not assess a resident's ability to determine danger from safety.
On 10/7/24 at 2:43 p.m., an interview was conducted with RN (registered nurse) #3, MDS coordinator). RN #3 stated she completes functional abilities and goals assessments based on documentation the CNAs (certified nursing assistants) chart in the clinical record. RN #3 stated the assessments demonstrate what the residents can do in terms of their activities of daily living. RN #3 stated she did not think the assessments determined residents' safety abilities. RN #3 stated maybe the BIMS assessments determined residents' safety abilities but that would be hard to determine because she is not with the residents and does not know what they do when they leave the property.
On 10/7/24 at 2:51 p.m., an interview was conducted with OSM (other staff member) #5, PT (physical therapist). OSM #5 stated that PT staff did not do a formal safety assessment on residents for leaving the facility independently in the community. He stated that they barely took residents outside and did some wheelchair training with residents but did not leave the property. He stated that they had not been doing any formal safety assessments since he had been working at the facility in July of 2024. He stated that the assessments that he completed on Resident #164 were completed in the hallway of the facility or the gym.
On 10/7/24 at 2:59 p.m., an interview was conducted with ASM #7, physician. ASM #7 stated that the leave of absence orders for the residents were intended for residents to go out with families for extended periods and then return to the facility. He stated that there were residents at the facility for long term care who had family that wanted to take them home for a long weekend or overnight and the order was intended for them to be able to do that and take their medications with them for the leave of absence.
On 10/8/24 at 1:51 p.m., an interview was conducted with LPN (licensed practical nurse) #7. LPN #7 stated the executive director was initially signing for residents to go out on LOA but then the nurses were allowed to sign residents out on LOA. LPN #7 stated the nurses write a note that documents the time residents leave the facility then write a note when the residents return. LPN #7 stated there were no assessments completed to determine if residents are physically or mentally safe to leave the property.
On 10/9/24 at 7:40 a.m., an interview was conducted with CNA (certified nursing assistant) #1. CNA #1 stated that he was coming in to work the evening shift on 10/2/24 when he saw the residents outside and came out to speak with them. He stated that he told them to move from the right end of the road because he thought it was not safe because they were in the street too much. He stated that there may be a serious accident, outcome, or someone could get harmed.
On 10/9/24 at 8:36 a.m., an interview was conducted with OSM #13, occupational therapist. OSM #13 stated the only time she completes an evaluation to determine if a resident can safely go outside of the building and into the community is if a resident is being discharged home. OSM #13 stated she has not completed any evaluation to determine if R164 can safely and independently go outside and off the facility property.
On 10/2/24 at 5:50 p.m., ASM #1, the executive director, ASM #2, the director of nursing, ASM #4, the regional director of clinical operations, and ASM #5, the regional director of operations were informed of these concerns, and of immediate jeopardy.
No further information was provided prior to exit.
Reference:
(1) hemiplegia and hemiparesis
Also called: Hemiplegia,
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, and facility document review, the facility staff failed to promote dignity for two of 63 residents in the survey sample, Residents #142 and #162.
The findings in...
Read full inspector narrative →
Based on observation, staff interview, and facility document review, the facility staff failed to promote dignity for two of 63 residents in the survey sample, Residents #142 and #162.
The findings include:
1. For Resident #142 (R142), the facility staff failed to serve lunch in a dignified manner. R142's roommate was served lunch on 10/2/24 at 1:20 p.m. and R142 was not served lunch until ten minutes later.
On 10/2/24 at 1:20 p.m., R142 and the resident's roommate was observed in their bedroom. At this time, R142's roommate was served lunch. R142 was not served and fed by a CNA (certified nursing assistant) until 1:30 p.m. (ten minutes later).
On 10/3/24 at 3:21 p.m., an interview was conducted with CNA #2. CNA #2 stated she does not serve and feed residents who require assistance until residents who eat independently are served. CNA #2 stated that if one resident in a room is eating and his roommate requires assistance, she will ask other CNAs to finish passing meal trays so she can feed the resident who requires assistance. CNA #2 stated a resident who requires assistance should be served and fed within two to three minutes of his roommate being served. CNA #2 stated that if she required assistance with eating and she was sitting in a room with a resident who was eating, she would feel bad because the other person is eating, and she is not. CNA #2 stated ten minutes is too long of a wait for a resident to be served and fed while his roommate is eating.
On 10/4/24 at 11:41 a.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
The facility policy titled, Resident Rights documented, The purpose of this policy is to guide employees in the general principles of dignity and respect of caring for residents .
No further information was presented prior to exit.
2. For Resident #162 (R162), the facility staff failed to maintain the resident's shirt in a dignified manner.
On 10/1/24 at 10:06 a.m., R162 was observed in a hallway wearing a shirt with the resident's first name and room number written on the front of the shirt.
On 10/3/24 at 3:21 p.m., an interview was conducted with CNA (certified nursing assistant) #2. CNA #2 stated residents' names and room numbers are written on resident's shirts for laundry purposes, but the names and room numbers are supposed to be written on the inside of the back collar of the shirt. CNA #2 stated that if she was wearing a shirt with her name and room number written on the front of the shirt, she would feel bad because everybody would know her personal information. CNA #2 stated that is a dignity issue.
On 10/4/24 at 11:41 a.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
No further information was presented prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
Based on observation, resident interview, staff interview and facility document review it was determined the facility staff failed to assess a resident for self-administration of over-the-counter eye ...
Read full inspector narrative →
Based on observation, resident interview, staff interview and facility document review it was determined the facility staff failed to assess a resident for self-administration of over-the-counter eye drops that were on the over the bed table, for one of 63 residents in the survey sample, Resident #65.
The findings include:
For Resident #65 (R65), over the counter Opcon A eye drops were found on her over the bed table, there was no evidence of an assessment for self-administration of medications.
Observation was made on 9/30/24 at approximately 6:35 p.m. of Opcon A eye drops, an over-the-counter medication, was observed on the over the bed table. The bottle of eye drops was noted again on the bedside table on 10/1/24 at 3:50 p.m.
An interview was conducted with R65 on 9/30/24 at 6:35 p.m. R65 stated she uses these drops to help her eyes.
Review of the physician orders failed to evidence a physician order for the above stated drops.
Further review of the clinical record failed to evidence an assessment for the self-administration of medications.
An interview was conducted with LPN (licensed practical nurse) #6 on 10/3/24 at 11:31a.m. LPN #6 stated the resident cannot keep over the counter drops at their bedside and stated sometimes residents overuse them and it's not safe for them to have medications with them. LPN #6 further stated that sometimes they have them and we don't have an order for them (eye drops).
The facility policy, Resident Self-Administration of Medications documented in part, 1. Determine if the resident desires to self-administer their own medication; a. Resident may not self-administer medication until the assessment is completed by the IDT team and determined to be safe to do so. c. Physician/ Provider order is required for residents to self-administer medication. 2. Resident may self-administer some or all of their medications; a. If only some of the medications will be self-administered clearly indicate which drug(s) including time and route, by physician order.
ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing, and ASM #5, regional director of operations, were made aware of the above concern on 10/8/24 at 6:15 p.m.
No further information was provided prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on staff interview, facility document review, and clinical record review, the facility staff failed to report an injury of unknown origin within the required time frame for one of 63 residents i...
Read full inspector narrative →
Based on staff interview, facility document review, and clinical record review, the facility staff failed to report an injury of unknown origin within the required time frame for one of 63 residents in the survey sample, Resident #68.
The findings include:
For Resident #68 (R68), the facility staff failed to report a left-hand fracture of unknown origin to the state agency within two hours.
A review of R68's clinical record revealed a nurse's note dated 3/14/24 that documented the resident presented with left hand swelling. Tylenol was administered with an effective effect and an x-ray was ordered. An x-ray result dated 3/16/24 documented, Undisplaced fracture mid portion left fourth metacarpal (a bone in the hand). Further review of R68's clinical record failed to reveal a known cause of the fracture.
A facility synopsis of events submitted to the state agency documented, Report date: 3/18/24. Incident date: 3/14. Incident type: Injury of unknown origin. The facility received X ray results stating undisplaced fourth metacarpal of the left hand. The resident is not fearful and exhibits no pain or limited range of motion. Resident continues with routines [sic] activities and was evaluated by Nursing staff and physician extender. Resident received pain evaluation, skin assessment and there were no noted findings.
On 10/4/24 at 9:10 a.m., an interview was conducted with ASM (administrative staff member) #2 (the director of nursing). ASM #2 stated a fracture of unknown origin should be reported to the state agency as soon as possible but within two hours to make the agency aware.
On 10/4/24 at 11:41 a.m., ASM #1 (the executive director) and ASM #2 were made aware of the above concern.
The facility policy titled, Abuse, Neglect and Exploitation Policy-Virginia documented, Injury of Unknown Origin: an injury should be classified as an injury of unknown origin when both of the following conditions are met: a) the source of the injury was not observed by any person. b) the source of injury could not be explained by the resident AND the injury is suspicious because of: a. the extent of the injury; or b. the location of the injury; or c. the number of injuries observed at one particular point in time; or d. the incidence of injuries over time .V. Reporting of Incidents and Facility Response. 1. All alleged violations involving abuse, neglect, exploitation or mistreatment, including injuries of unknown source and misappropriation of resident property, are reported immediately, but not later than 2 hours after the allegation is made, if the events that cause the allegation involve abuse or result in serious bodily injury.
No further information was presented prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #4 (R4), the facility staff failed to provide evidence of written notification of the resident's discharge to th...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #4 (R4), the facility staff failed to provide evidence of written notification of the resident's discharge to the hospital on 6/2/24 and 6/24/24.
A review of R4's clinical record revealed she was transferred to the hospital on 6/2/24 for a dislodged nephrostomy tube, and on 6/24/24 for an acute change in mental status. Further review revealed no evidence that the resident/RR (resident representative) and ombudsman were informed in writing of the reason for the discharge.
On 10/3/24 at 11:31 a.m., LPN (licensed practical nurse) #6 was interviewed. She stated if a resident is sent to the hospital, she calls the family to let them know about the transfer. If the RR is in the building, they are given a written notification about the discharge. She stated this should be included in the discharging nurse's progress notes. She stated nurses do not provide a written discharge notice to the ombudsman.
On 10/3/24 at 2:32 p.m., OSM (other staff member) #2, director of social services, was interviewed. She stated the facility sends the ombudsman a monthly list at the end of each month to notify the ombudsman of all the discharges. She stated she had just started in this position, and was not able to locate evidence that the ombudsman had been notified of R4's discharges in June 2024.
On 10/4/24 at 12:40 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing, and ASM #5, the regional director of operations were informed of these concerns.
No further information was provided prior to exit.
Based on staff interview, facility document review and clinical record review, it was determined the facility staff failed to provide written notification to the resident and/or responsible party and failed to notify the ombudsman upon transfer for two of 63 residents in the survey sample, Residents #1 and #4.
The findings include:
1. For Resident #1 (R1), the facility staff failed to evidence a written notice was provided to the resident and/or responsible party and failed to notify the ombudsman upon transfer to the hospital on 7/4/25.
The nurse's note dated, 7/4/24 at 3:31 p.m. documented, Critical Lab (laboratory) value: Creatinine 10.78, BUN (blood urea nitrogen) 121. Contributing DX (diagnosis) CKD (chronic kidney disease) Stage 4. Currently on Bumetanide (used to treat edema/fluid retention) (1) 6 mg daily. VS (vital signs) 128/70 (blood pressure), 97.8 (temperature), 72 (pulse), 17 (respirations)[NAME], sat (oxygen saturation) 98% RA (room air). NP (nurse practitioner) review results with resident via video conference with nurse at bedside. Order obtained to transfer resident to ER (emergency room) for further evaluation and treatment. (Name of ambulance service) notify of transfer and will be in facility within an hour. Daughter made aware.
The nurse's note dated, 7/4/24 at 6:09 p.m. documented, Resident was picked up at about 5 pm with (name of ambulance company).
Review of the clinical record failed to evidence the facility provided the resident and/or responsible party with a written notification of the reason for the transfer.
An interview was conducted with LPN (licensed practical nurse) #6 on 10/3/24 at 11:31 a.m. LPN #6 stated if the family is here at the time of transfer, then they give them a notice, if they are not here, they do not give the resident and/or the responsible party anything in writing when they are transferred to the hospital.
A request was made for the evidence that the ombudsman was notified of the transfer. None was provided.
An interview was conducted with OSM (other staff member) #2, the director of social services, on 10/3/24 at 2:32 p.m. OSM #2 stated the process for notifying the ombudsman of resident transfers is to send a list at the end of the month of all discharges, schedule, unscheduled and against medical advice. OSM #2 stated she could not find any evidence that the ombudsman had been notified for the year 2024. OSM #2 had just started working at the facility on 9/27/24.
The facility policy, Admission, Discharge and Transfers, documented in part, a. Notice before transfer. I. Before a facility transfers or discharges a resident, the facility must:1. Notify the resident and the resident's representative(s) of the transfer or discharge and the reasons for the move in writing and in a language and manner they understand.
ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing, and ASM #5, the regional director of operations, were made aware of the above concerns on 10/8/24 at 6:16 p.m.
No further information was provided prior to exit.
(1) This information was obtained from the following website: https://medlineplus.gov/druginfo/meds/a684051.html.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #4 (R4), the facility staff failed to provide evidence of providing a bed hold notification for her 6/2/24 and 6...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #4 (R4), the facility staff failed to provide evidence of providing a bed hold notification for her 6/2/24 and 6/24/24 hospital discharges.
A review of R4's clinical record revealed she was transferred to the hospital on 6/2/24 for a dislodged nephrostomy tube, and on 6/24/24 for an acute change in mental status. Further review revealed no evidence that the resident received a bed hold notice for these discharges.
On 10/3/24 at 11:31 a.m., LPN (licensed practical nurse) #6 was interviewed. She stated if a resident is sent to the hospital, the nurse is required to give the resident or RR a copy of the bed hold policy. She stated the nurse who discharges the resident should write a progress note that she has done this, and should make a copy for the clinical record.
On 10/4/24 at 12:40 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing, and ASM #5, the regional director of operations were informed of these concerns.
No further information was provided prior to exit.
Based on staff interview, facility document review and clinical record review, it was determined the facility staff failed to provide a bed hold notice at the time of transfer for two of 63 residents in the survey sample, Residents #1 and #4.
The findings include:
1. For Resident #1, the facility staff failed to evidence a bed hold notice was provided to the resident and/or responsible party at the time of transfer to the hospital on 7/4/24.
The nurse's note dated, 7/4/24 at 3:31 p.m. documented, Critical Lab (laboratory) value: Creatinine 10.78, BUN (blood urea nitrogen) 121. Contributing DX (diagnosis) CKD (chronic kidney disease) Stage 4. Currently on Bumetanide (used to treat edema/fluid retention) (1) 6 mg daily. VS (vital signs) 128/70 (blood pressure), 97.8 (temperature), 72 (pulse), 17 (respirations)[NAME], sat (oxygen saturation) 98% RA (room air). NP (nurse practitioner) review results with resident via video conference with nurse at bedside. Order obtained to transfer resident to ER (emergency room) for further evaluation and treatment. (Name of ambulance service) notify of transfer and will be in facility within an hour. Daughter made aware.
The nurse's note dated, 7/4/24 at 6:09 p.m. documented, Resident was picked up at about 5 pm with (name of ambulance company).
Review of the clinical record failed to evidence a bed hold notice was provided to the resident upon transfer on 7/4/24.
An interview was conducted with LPN (licensed practical nurse) #6 on 10/3/24 at 11:31 a.m. LPN #6 stated they have to give the resident the bed hold policy, the nurse should document in the progress notes that it was given to the resident and keep a copy of it for the record.
The facility policy, Bed Hold Policy documented in part, Procedure: 1. In the event a resident returns to the hospital or goes on a leave, the following process will be followed by the facility: a. The nurse or designee will present the Acute Transfer Letter at time of transfer with a copy going with the resident and a copy going to the Business Office Manager. Designee will scan to the ombudsman. b. If applicable according to state law if the bed hold authorization form cannot be signed prior to the resident leaving and needs to be mailed, it must be mailed certified return receipt requested by the Business Office Manager or designee. c. The Admissions Director or designee will notify the resident and/or responsible party of the days available under their Medicaid benefits or the private pay cost associated with holding the bed will be explained, within 24 hours of the patient leaving the facility, or the following business day if the patient leaves on the weekend or a holiday.
ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing, and ASM #5, the regional director of operations, were made aware of the above concerns on 10/8/24 at 6:16 p.m.
No further information was provided prior to exit.
(1) This information was obtained from the following website: https://medlineplus.gov/druginfo/meds/a684051.html.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
Based on staff interview and clinical record review, the facility staff failed to maintain a complete MDS (minimum data set) assessment for one of 63 residents in the survey sample, Resident #125.
The...
Read full inspector narrative →
Based on staff interview and clinical record review, the facility staff failed to maintain a complete MDS (minimum data set) assessment for one of 63 residents in the survey sample, Resident #125.
The findings include:
For Resident #125 (R125), the facility staff failed to assess the resident's BIMS (Brief Interview for Mental Status) for the 8/27/24 quarterly MDS assessment.
Section C Cognitive Patterns of R125's quarterly MDS assessment with an ARD of 8/27/24 documented, C0100. Should Brief Interview for Mental Status (C0200-C0500) be Conducted? Attempt to conduct interview with all residents. A dash was coded, indicated the resident's BIMS was not assessed.
On 10/8/24 at 10:23 a.m., an interview was conducted with RN (registered nurse) #2 (the mobile MDS coordinator). RN #2 stated the BIMS on R125's 8/27/24 MDS assessment was accidentally missed. RN #2 stated staff was in the process of completing a corrected MDS.
On 10/8/24 at 6:25 p.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
On 10/9/24 at 1:21 p.m., ASM #5 (the regional director of operations) stated the facility did not have a policy regarding MDS assessments and the staff follow the CMS (Centers for Medicare and Medicaid Services) RAI (Resident Assessment Instrument) manual.
The CMS RAI manual documented,
SECTION C: COGNITIVE PATTERNS
Intent: The items in this section are intended to determine the resident's attention, orientation and ability to register and recall new information and whether the resident has signs and symptoms of delirium. These items are crucial factors in many care-planning decisions.
Item Rationale
Health-related Quality of Life
-Most residents are able to attempt the Brief Interview for Mental Status (BIMS), a structured cognitive interview.
-A structured cognitive test is more accurate and reliable than observation alone for observing cognitive performance. - Without an attempted structured cognitive interview, a resident might be mislabeled based on their appearance or assumed diagnosis. Structured interviews will efficiently provide insight into the resident's current condition that will enhance good care.
Coding Tips
-Attempt to conduct the interview with ALL residents .
No further information was presented prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, facility document review, and clinical record review, the facility staff failed to provide the residen...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, facility document review, and clinical record review, the facility staff failed to provide the resident/RR (resident representative) with a written summary of the baseline care plan for two of 63 residents in the survey sample, Residents #468 and #469.
The findings include:
1. For Resident #468 (R468) the facility staff failed to provide a written summary of the baseline care plan after admission on [DATE].
A review of R468's clinical record revealed she was admitted to the facility on [DATE]. A review of her clinical record, including assessments and progress notes, failed to reveal evidence that the resident and/or her RR had been given a written summary of her baseline care plan.
On 10/8/24 at 9:28 a.m., LPN (licensed practical nurse) #3, a unit manager, was interviewed. She stated the nursing and social services are responsible for developing the baseline care plan. She stated the social worker is responsible for giving the resident a written copy of the summary of the baseline care plan.
On 10/8/24 at 10:08 a.m., OSM (other staff member) #2, the director of social services stated the baseline care plan covers the first 24 to 72 hours of a resident's stay in the facility. She stated the baseline care plan triggers from the nursing assessment. She stated every member of the IDT (interdisciplinary team) should be giving the resident/RR a written copy of their portion of the baseline care plan, and should document this in the progress notes.
On 10/9/24 at 8:57 a.m., ASM (administrative staff member) #2, the director of nursing, was interviewed. She stated the resident's baseline care plan is initiated on admission by the admitting nurse. She stated the IDT talks about the resident's plan of care once the orders are in, and discusses the baseline care plan with the resident/RR. She stated social services is responsible for printing the summary out and giving it to the resident/RR.
On 10/5/24 at 6:17 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
A review of the facility policy, Care Planning Overview, revealed, in part: The facility will provide a summary of the baseline care plan to the resident and their representative.
No further information was provided prior to exit.
2. For Resident #469 (R469), the facility staff failed to provide a written summary of the baseline care plan after admission on [DATE].
A review of R469's clinical record revealed he was admitted to the facility on [DATE]. A review of his clinical record, including assessments and progress notes, failed to reveal evidence that the resident and/or his RR had been given a written summary of his baseline care plan.
On 10/8/24 at 9:28 a.m., LPN (licensed practical nurse) #3, a unit manager, was interviewed. She stated the nursing and social services are responsible for developing the baseline care plan. She stated the social worker is responsible for giving the resident a written copy of the summary of the baseline care plan.
On 10/8/24 at 10:08 a.m., OSM (other staff member) #2, the director of social services stated the baseline care plan covers the first 24 to 72 hours of a resident's stay in the facility. She stated the baseline care plan triggers from the nursing assessment. She stated every member of the IDT (interdisciplinary team) should be giving the resident/RR a written copy of their portion of the baseline care plan, and should document this in the progress notes.
On 10/9/24 at 8:57 a.m., ASM (administrative staff member) #2, the director of nursing, was interviewed. She stated the resident's baseline care plan is initiated on admission by the admitting nurse. She stated the IDT talks about the resident's plan of care once the orders are in, and discusses the baseline care plan with the resident/RR. She stated social services is responsible for printing the summary out and giving it to the resident/RR.
On 10/5/24 at 6:17 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
No further information was provided prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
Based on clinical record review, staff interview and facility document review, it was determined the facility staff failed to follow professional standards of practice for one of 63 residents in the s...
Read full inspector narrative →
Based on clinical record review, staff interview and facility document review, it was determined the facility staff failed to follow professional standards of practice for one of 63 residents in the survey sample, Resident #164.
The findings include:
For Resident #164 (R164), the facility staff failed to clarify physician orders for administration of Acetaminophen and Ibuprofen.
The physician orders documented in part,
- Acetaminophen Oral Tablet 325 MG (milligram) (Acetaminophen) Give 1 tablet by mouth every 6 hours as needed for PAIN GIVE WITH IBUPROFEN. Order Date: 05/29/2024.
- Ibuprofen Oral Tablet 200 MG (Ibuprofen) Give 2 tablet by mouth every 4 hours as needed for PAIN scale 1-3, GIVE WITH APAP. Order Date: 11/21/2023.
The eMAR (electronic medication administration record) for R164 dated 8/1/24-8/31/24 documented the resident receiving the Acetaminophen 325mg 1 tablet on 8/24/24 at 1:38 p.m. The eMAR failed to evidence the resident receiving Ibuprofen.
The eMAR for R164 dated 9/1/24-9/30/24 documented the resident receiving the Acetaminophen 325mg 1 tablet on 9/28/24 at 4:41 p.m. The eMAR failed to evidence the resident receiving Ibuprofen.
On 10/7/24 at 4:39 p.m., an interview was conducted with LPN (licensed practical nurse) #3. LPN #3 reviewed the acetaminophen and ibuprofen orders for R164 documented above and stated that they would read the orders as that the medications could be given either together or by themselves depending on the pain level because the timing was different.
On 10/8/24 at 1:08 p.m., an interview was conducted with LPN #8. LPN #8 reviewed the acetaminophen and ibuprofen orders for R164 documented above and stated that the orders were complicated, and she would need to clarify them with the physician.
The facility policy, Physician Orders failed to evidence guidance on clarifying the physician orders.
On 10/9/24 at approximately 6:15 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0661
(Tag F0661)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, facility document review, and clinical record review, the facility staff failed to develop a complete ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, facility document review, and clinical record review, the facility staff failed to develop a complete post-discharge plan of care for one of 63 residents in the survey sample, Resident #227.
The findings include:
For Resident #227 (R227) (who discharged on 3/30/24), the facility staff failed to develop a discharge summary that included a recapitulation of the resident's stay, a final summary of the resident's status, and reconciliation of medications. The facility staff also failed to ensure R227 was able to obtain medications after discharge.
A review of R227's clinical record revealed a nurse's note dated 3/30/24 that documented the resident discharged home, was provided discharge instructions, verbalized understanding, and signed. The note failed to document any further information regarding the discharge. A Discharge summary dated [DATE] documented the resident's vital signs and a social services section that included the discharge date , discharge location, and discharge goals. The following sections of the discharge summary were blank: nursing final summary, labs and radiology tests, physical function, dietary services final summary, and an activity director final summary. There was a section that documented to provide the resident/resident representative a copy of the completed and signed discharge summary and a space for the resident/resident representative to sign. This section was blank. Further review of R227's clinical record failed to reveal the facility staff completed a recapitulation of the resident's stay, a final summary of the resident's status, a reconciliation of pre-discharge and post-discharge medications, and failed to reveal the facility staff provided R227 (or the resident's representative) with prescriptions so the resident's medications could be obtained after discharge.
On 10/8/24 at 1:09 p.m., an interview was conducted with LPN (licensed practical nurse) #8 (the nurse who documented the 3/30/24 note). LPN #8 stated that when a resident is scheduled for discharge, she obtains prescriptions from the physician, gives the prescriptions to the resident, gives the resident a copy of the personal belongings inventory list that was completed on admission, and packs the resident's belongings. LPN #8 stated a RN (registered nurse) is responsible for completing and providing a discharge summary and discharge instructions. LPN #8 stated nurses should evidence prescriptions, a discharge summary, and discharge instructions are provided by documenting this in the clinical record. LPN #8 could not remember R227.
On 10/8/24 at 6:25 p.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
The facility policy titled, Discharge Planning documented, 10) Document, complete on a timely basis based on the resident's needs, and include in the clinical record, the evaluation of the resident's discharge needs and discharge plan. a) The results of the evaluation must be discussed with the resident or resident's representative. All relevant resident information must be incorporated into the discharge plan to facilitate its implementation and to avoid unnecessary delays n [sic] the resident's discharge or transfer.
No further information was presented prior to exit.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
Based on clinical record review, staff interview, and facility document review, it was determined that the facility staff failed to provide ADL (activities of daily living) care to a dependent residen...
Read full inspector narrative →
Based on clinical record review, staff interview, and facility document review, it was determined that the facility staff failed to provide ADL (activities of daily living) care to a dependent resident for one of 63 residents in the survey sample, Resident #219.
The findings include:
For Resident #219 (R219), the facility staff failed to provide incontinence care during dates in September and November of 2022.
On the most recent MDS (minimum data set) assessment, a quarterly assessment with an ARD (assessment reference date) of 9/15/22, the resident was assessed as being severely impaired for making daily decisions, requiring extensive assistance of one person for toileting and being frequently incontinent of bowel and bladder.
Review of the ADL documentation for R219 dated 9/1/22-9/30/22 failed to evidence incontinence care, toileting assistance or personal hygiene assistance provided on night shift (11:00 p.m. to 7:00 a.m.) of 9/12/22 and 9/14/22.
Review of the ADL documentation for R219 dated 11/1/22-11/30/22 failed to evidence incontinence care, toileting assistance or personal hygiene assistance provided on night shift of 11/5/22 and 11/11/22.
The comprehensive care plan for R219 documented in part, Resident has bowel and bladder incontinence disease process, immobility, dementia. Date Initiated: 09/11/2022. Under Interventions/Tasks it documented in part, Provide assistance with toileting as needed. Date Initiated: 09/11/2022 .Provide peri-care after each incontinence episode .Date Initiated: 09/11/2022 .
On 10/8/24 at 1:11 p.m., an interview was conducted with CNA (certified nursing assistant) #3. CNA #3 stated that incontinence care and toileting assistance were provided to residents throughout the shifts and at least every two hours. She stated that they evidenced the care they provided to the residents by their documentation in the ADL charting every shift. She stated that she remembered R219 but did not work the hallway that they resided on at the facility.
The facility provided ADL process policy provided dated 12/1/23 documented in part, .If a resident requires any level of assistance, the ADL care plan will reflect applicable level of assistance where the assistance of 1 care staff is implied/required per definition unless otherwise specified .
On 10/9/24 at approximately 6:15 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #221 (R221), the facility staff failed to administer Cefepime (1) as ordered by the physician when it was availa...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #221 (R221), the facility staff failed to administer Cefepime (1) as ordered by the physician when it was available in the facility.
R221 was admitted to the facility on [DATE] with diagnoses that included but were not limited to methicillin resistant staphylococcus aureus infection (2) and local infection of the skin and subcutaneous tissue, unspecified.
The physician orders for R221 documented in part, Cefepime HCl Intravenous Solution 2 GM/100ML (Cefepime HCl) Use 2 gram intravenously every 8 hours for Wound Infection for 15 Days. Order Date: 12/15/22. Start Date: 12/16/22.
The eMAR (electronic medication administration record) for R221 dated 12/1/22-12/31/22 documented R221 receiving the first dosage of the Cefepime intravenous solution on 12/16/22 at 10:00 p.m. The eMAR documented the first scheduled dose being 2:00 p.m., which was observed to be blank.
On 10/8/24 at approximately 10:00 a.m., a request was made to ASM (administrative staff member) #5, the regional director of operations for evidence of the facility in house medications available December 2022 and if Cefepime was available at that time in the facility.
On 10/8/24 at 2:26 p.m., ASM #5 provided a pharmacy delivery manifest which documented the intravenous Cefepime solution delivered on 12/16/22 at 8:50 a.m. and signed for by facility staff.
On 10/8/24 at 1:08 p.m., an interview was conducted with LPN (licensed practical nurse) #8. LPN #8 stated that when a new admission came in, they reviewed the medications list sent by the hospital and verified them with the physician. She stated that the discharge summary listed any antibiotics, and they always encouraged the hospital to administered doses prior to sending the resident to them. She stated that if a resident were admitted today, they would get the orders entered for the antibiotic, check the stat box for the medication if available and if not, the pharmacy could send it over stat or the physician would be notified to possibly change to an alternate.
On 10/9/24 at 7:49 a.m., an interview was conducted with RN (registered nurse) #6. RN #6 stated that medications were evidenced as administered by signing off on the eMAR and if they were not administered for any reason the physician should be notified.
On 10/9/24 at approximately 6:15 p.m., ASM #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the concern.
No further information was provided prior to exit.
Reference:
(1) Cefepime injection is used to treat certain infections caused by bacteria including pneumonia, and skin, urinary tract, and kidney infections. This information was obtained from the website: https://medlineplus.gov/druginfo/meds/a698021.html
(2) MRSA stands for methicillin-resistant Staphylococcus aureus. It causes a staph infection (pronounced staff infection) that is resistant to several common antibiotics. There are two types of infection. Hospital-associated MRSA happens to people in health care settings. Community-associated MRSA happens to people who have close skin-to-skin contact with others, such as athletes involved in football and wrestling. This information was obtained from the website: https://medlineplus.gov/mrsa.html
Based on staff interview, facility document review and clinical record review, it was determined the facility staff failed to administer medications as order by the physician for two of 63 residents in the survey sample, Resident #82 and #221.
The findings include:
1. For Resident #82 (R82), the facility staff failed to administer an antibiotic per the physician order.
The physician order dated 9/20/24 documented, Ciprofloxacin HCL (hydrochloride) Oral Tablet 500 MG (milligrams); Give 1 tablet by mouth two times a day for UTI (urinary tract infection) for 7 days.
The September 2024 MAR (medication administration record) documented the above order. On 9/20/24 the 6:00 p.m. dose documented a 5. A 5 indicates See Nurses Note.
The nurse's note dated 9/20/24, documented, Not available.
Review of the (Emergency backup medication system) contents revealed Ciprofloxacin 250 mg tablets were available in the backup system.
The comprehensive care plan dated, 9/22/24, documented in part, Focus: Resident has an infection disease process R/T (related to) dx (diagnosis) of UTI. The Interventions documented in part, Administer antibiotics/antimicrobials per medical provider's orders.
An interview was conducted with LPN (licensed practical nurse) #6 on 10/3/24 at 11:31 a.m. LPN #6 stated if a medication is not in the medication cart at the time of administration, the nurse should call the pharmacy and try to get the medication. LPN #6 stated, also, she could check the (Name of emergency backup medication system) that is here on the unit and most antibiotics are in there.
The facility policy, Missed Medication/Medication Error, documented in part, Procedure: I. For a new medication or a change in medication: 1. The nurse receives an order for a medication and/or changes in medication and will notify the pharmacy in a timely manner. 2. In the event the medication is not received in the next pharmacy delivery, the Charge Nurse will contact the pharmacy to attempt to resolve. a. In the event, the medication cannot be delivered in time for the next med pass, the DON/or designee will be notified to let him/her know of the failure of the medication to be delivered. 3. The Charge Nurse will check the E-kit to attempt to offer medication as prescribed. 4. In the event the medication is taken from the E-kit, the pharmacy will be notified so the E-kit can be exchanged. a. Complete required paperwork for E-kit replenishment.
ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing, and ASM # 5, the regional director of operations, were made aware of the above findings on 10/8/24 at 6:15 p.m.
No further information was obtained prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0688
(Tag F0688)
Could have caused harm · This affected 1 resident
Based on observation, resident interview, staff interview, facility document review, and clinical record review, the facility staff failed to implement interventions to treat a contracture for one of ...
Read full inspector narrative →
Based on observation, resident interview, staff interview, facility document review, and clinical record review, the facility staff failed to implement interventions to treat a contracture for one of 63 residents in the survey sample, Resident #62.
The findings include:
For Resident #62 (R62), the facility staff failed to implement a splint to prevent a right hand contracture from worsening.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) 6/25/24, R62 was coded as having no cognitive impairment according to the BIMS (brief interview for mental status). He was coded as having upper extremity range of motion impairment on one side.
On 10/26/24 at 12:36 p.m. and 10/2/24 at 11:05 a.m., R62 was observed sitting up in bed. His right hand was contracted, and there was no splint visible. When asked if he ever was provided a splint for his right hand, he stated he had one in the past, but did not know what happened to it. He added that the staff did not know where the splint was located either.
A review of R62's occupational evaluation dated 6//11/24 revealed, in part: Range of Motion UP (upper extremity) .RUE (right upper extremity) impaired .with contracture. Has a resting splint .Recs (recommendations) Splint/Orthotic Recommendations: It is recommended the patient wear a resting hand splint on right hand for 4 hours on/4 hours off in order to improve PROM (passive range of motion) for adequate hygiene and reduce pain caused by muscle tightening.
A review of R62's physician's orders failed to reveal any information related to a splint for the resident's right hand.
On 10/8/24 at 1:08 p.m., LPN (licensed practical nurse) #8 was interviewed. She stated she regularly takes care of R62. She stated she had never seen R62 with a splint, and did not know if he had ever used one. She stated she would check to see what interventions had been implemented for the resident's right hand contracture.
On 10/8/24 at 3:01 p.m., LPN #8 stated she had checked on R62's right hand contracture and the occupational therapist was currently in the room working with the resident. She stated the therapy evaluation had been ordered just a few minutes ago.
On 10/9/24 at 8:34 a.m., OSM (other staff member) #13, an occupational therapist, was interviewed. She stated she had written the report and recommendations on the 6/11/24 report for R62. She stated the resident was discharged from therapy services with a resting hand splint for his right hand. She stated there was an established schedule for putting it on and taking it off, and the CNAs (certified nursing assistants) helped him with it. She stated she evaluated the resident on 10/8/24 because the splint was misplaced. She confirmed that the discharge instructions she gave the staff on 6/11/24 contained recommendations for the resident to wear the hand splint. She stated she gives the recommendation to nurses, who are then responsible for transcribing the recommendations into orders.
On 10/9/24 at 9:23 a.m., CNA #9 was interviewed. She stated she regularly took care of R62, and that he cannot use his right hand because he has a contracture. She stated therapy has recently come to work with him for a brace, but the resident does not have a brace right now.
On 10/5/24 at 6:17 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
No further information was provided prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, facility document review and clinical record review, it was determined the facility staff failed to provide care and services for an external catheter for one of...
Read full inspector narrative →
Based on observation, staff interview, facility document review and clinical record review, it was determined the facility staff failed to provide care and services for an external catheter for one of 63 residents in the survey sample, Resident #82.
The findings include:
For Resident #82(R82), the facility staff failed to obtain a physician order for the use of an external catheter.
Observation was made of R82 was made on 9/30/24 at approximately 6:50 p.m. The resident was in bed with a urinary collection bag hanging off the bed frame.
The most recent MDS (minimum data set) assessment, with an assessment reference date of 8/8/24, in Section H - Bladder and Bowel, did not coded R82 as having an internal catheter or an external catheter.
Review of the physician orders failed to evidence a physician order for an indwelling or external urinary catheter.
On 10/2/24 12:43p.m. a second observation was made of R82. The personal aide showed this surveyor an external catheter that she was given to use for the resident and that was what was in place.
On 10/3/24 at 11:26 a.m. an interview was conducted with CNA (certified nursing assistant) #5. CNA #5 stated the way she knew a resident has an external catheter is when she goes to provide care, and she sees it in place. CNA #5 stated she was not aware of any resident on the unit that had one.
An interview was conducted with LPN (licensed practical nurse) #6 on 10/3/24 at 11:31 a.m. LPN #6 stated that she was not aware of any resident on the unit with an external catheter. She stated that the use of one required a physician order. LPN #6 stated it should be changed every two to three days and the nurse should assess the skin every day for redness or breakdown.
Further review of the clinical record failed to evidence any documentation related to the use of an external catheter.
The facility policy, Condom Care External Catheter Application and Removal, documented in part, Pre-application a. Check physician orders .Monitoring: a. Perform peri-care at least twice daily for residents with an external condom catheter. i. May perform peri-care more frequently if skin integrity is compromised. ii. Care plan individualized peri-care needs for condom catheter. b. Change condom catheter daily or more frequently if becomes soiled or falls off. c. Assess skin integrity and circulation daily.
ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing, and ASM # 5, the regional director of operations, were made aware of the above findings on 10/8/24 at 6:15 p.m.
No further information was obtained prior to exit.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected 1 resident
Based on staff interview, employee record review, and facility document review, it was determined the facility staff failed to meet the CNA (certified nursing assistant) requirements for two of five e...
Read full inspector narrative →
Based on staff interview, employee record review, and facility document review, it was determined the facility staff failed to meet the CNA (certified nursing assistant) requirements for two of five employee records reviewed, CNA #7 and #8.
The findings include:
For CNA #7 and #8, the facility staff failed to evidence the two CNAs had completed their annual mandatory 12 hours of in-service training.
CNA #7 was hired on 8/27/07. The training record documented he had 3.6 hours of in-service training in the past 12 months.
CNA #8 was hired on 87/30/12. The training record documented he had 8.1 hours of in-service training the past 12 months.
An interview was conducted with ASM (administrative staff member) #2, the director of nursing, on 10/9/24 at 8:49 a.m. ASM #2 stated she tracks the staffing education. She stated she looks at the report from (name of electronic training program) and sees who is due for training. The percentage numbers of those completed are brought to the morning meeting. The program will tell her what is due, past due and what is completed. The staff members get notification as to what they need to complete. ASM #2 stated they hold the employee responsible to complete their trainings. She stated they have the employees come in to do their training. If the staff member has not completed their hours they can't be on the schedule. ASM #2 was asked since she stated she has this system in place for checking the trainings, how did these two employees get missed, ASM #2 stated it was an oversight.
The facility policy, Staff Education and Competency Testing documented in part, Procedure: I. Assessment of Needs: a. Areas to be evaluated are determined by facility needs including but not limited to areas that are .6) Annual regulatory requirements.
ASM #1, the executive director, ASM #2, the director of nursing, and ASM #5, the regional director of operations, were made aware of the above concerns on 10/8/24 at 6:16 p.m.
No further information was provided prior to exit.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, clinical record review and facility document review, it was determined that the facility staff failed to provide medically related social services for 1 of 63 re...
Read full inspector narrative →
Based on observation, staff interview, clinical record review and facility document review, it was determined that the facility staff failed to provide medically related social services for 1 of 63 residents in the survey sample, Resident #132.
The findings include:
For Resident #132 (R132), the facility staff failed to identify the need for medically related social services and make attempts to ensure services were pursued. R132 lacked an effective support from family or community and no legal representative, was cognitively impaired with documented behavioral disturbances however the facility staff never contacted any outside services for evaluation.
R132 was admitted to the facility with diagnoses that included but were not limited to dementia, unspecified severity with other behavioral disturbance (1), major depressive disorder (2) and psychotic disorder with delusions due to known physiological condition (3).
The admission record for R132 documented the resident being their own responsible party and own emergency contact.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 7/19/24, the resident scored 3 out of 15 on the BIMS (brief interview for mental status) assessment, indicating the resident was severely impaired for making daily decisions. The assessment documented R132 displaying physical behavioral symptoms directed towards others 1 to 3 days during the assessment look-back period. Review of the BIMS assessments completed for R132 for MDS assessments completed during 3/13/23-5/16/24 documented scores ranging between 6-9, indicating moderate to severe impairment for making daily decisions.
Observations of R132 conducted during the survey dates revealed the resident to be pleasant however confused. On 9/30/24 at 7:21 p.m., R132 was observed in his room moving items around on the table talking to himself. On 10/1/24 at 1:19 p.m., R132 was observed walking in their room straightening out the sheets on the bed and moving the lunch dishes from the bed to the tray. R132 was observed in a manual wheelchair in the hallways and in the common area with no behaviors observed during the survey dates.
The comprehensive care plan for R132 documented in part,
- Cognition: [Name of R132] has impaired cognitive function. Date Initiated: 04/20/2022. Revision on: 07/18/2024.
- Behaviors: [Name of R132] has a behavior r/t (related to) hoarding garbage, keep drinks, cereals, milk along the headboard, clutter his room, including stuffing garbage under his bed, throwing meals tray at others, Screaming and yelling at others, attempting to strike staff, breaking the TV and the computer screen. Date Initiated: 09/22/2023. Revision on: 03/15/2024. Under Interventions/Tasks it documented in part, .Encourage active support by family/resident representatives. Date Initiated: 09/22/2023 .
The most recent psychiatry progress note dated 5/16/24 documented in part, .He continues to wax and wane but overall there have been no evidence of any recurrent aggression or disinhibited behavior. He does seem much calmer and less volatile. He is tolerating his psychotropic medications (Abilify and mirtazapine) without side effects .Refused cognitive testing. Obviously has some impairment .
The progress notes documented in part,
- 11/01/23 15:00 (3:00 p.m.) Review of Care Plan: Review of care plan: Resident had a scheduled care plan meeting for 10/24/2023. IDT members were present during the meeting to provide an update on resident clinical status. Medication reviewed. Resident remains LTC (long term care) . Resident does not have an advance directive/POA (power of attorney) .
- 11/09/23 17:23 (5:23 p.m.) Physician progress note . Of note, previous imaging from October shows bladder cancer, unsure if POA (power of attorney) has been made aware and what follow up care has been decided on. Attempted to contact POA however not listed, unknown by [Name of facility] as patient was brought to them after landlord called for wellness check April 2022 where APS (adult protective services) decided he is no longer able to care for himself. Appreciate CM (case manager) attempts to contact POA for further discussion on plans of care which will likely return with response tomorrow as APS is not open on the weekends. Patient remains calm and cooperative .
- 1/10/24 13:23 (1:23 p.m.) Resident is schedule for trans-urethral resection at [Name of hospital] (Ambulatory surgery center) on 2/5 arrive time at 7 am. Resident to be npo (nothing by mouth) after midnight prior. Transportation arranged. Resident was informed.
- 1/31/24 08:49 (8:49 a.m.) Note Text: Writer told the resident yesterday and this morning regarding the appointment Resident agreed to go but when the transportation arrived resident refused. He said, I am not going. Risks vs benefits explained, he still decline to go. Pre-op office was informed she will notify the nurse.
- 2/5/24 08:15 (8:15 a.m.) Note Text: Resident alert and verbally responsive. A quiet and restful night sleep maintained with no acute distress nor sob (shortness of breath). Tolerated meds with a sip od [sic] water. NPO maintained this shift. Refuse care as needed. Frequent safety checks + precautions maintained. Resident outrightly refused to go LOA (leave of absence) for a surgical appt this AM. All efforts and ooaxing [sic] made were futile. A call placed to [Name of hospital] hospital surgical unit and spoke to [Name of staff] the unit secretary as appt was properly cancelled. No chills nor fever. Nsg will cont to monitor.
- 2/5/24 08:21 (8:21 a.m.) Note Text: Resident is his own RP (responsible party).
- 3/10/24 14:03 (2:03 p.m.) Clinical team and Social Worker contacted police, CSB, and non-emergency services to request emergency mental health support regarding resident. Resident will not allow staff to enter and has barricaded himself in the room. Officer arrived without co-responder. Team made another call to the CSB and police to request a co-responder for a mental health evaluation.
- 3/15/24 10:45 (10:45 a.m.) IDT (interdisciplinary team) met: [Name of R132] is a [age of R132] with bims of 6. His diagnosis are dementia unspecified severity with other behavioral disturbance, CAD, anemia, depression, bladder cancer, adult failure to thrive. Resident went to the lobby took the trash bag smacking at the exit door nocked [sic] down the exit sign. He went to East nurses' station attempted to hit the nurse. The nurse got away resident then broke the computer screen and was going to hit other resident. Staff able to take him to the front desk to get back to the unit, resident then lay down the floor said I want the phone I want music he took my wife away. Staff was able to get resident to get up when he walked by the exit door he attempt to get out saying I am going home in Springfield. When staff attempted to redirect him, he laid on the floor again. He pulled down his pants kicking, grabbing staff. 3 staff were able to get him back to his room. Staff reoriented him his belonging resident calm down and allow staff to assist him to put his pants on. [Name of physician] saw resident new order received for Abilify 2 mg daily. Staff will continue to monitor the behavior and redirect. Care plan was updated.
The clinical record failed to evidence attempts to locate family, a power of attorney, contact with APS regarding the case prior to admission or any assessments to indicate that R132 was capable to make decisions as their own responsible party. All documents in the clinical record were signed by R132 including a Medicaid renewal application dated 7/23/24.
On 10/3/24 at 2:32 p.m., an interview was conducted with OSM (other staff member) #2, the social services director. OSM #2 had only worked at the facility for approximately a week and the former social worker no longer worked at the facility and could not be interviewed. She stated that when a cognitively impaired resident did not have a responsible party or family there were steps that they could take to assist them. She stated that they reviewed the psychiatric evaluations, assessments from the psychiatrist and involved the ombudsman to assist in a guardianship application which was a lengthy process. She stated that she was not aware of any specific policy for a resident who was cognitively impaired with no responsible party unless there were financial needs for management of funds. She stated that the facility would seek guardianship if the resident owed a specific amount to the facility.
On 10/3/24 at 3:32 p.m., an interview was conducted with OSM #16, business office manager. OSM #16 stated that she thought that someone was working on setting up a guardianship for R132 and would have to confirm. She stated that R132 had lost their Medicaid coverage a few months ago and did not have a patient funds account at the facility. She provided an authorization signed by R132 to automatically withdraw the patient liability each month from their personal bank account with the last 12 months account statements and stated that R132's patient account was paid up.
On 10/3/24 at 4:49 p.m., a follow up interview was with OSM #2. OSM #2 stated that she had not met R132 yet, but they were on their list of residents to see. She stated that R132 sounded like a resident that could possibly need a guardian to safely make decisions for them and the social workers job would be to keep an eye on them. She stated that she would expect there to be regular notes and documentation in the care plan regarding resources advocated for the resident. She stated that a resident with a BIMS of 12 or higher would be considered able to sign documents and lower than they would not be able to sign. She stated that normally they would write on the document that the resident was not able to sign, that the resident did not have a responsible party and sign the forms.
On 10/7/24 at 3:33 p.m., an interview was conducted with LPN (licensed practical nurse) #4. LPN #4 stated that R132 had behaviors at times and was seen by the psychiatrist. She stated that the staff knew how to approach R132 and when to leave him alone and reapproach later to let him calm down before providing care. She stated that his cognition varied and was better recently, she stated that he had refused to have surgery for cancer and to see the oncologist. She stated that she had never seen any family come to visit and knew that he had an ex-wife because he talked about her when he became upset, but she had never been to the facility. She stated that R132 did not have a responsible party, and she would refer to the social worker if there was an emergency and there was no one to contact.
The facility policy Social Service Addendum undated, documented in part, .The facility must provide medically related social services to attain or maintain the highest practicable physical, mental, and psychosocial well being of each resident, including the following where appropriate: (1) Assessment of each resident's psychosocial needs and development of a plan for providing care. (2) Review of the resident's needs and care plan with progress notes indicating implementation of methods to respond to identified needs. (3) Assistance to residents and spouses to utilize community resources through referral when the services needed are not provided by the facility
On 10/7/24 at 5:00 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the concern.
No further information was provided prior to exit.
Reference:
(1) dementia
A loss of brain function that occurs with certain diseases. It affects memory, thinking, language, judgment, and behavior. This information was obtained from the website: https://medlineplus.gov/ency/article/000739.htm.
(2) major depressive disorder
Major depression is a mood disorder. It occurs when feelings of sadness, loss, anger, or frustration get in the way of your life over a long period of time. It also changes how your body works. This information was obtained from the website: https://medlineplus.gov/ency/article/000945.htm.
(3) psychotic disorder
Psychotic disorders are severe mental disorders that cause abnormal thinking and perceptions. People with psychoses lose touch with reality. Two of the main symptoms are delusions and hallucinations. Delusions are false beliefs, such as thinking that someone is plotting against you or that the TV is sending you secret messages. Hallucinations are false perceptions, such as hearing, seeing, or feeling something that is not there. This information is taken from the website https://medlineplus.gov/psychoticdisorders.html.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on staff interview, facility document review, and clinical record review, the facility pharmacy failed to provide medications for one of 63 residents in the survey sample, Resident #4.
The findi...
Read full inspector narrative →
Based on staff interview, facility document review, and clinical record review, the facility pharmacy failed to provide medications for one of 63 residents in the survey sample, Resident #4.
The findings include:
For Resident #4 (R4), the pharmacy failed to provide Zosyn (1) for administration on 9/7/24.
A review of R4's clinical record revealed the following order dated 9/6/24: Piperacillin Sod-Tazobactam So Solution (1) (Zosyn) Reconstituted 4-0.5 GM (grams) Use 4.5 gram intravenously every 6 hours for osteomyelitis (infection of the bone).
A review of R4's progress notes revealed the following nurses' note dated 9/7/24: eMar - Medication Administration Note: Piperacillin Sod-Tazobactam So Solution Reconstituted 4-0.5 GM
Use 4.5 gram intravenously every 6 hours for Osteomyelitis until 10/08/2024 .Resident meds (medications) are pending for pharmacy delivery.
On 10/8/24 at 9:28 a.m., LPN (licensed practical nurse) #3 was interviewed. After reviewing R4's progress notes and September 2024 MAR (medication administration record), she stated the Zosyn was ordered for R4 as a discharge medication from the hospital. The Zosyn was to treat an infection of the resident's bone. She stated the 12:00 noon Zosyn dose was not administered because it had not arrived from the pharmacy, and she could not see that the physician was notified. She stated if a medication is not available, the nurse should contact the pharmacy and the physician, and make a note of both responses in the progress notes.
On 10/8/24 at 1:08 p.m., LPN #8 was interviewed. She stated if a medication is not available in her medication cart, she checks the facility emergency medication supply. She stated if the medication is not in the emergency supply, she contacts the physician and the pharmacy. She added: I would document what I did, and what the physician wanted to do about it.
On 10/5/24 at 6:17 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
A review of the facility policy, Missed Medication/Medication Error, revealed, in part: For any medications not available during a routine medication pass .the Charge Nurse will check the E-kit to attempt to offer medication in a timely manner .In the event the medication is not available from the E-kit or the emergency pharmacy, the charge nurse will notify the physician immediately and receive guidance on how to proceed .the Charge Nurse will notify the pharmacy and attempt to obtain the medication.
No further information was provided prior to exit.
Reference
(1) Piperacillin and tazobactam injection is used to treat pneumonia and skin, gynecological, and abdominal (stomach area) infections caused by bacteria. Piperacillin is in a class of medications called penicillin antibiotics. It works by killing bacteria that cause infection. Tazobactam is in a class called beta-lactamase inhibitor. It works by preventing bacteria from destroying piperacillin. This information is taken from the website https://medlineplus.gov/druginfo/meds/a694003.html#:~:text=Piperacillin%20is%20in%20a%20class,class%20called%20beta%2Dlactamase%20inhibitor.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
Based on staff interview, facility document review, and clinical record review, the facility staff failed to act on the pharmacist's recommendation for one of 63 residents in the survey sample, Reside...
Read full inspector narrative →
Based on staff interview, facility document review, and clinical record review, the facility staff failed to act on the pharmacist's recommendation for one of 63 residents in the survey sample, Resident #130.
The findings include:
For Resident #130 (R130), the facility staff failed to act on the pharmacist's recommendations to perform laboratory tests and failed to address a recommendation regarding an as-needed psychoactive medication for multiple months in 2023 and 2024, .
A review of R130's monthly pharmacy medication regimen reviews revealed, in part:
10/18/23 The following labs for Lipid panel and CMP (complete metabolic panel) (was due in August) are ordered .however the results for the lipids are currently not available. A review of R130's laboratory results revealed no lipid panel or CMP between 10/18/23 and 12/2/23.
12/29/23 Resident has a current order for Trazodone (1) which is a prn (as-needed) psychotropic medication without a stop date .State operations manual requires an assessment to continue a prn psychotropic medication beyond 14 days .Please reassess the prn psychotropic order.
2/6/24 Resident has a current order for Trazodone (1) which is a prn (as-needed) psychotropic medication without a stop date .State operations manual requires an assessment to continue a prn psychotropic medication beyond 14 days .Please reassess the prn psychotropic order.
A review of R130's physician orders revealed the following order dated 12/15/23: Trazodone Oral Tablet 100 mg (milligrams) Give 200 mg by mouth every 24 hours as needed for insomnia nightly. Further review of R130's orders revealed the order for the as-needed medication was not addressed by the provider until 2/21/24.
On 10/8/24 at 1:57 p.m., ASMs (administrative staff members) #8 and #9, both of whom are nurse practitioners, were interviewed. ASM #8 stated their role in responding to a pharmacist's monthly medication regimen review recommendations starts with ASM #2, the director of nursing. He stated ASM #2 is responsible for bringing the recommendations to his attention, and he responds to the recommendations as he sees fit. ASM #9 stated she follows the same process. Neither staff member ordinarily remembers to ask for the recommendations; they rely on ASM #2 to provide them.
On 10/8/24 at 2:27 p.m., LPN (licensed practical nurse) #3, a unit manager, was interviewed. She stated if she sees a recommendation from the pharmacist, she gives it to ASM #2. She stated ASM #2 is responsible for making sure the providers respond to the pharmacist's recommendations for each resident.
On 10/9/24 at 8:57 a.m., ASM #2 was interviewed. She stated she receives the pharmacist's monthly recommendations by email. She prints them and gives them to each unit manager at the morning meeting. She stated if the provider for a particular resident attends the morning meeting, that provider receives the recommendation in person. She stated once the providers address the pharmacist's concern and document their response, the unit managers are responsible for implementing the providers' orders. She stated psychoactive medications should only be ordered on an as-needed basis for 14 days.
On 10/5/24 at 6:17 p.m., ASM #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
A review of the facility policy, Medication Regimen Review, revealed, in part: The monthly medication review will be performed by a licensed pharmacist .The pharmacist will report any irregularities to the attending physician, the facility's medical director and director of nursing, and these reports must be acted upon in a timely manner that meet the needs of the residents .Any medication irregularities noted by the Consultant Pharmacist during the monthly review shall be documented on a separate, written report .The Director of Nursing or designee will be responsible for addressing all medication irregularity reports with the attending physicians in a manner that meets the needs of the resident. The consultant pharmacist shall review the reports with the director of nursing each month .The attending physician must document in the medical record that the identified irregularity has been reviewed, and what, if any action has been taken to address it.
No further information was provided prior to exit.
Reference
(1) Trazodone is used to treat depression. Trazodone is in a class of medications called serotonin modulators. It works by increasing the amount of serotonin, a natural substance in the brain that helps maintain mental balance. This information is taken from the website https://medlineplus.gov/druginfo/meds/a681038.html.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on staff interview, facility document review, and clinical record review, the facility staff failed to implement interventions to prevent unnecessary medication administration for one of 63 resi...
Read full inspector narrative →
Based on staff interview, facility document review, and clinical record review, the facility staff failed to implement interventions to prevent unnecessary medication administration for one of 63 residents in the survey sample, Resident #130.
The findings include:
A review of R130's physician orders revealed the following order dated 12/15/23: Trazodone Oral Tablet 100 mg (milligrams) Give 200 mg by mouth every 24 hours as needed for insomnia nightly. Further review of R130's orders revealed the order for the as-needed medication was not addressed by the provider until 2/21/24.
On 10/8/24 at 1:57 p.m., ASMs (administrative staff members) #8 and #9, both of whom are nurse practitioners, were interviewed. ASM #9 stated she was aware that any psychotropic prn (as-needed) order could only last for 14 days. She stated: It is regulatory. She stated she tries to always put a 14 day stop order if a resident needs a temporary as-needed psychoactive medication.
On 10/8/24 at 2:27 p.m., LPN (licensed practical nurse) #3, a unit manager, was interviewed. She stated any psychoactive order that is ordered on an as-needed basic should have a stop date. She stated these as-needed orders can only be for a total of 14 days. After this, the provider should be notified.
On 10/9/24 at 8:57 a.m., ASM #2 was interviewed. She stated psychoactive medications should only be ordered on an as-needed basis for 14 days. She stated the providers are responsible for giving a stop date for the medication.
On 10/5/24 at 6:17 p.m., ASM #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
A review of the facility policy, Pharmacy and Therapeutics Monthly Meeting, revealed, in part: Goals of Meeting .Review and address all non-responded-to Consultant Pharmacist Drug Regimen Review recommendations [greater than 30 days].
No further information was provided prior to exit.
Reference
(1) Trazodone is used to treat depression. Trazodone is in a class of medications called serotonin modulators. It works by increasing the amount of serotonin, a natural substance in the brain that helps maintain mental balance. This information is taken from the website https://medlineplus.gov/druginfo/meds/a681038.html.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected 1 resident
Based on staff interview, facility document review, and clinical record review, the facility pharmacy failed to for one of prevent a significant medication error for one of 63 residents in the survey ...
Read full inspector narrative →
Based on staff interview, facility document review, and clinical record review, the facility pharmacy failed to for one of prevent a significant medication error for one of 63 residents in the survey sample, Resident #4.
The findings include:
For Resident #4 (R4), the facility staff failed to administer Zosyn (1) at noon on 9/7/24, resulting in a significant medication error.
A review of R4's clinical record revealed the following order dated 9/6/24: Piperacillin Sod-Tazobactam So Solution (1) (Zosyn) Reconstituted 4-0.5 GM (grams) Use 4.5 gram intravenously every 6 hours for osteomyelitis (infection of the bone).
A review of R4's progress notes revealed the following nurses' note dated 9/7/24: eMar - Medication Administration Note: Piperacillin Sod-Tazobactam So Solution Reconstituted 4-0.5 GM Use 4.5 gram intravenously every 6 hours for Osteomyelitis until 10/08/2024 .Resident meds (medications) are pending for pharmacy delivery.
On 10/8/24 at 9:28 a.m., LPN (licensed practical nurse) #3 was interviewed. After reviewing R4's progress notes and September 2024 MAR (medication administration record), she stated the Zosyn was ordered for R4 as a discharge medication from the hospital. The Zosyn was to treat an infection of the resident's bone. She stated the 12:00 noon Zosyn dose was not administered because it had not arrived from the pharmacy, and she could not see that the physician was notified. She stated if a medication is not available and not administered, it is a medication error. She stated the physician should have the opportunity to adjust the order. She added that the nurse should make a note of the physician's notification and response in the progress notes.
On 10/8/24 at 1:08 p.m., LPN #8 was interviewed. She stated if a medication is not available in her medication cart, she checks the facility emergency medication supply. She stated if the medication is not in the emergency supply, she contacts the physician and the pharmacy. She added: I would document what I did, and what the physician wanted to do about it. She stated it is an error if the medication is not administered as the physician ordered it.
On 10/5/24 at 6:17 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
A review of the facility policy, Missed Medication/Medication Error, revealed, in part: For any medications not available during a routine medication pass .the Charge Nurse will check the E-kit to attempt to offer medication in a timely manner .In the event the medication is not available from the E-kit or the emergency pharmacy, the charge nurse will notify the physician immediately and receive guidance on how to proceed. the phyisician may give orders to hold the medication or an order to change the medication to something that is currently available .Failure to administer a prescribed medication as ordered is considered a medication error regardless of the reason or drug category.
No further information was provided prior to exit.
Reference
(1) Piperacillin and tazobactam injection is used to treat pneumonia and skin, gynecological, and abdominal (stomach area) infections caused by bacteria. Piperacillin is in a class of medications called penicillin antibiotics. It works by killing bacteria that cause infection. Tazobactam is in a class called beta-lactamase inhibitor. It works by preventing bacteria from destroying piperacillin. This information is taken from the website https://medlineplus.gov/druginfo/meds/a694003.html#:~:text=Piperacillin%20is%20in%20a%20class,class%20called%20beta%2Dlactamase%20inhibitor.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
Based on observation, resident interview, staff interview, and clinical record review, the facility staff failed to provide food in a form to meet a resident's needs for one of 63 residents in the sur...
Read full inspector narrative →
Based on observation, resident interview, staff interview, and clinical record review, the facility staff failed to provide food in a form to meet a resident's needs for one of 63 residents in the survey sample, Resident #170.
The findings include:
For Resident #170 (R170), the facility staff failed to cut the resident's food into bite-sized pieces, per a physician's order.
A review of R170's clinical record revealed a physician's order dated 4/10/24 for a regular diet and to cut food into bite-sized pieces.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/25/24, the resident scored 12 out of 15 on the BIMS (brief interview for mental status, indicating the resident was moderately cognitively impaired for making daily decisions.
On 10/1/24 at 9:21 a.m., R170 was served a meal tray that contained toast with sausage gravy. The meal ticket on the tray documented, CUT FOOD INTO BITE SIZE PIECES. The toast with sausage gravy was not cut into bite-sized pieces. On 10/1/24 at 1:23 p.m., R170 was served a meal tray that contained spaghetti with meat sauce and a breadstick. The meal ticket on the tray documented, CUT FOOD INTO BITE SIZE PIECES. The spaghetti or breadstick was not cut into bite-sized pieces. R170 stated the facility staff never cut up his food. On 10/2/24 at 1:20 p.m., R170 was served a meal tray that contained sliced turkey, mixed vegetables, mashed potatoes, pears, and a roll. The meal ticket on the tray documented, CUT FOOD INTO BITE SIZE PIECES. None of the food was cut into bite-sized pieces.
On 10/3/24 at 3:21 p.m., an interview was conducted with CNA (certified nursing assistant) #2. CNA #2 stated the CNAs are the primary staff who serves meal trays, and she looks at the meal tickets for special instructions. CNA #2 stated that if a meal ticket documents to cut a resident's food into bite-sized pieces, then the CNA is responsible for cutting the food. CNA #2 stated that if a resident's meal ticket documented to cut the resident's food into bite-sized pieces, she would cut the toast, the breadstick, the spaghetti, the sliced turkey, the carrot rounds in the vegetable blend, the pears, and the roll into bite-sized pieces.
On 10/4/24 at 10:32 a.m., an interview was conducted with LPN (licensed practical nurse) #2. LPN #2 stated
R170's food is supposed to be cut into bite-sized pieces because the resident presents with left sided weakness.
On 10/4/24 at 11:41 a.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern. The facility did not have a specific policy regarding providing food in a form to meet residents' needs.
No further information was presented prior to exit.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
Based on clinical record review, staff interview, and facility document review, it was determined that the facility staff failed to maintain a complete and accurate clinical record for one of 63 resid...
Read full inspector narrative →
Based on clinical record review, staff interview, and facility document review, it was determined that the facility staff failed to maintain a complete and accurate clinical record for one of 63 residents in the survey sample, Resident #224.
The findings include:
For Resident #224 (R224), the facility staff failed to maintain an accurate medical record including consultation report documentation from the facility consulted dermatologist.
The physician orders for R224 documented in part,
- Dermatology consults if the blister open/un-opened does not get better, one time only for consult for 1 day. Order Date: 03/28/2023.
- Resident is schedule for a Dermatology appointment on Thursday 4/20/2023 at 11:45 am. [Address and phone number]. Order Date: 04/17/2023.
- Dermatologist appointment on 05/11/2023 at 11:45 a.m. [Address and phone number]. Order Date: 04/20/2023.
The progress notes for R224 documented the resident going to the dermatology appointment with their POA (power of attorney) on 4/20/23 and 5/11/23. The progress notes further documented, 4/27/2023 13:55 (1:55 p.m.) Note Text: The Resident's POA came today and stated that the test result from the dermatologist came back to her and the left-hand index finger result is positive for MRSA, Resident currently taking ABT (antibiotic) and has a follow-up with the derm (dermatology) Dr. on May 11, 2023. The resident is on contact precaution. MD and house NP and POA were notified.
The clinical record failed to evidence any consultation notes regarding the dermatology visits or the culture results from the dermatologist. On 10/7/24 at approximately 5:00 p.m., a request was made to ASM (administrative staff member) #1, the executive director for the dermatology consultation notes for R224. None were received.
On 10/8/24 at 1:49 p.m., an interview was conducted with RN (registered nurse) #4, the regional educator. RN #4 stated that the staff should have followed up with the dermatologist to get a hard copy of the culture report to have the positive MRSA report in the record.
On 10/9/24 at 11:10 a.m., an interview was conducted with LPN (licensed practical nurse) #10. LPN #10 stated that when residents were sent out to consulting physicians, they normally came back with paperwork that the nurses reviewed for any new orders and follow up appointments. She stated that after the paperwork was reviewed it was kept in the medical record and stayed with the chart because it was a part of the patients' information and should stay with the record.
A review of the facility policy, Maintaining the discharged clinical record file failed to provide guidance on maintaining a complete and accurate medical record.
On 10/10/24 at 12:00 p.m., ASM #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, facility document review, and clinical record review, the facility staff failed to implement infection prevention interventions for one of 63 residents in the su...
Read full inspector narrative →
Based on observation, staff interview, facility document review, and clinical record review, the facility staff failed to implement infection prevention interventions for one of 63 residents in the survey sample, Resident #4.
The findings include:
For Resident #4 (R4), the facility staff failed to wear appropriate PPE (personal protective equipment) when they provided wound care to R4 on 10/4/24.
On 10/4/24 at 10:55 a.m., RN (registered nurse) #5, the wound nurse, was observed changing R4's pressure injury dressings. At no time during the process of changing R4's dressings did RN #5 wear a protective gown. She only wore gloves.
A review of R4's orders revealed the following order written 9/6/24: Enhanced barrier precautions .related to IV (intravenous) therapy .wounds.
On 10/8/24 at 9:28 a.m., LPN (licensed practical nurse) #3, a unit manager, was interviewed. She stated if a resident has orders for enhanced barrier precautions, any nurse providing wound care should be wearing both gloves and gown. She stated this is not only to protect the nurse and the resident who is receiving wound care, but also to protect other residents with whom the nurse might come into contact later in the shift.
On 10/8/24 at 10:28 a.m., LPN #9, the infection preventionist, was interviewed. She stated: Enhanced barrier precaustions mean gown and gloves for PPE. She stated unless a gown is worn by the nurse providing wound care, there is a risk that bacteria could be carried to other residents.
On 10/8/24 at 10:56 a.m., RN #5 was interviewed. She stated when she provided wound care to R4, she should have worn a gown to protect the resident, herself, and any other residents she might have seen that day.
On 10/5/24 at 6:17 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
No further information was provided prior to exit.
Reference
Enhanced Barrier Precautions are an infection control intervention designed to reduce transmission of multidrug-resistant organisms (MDROs) in nursing homes. Enhanced Barrier Precautions involve gown and glove use during high-contact resident care activities for residents known to be colonized or infected with a MDRO as well as those at increased risk of MDRO acquisition (e.g., residents with wounds or indwelling medical devices). This information is taken from the website https://www.cdc.gov/long-term-care-facilities/hcp/prevent-mdro/faqs.html.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0944
(Tag F0944)
Could have caused harm · This affected 1 resident
Based on staff interview, employee record review and facility document review, it was determined that one of five employee record reviews, failed to meet the training requirements for QAPI (quality as...
Read full inspector narrative →
Based on staff interview, employee record review and facility document review, it was determined that one of five employee record reviews, failed to meet the training requirements for QAPI (quality assurance performance improvement), OSM (other staff member) #13.
The findings include:
For OSM #13, the facility staff failed to provide evidence of documentation of the facility's QAPI training.
The review of OSM #13's completed trainings failed to evidence documentation of training in the QAPI process.
An interview was conducted with OSM #11, the director of rehabilitation, on 10/8/24 at 2:50 p.m. OSM #11 stated, QAPI training is not required for the therapy department, but they do attend QAPI.
The facility policy, Staff Education and Competency Testing documented in part, Procedure: I. Assessment of Needs: a. Areas to be evaluated are determined by facility needs including but not limited to areas that are .6) Annual regulatory requirements.
ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing, and ASM #5, the regional director of operations, were made aware of the above concerns on 10/8/24 at 6:16 p.m.
No further information was provided prior to exit.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0949
(Tag F0949)
Could have caused harm · This affected 1 resident
Based on staff interview, employee record review and facility document review, it was determined that one of five employee record reviews, failed to meet the training requirements for behavioral healt...
Read full inspector narrative →
Based on staff interview, employee record review and facility document review, it was determined that one of five employee record reviews, failed to meet the training requirements for behavioral health training, OSM (other staff member) #13.
The findings include:
For OSM #13, the facility staff failed to provide evidence of documentation of the facility's behavioral health training.
The review of OSM #13's completed trainings failed to evidence documentation of training in behavioral health.
An interview was conducted with OSM #11, the director of rehabilitation, on 10/8/24 at 2:50 p.m. OSM #11 stated, that behavioral health training is not required for the therapy department, many times if anything we need to know, we will get an in-service by the staff in the building.
The facility policy, Staff Education and Competency Testing documented in part, Procedure: I. Assessment of Needs: a. Areas to be evaluated are determined by facility needs including but not limited to areas that are .6) Annual regulatory requirements.
ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing, and ASM #5, the regional director of operations, were made aware of the above concerns on 10/8/24 at 6:16 p.m.
No further information was provided prior to exit.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected multiple residents
Based on clinical record review, staff interview and facility document review, it was determined that the facility staff failed to notify the physician of medications that were not administered for 2 ...
Read full inspector narrative →
Based on clinical record review, staff interview and facility document review, it was determined that the facility staff failed to notify the physician of medications that were not administered for 2 of 63 residents in the survey sample, Residents #421 and #4.
The findings include:
1. For Resident #421 (R421), the facility staff failed to notify the physician of medications not administered on multiple dates from May 2024 through September 2024.
Review of R421's eMAR (electronic medication administration record) dated 5/1/24-5/31/24 documented the resident not receiving the following scheduled medications:
- Gabapentin (1) 400mg (milligram) 2 capsules every 8 hours for neuropathy pain. On 5/14/24 at 10:00 p.m., 5/18/24 at 10:00 p.m., 5/21/24 at 2:00 p.m., 5/26/24 at 2:00 p.m., and 5/29/24 at 2:00 p.m.
- Indomethacin (2) 50mg three times a day for pain. Afternoon doses on 5/19/24, 5/21/24, 5/26/24, and 5/29/24.
- Methocarbamol (3) 500mg 2 tablets four times a day for muscle spasm. At 12:00 p.m. on 5/21/24, 5/26/24, and 5/29/24.
Review of R421's eMAR dated 6/1/24-6/30/24 documented the resident not receiving the following scheduled medications:
- Gabapentin 400mg 2 capsules every 8 hours for neuropathy pain. On 6/14/24 at 2:00 p.m., 6/17/24 at 2:00 p.m., and 6/25/24 at 2:00 p.m.
- Indomethacin 50mg 1 capsule three times a day for pain. Afternoon doses on 6/4/24, 6/14/24 and 6/17/24.
- Methocarbamol 500mg 2 tablet four times a day for muscle spasm. On 6/4/24 at 12:00 p.m., 6/14/24 at 12:00 p.m., 6/17/24 at 12:00 p.m. and 6/25/24 at 12:00 p.m.
Review of R421's eMAR dated 7/1/24-7/31/24 documented the resident not receiving the following scheduled medications:
- Lamotrigine (4) 100mg at bedtime for seizure. On 7/3/24 and 7/30/24.
- Methadone (5) 10mg 7 tablets in the morning for chronic pain. On 7/29/24.
- Trazodone (6) 75mg at bedtime for depression. On 7/7/24 and 7/30/24.
- Gabapentin 400mg 2 capsules every 8 hours for neuropathy pain. On 7/7/24 at 10:00 p.m., 7/16/24 at 10:00 p.m., 7/24/24 at 6:00 a.m. and 2:00 p.m., 7/28/24 at 2:00 p.m. and 7/30/24 at 10:00 p.m.
Review of R421's eMAR dated 8/1/24-8/30/24 documented the resident not receiving the following scheduled medications:
- Lamotrigine 100mg at bedtime for seizure. On 8/16/24, 8/20/24, 8/25/24 and 8/26/24.
- Trazodone 75mg at bedtime for depression. On 8/16/24, 8/19/24, 8/25/24 and 8/26/24.
- Gabapentin 400mg 2 capsules every 8 hours for neuropathy pain. On 8/3/24 at 2:00 p.m., 8/19/24 at 2:00 p.m. and 10:00 p.m., 8/21/24 at 2:00 p.m. and 10:00 p.m., 8/23/24 at 2:00 p.m. and 8/25/24 at 10:00 p.m.
- Methocarbamol 500mg 2 tablets four times a day for muscle spasm. On 8/2/24 at 4:00 p.m. and 8:00 p.m., 8/3/24 at 12:00 p.m., 8/16/24 at 4:00 p.m. and 8:00 p.m., 8/21/24 at 12:00 p.m., 8/21/24 at 12:00 p.m., 8/25/24 at 4:00 p.m. and 8:00 p.m., and 8/26/24 at 4:00 p.m. and 8:00 p.m.
- Methadone 10mg 7 tablets in the morning for chronic pain. On 8/4/24 and 8/16/24.
- Doxycycline (7) 100mg twice a day for cellulitis of the left third toe for 10 days. On 8/20/24 evening, 8/25/24 evening and 8/26/24 evening.
Review of R421's eMAR dated 9/1/24-9/30/24 documented the resident not receiving the following scheduled medications.
- Lamotrigine 100mg at bedtime for seizure. On 9/6/24.
- Trazodone 75mg at bedtime for depression. On 9/6/24.
- Gabapentin 400mg 2 capsules every 8 hours for neuropathy pain. On 9/6/24 at 10:00 p.m.
- Methocarbamol 500mg 2 tables four times a day for muscle spasm. On 9/6/24 at 4:00 p.m. and 8:00 p.m.
Review of R421's progress notes failed to evidence notification of the physician of the resident not receiving the scheduled medications listed on the above dates from May 2024 to September 2024. The progress notes documented either the resident being out on LOA (leave of absence), the medications held due to the resident returning to the facility intoxicated, the medications not available, or failed to document the reason the medications were not administered.
Review of the completed Leave of Absence forms for R421 documented the resident leaving the facility independently on 96 occasions between 5/7/24 and 9/12/24. Review of the LOA forms for R421 documented the resident signing out on leave of absence from the facility LOA 23 of 26 dates listed above.
On 10/9/24 at 7:49 a.m., an interview was conducted with RN (registered nurse) #6. RN #6 stated that medication administration was evidenced by the documentation on the eMAR. She stated that if the medication was not administered for any reason, the physician was notified that the medication was not given. She stated that if a resident was going on LOA overnight, they would send the medication with the family but if they were only going for the day the residents normally took the morning medications and came back to get their next scheduled medications. She stated that if the resident was due for medication and still out on LOA, they would call the physician and let them know to see if they could delay the dosage for when they returned and if they consistently missed their medications the physician should be notified to see if the schedule needed to be changed.
On 10/9/24 at 8:57 a.m., an interview was conducted with ASM (administrative staff member) #2, the director of nursing. ASM #2 stated that if a medication was not given the staff were to notify the physician. She stated that she was not aware of any residents missing their medications while out on leave of absence and as far as she knew the residents would come back to get their medications.
The facility policy Missed Medication/Medication Error undated, documented in part, . Resident's rights compliance includes providing for timely medical needs in which the physician has the opportunity to adjust and/or change medication(s) for the resident, including an awareness of risk factors when resident does not receive medication in an appropriate time frame .
On 10/10/24 at 12:00 p.m., ASM #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
Reference:
(1) Gabapentin is also sometimes used to relieve the pain of diabetic neuropathy (numbness or tingling due to nerve damage in people who have diabetes), and to treat and prevent hot flashes (sudden strong feelings of heat and sweating) in women who are being treated for breast cancer or who have experienced menopause (''change of life'', the end of monthly menstrual periods). Talk to your doctor about the risks of using this medication for your condition. This information was obtained from the website: https://medlineplus.gov/druginfo/meds/a694007.html
(2) Indomethacin is used to relieve moderate to severe pain, tenderness, swelling, and stiffness caused by osteoarthritis (arthritis caused by a breakdown of the lining of the joints), rheumatoid arthritis (arthritis caused by swelling of the lining of the joints), and ankylosing spondylitis (arthritis that mainly affects the spine). This information was obtained from the website: https://medlineplus.gov/druginfo/meds/a681027.html
(3) Methocarbamol is used with rest, physical therapy, and other measures to relax muscles and relieve pain and discomfort caused by strains, sprains, and other muscle injuries. Methocarbamol is in a class of medications called muscle relaxants. It works by slowing activity in the nervous system to allow the body to relax. This information was obtained from the website: https://medlineplus.gov/druginfo/meds/a682579.html
(4) Lamotrigine extended-release (long-acting) tablets are used with other medications to treat certain types of seizures in patients who have epilepsy. This information was obtained from the website: https://medlineplus.gov/druginfo/meds/a695007.html
(5) Methadone is used to relieve severe and persistent pain in people who are expected to need an opioid pain medication around the clock for a long time and who cannot be treated with other medications. Methadone should not be used to treat mild or moderate pain, short-term pain, or pain that can be controlled by medication that is taken as needed. Methadone also is used to prevent withdrawal symptoms in patients who were addicted to opiate drugs and are enrolled in treatment programs in order to stop taking or continue not taking the drugs. Methadone is in a class of medications called opiate (narcotic) analgesics. Methadone works to treat pain by changing the way the brain and nervous system respond to pain. It works to treat people who were addicted to opiate drugs by producing similar effects and preventing withdrawal symptoms in people who have stopped using these drugs. This information was obtained from the website: https://medlineplus.gov/druginfo/meds/a682134.html
(6) Trazodone is used to treat depression. Trazodone is in a class of medications called serotonin modulators. It works by increasing the amount of serotonin, a natural substance in the brain that helps maintain mental balance. This information was obtained from the website: https://medlineplus.gov/druginfo/meds/a681038.html
(7) Doxycycline is used to treat a variety of infections caused by certain types of bacteria. This information was obtained from the website: https://medlineplus.gov/druginfo/meds/a682063.html2. For Resident #4 (R4) the facility staff failed to notify the physician when a medication was not available for administration.
A review of R4's clinical record revealed the following order dated 9/6/24: Piperacillin Sod-Tazobactam So Solution (1) (Zosyn) Reconstituted 4-0.5 GM (grams) Use 4.5 gram intravenously every 6 hours for osteomyelitis (infection of the bone).
A review of R4's progress notes revealed the following nurses' note dated 9/7/24: eMar - Medication Administration Note: Piperacillin Sod-Tazobactam So Solution Reconstituted 4-0.5 GM Use 4.5 gram intravenously every 6 hours for Osteomyelitis until 10/08/2024 .Resident meds (medications) are pending for pharmacy delivery.
On 10/8/24 at 9:28 a.m., LPN (licensed practical nurse) #3 was interviewed. After reviewing R4's progress notes and September 2024 MAR (medication administration record), she stated the Zosyn was ordered for R4 as a discharge medication from the hospital. The Zosyn was to treat an infection of the resident's bone. She stated the 12:00 noon Zosyn dose was not administered because it had not arrived from the pharmacy, and she could not see that the physician was notified. She stated if a medication is not available and not administered, it is a medication error. She stated the physician should have the opportunity to adjust the order. She added that the nurse should make a note of the physician's notification and response in the progress notes.
On 10/8/24 at 1:08 p.m., LPN #8 was interviewed. She stated if a medication is not available in her medication cart, she checks the facility emergency medication supply. She stated if the medication is not in the emergency supply, she contacts the physician and the pharmacy. She added: I would document what I did, and what the physician wanted to do about it. She stated it is an error if the medication is not administered as the physician ordered it.
On 10/5/24 at 6:17 p.m., ASM #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
No further information was available prior to exit.
(1) Piperacillin and tazobactam injection is used to treat pneumonia and skin, gynecological, and abdominal (stomach area) infections caused by bacteria. Piperacillin is in a class of medications called penicillin antibiotics. It works by killing bacteria that cause infection. Tazobactam is in a class called beta-lactamase inhibitor. It works by preventing bacteria from destroying piperacillin. This information is taken from the website https://medlineplus.gov/druginfo/meds/a694003.html#:~:text=Piperacillin%20is%20in%20a%20class,class%20called%20beta%2Dlactamase%20inhibitor.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
4. The facility staff failed to provide a clean and homelike environment in three of six facility shower rooms, [NAME] 2, South and [NAME] 1 units.
On 10/1/24 at 11:31 a.m., an observation was made of...
Read full inspector narrative →
4. The facility staff failed to provide a clean and homelike environment in three of six facility shower rooms, [NAME] 2, South and [NAME] 1 units.
On 10/1/24 at 11:31 a.m., an observation was made of the shower room on the west 2 unit. Observation of the shower room revealed a black film covering the edging of the tile border along three of four walls. The film was observed along the grout area of the tiles and along the corners of the surface where the floor met the tile wall.
On 10/1/24 at 1:20 p.m., observation of the shower room on the west 2 unit revealed the black film remained in the same locations as described above. A shower chair was observed in the shower room with a wet towel on the chair and a gown on top of the shower chair.
On 10/2/24 at 1:17 p.m., an interview was conducted with OSM (other staff member) #1, the director of housekeeping. OSM #1 stated that housekeeping staff went in and cleaned the shower rooms daily. She stated that the CNA (certified nursing assistant) staff were responsible for picking up the linens and the housekeeping staff cleaned the walls and wiped down anything that was touched and then mopped the floors every day. She stated that once a week they did a scrubbing of the shower rooms using the floor buffer with a scrubbing pad on it. She stated that this was normally done on Saturdays but depended on the resident's shower schedules.
On 10/2/24 at 1:27 p.m., an observation of the shower room on the South unit was made with OSM #1. Observation of the South unit shower room revealed a black film in the left and right corners of the floor and wall tile. OSM #1 stated that the staff kept the shower room door closed due to the dementia residents and there was no air circulation which caused the film to grow faster.
On 10/2/24 at 1:44 p.m., an observation of the shower room on the [NAME] 2 unit revealed the findings documented above. OSM #1 stated that the shower room needed attention from housekeeping staff.
On 10/2/24 at 1:48 p.m., an observation of the shower room on the [NAME] 1 revealed a black film on the right wall around 12 tiles, along the baseboard approximately 24 inches on the front wall and in the right corner. OSM #1 stated that the black film was not homelike, and they should not have a shower room looking like that.
On 10/7/24 at 5:00 p.m., ASM (administrative staff member) #1, the executive director and ASM #2, the director of nursing were made aware of the above concern.
No further information was provided prior to exit.
2. For Resident #170 (R170), the facility staff failed to maintain the resident's toilet in a clean and homelike manner. A brown substance was observed splattered and smeared on the outside of the toilet bowl.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/25/24, the resident scored 12 out of 15 on the BIMS (brief interview for mental status), indicating the resident was moderately cognitively impaired for making daily decisions.
On 10/1/24 at 9:21 a.m., 10/2/24 at 1:10 p.m., and 10/3/24 at 11:10 a.m., a brown substance was observed splattered and smeared on the outside front and side of R170's toilet bowl. On 10/1/24 at 11:10 a.m., an interview was conducted with R170. The resident stated he uses the toilet, and he likes for it to be nice and clean because if it is not, it is an eye sore. R170 stated the staff used to clean the toilet but he had not seen the toilet cleaned in a while.
On 10/3/24 at 3:04 p.m., an interview was conducted with OSM (other staff member) #1 (the director of housekeeping). OSM #1 stated staff are supposed to clean resident bathrooms and wipe down the outside of the toilet bowls every day. At this time, R170's toilet was observed with OSM #1. OSM #1 stated the brown substance on the toilet was feces. OSM #1 stated the housekeeping staff should be observing for feces on the outside of the toilet bowl, but the CNAs (certified nursing assistants) have to wipe the feces off before the housekeepers can disinfect the toilet bowl. OSM #1 stated R170's toilet was not clean or homelike.
On 10/4/24 at 11:41 a.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
No further information was presented prior to exit.
3. For the East unit and [NAME] one unit, the facility staff failed to maintain the hallways in a clean, comfortable, and homelike manner. A marijuana odor was observed on multiple occasions.
On 10/1/24 at 12:50 p.m., 10/2/24 at 11:10 a.m., and 10/2/24 at 4:32 p.m., a marijuana odor was observed in the hallway on the east unit. On 10/2/24 at 6:27 p.m., a marijuana odor was observed in the hallway on the west one unit.
On 10/7/24 at 4:53 p.m., an interview was conducted with LPN (licensed practical nurse) #3 (the east and west one unit manager). LPN #3 stated she has smelled cigarette smoke in the hallways when residents return inside after smoking, but she wasn't sure if she has smelled marijuana. LPN #3 stated the odor is not clean, comfortable, or homelike.
On 10/7/24 at 5:07 p.m., an interview was conducted with ASM (administrative staff member) #5 (the regional director of operations). ASM #5 stated the marijuana odor in the facility had been brought to their attention, but no residents had been observed smoking marijuana. ASM #5 stated the residents had been provided education and are aware marijuana is not allowed in the facility.
On 10/8/24 at 6:25 p.m., ASM #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
No further information was presented prior to exit.
Based on observation, resident interview, staff interview, and facility document review, the facility staff failed to provide a clean, comfortable and homelike environment for three of 63 residents in the survey sample, Residents # 73 and #170 and on two of six units (East and [NAME] 1) and in , three of six shower rooms (South, [NAME] 1 and [NAME] 2).
The findings include:
1. For Resident #73(R73), the facility staff failed to maintain a homelike environment, the staff were heard yelling from room to room, around the circular unit, for each other.
On the most recent MDS (minimum data set) assessment, a quarterly assessment, with a assessment reference date of 9/23/24, the resident scored a 14 out of 15 on the BIMS (brief interview for mental status) score, indicating the resident was not cognitively impaired for making daily decisions.
An interview was conducted with R73 on 9/30/24 at approximately 6:50 p.m. The resident stated the staff yell back and forth to each other all through the day and sometimes through the night. She stated it was very disturbing when you are trying to rest.
On 10/1/24 at 10:32 a.m. Observation of the unit on which R73 resides, it was noted that two CNAs (certified nursing assistants) calling out to each other from inside resident rooms. The female CNA called for the male CNA, and he answered and then the female CNA called out again for the male CNA. The surveyor was in the hallway and the CNA were not in close vicinity of each other. They were several rooms away from each other.
An interview was conducted on 10/3/24 11:46 a.m. with CNA #4. CNA #4 stated she has not heard anyone calling out to each other, but this was not her normal unit to work. When asked why we should not call out for staff members, CNA #4 stated she could 't tell as she doesn't do that, and it was not making a homelike environment for the residents.
No policy was received for a clean, comfortable and homelike environment.
ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing, and ASM #5, the regional director of operations, were made aware of the above concerns on 10/8/24 at 6:16 p.m.
No further information was provided prior to exit.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected multiple residents
Based on staff interview and facility document review, the facility staff failed to maintain evidence of grievances for one of three years, the year 2022.
The findings include:
The facility staff fail...
Read full inspector narrative →
Based on staff interview and facility document review, the facility staff failed to maintain evidence of grievances for one of three years, the year 2022.
The findings include:
The facility staff failed to provide evidence of grievances for the year 2022.
On 10/7/24 at 12:58 p.m., grievance/concern forms for the year of 2022 were requested.
On 10/8/24 at 9:48 a.m., an interview was conducted with ASM (administrative staff member) #5 (the regional director of operations). ASM #5 stated the social worker who was employed during 2022 was no longer employed at the facility and the staff were not able to find all grievance/concern forms from that year. ASM #5 stated the staff were only able to find pieces of grievance/concern forms and she knew more were completed then the staff could find.
On 10/8/24 at 10:15 a.m., an interview was conducted with OSM (other staff member) #2 (the current director of social services). OSM #2 stated grievances and the resolutions should be documented on a concern form and kept in a folder in the social services office.
On 10/8/24 at 6:25 p.m., ASM #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
The facility policy titled, Resident Grievance
5. Documentation
a. The facility will keep evidence of the resolution of all grievances for a period of three (3)
years from the date the grievance decision is issued.
No further information was presented prior to exit.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected multiple residents
3. For Resident #74 (R74), the facility staff failed to implement the comprehensive care plan to obtain laboratory testing as ordered.
The comprehensive care plan for R74 documented in part, Parkinson...
Read full inspector narrative →
3. For Resident #74 (R74), the facility staff failed to implement the comprehensive care plan to obtain laboratory testing as ordered.
The comprehensive care plan for R74 documented in part, Parkinsons: [Name of R74] has Parkinsons. Date Initiated: 06/15/2024. Under Interventions/Tasks it documented in part, .Obtain and monitor lab/diagnostic studies, as ordered. Report abnormal findings to medical provider, resident and resident representative. Date Initiated: 06/15/2022 .
The physician orders for R74 documented in part, TSH (thyroid stimulating hormone) every 6 month in December and June on 15 every night shift every 6 month(s) starting on the 15th for 168 day(s). Order Date: 07/24/2023. Start Date: 12/14/2023. End Date: 01/17/2024.
The eTAR (electronic treatment administration record) for R74 dated 12/1/23-12/31/23 documented the TSH scheduled beginning on 12/15/23.
Review of the clinical record failed to evidence results for a TSH completed on 12/15/23. The progress notes failed to evidence the resident refusing the laboratory testing or documentation of the laboratory testing completed as ordered in December of 2023.
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1, regarding the purpose of the care plan. RN #1 stated, If there is no care plan, there is no care. RN #1 stated everything revolves around the care plan and if staff are not able to plan for the patient, then there is no way for staff to care for them. RN #1 stated staff must follow the care plan to provide care.
On 10/8/24 at 9:28 a.m., an interview was conducted with LPN (licensed practical nurse) #3. LPN #3 stated that they had an outside lab company that came in to draw labs. She stated that the technician came in during the week early in the morning and was given a printout of the residents who were scheduled for lab testing. She stated that the nurse and the technician signed the forms, and they drew the labs. She stated that if there were any issues getting the specimen the technician let the nurse know and they called the physician and attempted on the next lab draw day.
On 10/8/24 at 1:08 p.m., an interview was conducted with LPN #8. LPN #8 stated that the night nurse printed out all lab orders from the medical records and flagged them for the lab technician who came in early in the morning. She stated that the labs were normally done before she arrived for the day shift, so she watched for the results to come into the medical record during the day. She stated that the labs that were scheduled triggered on the eMAR or eTAR showing that they needed to be done.
On 10/9/24 at approximately 6:15 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
4. For Resident #421 (R421), the facility staff failed to implement the comprehensive care plan to administer medications as ordered on multiple dates from July 2024 through September 2024.
The comprehensive care plan for R421 documented in part, [Name of R421] uses, anti-depressant medication . Date Initiated: 07/06/2024. Under Interventions/Tasks it documented in part, .Provide anti-depressant medication per medical provider's orders. Date Initiated: 05/08/2024. The care plan further documented, Resident has cellulitis to left 3rd toe and on ABT (antibiotic) doxycycline. Date Initiated: 08/20/2024. Under Interventions/Tasks it documented in part, Administer antibiotics / antimicrobials per medical provider's orders . Date Initiated 08/20/2024.
Review of R421's eMAR dated 7/1/24-7/31/24 documented the resident not receiving the following scheduled medications:
- Trazodone 75mg at bedtime for depression. On 7/7/24 and 7/30/24.
Review of R421's eMAR dated 8/1/24-8/30/24 documented the resident not receiving the following scheduled medications:
- Trazodone 75mg at bedtime for depression. On 8/16/24, 8/19/24, 8/25/24 and 8/26/24.
- Doxycycline 100mg twice a day for cellulitis of the left third toe for 10 days. On 8/20/24 evening, 8/25/24 evening and 8/26/24 evening.
Review of R421's eMAR dated 9/1/24-9/30/24 documented the resident not receiving the following scheduled medications.
- Trazodone 75mg at bedtime for depression. On 9/6/24.
Review of R421's progress notes failed to evidence notification of the physician of the resident not receiving the scheduled medications listed on the above dates above.
Review of the completed Leave of Absence forms for R421 documented the resident signing out on leave of absence on the dates listed above.
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1, regarding the purpose of the care plan. RN #1 stated, If there is no care plan, there is no care. RN #1 stated everything revolved around the care plan and if staff were not able to plan for the patient, then there was no way for staff to care for them. RN #1 stated staff had to follow the care plan to provide care. RN #1 stated nurses could access and look at residents' care plans and nurses communicated residents' needs to CNAs (certified nursing assistants) during shift report.
On 10/9/24 at 7:49 a.m., an interview was conducted with RN #6. RN #6 stated that medication administration was evidenced by the documentation on the eMAR. She stated that if the medication was not administered for any reason, the physician was notified that the medication was not given. She stated that if a resident was going on LOA overnight, they would send the medication with the family but if they were only going for the day the residents normally took the morning medications and came back to get their next scheduled medications. She stated that if the resident was due for medication and still out on LOA, they would call the physician and let them know to see if they could delay the dosage for when they returned and if they consistently missed their medications the physician should be notified to see if the schedule needed to be changed.
On 10/9/24 at 8:57 a.m., an interview was conducted with ASM (administrative staff member) #2, the director of nursing. ASM #2 stated that if a medication was not given the staff were to notify the physician. She stated that she was not aware of any residents missing their medications while out on leave of absence and as far as she knew the residents would come back to get their medications.
On 10/10/24 at 12:00 p.m., ASM #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
5. For Resident #219 (R219), the facility staff failed to implement the comprehensive care plan to provide incontinence care during dates in September and November of 2022.
On the most recent MDS (minimum data set) assessment, a quarterly assessment with an ARD (assessment reference date) of 9/15/22, the resident was assessed as being severely impaired for making daily decisions, requiring extensive assistance of one person for toileting and being frequently incontinent of bowel and bladder.
The comprehensive care plan for R219 documented in part, Resident has bowel and bladder incontinence disease process, immobility, dementia. Date Initiated: 09/11/2022. Under Interventions/Tasks it documented in part, Provide assistance with toileting as needed. Date Initiated: 09/11/2022 .Provide peri-care after each incontinence episode .Date Initiated: 09/11/2022 .
Review of the ADL (activities of daily living) documentation for R219 dated 9/1/22-9/30/22 failed to evidence incontinence care, toileting assistance or personal hygiene assistance provided on night shift (11:00 p.m. to 7:00 a.m.) of 9/12/22 and 9/14/22.
Review of the ADL documentation for R219 dated 11/1/22-11/30/22 failed to evidence incontinence care, toileting assistance or personal hygiene assistance provided on night shift of 11/5/22 and 11/11/22.
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1, regarding the purpose of the care plan. RN #1 stated, If there is no care plan, there is no care. RN #1 stated everything revolved around the care plan and if staff were not able to plan for the patient, then there was no way for staff to care for them. RN #1 stated staff had to follow the care plan to provide care. RN #1 stated nurses could access and look at residents' care plans and nurses communicated residents' needs to CNAs (certified nursing assistants) during shift report.
On 10/8/24 at 1:11 p.m., an interview was conducted with CNA #3. CNA #3 stated that incontinence care and toileting assistance were provided to residents throughout the shifts and at least every two hours. She stated that they evidenced the care they provided to the residents by their documentation in the ADL charting every shift. She stated that she remembered R219 but did not work the hallway that they resided on at the facility.
On 10/9/24 at approximately 6:15 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.6. For Resident #4 (R4), the facility staff failed to implement the care plan to treat an infection in the resident's bone.
A review of R4's clinical record revealed the following order dated 9/6/24: Piperacillin Sod-Tazobactam So Solution (1) (Zosyn) Reconstituted 4-0.5 GM (grams) Use 4.5 gram intravenously every 6 hours for osteomyelitis (infection of the bone).
A review of R4's progress notes revealed the following nurses' note dated 9/7/24: eMar - Medication Administration Note: Piperacillin Sod-Tazobactam So Solution Reconstituted 4-0.5 GM Use 4.5 gram intravenously every 6 hours for Osteomyelitis until 10/08/2024 .Resident meds (medications) are pending for pharmacy delivery.
A review of R4's care plan dated 5/20/24 and updated 9/24/24 revealed, in part: Resident is currently on intravenous therapy r/t (related to) [osteomyelitis] .Administer IV medications per medical provider's orders.
On 10/3/24 at 5:23 p.m., RN (registered nurse) #1 was interviewed. RN #1 stated, If there is no care plan, there is no care. RN #1 stated everything revolves around the care plan and if staff are not able to plan for the patient, then there is no way for staff to care for them. RN #1 stated staff have to follow the care plan to provide care. RN #1 stated nurses can access and look at residents' care plans and nurses communicate residents' needs to CNAs (certified nursing assistants) during shift report.
On 10/8/24 at 9:28 a.m., LPN (licensed practical nurse) #3 was interviewed. After reviewing R4's progress notes and September 2024 MAR (medication administration record), she stated the Zosyn was ordered for R4 as a discharge medication from the hospital. The Zosyn was to treat an infection of the resident's bone. She stated the 12:00 noon Zosyn dose was not administered because it had not arrived from the pharmacy.
On 10/5/24 at 6:17 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
No further information was provided prior to exit.
7. For Resident #62 (R62), the facility staff failed to implement the resident's care plan for a resting hand splint on his right hand.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) 6/25/24, R62 was coded as having no cognitive impairment according to the BIMS (brief interview for mental status). He was coded as having upper extremity range of motion impairment on one side.
On 10/26/24 at 12:36 p.m. and 10/2/24 at 11:05 a.m., R62 was observed sitting up in bed. His right hand was contracted, and there was no splint visible. When asked if he ever was provided a splint for his right hand, he stated he had one in the past, but did not know what happened to it. He added that the staff did not know where the splint was located either.
A review of R62's occupational evaluation dated 6//11/24 revealed, in part: Range of Motion UP (upper extremity) .RUE (right upper extremity) impaired .with contracture. Has a resting splint .Recs (recommendations) Splint/Orthotic Recommendations: It is recommended the patient wear a resting hand splint on right hand for 4 hours on/4 hours off in order to improve PROM (passive range of motion) for adequate hygiene and reduce pain caused by muscle tightening.
A review of R62's physician's orders failed to reveal any information related to a splint for the resident's right hand.
A review of R62's care plan dated 7/8/23 failed to reveal any information related to his contracture and the need for a resting hand splint.
On 10/8/24 at 1:08 p.m., LPN (licensed practical nurse) #8 was interviewed. She stated she regularly takes care of R62. She stated she had never seen R62 with a splint, and did not know if he had ever used one. She stated she would check to see what interventions had been implemented for the resident's right hand contracture.
On 10/8/24 at 3:01 p.m., LPN #8 stated she had checked on R62's right hand contracture and the occupational therapist was currently in the room working with the resident. She stated the therapy evaluation had been ordered just a few minutes ago.
On 10/9/24 at 8:34 a.m., OSM (other staff member) #13, an occupational therapist, was interviewed. She stated she had written the report and recommendations on the 6/11/24 report for R62. She stated the resident was discharged from therapy services with a resting hand splint for his right hand. She stated there was an established schedule for putting it on and taking it off, and the CNAs (certified nursing assistants) helped him with it. She stated she evaluated the resident on 10/8/24 because the splint was misplaced. She confirmed that the discharge instructions she gave the staff on 6/11/24 contained recommendations for the resident to wear the hand splint. She stated she gives the recommendation to nurses, who are then responsible for transcribing the recommendations into orders. She stated there should be a care plan for the resident's contracture and interventions to treat it.
On 10/5/24 at 6:17 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
No further information was provided prior to exit.
Based on observation, resident interview, staff interview, facility document review, and clinical record review, the facility staff failed to develop and/or implement a comprehensive care plan for eight of 63 residents in the survey sample, Residents #228, #170, #74, #421, #219, #4, #62, and #82.
The findings include:
1. For Resident #228 (R228), the facility staff failed to develop a comprehensive care plan for activities.
A review of R228's clinical record revealed an activity preference interview dated 9/23/23 that documented the resident reported a current interest in spending time outdoors and walking. R228's comprehensive care plan dated 9/20/23 failed to document information regarding activities.
On 10/8/24 at 9:03 a.m., an interview was conducted with OSM (other staff member) #8 (the activities director). OSM #8 stated every resident should have an activities care plan because the activities staff must have a plan of care to know exactly what they are going to do with the residents. OSM #8 stated the activities care plan should be developed on admission and reviewed/revised annually or with significant changes. OSM #8 stated a lot of residents' activities care plans were not done when she began employment at the facility in January 2024 and she was still trying to complete the care plans.
On 10/8/24 at 6:25 p.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
The facility policy titled, Plan of Care Overview documented,
II. Care Plan Team
a. An interdisciplinary care team that participates in the planning and implementation of care may include but is not limited to:
i. Clinical team, licensed and non-licensed personnel
1. The 'MDS (minimum data set) Coordinator' will oversee and coordinate the care team and PoC (Plan of Care)
2. Nurses are expected to participate in the resident plan of care for reviewing and revising the care plan of residents they provide care for as the resident's condition warrants
ii. Therapy team
iii. Social services and Activities team
iv. Nutritional dietary team
v. Medical providers
vi. Pharmacists or other ad hoc consultants, when appropriate
vii. Business team, where applicable
viii. Administrative team, where applicable
ix. Family, resident, resident representative or other individual the resident requests
to be present
b. Members of the care planning team will coordinate care to meet resident preferences and care needs utilizing a holistic approach to care.
No further information was presented prior to exit.
2. For Resident #170 (R170), the facility staff failed to implement the resident's comprehensive care plan for nutrition.
R170's comprehensive care plan dated 10/12/23 documented, Potential for altered nutrition status/nutrition. Provide meals per diet order of Regular diet, Regular texture, Regular consistency. Cut food into bite-sized pieces .
A review of R170's clinical record revealed a physician's order dated 4/10/24 for a regular diet and to cut food into bite-sized pieces.
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 6/25/24, the resident scored 12 out of 15 on the BIMS (brief interview for mental status), indicating the resident was moderately cognitively impaired for making daily decisions.
On 10/1/24 at 9:21 a.m., R170 was served a meal tray that contained toast with sausage gravy. The meal ticket on the tray documented, CUT FOOD INTO BITE SIZE PIECES. The toast with sausage gravy was not cut into bite-sized pieces. On 10/1/24 at 1:23 p.m., R170 was served a meal tray that contained spaghetti with meat sauce and a breadstick. The meal ticket on the tray documented, CUT FOOD INTO BITE SIZE PIECES. The spaghetti or breadstick was not cut into bite-sized pieces. R170 stated the facility staff never cut up his food. On 10/2/24 at 1:20 p.m., R170 was served a meal tray that contained sliced turkey, mixed vegetables, mashed potatoes, pears, and a roll. The meal ticket on the tray documented, CUT FOOD INTO BITE SIZE PIECES. None of the food was cut into bite-sized pieces.
On 10/3/24 at 3:21 p.m., an interview was conducted with CNA (certified nursing assistant) #2. CNA #2 stated the CNAs are the primary staff who serve meal trays, and she looks at the meal tickets for special instructions. CNA #2 stated that if a meal ticket documents to cut a resident's food into bite-sized pieces, then the CNA is responsible for cutting the food. CNA #2 stated that if a resident's meal ticket documented to cut the resident's food into bite-sized pieces, she would cut the toast, the breadstick, the spaghetti, the sliced turkey, the carrot rounds in the vegetable blend, the pears, and the roll into bite-sized pieces.
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1, regarding the purpose of the care plan. RN #1 stated, If there is no care plan, there is no care. RN #1 stated everything revolves around the care plan and if staff are not able to plan for the patient, then there is no way for staff to care for them. RN #1 stated staff have to follow the care plan to provide care. RN #1 stated nurses can access and look at residents' care plans and nurses communicate residents' needs to CNAs during shift report.
On 10/4/24 at 10:32 a.m., an interview was conducted with LPN (licensed practical nurse) #2. LPN #2 stated
R170's food is supposed to be cut into bite-sized pieces because the resident presents with left sided weakness.
On 10/4/24 at 11:41 a.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
No further information was presented prior to exit.
8. For Resident #82 (R82), the facility staff failed to implement the comprehensive care plan for administering antibiotics per the physician order.
The comprehensive care plan dated, 9/22/24, documented in part, Focus: Resident has an infection disease process R/T (related to) dx (diagnosis) of UTI. The Interventions documented in part, Administer antibiotics/antimicrobials per medical provider's orders.
The physician order dated 9/20/24 documented, Ciprofloxacin HCL (hydrochloride) Oral Tablet 500 MG (milligrams); Give 1 tablet by mouth two times a day for UTI (urinary tract infection) for 7 days.
The September 2024 MAR (medication administration record) documented the above order. On 9/20/24 the 6:00 p.m. dose documented a 5. A 5 indicates See Nurses Note.
The nurse's note dated 9/20/24, documented, Not available.
Review of the (Emergency backup medication system) contents revealed Ciprofloxacin 250 mg tablets were available in the backup system.
An interview was conducted on 10/3/24 at 11:31 a.m. with LPN (licensed practical nurse) #6. LPN #6 stated the purpose of the care plan is to know what the patient needs and what care will be provided. LPN #6 stated the care plan should be followed.
ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing, and ASM # 5, the regional director of operations, were made aware of the above findings on 10/8/24 at 6:15 p.m.
No further information was obtained prior to exit.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
Based on observation, staff interview, facility document review, and clinical record review, the facility staff failed to review and revise the comprehensive care plan for five of 63 residents in the ...
Read full inspector narrative →
Based on observation, staff interview, facility document review, and clinical record review, the facility staff failed to review and revise the comprehensive care plan for five of 63 residents in the survey sample, Residents #48, #110, #123, #162, #190.
The findings include:
1. For Resident #48 (R48), the facility staff failed to review and revise the resident's comprehensive care plan for bed rails.
R48's comprehensive care plan, revised on 8/22/24, failed to document information regarding bed rails.
On 10/1/24 at 12:05 p.m., R48 was observed lying in bed with bilateral grab bars (bed rails) in the upright position.
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1, regarding the purpose of the care plan. RN #1 stated, If there is no care plan, there is no care. RN #1 stated everything revolves around the care plan and if staff are not able to plan for the patient, then there is no way for staff to care for them. RN #1 stated residents' care plans should include documentation regarding grab bars because this communicates the use of grab bars to staff in case they have a question.
On 10/8/24 at 6:25 p.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
The facility policy titled, Plan of Care Overview documented,
II. Care Plan Team
a. An interdisciplinary care team that participates in the planning and implementation of care may include but is not limited to:
i. Clinical team, licensed and non-licensed personnel
1. The MDS Coordinator will oversee and coordinate the care team and PoC (Plan of Care)
2. Nurses are expected to participate in the resident plan of care for reviewing and revising the care plan of residents they provide care for as the resident's condition warrants
ii. Therapy team
iii. Social services and Activities team
iv. Nutritional dietary team
v. Medical providers
vi. Pharmacists or other ad hoc consultants, when appropriate
vii. Business team, where applicable
viii. Administrative team, where applicable
ix. Family, resident, resident representative or other individual the resident requests
to be present
b. Members of the care planning team will coordinate care to meet resident preferences and care needs utilizing a holistic approach to care.
No further information was presented prior to exit.
2. For Resident #110 (R110), the facility staff failed to review and revise the resident's comprehensive care plan when the resident hit another resident on 5/13/24.
A review of R110's clinical record revealed a nurse practitioner's note dated 5/13/24 that documented the resident hit another resident on that date. Further review of R110's clinical record revealed the resident was transferred to another unit and evaluated by a psychiatrist but failed to reveal R110's comprehensive care plan (initiated on 10/1/21) was reviewed and revised regarding the incident.
On 10/3/24 at 2:38 p.m., an interview was conducted with OSM (other staff member) #2 (the director of social services). OSM #2 stated if a resident hits another resident, his or her care plan should be reviewed and revised because it's important for all staff to observe and be mindful of potential interventions.
On 10/4/24 at 11:41 a.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
No further information was presented prior to exit.
3. For Resident #123 (R123), the facility staff failed to review and revise the resident's comprehensive care plan when the resident hit another resident on 5/1/24.
A review of R123's clinical record revealed a nurse's note dated 5/1/24 that documented the resident hit another resident on that date. Further review of R123's clinical record revealed the resident was transferred to another unit and evaluated by a psychiatrist but failed to reveal R123's comprehensive care plan (initiated on 1/29/22) was reviewed and revised regarding the incident.
On 10/3/24 at 2:38 p.m., an interview was conducted with OSM (other staff member) #2 (the director of social services). OSM #2 stated if a resident hits another resident, his or her care plan should be reviewed and revised because it's important for all staff to observe and be mindful of potential interventions.
On 10/4/24 at 11:41 a.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
No further information was presented prior to exit.
4. For Resident #162 (R162), the facility staff failed to review and revise the resident's comprehensive care plan when the resident was hit by another resident on 5/1/24 and 5/13/24.
A review of R162's clinical record revealed progress notes that documented a resident hit R162 on 5/1/24 and another resident hit R162 on 5/13/24. Further review of R162's clinical record revealed the resident was evaluated by a psychiatrist but failed to reveal R162's comprehensive care plan (initiated on 7/25/23) was reviewed and revised regarding both incidences.
On 10/3/24 at 2:38 p.m., an interview was conducted with OSM (other staff member) #2 (the director of social services). OSM #2 stated if a resident is hit by another resident, his or her care plan should be reviewed and revised so staff are aware of potential triggers, any potential safety concerns of the resident not feeling safe, and to provide coping skills if needed.
On 10/4/24 at 11:41 a.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
No further information was presented prior to exit.
5. For Resident #190, the facility staff failed to review and revise the comprehensive care plan for the treatment of a urinary tract infection (UTI).
The physician order dated, 9/30/24, documented, Levofloxacin (an antibiotic used to treat infection) Tablet 250 MG (milligrams); Give 1 tablet by mouth one time a day for UTI for 3 days.
Review of the comprehensive care plan last updated on 10/1/24, failed to evidence documentation related to the treatment of a uriary tract infection.
An interview was conducted with LPN (licensed practical nurse) #6 on 10/3/24 at 11:26 a.m. LPN #6 stated the unit manager and supervisors update the care plans, the floor nurses do not update the care plans. She stated the treatment of a urinary tract infection should be on the care plan.
ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing, and ASM # 5, the regional director of operations, were made aware of the above findings on 10/8/24 at 6:15 p.m.
No further information was obtained prior to exit.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0679
(Tag F0679)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff interview and facility document review, it was determined that the facility staff failed ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review, staff interview and facility document review, it was determined that the facility staff failed to provide activities based on resident preferences for two of 63 residents in the survey sample, Residents #219 and #228.
The findings include:
1. For Resident #219 (R219), the facility staff failed to provide activities based on the comprehensive assessment and care plan preferences.
On the admission MDS (minimum data set) with an ARD (assessment reference date) of 9/8/22, the resident scored 2 out of 15 on the BIMS (brief interview for mental status) assessment, indicating the resident was severely impaired for making daily decisions. The assessment documented preferences for music being very important and participating in activities, doing things with groups of people, being around animals, having books and magazines, going outside and participating in religious services being somewhat important to the resident as reported by the family or significant other.
The activity preferences interview for R219 dated 9/2/22 documented past interest in playing checkers, reading, golfing, football, cooking, news, outings, religious services, and attending social events. It further documented current interest in walking, music, game shows, spending time outdoors, and talking. It documented that R219 preferred to participate in morning activities in the day/activity room and was cooperative and interested in activities per the responsible party interview.
The comprehensive care plan for R219 documented in part, The resident has impaired cognitive function Alzheimer's Dementia. Date Initiated: 09/11/2022. Under Interventions/Tasks it documented in part, Provide a program of activities that accommodates abilities. Date Initiated: 09/11/2022 . The care plan further documented, I have no plans for discharge secondary to community. Date Initiated: 9/13/2022. Revision on: 11/16/2022. Under Interventions/Tasks it documented in part, .Invite and encourage [Name of R219] to attend activities of interest. Date Initiated: 09/13/2022. Revision on: 11/16/2022.
On 10/8/24 at 8:26 a.m., an interview was conducted with OSM (other staff member) #8, activities director. OSM #8 stated that they had worked at the facility since January of 2024 and had started tracking activity participation then. She stated that they did not have any records of activity participation prior to then. She stated that when she started working at the facility there was an activities assistant running the program and had been for about three or four months before. She stated that assessments were completed on all residents to gather the information they needed to determine which activities were the best fit for the residents based on their preferences. She stated that they currently offered activities such as one to one in rooms, patio activities, carnivals, basketball games, cookouts, sports days, Hawaiian days, Western days, shopping trips, restaurant trips and music activities. She stated that on the dementia unit they also brought residents outside on the patio to participate in fresh air activities.
On 10/8/24 at 10:30 a.m., an interview was conducted with OSM #19, activity leader. OSM #19 stated that they were working on the dementia unit during the time that R219 resided there. She stated that they were doing activities such as music therapy, balloon batting, arts and crafts, coloring, ball, hot potato, sing alongs, snacks, drinks, and movies. She stated that she would check to see if there was any evidence of R219 participating in any activities in September to November of 2022, but they did not remember the resident.
The facility policy Activities Program undated, documented in part, .It is the policy of this facility to provide resident centered care that meets the psychosocial, physical and emotional needs and concerns of the residents . The activity program is: a. Designed to encourage restoration to self-care and maintenance of normal activity that is geared to the individual resident's needs. b. Scheduled daily and residents are given an opportunity to contribute to the planning, preparation, conducting, cleanup and critique of the program. c. Consists of individual and small and large group activities which are designed to meet the needs and interests of each resident and includes, at a minimum: i. Social activities. ii. Indoor and outdoor activities. iii. Activities away from the facility. iv. Religious programs. v. Creative activities. vi. Intellectual and educational activities. vii. Exercise activities. viii. Individualized activities. ix. In-room activities. x. Community activities .
On 10/9/24 at approximately 6:15 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the concern.
No further information was provided prior to exit.2. For Resident #228 (R228), the resident was assessed as reporting a current interest in spending time outdoors. The facility staff failed to provide this desired activity.
R228 was admitted to the facility on [DATE]. A review of R228's clinical record revealed an activity preference interview dated 9/23/23 that documented the resident reported a current interest in spending time outdoors and walking. R228's comprehensive care plan dated 9/20/23 failed to document information regarding activities. Further review of R228's clinical record (including nurses' notes and activities program documentation forms for January 2024 through June 2024) failed to reveal the resident spent any time outdoors. R228 discharged from the facility on 6/26/24.
On 10/8/24 at 9:03 a.m., an interview was conducted with OSM (other staff member) #8 (the activities director). OSM #8 stated an assessment to determine residents' preferred activities is completed so staff can gather information and determine an activities plan for residents. OSM #8 stated that when activities staff take residents outside for fresh air, they should write that activity on the activities program documentation forms and document the activity occurred. OSM #8 stated R228 didn't want to go outside and was very content in her own space inside. Further review of R228's clinical record failed to reveal the resident was offered to be taken outside or refused to go outside.
On 10/8/24 at 6:25 p.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
No further information was presented prior to exit.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected multiple residents
2. For Resident #166 (R166), the facility staff failed to evidence a consent for the use of bed rails, alternatives attempted prior to installing bed rails, and review of the risks and benefits of bed...
Read full inspector narrative →
2. For Resident #166 (R166), the facility staff failed to evidence a consent for the use of bed rails, alternatives attempted prior to installing bed rails, and review of the risks and benefits of bed rails prior to installation.
On the most recent MDS (minimum data set) assessment, an annual assessment, with an assessment reference date of 6/3/24, the resident scored 15 out of 15 on the BIMS (brief interview for mental status) assessment, indicating they were cognitively intact for making daily decisions. The resident was coded as requiring set up assistance with bed mobility and dependent for transfers.
On 10/1/24 at 8:44 a.m., an observation was made of R166 in bed with bilateral bar shaped bed rails in place. At that time, an interview was conducted with R166 who stated that they grabbed on the bar when turning in the bed. R166 stated that the bed had always that the bars on it and they used them and had never used anything else.
An additional observation of R166 in the bed with the bilateral bar shaped bed rails in place were made on 10/1/24 at 2:18 p.m. and 10/2/24 at 8:10 a.m.
The physician orders for R166 failed to evidence an order for the bed rails.
The comprehensive care plan for R166 failed to evidence the use of bed rails.
The admission assessment for R166 dated 9/27/24 failed to evidence the use of bed rails.
A bed safety evaluation dated 9/27/24 for R166 documented the use of grab bar currently for bed mobility or support. The evaluation documented in part, Has the resident expressed the desire to have an assist device on their bed? No . The evaluation failed to evidence review of risk and benefits, use of alternative prior to bed rail installation and consent for use.
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1. RN #1 stated that bed rails were included in the admission process and that during the nursing admission assessment they determined if the resident were going to use the bed rails to turn and reposition themselves. He stated that he did not recall if there was an option for alternate devices prior to the bed rails or not. He stated that they did assess for the risk of entrapment during the admission assessment, and he believed that in the bed evaluation there was a risk and benefit and consent.
On 10/7/24 at 5:00 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
3. For Resident #187 (R187), the facility staff failed to evidence a consent for the use of bed rails, alternatives attempted prior to installing bed rails, and review of the risks and benefits of bed rails prior to installation.
On the most recent MDS (minimum data set) assessment, an admission assessment, with an assessment reference date of 9/4/24, the resident scored 3 out of 15 on the BIMS (brief interview for mental status) assessment, indicating they were severely impaired for making daily decisions. The resident was coded as being dependent for bed mobility and transfers.
On 10/1/24 at 9:02 a.m., an observation was made of R187 in bed with bilateral bar shaped bed rails in place.
An additional observation of R187 in the bed with the bilateral bar shaped bed rails in place were made on 10/1/24 at 1:14 p.m. and 10/2/24 at 8:14 a.m.
The physician orders for R187 failed to evidence an order for the bed rails.
The comprehensive care plan for R187 failed to evidence the use of bed rails.
The admission assessment for R187 dated 8/29/24 failed to evidence the use of bed rails.
A bed safety evaluation dated 8/29/24 for R187 documented the resident not capable of decision making and use of grab bar currently for bed mobility or support. The evaluation documented in part, Has the resident expressed the desire to have an assist device on their bed? No . The evaluation failed to evidence review of risk and benefits, use of alternative prior to bed rail installation and consent for use.
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1. RN #1 stated that bed rails were included in the admission process and that during the nursing admission assessment they determined if the resident were going to use the bed rails to turn and reposition themselves. He stated that he did not recall if there was an option for alternate devices prior to the bed rails or not. He stated that they did assess for the risk of entrapment during the admission assessment, and he believed that in the bed evaluation there was a risk and benefit and consent.
On 10/7/24 at 5:00 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
4. For Resident #221 (R221), the facility staff failed to evidence a consent for the use of bed rails, alternatives attempted prior to installing bed rails, and review of the risks and benefits of bed rails prior to installation.
On the most recent MDS (minimum data set) assessment, an admission assessment, with an assessment reference date of 12/20/22, the resident scored 15 out of 15 on the BIMS (brief interview for mental status) assessment, indicating they were cognitively intact for making daily decisions. The resident was coded as requiring limited assistance for bed mobility and independent with transfers.
The progress notes for R221 documented in part, 12/15/2022 17:29 (5:29 p.m.) admission note .Requires Grab bar(s) . The progress notes failed to evidence review of risk and benefits, use of alternative prior to bed rail installation and consent for use.
The physician orders for R221 failed to evidence an order for the bed rails.
The comprehensive care plan for R221 failed to evidence the use of bed rails.
The admission assessment for R221 dated 12/15/22 documented the resident verbalizing/demonstrating the use of side rails/helping handles/grab bars and using bed assist bars. The assessment failed to evidence review of risk and benefits, use of alternative prior to bed rail installation and consent for use.
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1. RN #1 stated that bed rails were included in the admission process and that during the nursing admission assessment they determined if the resident were going to use the bed rails to turn and reposition themselves. He stated that he did not recall if there was an option for alternate devices prior to the bed rails or not. He stated that they did assess for the risk of entrapment during the admission assessment, and he believed that in the bed evaluation there was a risk and benefit and consent.
On 10/9/24 at approximately 6:15 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
Based on observation, staff interview, facility document review, and clinical record review, the facility staff failed to implement bed rail requirements for four of 63 residents in the survey sample, Residents #48, #166, #187, and #221.
The findings include:
1. For Resident #48 (R48), the facility staff failed to attempt alternatives prior to bed rail use, assess the resident for risk of entrapment, review the risks and benefits of bed rails with the resident or resident representative, and obtain informed consent.
A review of R48's clinical record revealed an admission evaluation dated 5/24/22 that failed to document information regarding bed rails. A bed safety evaluation dated 8/26/24 documented, 7. Has the resident expressed the desire to have an assist device on their bed? No. A review of physician's orders for October 2024 failed to reveal an order for bed rails.
On 10/1/24 at 12:05 p.m., R48 was observed lying in bed with bilateral grab bars (bed rails) in the upright position.
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1. RN #1 stated he did not recall that staff assess residents for appropriate alternatives prior the use of bed rails. RN #1 stated an assessment for risk of entrapment, education regarding the risks of benefits and benefits of bed rails and obtaining informed consent should be done during the admission process and documented on the admission assessment.
On 10/4/24 at 11:41 a.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
The facility policy titled, Safe Use of Bed Rails documented,
Procedure:
1. Assessment of residents with bed rails include:
a. Level of independence with bed mobility
b. Review of prior interventions and outcomes prior to the initiation of bed rails
c. Medical diagnosis, conditions, symptoms, and/or behavioral symptoms should be
evaluated prior to initiation
d. Bed meets manufacturer's recommendations and specifications pertaining to resident's
height and weight.
2. Consent
a. Disclosure of the needs, risk and benefits of use
b. Education provided to the resident or resident representative
c. Signed by the resident or, if applicable, the resident representative.
No further information was presented prior to exit.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0712
(Tag F0712)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #164 (R164), the facility staff failed to provide timely physician visits.
R164 was admitted to the facility on ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #164 (R164), the facility staff failed to provide timely physician visits.
R164 was admitted to the facility on [DATE].
On the most recent MDS (minimum data set), a quarterly assessment with an ARD (assessment reference date) of 8/24/24, the resident scored 15 out of 15 on the BIMS (brief interview for mental status) assessment, indicating that they were cognitively intact for making daily decisions.
On 10/1/24 at 8:24 a.m., an interview was conducted with R164 who stated that they had been at the facility for about nine months and had a good relationship with the nurse practitioner who they saw often. R164 stated that they rarely saw the physician and had not seen him in months now.
Review of the clinical record for R164 documented physician visits 11/15/23, 2/22/24 and 8/15/24.
On 10/7/24 at 2:59 p.m., an interview was conducted with ASM (administrative staff member) #7, physician. ASM #7 stated that he tries to see residents every 60 days.
On 10/9/24 at 9:00 a.m., and interview was conducted with ASM #2, the director of nursing. ASM #2 stated the medical records employee is responsible for tracking physician visits and notifying the physicians of a need for visits.
On 10/9/24 at approximately 6:15 p.m., ASM #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.4. For Resident #155 (R155), the facility staff failed to provide physician visits between his admission on [DATE] and 4/16/24 (371 days).
A review of R155's clinical record revealed he was admitted on [DATE], but was not seen by a physician until 4/16/35, a total of 371 days later.
On 10/7/24 at 2:59 p.m., ASM (administrative staff member) #7, the physician, was interviewed. ASM #7 stated he tries to see residents every 60 days.
On 10/9/24 at 9:00 a.m., ASM #2, the director of nursing, was interviewed. ASM #2 stated the medical records employee is responsible for tracking physician visits and notifying the physicians of a need for visits.
On 10/5/24 at 6:17 p.m., ASM #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
No further information was provided prior to exit.
3. For Resident #48 (R48), the facility staff failed to ensure the resident was seen by a physician between 1/4/24 and 5/23/24 (a total of 140 days).
A review of R48's clinical record revealed the resident was seen by a physician on 1/4/24. Further review of R48's clinical record revealed the resident was seen by a nurse practitioner on multiple dates but was not seen by a physician again until 5/23/24 (a total of 140 days).
On 10/7/24 at 2:59 p.m., an interview was conducted with ASM (administrative staff member) #7 (the physician). ASM #7 stated he tries to see residents every 60 days.
On 10/8/24 at 6:25 p.m., ASM #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
On 10/9/24 at 9:00 a.m., ASM #2 stated the medical records employee is responsible for tracking physician visits and notifying the physicians of a need for visits.
No further information was presented prior to exit.
Based on staff interview, facility document review and clinical record review, it was determined the facility staff failed to make required physician visits for four of 63 residents in the survey sample, Residents #52, #164, #48, and #155.
The findings include:
1. For Resident #52, the facility staff failed to ensure the physician made the required visits.
Review of the clinical record failed to evidence the physician did any required visits since 3/21/24.
On 10/7/24 at 2:59 p.m., an interview was conducted with ASM (administrative staff member) #7, the physician. ASM #7 stated he tries to see residents every 60 days.
On 10/9/24 at 9:00 a.m., and interview was conducted with ASM #2, the director of nursing. ASM #2 stated the medical records employee is responsible for tracking physician visits and notifying the physicians of a need for visits.
The facility policy, Physician Visit Logs documented in part, Policy: It is the policy of this facility to maintain a system to monitor physician's visits for all in-house residents to ascertain routine visits are conducted as outlined in state and federal regulations. The physician visit log may be maintained manually or electronically. Procedure: 1. The clinical records coordinator will maintain the Physician's Visit Log. 2. The Physician's Visit Log will be maintained in the electronic record. 3. The date of each physician's visit will be recorded and updated in the E MAR .5. If the resident is on an alternate visitation schedule, the clinical records coordinator will monitor and follow up on visits as follows: a. If the physician fails to visit within 50 days of the last visit, the clinical records coordinator will notify the physician by telephone that the visit is now due within the next 10 days and document the notification on a notification log. b. If the physician fails to visit within 60 days of the last visit, the clinical records coordinator will notify the physician by telephone that the visit is due and document the notification on the log. c. Notify the Executive Director and director of nursing services, in writing, that the physicians visit is overdue and include the physician's name, date of last visit, resident's name and Medical record number. Request administrative intervention such as a letter or phone call to the physician, medical director and the resident or resident's representative. d. Repeat this step weekly until the physician visits, there is a change of physician, or a physician has assumed care for this resident.
ASM #1, the executive director, ASM #2, and ASM # 5, the regional director of operations, were made aware of the above findings on 10/8/24 at 6:15 p.m.
No further information was obtained prior to exit.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Laboratory Services
(Tag F0770)
Could have caused harm · This affected multiple residents
2. For Resident #74 (R74), the facility staff failed to obtain laboratory testing as ordered.
The physician orders for R74 documented in part, TSH (thyroid stimulating hormone) every 6 month in Decemb...
Read full inspector narrative →
2. For Resident #74 (R74), the facility staff failed to obtain laboratory testing as ordered.
The physician orders for R74 documented in part, TSH (thyroid stimulating hormone) every 6 month in December and June on 15 every night shift every 6 month(s) starting on the 15th for 168 day(s). Order Date: 07/24/2023. Start Date: 12/14/2023. End Date: 01/17/2024.
The eTAR (electronic treatment administration record) for R74 dated 12/1/23-12/31/23 documented the TSH scheduled beginning on 12/15/23.
The comprehensive care plan for R74 documented in part, Parkinsons: [Name of R74] has Parkinsons. Date Initiated: 06/15/2024. Under Interventions/Tasks it documented in part, .Obtain and monitor lab/diagnostic studies, as ordered. Report abnormal findings to medical provider, resident and resident representative. Date Initiated: 06/15/2022 .
Review of the clinical record failed to evidence results for a TSH completed on 12/15/23. The progress notes failed to evidence the resident refusing the laboratory testing or documentation of the laboratory testing completed as ordered in December of 2023.
On 10/7/24 at approximately 5:00 p.m., a request was made to ASM (administrative staff member) #1, the executive director, for evidence of the TSH ordered for 12/15/23 for R74.
On 10/8/24 at 9:28 a.m., an interview was conducted with LPN (licensed practical nurse) #3. LPN #3 stated that they had an outside lab company that came in to draw labs. She stated that the technician came in during the week early in the morning and was given a printout of the residents who were scheduled for lab testing. She stated that the nurse and the technician signed the forms, and they drew the labs. She stated that if there were any issues getting the specimen the technician let the nurse know and they called the physician and attempted on the next lab draw day.
On 10/8/24 at 1:08 p.m., an interview was conducted with LPN #8. LPN #8 stated that the night nurse printed out all lab orders from the medical records and flagged them for the lab technician who came in early in the morning. She stated that the labs were normally done before she arrived for the day shift, so she watched for the results to come into the medical record during the day. She stated that the labs that were scheduled triggered on the eMAR or eTAR showing that they needed to be done.
On 10/9/24 at approximately 6:15 p.m., ASM #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
Based on staff interview, facility document review, and clinical record review, the facility staff failed to perform laboratory tests as ordered by the physician/provider for two of 63 residents in the survey sample, Residents #130 and #74.
The findings include:
1. For Resident #130, the facility staff failed to perform Hemoglobin A1C (test to measure long term blood sugar levels), lipid, and CMP (comprehensive metabolic panel) laboratory tests for multiple months in 2023.
A review of R130's orders revealed, in part:
4/3/23 Hemoglobin A1C every three months.
8/11/23 HgbA1c, CMP One time.
A review R130's of laboratory results for 2023 revealed no Hemoglobin A1C results between 4/1/23 and 12/2/23. This review revealed no CMP between 8/11/23 and 12/2/23.
On 10/8/24 at 1:08 p.m., LPN (licensed practical nurse) #8 was interviewed. She stated the night nurses are responsible for acknowledging when the EMR (electronic medical record) generates a reminder for a resident lab test. The night nurses print out the laboratory orders and put these in a book. When the outside laboratory company staff arrive at the facility to draw residents' blood, they perform the tests according to the orders in their book on each unit. She stated laboratory tests show up on either the MAR (medication administration record) or TAR (treatment administration record) as needing to be done. She stated the night nurse on each unit provides a list of lab tests that have been done to the day nurse, and the day nurse is responsible for looking for the results.
On 10/8/24 at 2:27 p.m., LPN #3, a unit manager, was interviewed. She stated the night shift nurses produce the orders and lab slips for the laboratory staff.
On 10/5/24 at 6:17 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, and ASM #5, the regional director of operations, were informed of these concerns.
A review of the facility policy, Laboratory and Radiological Services and Results Reporting, revealed, in part: The facility is responsible for the quality and timeliness of services whether services are provided by the facility or an outside resource .There are clinical and physiological risks when laboratory .services are not performed in a timely manner.
No further information was provided prior to exit.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0909
(Tag F0909)
Could have caused harm · This affected multiple residents
2. For Resident #166 (R166), the facility staff failed to conduct an inspection of the resident's bed rails to identify areas of possible entrapment.
On the most recent MDS (minimum data set) assessme...
Read full inspector narrative →
2. For Resident #166 (R166), the facility staff failed to conduct an inspection of the resident's bed rails to identify areas of possible entrapment.
On the most recent MDS (minimum data set) assessment, an annual assessment, with an assessment reference date of 6/3/24, the resident scored 15 out of 15 on the BIMS (brief interview for mental status) assessment, indicating they were cognitively intact for making daily decisions. The resident was coded as requiring set up assistance with bed mobility and dependent for transfers.
On 10/1/24 at 8:44 a.m., an observation was made of R166 in bed with bilateral bar shaped bed rails in place. At that time, an interview was conducted with R166 who stated that they grabbed on the bar when turning in the bed. R166 stated that the bed had always that the bars on it and they used them and had never used anything else.
An additional observation of R166 in the bed with the bilateral bar shaped bed rails in place were made on 10/1/24 at 2:18 p.m. and 10/2/24 at 8:10 a.m.
The admission assessment for R166 dated 9/27/24 failed to evidence the use of bed rails.
A bed safety evaluation dated 9/27/24 for R166 documented the use of grab bar currently for bed mobility or support. The evaluation documented in part, Has the resident expressed the desire to have an assist device on their bed? No . The evaluation failed to evidence inspection of the resident's bed rails to identify areas of possible entrapment.
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1. RN #1 stated that an assessment for risk of entrapment should be done during the admission process and documented on the admission assessment.
On 10/8/24 at 9:16 a.m., an interview was conducted with OSM (other staff member) #9, maintenance director. OSM #9 stated he tested the beds every year to make sure they were functional, and the electrical components were working. OSM #9 stated the facility used quarter bed rails and grab bars, so it didn't seem like there was a risk of entrapment and he did not complete a formal assessment to identify areas of possible entrapment.
On 10/7/24 at 5:00 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
3. For Resident #187 (R187), the facility staff failed to conduct an inspection of the resident's bed rails to identify areas of possible entrapment.
On the most recent MDS (minimum data set) assessment, an admission assessment, with an assessment reference date of 9/4/24, the resident scored 3 out of 15 on the BIMS (brief interview for mental status) assessment, indicating they were severely impaired for making daily decisions. The resident was coded as being dependent for bed mobility and transfers.
On 10/1/24 at 9:02 a.m., an observation was made of R187 in bed with bilateral bar shaped bed rails in place.
An additional observation of R187 in the bed with the bilateral bar shaped bed rails in place were made on 10/1/24 at 1:14 p.m. and 10/2/24 at 8:14 a.m.
The admission assessment for R187 dated 8/29/24 failed to evidence the use of bed rails.
A bed safety evaluation dated 8/29/24 for R187 documented the resident not capable of decision making and use of grab bar currently for bed mobility or support. The evaluation documented in part, Has the resident expressed the desire to have an assist device on their bed? No . The evaluation failed to evidence inspection of the resident's bed rails to identify areas of possible entrapment.
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1. RN #1 stated that an assessment for risk of entrapment should be done during the admission process and documented on the admission assessment.
On 10/8/24 at 9:16 a.m., an interview was conducted with OSM (other staff member) #9, maintenance director. OSM #9 stated he tested the beds every year to make sure they were functional, and the electrical components were working. OSM #9 stated the facility used quarter bed rails and grab bars, so it didn't seem like there was a risk of entrapment and he did not complete a formal assessment to identify areas of possible entrapment.
On 10/7/24 at 5:00 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
4. For Resident #221 (R221), the facility staff failed to conduct an inspection of the resident's bed rails to identify areas of possible entrapment.
On the most recent MDS (minimum data set) assessment, an admission assessment, with an assessment reference date of 12/20/22, the resident scored 15 out of 15 on the BIMS (brief interview for mental status) assessment, indicating they were cognitively intact for making daily decisions. The resident was coded as requiring limited assistance for bed mobility and independent with transfers.
The progress notes for R221 documented in part, 12/15/2022 17:29 (5:29 p.m.) admission note .Requires Grab bar(s) . The progress notes failed to evidence inspection of the resident's bed rails to identify areas of possible entrapment.
The admission assessment for R221 dated 12/15/22 documented the resident verbalizing/demonstrating the use of side rails/helping handles/grab bars and using bed assist bars. The assessment failed to evidence inspection of the resident's bed rails to identify areas of possible entrapment.
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1. RN #1 stated that an assessment for risk of entrapment should be done during the admission process and documented on the admission assessment.
On 10/8/24 at 9:16 a.m., an interview was conducted with OSM (other staff member) #9, maintenance director. OSM #9 stated he tested the beds every year to make sure they were functional, and the electrical components were working. OSM #9 stated the facility used quarter bed rails and grab bars, so it didn't seem like there was a risk of entrapment and he did not complete a formal assessment to identify areas of possible entrapment.
On 10/9/24 at approximately 6:15 p.m., ASM (administrative staff member) #1, the executive director, ASM #2, the director of nursing and ASM #5, the regional director of operations were made aware of the findings.
No further information was provided prior to exit.
Based on observation, staff interview, facility staff interview, and clinical record review, the facility staff failed to conduct required bed inspections for four of 63 residents in the survey sample, Residents #48, #166, #187, and #221.
The findings include:
1. For Resident #48 (R48), the facility staff failed to conduct an inspection of the resident's bed rails to identify areas of possible entrapment.
A review of R48's clinical record revealed an admission evaluation dated 5/24/22 that failed to document information regarding bed rails. A bed safety evaluation dated 8/26/24 documented, 7. Has the resident expressed the desire to have an assist device on their bed? No. Further review of R48's clinical record failed to reveal an inspection of the resident's bed rails to identify areas of possible entrapment.
On 10/1/24 at 12:05 p.m., R48 was observed lying in bed with bilateral grab bars (bed rails) in the upright position
On 10/3/24 at 5:23 p.m., an interview was conducted with RN (registered nurse) #1. RN #1 stated an assessment for risk of entrapment should be done during the admission process and documented on the admission assessment.
On 10/8/24 at 9:16 a.m., an interview was conducted with OSM (other staff member) #9 (the maintenance director). OSM #9 stated he tests the beds every year to make sure they are functional, and the electrical components are working. OSM #9 stated the facility uses quarter bed rails and grab bars, so it doesn't seem like there is a risk of entrapment and he does not complete a formal assessment to identify areas of possible entrapment.
On 10/8/24 at 6:25 p.m., ASM (administrative staff member) #1 (the executive director) and ASM #2 (the director of nursing) were made aware of the above concern.
The facility policy titled, Safe Use of Bed Rails documented, 6. Documentation .b. Completion of Bed Safety Evaluation.
No further information was presented prior to exit.