HARRISONBURG HLTH & REHAB CNTR



Over 2 years since last inspection. Current conditions may differ from available data.
Harrisonburg Health & Rehab Center has received a Trust Grade of F, indicating significant concerns and a poor overall assessment of care. They rank #193 out of 285 nursing homes in Virginia, placing them in the bottom half, and #3 out of 3 in Harrisonburg City County, meaning there is only one other facility in the area that performs better. The facility is worsening, with the number of issues increasing from 4 in 2024 to 21 in 2025. Staffing is a major weakness, rated at only 1 out of 5 stars with a high turnover rate of 61%, which is concerning compared to the Virginia average of 48%. Additionally, they have incurred $116,624 in fines, indicating compliance issues that are more frequent than 93% of other facilities in the state. The RN coverage is also below average, with less than 94% of state facilities, which may hinder the ability to catch potential problems early. Specific incidents include a resident who ingested body wash and required hospitalization, and another resident left sitting in feces for fifty minutes due to staff neglect, both resulting in significant harm. Overall, while there are some positive quality measures, serious staffing and safety issues are evident, making this facility a concerning choice for families.
- Trust Score
- F
- In Virginia
- #193/285
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 61% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $116,624 in fines. Lower than most Virginia facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 15 minutes of Registered Nurse (RN) attention daily — below average for Virginia. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 78 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Virginia average (3.0)
Below average - review inspection findings carefully
15pts above Virginia avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Significant penalties indicating serious issues
Part of a multi-facility chain
Ask about local staffing decisions and management
13 points above Virginia average of 48%
The Ugly 78 deficiencies on record
Jun 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected 1 resident
Based on observation, resident interview, staff interview, and facility documentation review, the facility staff failed to provide a safe, functional and comfortable environment for one resident (Resi...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on resident interview, staff interview, clinical record review, and facility documentation review, the facility staff failed to have medications available for administration for one resident (re...
Read full inspector narrative →
Apr 2025
19 deficiencies
2 IJ (1 affecting multiple)
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Free from Abuse/Neglect
(Tag F0600)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #10 (R10), the facility staff neglected to respond to the residents call for assistance to have incontinence car...
Read full inspector narrative →
CRITICAL
(K)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, clinical record review and facility documentation review, the facility staff failed to pr...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Incontinence Care
(Tag F0690)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. For Resident #10 (R10), who suffered from quadriplegia and was totally dependent upon facility staff, the facility staff fail...
Read full inspector narrative →
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Deficiency F0692
(Tag F0692)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident interview, staff interview, clinical record review, and facility documentation review, the facili...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on the facility documentation and staff interview the facility staff failed to implement abuse policy regarding reporting to the Department of Health Professionals (DHP) for two residents (Resid...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on the facility documentation and staff interviews, the facility staff failed to report an allegation of abuse and neglect timely for two residents (Resident #17 and Resident #23) out of a surve...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #12 (R12) who was presumed to have ingested a body wash, which resulted in hospitalization, the facility staff f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, clinical record review and facility documentation review, the facility staff failed to re...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
ADL Care
(Tag F0677)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interviews, clinical reviews and facility documents, the facility staff failed to provide activity of daily livin...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
Based on resident interview, clinical record review, and facility documentation review, the facility staff failed to administer medications as ordered by the physician for one resident (Resident #8-R8...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. For Resident #12 (R12), the facility staff failed to accurately complete a hot liquid safety evaluation.
On 4/7/25 a closed ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0943
(Tag F0943)
Could have caused harm · This affected 1 resident
Based on staff interviews and facility documentation the facility staff failed to ensure staff had abuse training for two certified nursing assistants, CNA#11 (CNA11) and CNA#12 (CNA12) out of eight e...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0945
(Tag F0945)
Could have caused harm · This affected 1 resident
Based on staff interviews and facility documentation the facility staff failed to provide infection control training for two certified nursing assistants, CNA#11 (CNA11) and CNA#12 (CNA12) out of eigh...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, resident and staff interview and facility documentation review, the facility staff failed to provide a comfortable environment with internal temperatures affecting two of three u...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
Based on resident interview, clinical record review and facility documentation review, the facility staff failed to ensure medications were available for administration in accordance with physician or...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation and staff interviews, the facility staff failed to follow infection control standards on three of three units.
The findings included:
The facility staff failed to handle soiled li...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
2. In a resident room on west wing the facility staff failed to clean the bathroom to remove brownish/black substances from the wall and trashcan.
On 4/3/25 at 9:38 a.m., during observations within t...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0949
(Tag F0949)
Could have caused harm · This affected multiple residents
Based on staff interviews, staff record review and facility documentation review, the facility staff failed to provide behavioral health training to five of eight employees.
The findings included:
Fo...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0925
(Tag F0925)
Could have caused harm · This affected most or all residents
Based on observation, staff interviews and facility documents, the facility staff failed to maintain an effective pest control program that affected three of three units.
The findings included:
The fa...
Read full inspector narrative →
Jul 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on observation, resident interviews, and staff interviews, the facility staff failed to provide appetizing food with palatable temperatures and appearance to residents on one of three units (Wes...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, staff interviews, resident interviews, and facility documents, the facility staff failed to ensure a sani...
Read full inspector narrative →
Jan 2024
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview and clinical record review, the facility failed to develop a care plan for one of two residents. Reside...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0699
(Tag F0699)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview and clinical record review, the facility failed initiate trauma informed care for one of two residents....
Read full inspector narrative →
Aug 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0773
(Tag F0773)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, facility document review, and clinical record review, the facility staff failed to promptly notify the...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident interview, staff interview, facility document review, and clinical record review, the facility staff failed to...
Read full inspector narrative →
Nov 2022
10 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
Based on resident interview, staff interview, facility document review, clinical record review and complaint investigation, the facility staff failed to protect the residents' right to be free from se...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident interview, staff interview, facility document review, clinical record review and complaint investigation, the ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident interview, staff interview, facility document review, clinical record review and complaint investigation, the ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review and staff interview during a complaint investigation, the facility staff failed to follow physic...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0694
(Tag F0694)
Could have caused harm · This affected 1 resident
Based on staff interview, clinical record review, and in the course of a complaint investigation, the facility staff failed to provide care to a PICC (peripherally inserted central catheter) line per ...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0745
(Tag F0745)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident interview, staff interview, facility document review, clinical record review and complaint investigation, the ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident interview, staff interview, facility document review, clinical record review and complaint investigation, the ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, and clinical record review, the facility staff failed to incorporate and follow Level II ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, resident interview, and clinical record review, the facility staff failed to implement in...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, resident interview, and clinical record review, the facility staff failed to ensure behav...
Read full inspector narrative →
May 2022
16 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0583
(Tag F0583)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, and clinical record review, the facility staff failed to ensure one of 38 residents had privacy while in his room, Resident #38. Resident #38 who resided in a pr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview and clinical record review, the facility staff failed to ensure an accurate assessment for two of 38 re...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on clinical record review and staff interview, the facility staff failed to ensure one of 38 residents were free from acci...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, facility document review and clinical record review, the facility staff failed to respond to pharmacy ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on medication pass and pour observation, staff interview, clinical record review, and facility document review, the facility staff failed to ensure a medication error rate less than 5 percent. T...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and staff interview, the facility staff failed to ensure expired medication was not available for administr...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interviews, clinical record review and facility document review, the facility staff failed to ensure records of w...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0567
(Tag F0567)
Could have caused harm · This affected multiple residents
Based on group interview, staff interview, and facility document review, the facility staff failed to ensure residents had unlimited access to petty cash funds during the week and on weekends for four...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
PASARR Coordination
(Tag F0644)
Could have caused harm · This affected multiple residents
Based on observation, staff interview, and clinical record review, the facility staff failed to incorporate and follow Level II PASARR recommendations for one of 38 residents, Resident #38.
Findings ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3.a. Resident # 322 was admitted to the facility with diagnoses to include, but were not limited to: acute respiratory failure, ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0740
(Tag F0740)
Could have caused harm · This affected multiple residents
Based on observation, staff interview, and clinical record review, the facility staff failed to ensure behavioral health services were provided to maintain his highest practicable level of well being ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #121 was admitted with diagnoses which included: Parkinson's disease, COPD , depression, bipolar disorder, dementia,...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0760
(Tag F0760)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident interview, clinical record review, and staff interview, the facility staff failed to ensure one of 38 resident...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0800
(Tag F0800)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, and group interview, the facility staff failed to provide condiments, menu items, and hon...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview and clinical record review, the facility staff failed to ensure a complete and accurate cl...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0576
(Tag F0576)
Minor procedural issue · This affected most or all residents
Based on group interview and staff interview, the facility staff failed to ensure resident mail was delivered on weekends. This facility census was 159 residents.
Findings include:
On 5/25/22 at 10:00...
Read full inspector narrative →
Apr 2021
8 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, clinical record review, facility document review, and in the course of a complaint investigation, the ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, clinical record review, facility document review and in the course of a complaint investigation, the f...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, clinical record review, and facility document review, the facility staff failed to develop a baseline ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, clinical record review and in the course of a complaint investigation, the facility staff...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0658
(Tag F0658)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview, facility document review, and clinical record review, the facility staff failed to follow professional...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview and clinical record review the facility staff failed to provide a complete and accurate cl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident interview, resident council interview and staff interview, the facility staff failed to respond to call bells ...
Read full inspector narrative →
MINOR
(B)
Minor Issue - procedural, no safety impact
Room Equipment
(Tag F0908)
Minor procedural issue · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, and facility document review, the facility failed to ensure thermometers used for checkin...
Read full inspector narrative →
May 2019
17 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on resident interview and group interview, the facility staff failed to provide a dignified dining experience on the eveni...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview and resident interview, the facility staff failed to ensure a clean, safe, comfortable, ho...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, family interview, resident interview, staff interview, facility document review and clinical record review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, family interview, resident interview, staff interview, facility document review and clinical record review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, family interview, resident interview, staff interview, facility document review and clinical record review...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0655
(Tag F0655)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview and clinical record review, the facility staff failed to develop a baseline care that incl...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, and clinical record review the facility staff failed to provide foot care for two of 38 r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #62 was admitted to the facility on [DATE] with most recent readmission on [DATE]. Diagnoses for Resident #62 includ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident interview, staff interview, facility document review, and clinical record review, facility staff ...
Read full inspector narrative →
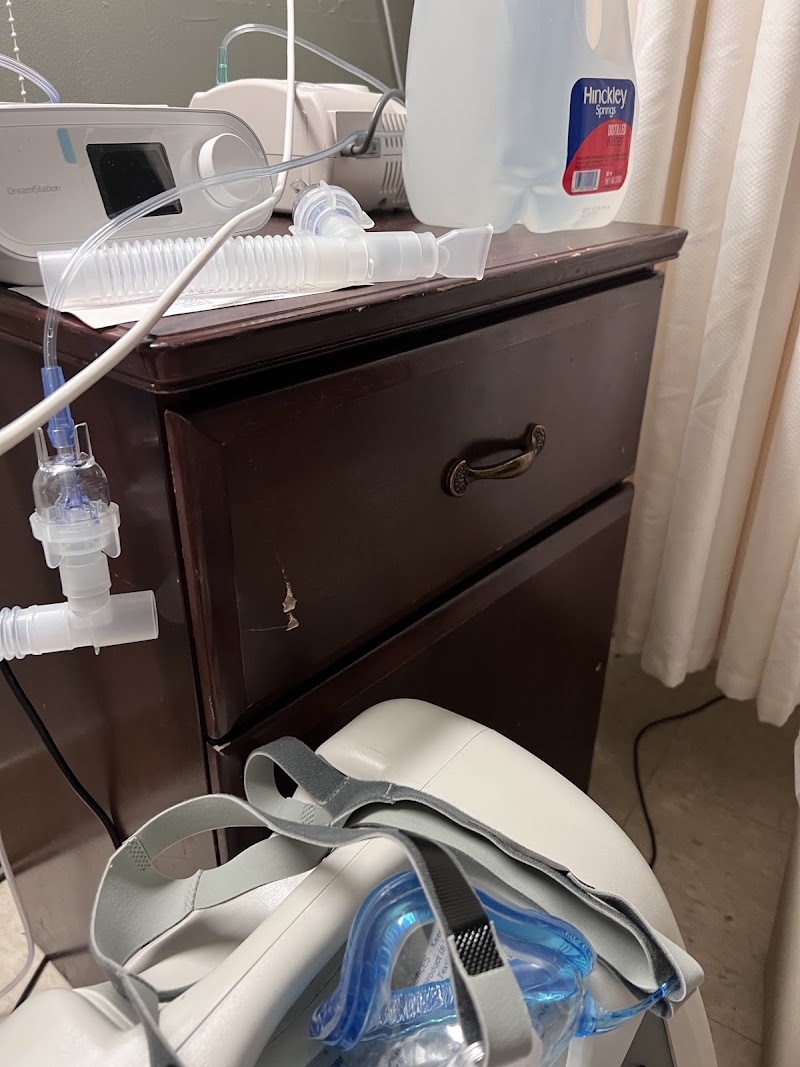
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview and clinical record review, the facility staff failed to ensure oxygen was administered as...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview and clinical record review, the facility staff failed to ensure one of 38 residents was not prescribed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0883
(Tag F0883)
Could have caused harm · This affected 1 resident
Based on staff interview and clinical record review, the facility staff failed to ensure one of 5 resident records reviewed was complete for the influenza vaccine: Resident # 62.
Findings include:
Res...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview and clinical record review, the facility staff failed to review and revise a comprehensive...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Resident #124 was admitted to the facility on [DATE]. Diagnoses for Resident #124 included; Fracture of left femur, atrial fi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0725
(Tag F0725)
Could have caused harm · This affected multiple residents
Based on resident interview, family interview, a resident group interview and staff interview, the facility staff failed to respond to call bells in a timely manner. Residents, the resident council gr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on staff interview and clinical record review, the facility staff failed to ensure one of 38 residents were free of an unn...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Resident #120 was admitted to the facility on [DATE] with diagnoses including, but not limited to: Diabetes, Peripheral Vascu...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "What safeguards are in place to prevent abuse and neglect?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: Federal abuse finding, 2 life-threatening violation(s), 3 harm violation(s), $116,624 in fines. Review inspection reports carefully.
- • 78 deficiencies on record, including 2 critical (life-threatening) violations. These warrant careful review before choosing this facility.
- • $116,624 in fines. Extremely high, among the most fined facilities in Virginia. Major compliance failures.
- • Grade F (0/100). Below average facility with significant concerns.
About This Facility
What is Harrisonburg Hlth & Rehab Cntr's CMS Rating?
CMS assigns HARRISONBURG HLTH & REHAB CNTR an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Virginia, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Harrisonburg Hlth & Rehab Cntr Staffed?
CMS rates HARRISONBURG HLTH & REHAB CNTR's staffing level at 1 out of 5 stars, which is much below average compared to other nursing homes. Staff turnover is 61%, which is 15 percentage points above the Virginia average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at Harrisonburg Hlth & Rehab Cntr?
State health inspectors documented 78 deficiencies at HARRISONBURG HLTH & REHAB CNTR during 2019 to 2025. These included: 2 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 3 that caused actual resident harm, 71 with potential for harm, and 2 minor or isolated issues. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Harrisonburg Hlth & Rehab Cntr?
HARRISONBURG HLTH & REHAB CNTR is owned by a government entity. Government-operated facilities are typically run by state, county, or municipal agencies. The facility is operated by LIFEWORKS REHAB, a chain that manages multiple nursing homes. With 180 certified beds and approximately 156 residents (about 87% occupancy), it is a mid-sized facility located in HARRISONBURG, Virginia.
How Does Harrisonburg Hlth & Rehab Cntr Compare to Other Virginia Nursing Homes?
Compared to the 100 nursing homes in Virginia, HARRISONBURG HLTH & REHAB CNTR's overall rating (2 stars) is below the state average of 3.0, staff turnover (61%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Harrisonburg Hlth & Rehab Cntr?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "What safeguards and monitoring systems are in place to protect residents from abuse or neglect?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can you walk me through typical staffing levels on day, evening, and night shifts?" These questions are particularly relevant given the facility's Immediate Jeopardy citations, the substantiated abuse finding on record, the facility's high staff turnover rate, and the below-average staffing rating.
Is Harrisonburg Hlth & Rehab Cntr Safe?
Based on CMS inspection data, HARRISONBURG HLTH & REHAB CNTR has documented safety concerns. The facility has 1 substantiated abuse finding (meaning confirmed case of resident harm by staff or other residents). Inspectors have issued 2 Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Virginia. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Harrisonburg Hlth & Rehab Cntr Stick Around?
Staff turnover at HARRISONBURG HLTH & REHAB CNTR is high. At 61%, the facility is 15 percentage points above the Virginia average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Harrisonburg Hlth & Rehab Cntr Ever Fined?
HARRISONBURG HLTH & REHAB CNTR has been fined $116,624 across 1 penalty action. This is 3.4x the Virginia average of $34,245. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is Harrisonburg Hlth & Rehab Cntr on Any Federal Watch List?
HARRISONBURG HLTH & REHAB CNTR is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.