ASPIRE PHYSICAL RECOVERY CENTER AT CAHABA RIVER




Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
Aspire Physical Recovery Center at Cahaba River has received a Trust Grade of F, indicating significant concerns about their care and operations. Ranked #185 out of 223 facilities in Alabama, they fall in the bottom half, and #20 out of 34 in Jefferson County, suggesting limited local options for better care. The facility is worsening, with issues increasing from 6 in 2019 to 8 in 2024. Staffing is rated 4 out of 5 stars, which is a strength, but the turnover rate is concerning at 68%, significantly higher than the state average of 48%. Additionally, they have incurred $16,801 in fines, which is higher than 87% of Alabama facilities, indicating ongoing compliance problems. Specific incidents include a critical failure to honor a resident's Do Not Resuscitate order, where CPR was mistakenly administered against the resident's wishes. Another concern involved food being served at unappetizing temperatures, impacting many residents during meals. While the facility has some strengths in staffing, these serious deficiencies highlight significant weaknesses in care and operations that families should consider carefully.
- Trust Score
- F
- In Alabama
- #185/223
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 68% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ⚠ Watch
- $16,801 in fines. Higher than 99% of Alabama facilities. Major compliance failures.
- Skilled Nurses ✓ Good
- Each resident gets 57 minutes of Registered Nurse (RN) attention daily — more than average for Alabama. RNs are trained to catch health problems early.
- Violations ⚠ Watch
- 17 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
4-Star Staffing Rating · Above-average nurse staffing levels
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in staffing levels, fire safety.
The Bad
Below Alabama average (2.9)
Significant quality concerns identified by CMS
22pts above Alabama avg (46%)
Frequent staff changes - ask about care continuity
Below median ($33,413)
Minor penalties assessed
Part of a multi-facility chain
Ask about local staffing decisions and management
20 points above Alabama average of 48%
The Ugly 17 deficiencies on record
Jan 2024
8 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Deficiency F0578
(Tag F0578)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, Resident Identifier (RI) #264's medical record, FUNDAMENTALS OF NURSING NINTH EDITION, the facility's PROTO...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, residents' medical records, and the facility policy titled Federal Rights of Residents, the f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0553
(Tag F0553)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, record review, and the facility policy titled, Person Centered Care Plan, the facility failed to ensure Res...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0554
(Tag F0554)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, observations, resident's medical record, and the facility policy titled, . Self-Administration of Medicatio...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, observations, residents' medical records, and the facility policy titled, Person Centered Care Plans, the f...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, observation, residents' medical records, and the facility policy titled, Oxygen Administration, the facilit...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
Based on RI #215's medical record, interviews, facility pharmacy records titled CONSOLODATED DELIVERY SHEETS, and the facility policy titled, Ordering and Receiving Medications from Provider Pharmacy ...
Read full inspector narrative →
CONCERN
(F)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0804
(Tag F0804)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, medical records, and the facility policy titled Food Preparation Guidelines, the facility fai...
Read full inspector narrative →
Sept 2019
6 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Tube Feeding
(Tag F0693)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on the facility's policy titled, Tube Feeding-Formula Documentation, observation and interviews, the facility failed to en...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0806
(Tag F0806)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, resident tray tickets, medical record review, and a review of the facility's policies for Perso...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on a facility's policy titled, Isolation Food Trays, observation and interviews, the facility failed to ensure a disposabl...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Menu Adequacy
(Tag F0803)
Could have caused harm · This affected multiple residents
Based on observation, interview, the facility's Cycle Menus policy, the facility's Menu Changes policy, the facility's Menu Diet Guide Sheet, and the facility's Menu Measurement Conversion Factors, th...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation, interview, and the 2017 Food and Drug Administration (FDA) Food Code, the facility failed to ensure:
1.) the dishwasher drain pipe did not extend into the floor drain by one inc...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Garbage Disposal
(Tag F0814)
Could have caused harm · This affected most or all residents
Based on observation, interview, and the 2017 Food and Drug Administration (FDA) Food Code, the facility failed to ensure one of two dumpster's had the doors closed and further failed to ensure the ou...
Read full inspector narrative →
Aug 2018
3 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected 1 resident
Based on review of SNF (Skilled Nursing Facility) Beneficiary Protection Notices and interview, the facility failed to ensure Resident Identifiers (RI) #44 and RI #47 were issued a Medicare Coverage/L...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation and interviews, the facility failed to ensure a Licensed Practical Nurse (LPN) administered medications in a manner to prevent cross contamination. The LPN used a clip board fille...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observations, interviews and a facility policy titled, Cleaning of Miscellaneous Equipment and Utensils, the facility failed to ensure:
1. a heavy build up of what appeared to be burnt on foo...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s). Review inspection reports carefully.
- • 17 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $16,801 in fines. Above average for Alabama. Some compliance problems on record.
- • Grade F (26/100). Below average facility with significant concerns.
About This Facility
What is Aspire Physical Recovery Center At Cahaba River's CMS Rating?
CMS assigns ASPIRE PHYSICAL RECOVERY CENTER AT CAHABA RIVER an overall rating of 1 out of 5 stars, which is considered much below average nationally. Within Alabama, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is Aspire Physical Recovery Center At Cahaba River Staffed?
CMS rates ASPIRE PHYSICAL RECOVERY CENTER AT CAHABA RIVER's staffing level at 4 out of 5 stars, which is above average compared to other nursing homes. Staff turnover is 68%, which is 22 percentage points above the Alabama average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at Aspire Physical Recovery Center At Cahaba River?
State health inspectors documented 17 deficiencies at ASPIRE PHYSICAL RECOVERY CENTER AT CAHABA RIVER during 2018 to 2024. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death) and 16 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
Who Owns and Operates Aspire Physical Recovery Center At Cahaba River?
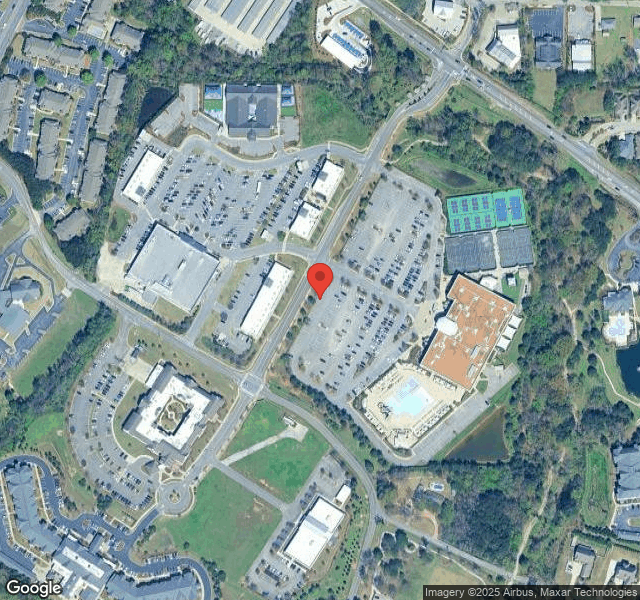
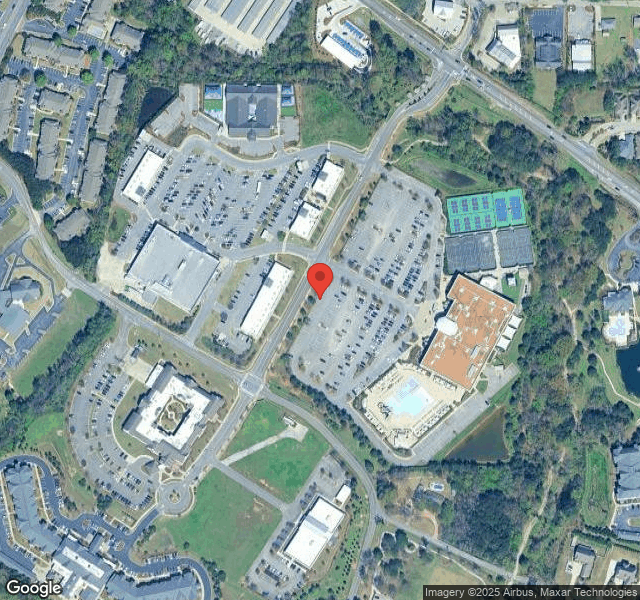
ASPIRE PHYSICAL RECOVERY CENTER AT CAHABA RIVER is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by NHS MANAGEMENT, a chain that manages multiple nursing homes. With 120 certified beds and approximately 112 residents (about 93% occupancy), it is a mid-sized facility located in VESTAVIA, Alabama.
How Does Aspire Physical Recovery Center At Cahaba River Compare to Other Alabama Nursing Homes?
Compared to the 100 nursing homes in Alabama, ASPIRE PHYSICAL RECOVERY CENTER AT CAHABA RIVER's overall rating (1 stars) is below the state average of 2.9, staff turnover (68%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting Aspire Physical Recovery Center At Cahaba River?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" These questions are particularly relevant given the facility's Immediate Jeopardy citations and the facility's high staff turnover rate.
Is Aspire Physical Recovery Center At Cahaba River Safe?
Based on CMS inspection data, ASPIRE PHYSICAL RECOVERY CENTER AT CAHABA RIVER has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 1-star overall rating and ranks #100 of 100 nursing homes in Alabama. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Aspire Physical Recovery Center At Cahaba River Stick Around?
Staff turnover at ASPIRE PHYSICAL RECOVERY CENTER AT CAHABA RIVER is high. At 68%, the facility is 22 percentage points above the Alabama average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was Aspire Physical Recovery Center At Cahaba River Ever Fined?
ASPIRE PHYSICAL RECOVERY CENTER AT CAHABA RIVER has been fined $16,801 across 1 penalty action. This is below the Alabama average of $33,247. While any fine indicates a compliance issue, fines under $50,000 are relatively common and typically reflect isolated problems that were subsequently corrected. Families should ask what specific issues led to these fines and confirm they've been resolved.
Is Aspire Physical Recovery Center At Cahaba River on Any Federal Watch List?
ASPIRE PHYSICAL RECOVERY CENTER AT CAHABA RIVER is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.