CRITICAL
(J)
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
Complaint, #NJ157771, #NJ157773, #NJ157831
Based on observations, interviews, record review, and review of other pertinent facility documentation, it was determined that on 09/21/22, the facility fail...
Read full inspector narrative →
Complaint, #NJ157771, #NJ157773, #NJ157831
Based on observations, interviews, record review, and review of other pertinent facility documentation, it was determined that on 09/21/22, the facility failed to ensure: a.) a resident with moderate cognitive impairment, who was at risk for elopement, and had a known history of wandering and exit seeking behavior was appropriately supervised and monitored to ensure safety, prevent elopement, or exiting of the building, and staff failed to follow their facility's policy and procedure on Wandering/Elopement.
This deficient practice was identified for one of five residents, (Resident #206) reviewed, who had moderate cognitive impairment, and were at risk for elopement. This placed Resident #206 as well as all other residents with moderate cognitive impairment, who were at risk for or had a known history of wandering and/or elopement in Immediate Jeopardy (IJ).
On 09/03/22, Resident #206 was able to exit the building unsupervised through an unlocked door at 10:12 AM, was found by the police, and subsequently expired on 09/03/22 at 4:19 PM. The IJ for Resident #206, occurred on 09/03/22, and was identified on 09/07/22 at 4:20 PM, when the Facility's Administrator (Admin) and the Director of Nursing (DON) were notified of the IJ situation. The survey team provided the facility with an IJ template on 09/07/22. The facility provided an acceptable Removal Plan (RP), on 09/08/22 at 10:16 AM to remove the immediacy.
The facility further failed to ensure: b.) staff provided a resident who was at risk for aspiration (when food, drink, or a foreign object is breathed into the lungs) with the correct liquid consistency to prevent aspiration pneumonia (an infection caused by a foreign substance entering the lungs), and staff failed to follow the facility's policy and procedure for the administration of thickened liquids. This deficient practice was identified for one of three residents, (Resident #191) reviewed for accidents related to mechanically altered diets. On 05/27/22, Resident #191 was provided with thin liquids when the resident had a physician's order for thickened liquids. This placed Resident #191 as well as all other residents who received a mechanically altered diet at risk for Immediate Jeopardy (IJ). The IJ for Resident #191 started on 05/27/22, and was identified by the survey team on 09/13/22. The survey team provided the facility with an IJ template on 09/13/22. The IJ was identified as past non-compliance from 05/27/22 through 05/31/22 when the facility provided the survey team with an acceptable Plan of Correction.
This deficient practice was further evidenced by the following:
Part A
The surveyor reviewed the medical record for Resident #206.
The surveyor reviewed the admission Record (AR), Resident #206 was admitted to the Facility with diagnoses which included but were not limited to: epilepsy, dementia, hyperlipidemia, hypothyroidism, protein-calorie malnutrition, atherosclerotic heart disease, injury of the head, anxiety disorder, mood disorder, anemia, depression, dysphasia, rhabdomyolysis, thrombocytopenia, and essential hypertension.
Review of the quarterly Minimum Data Set (MDS), an assessment tool dated 08/04/22, revealed that Resident #206 had a Brief Interview for Mental Status (BIMS) score of 8 out of 15, which indicated that Resident #206 had moderate cognitive impairment. Further review of the MDS in Section G for functional status, indicated that Resident #206 was independent with transfers, locomotion on the unit, and ambulation.
Review of the Care Plan (CP), with a documented resolved date of 03/29/22, revealed a focus area that Resident #206 was at risk for elopement due to wandering related to cognitive impairment, confusion, and dementia. The goal was that Resident #206 would not leave the facility unsupervised. The interventions included: to assess for change in behavior, to observe for unsafe behaviors, to provide with a program of activities that minimize the potential for wandering, wander guard in place left ankle, observe for placement, and proper functioning each shift. This CP was resolved and discontinued with the date of 03/29/22, which indicated that Resident #206 was no longer at risk for elopement.
Review of the Physician's Progress Note (PN) dated 8/2/2022 at 03:48 PM, revealed the resident was on the Psychotropic medication, Depakote 125 milligrams two times daily and had dementia with behavioral issues/wandering behavior with gait instability.
Review of the Medication Administration Record (MAR) dated 09/2022, revealed the nurses were monitoring Resident #206's behaviors to include; itching, picking at skin, restlessness, hitting, increase in complaints, biting, kicking, spitting, cussing, racial slurs, elopement, stealing, delusions, hallucinations, psychosis, aggression, and refusing care.
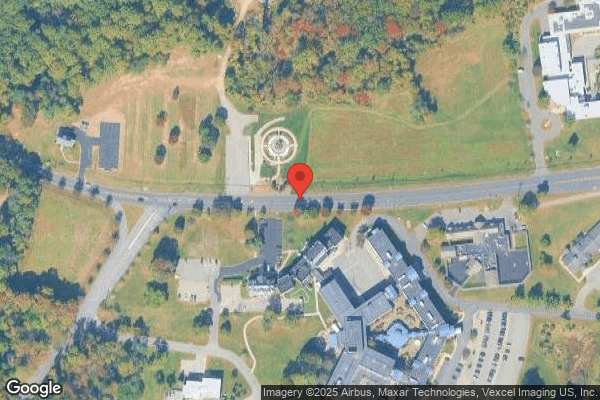
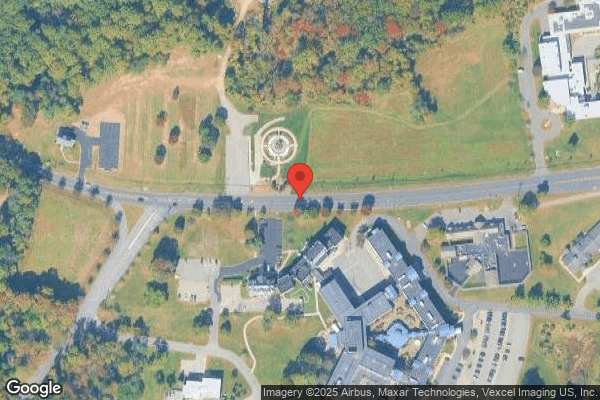
During a review of a Facility Reportable Event (FRE) form dated 09/05/22 at 09:13 AM, sent into NJ Department of Health (DOH) from the DON. On 09/03/22, the Certified Nursing Assistant (CNA #1) assigned to Resident #206 left unit 1A where he/she resided and went on break without giving report or asking someone to monitor their residents. During the break, Resident #206 was able to independently exit the facility unattended, without the staff's knowledge, through an unlocked door in unit 1D, and wandered off the facility grounds onto the main road. Resident #206 made it across the main road and was later found by police at 3:52 PM, laying on the ground at the 9/11 Memorial. The policeman immediately performed Cardiac Pulmonary Resuscitation (CPR) and Resident #206 was later reported to have expired at 4:16 PM.
The last time Resident #206 was observed within the facility was at 10:12 AM on video surveillance walking the hallway and exited through an unlocked door on unit 1D. The Licensed Practical Nurse/Unit Manager (LPN/UM #1) observed an empty wheelchair in the hallway of 1D which had a tag with Resident #206's name on it. This initiated a CODE GREY and all staff started a search of the interior of the facility then moved to the exterior of the facility. When Resident #206 was not found within the facility's grounds, the LPN/UM #2 initiated a call to the police at 12:14 PM on 09/03/22, to report Resident #206 missing. The facility searched for Resident #206, but was unaware of the whereabouts of Resident #206 until he/she was found by police on 09/03/22 at 03:52 PM.
On 09/06/22 at 11:53 AM, the surveyors observed Stairwell #4 on the 1st floor in the presence of the facility's Admin, Assistant Admin, and Maintenance Director (MD). The Admin stated this was the door that Resident #206 exited the facility from at approximately 10:10 AM on 09/03/22, and Resident #206 was not wearing a wander guard. The surveyors observed a horizontal metal bar on the top of the door and a keypad next to the door. The door was observed to be locked. The MD waved a tool by the keypad and an alarm sounded which indicated that the wander guard keypad system was functioning. The Admin stated the door was a delayed egress maglock and either the maglock system malfunctioned or the keypad itself malfunctioned when Resident #206 exited the building. The Admin told the surveyors that since Resident #206 exited the facility, the keypad, and the maglock were both replaced and were now, new. The surveyors exited the door that Resident #206 exited from and observed a parking lot with woods surrounding. The Admin told the surveyors that the office next to the door Resident #206 exited from was closed because it was a Saturday, and no cars were in the parking lot because no one was in the area that day. The Admin further stated that a Dietary Aide (DA) observed Resident #206 trying to open the patio door. Resident #206 had asked the DA to open the door and the DA stated that he/she could not open the door.
On 09/06/22 at 12:53 PM, the surveyors interviewed the DA, who stated that he/she worked at the facility since April 2022, and worked in the kitchen, the day Resident #206 left the facility. The DA stated that when he/she left the kitchen, it was to drop off and pick up meal trays. The DA stated that he/she had observed Resident #206 by the patio trying to open the door. Resident #206 asked the DA to open the door. The DA told Resident #206 that he/she could not, so the resident continued walking toward the unit. The DA told the surveyors that it was not the first time that DA had seen Resident #206 and had observed the resident on 1A when he/she dropped off the meal trays. The DA stated that he/she did not think it was an odd behavior for Resident #206 to ask the DA to open the door because he/she figured Resident #206 wanted to sit outside. The surveyors asked the DA approxiamtely what time he/she saw Resident #206 trying to exit onto the patio. The DA stated that it had to be before 12:00 PM because that was when he/she left the facility for the day. The DA stated that a nurse asked when he/she last saw Resident #206, so the DA provided the nurse with their observation and a statement. The surveyors asked when the DA was last educated on elopement and the DA said they learned about elopement in orientation, but was unable to speak to specifics, and stated that it was common sense to go look for the person, if they went missing.
On 09/06/22 at 1:22 PM, the surveyors reviewed the video surveillance from 09/03/22 from 10:07 AM to 10:10 AM. There were two cameras which provided the video surveillance. Both cameras were located on the first floor. One of the cameras was in hallway 1D with views of the hallway and patio entrance. The second camera faced the adjoining hallway between the facility and another outside organization. The Admin stated that there were no cameras outside of the facility.
On 09/03/22 at 10:07 AM, the video showed the DA walked to 1D unit.
At 10:08 AM, the surveyors observed Resident #206 self-ambulate from 1D unit, pointed at the patio area, observed the DA walk past Resident #206, and then observed Resident #206 ambulate toward the adjoining hallway.
At 10:08, the surveyors observed the DA walk towards the kitchen and returned food trays to the kitchen.
At 10:09 AM, the surveyors observed the DA leave the dietary area.
At 10:10 AM, the surveyors observed Resident #206 walk down the adjoining hallway when the DA was no longer in view of the camera. Resident #206 was observed in the video surveillance, walking toward the double doors that entered the adjoining area. The video ended when Resident #206 exited the door, and was no longer visible on the surveillance video.
On 09/06/22 at 1:55 PM, the survey team interviewed the Admin in the presence of the DON and asked, What should be done if the resident has wandering behavior and was confused? The Admin stated that residents had wandering behaviors, but it did not indicate that the resident was exit seeking.
On 09/06/22 at 1:56 PM, the survey team interviewed the DON in the presence of the Admin and asked, What does it mean when a resident wanders? The DON stated that a definition of wandering meant that a resident did not always remain in one space. The DON further stated that interventions to decrease wandering behavior included; to re-direct the resident, provide diversional activities, provide time in day room, provide the resident with verbal cues as to where they are. The DON told the survey team that if the resident had a history of wandering and displayed that behavior, it should be included in the resident's CP. The DON further stated that a wander guard assessment should be completed for a resident upon admission, quarterly, and annually.
On 09/06/22 at 3:52 PM, the surveyors interviewed the Admin who stated that the cameras were accurately time stamped, could not be edited, and the cameras captured live time.
On 09/06/22 at 3:56 PM, the survey team interviewed Resident #206 's Primary Care Physician (PCP), who stated that they had taken care of Resident #206 while he/she resided at the facility. The PCP did not take care of Resident #206 when he/she lived at home. The survey team asked the PCP to describe Resident #206. The PCP stated Resident #206 had a fair amount of confusion with day-to-day tasks, but was easily re-directed when Resident #206 was confused. The PCP stated that they never knew Resident #206 to have exit seeking behaviors at the facility, however, during the COVID-19 Pandemic there were a lot of room changes and Resident #206 would get confused and needed to be re-directed back to the location of their room, so staff placed a wander guard on Resident #206. The surveyors asked if the PCP knew when the wander guard was discontinued and the PCP could not recall specific dates, however, stated when PO's were discontinued, the nurse performed an assessment and PCP based the determination of discontinuing orders, off the nurse's assessment. The PCP stated that Resident #206 never expressed that he/she wanted to leave the facility. The PCP knew Resident #206's history prior to admission to the nursing facility. The PCP told the surveyors that Resident #206 was the primary caretaker of his/her spouse, the spouse became ill, and went to the hospital, and when the spouse was in the hospital, Resident #206 stayed at home and wandered around their home. The PCP stated that they never observed Resident #206 wandering and did not hear from staff that Resident #206 wandered and would assume that was why the wander guard was discontinued, because for the most part Resident #206 stayed in their room. The PCP stated that Resident #206's behavior of wandering was not exactly a chronic issue, it was an issue Resident #206 had in the past. The PCP gave the example of high blood pressure and stated that if wandering was in a resident's history, just like high blood pressure, that would always be something that should be monitored. The PCP further stated that they thought Resident #206's wandering should have been included in their plan of care because it would make Resident #206 challenging to go home without 24/7 supervision.
On 09/07/22 at 11:07 AM, LPN/UM #2 unit 1A stated that he/she was working on Saturday when Resident #206 eloped. LPN/UM #2 stated that Resident #206 did not have behaviors. Resident #206 would come out of the room and sit in the doorway and sometimes Resident #206 liked to sit in atrium. The atrium was closed a few weeks ago because it was under construction. Resident #206 would go to the atrium because he/she saw other people there and would just come back to the unit. The LPN/UM #2 stated Resident #206 was confused and could not put a complete sentence together. The LPN/UM #2 stated they had known Resident #206 for about a year and had never observed Resident #206 self-ambulate without an assistive device. The LPN/UM #2 saw Physical Therapist (PT) work with Resident #206 to use a rolling walker and Resident #206 was also assessed for use of a wheelchair. Even when Resident #206 stood in the room, he/she had an unsteady gait. Assistance of one person with care, would always need help. The LPN/UM #2 added that the Psychiatric Nurse Practitioner (PNP) recently decreased Resident #206's Depakote because he/she was not having behaviors. There were no noted changes in Resident #206's behavior or mood.
At one point, Resident #206 did have a wander guard in place, although LPN/UM #2 did not recall when it was removed but stated that they put the wander guard on Resident #206 when he/she was getting acclimated to the facility. Resident #206 and their spouse lived at the facility. Resident #206's spouse always expressed that they wanted to go home. That was why the facility put the wander guard on Resident #206. After Resident #206 was oriented to the facility and had a history of going to different areas on the first floor, Resident #206 never tried to exit the elevator, and was not exit seeking to the LPN/UM #2's knowledge. When asked about Resident #206's confusion, LPN/UM #2 stated when they asked Resident #206 something, he/she had a hard time to gather the words to answer the questions. Resident #206 knew the mealtimes, med times, staff, and other residents, but the resident would not have been safe to live in community based on their cognitive status. Resident #206 needed oversite- direction for showers and from the LPN/UM #2's experience, they did not identify Resident #206 as an elopement risk.
On 09/07/22 at 11:21 AM, the surveyor interviewed the Security Supervisor (SS) who stated that he/she was the head of the security for the facility and was employed by a security company that was subcontracted by the facility. The SS stated that there was no keypad to the left of the stairwell #4 door prior to 09/05/22, the day the repairs were done. The SS stated that There was not a keypad on that exit door prior to Monday. The SS also stated that The facility had just installed that keypad on Monday. The SS added that prior to 09/05/22, there was no lock on the door, and you could just walk out. The SS added that the security guards that were assigned to work at the facility had no responsibility of monitoring cameras and thought that the cameras were county property and unsure if they were working. The SS stated that the county personnel and visitors to the county clinic entered the adjoining hallway and used that same exit door to freely access the clinic, which was located on the second floor.
On 09/07/22 at 12:15 PM, the surveyor interviewed Resident #206's PNP who stated that he/she saw Resident #206 last week to follow up on their psychotropic medications and laboratory review. The PNP further stated that Resident #206 was first placed under psychiatric care because he/she had behaviors of refusing medications and care. The PNP told the surveyor that Resident #206 had diagnoses of depression, dementia, and mood disorders and was absolutely confused. The surveyor asked the PNP if Resident #206 had cognitive awareness of where they lived. The PNP stated that Resident #206 had periods of knowing where he/she was and at times did not. The PNP stated that he/she remembered that Resident #206 had a past history of wearing a wander guard, but they never verbalized or displayed behavior indicating that Resident #206 wanted to leave the facility. The PNP stated that they were surprised that Resident #206 walked out of the wheelchair because PNP always observed Resident #206 in their wheelchair.
On 09/07/22 at 02:32 PM, the surveyor interviewed the technician (tech) via telephone who stated that he/she provided a service on Monday Labor Day, 09/05/22. The tech stated he/she was called on Sunday, 09/04/22, but could not come and told the facility to call someone else but then he/she was called back and was able to come on Monday. The tech stated he/she was told that the wanderguard keypad was not working meaning that the wanderguard keypad was not keeping the door locked at all times. The tech added he/she was not an expert on wanderguards but had worked with them and knew they had more than one function and confirmed that the wanderguard was not keeping the door locked. The wanderguard was working when a wanderguard was in the vicinity because it would lock the door, but the relay to keep the door locked was not working. The tech referred to the new keypad he/she installed, on the left wall of the door, and a code had to be put in to unlock it. The tech added that there was no keypad on the left wall of the door before they put one in. When asked by the surveyor why the invoice had replaced keypad, the tech stated, I sort of replaced it, you say new and I say replaced, because I sort of replaced the keypad because they had a wanderguard keypad. The wanderguard keypad was on the opposite wall before the door.
Review of the document titled Police Department Investigation Report, dated 09/04/22, revealed that the police were called at 12:20 PM on 09/03/22. Once the police received a description of Resident #206, the police requested mutual aid from the sheriff's office, K-9 unit, as well as the utilization of the drone unit. After review of the facility's video, the police concluded that Resident #206 was last seen at approximately 10:12 AM walking down the dietary hallway of the facility, on the first floor, and walking through the exit door but it was undetermined from the video surveillance, which direction Resident #206 continued to walk. The police found Resident #206 on 09/03/22 at 3:52 PM, and Resident #206 expired at 4:19 PM on the same day.
A review of the facility's policy titled; Wandering/Elopement Policy with the revised dated of 01/2022, included; It is the objective of this facility to ensure the safety and protection of wandering residents by preventing their exit from the building. Under Policy Interpretation and Implementation; Section 1. Upon admission, annually, and when there is a significant change in status, resident will be assessed for wandering/elopement using the Elopement risk form. Any resident identified to be a risk for wandering either by preadmission history and/or observed behavior will be provided with a wander-guard and an appropriate plan of care will be developed.
Section 6- The Admin or in his/her absence the DON will notify Department of Health (DOH) if the resident is NOT FOUND as per DOH guidelines.
The facility's policy also did not indicate a specific time frame to notify DOH after a search for a missing resident that had not been found within the facility or on the facility's grounds.
This deficient practice placed Resident #206 and all other residents with moderate cognitive impairment who were at risk for or had a known history of wandering and/or exit seeking behavior, in an Immediate Jeopardy (IJ) situation. The IJ was identified on 09/07/22 at 4:15 p.m., when the Admin and DON were notified of the IJ situation, which ran from 09/03/22 until 09/05/22, when the door was monitored and repaired. The facility provided an acceptable removal plan on 09/08/22 at 10:16 AM, to remove the Immediacy.
The Removal Plan was verified by the survey team on 09/08/21 at 10:40 AM, the sixth day of the survey. This deficient practice continues at a lower S/S for no actual harm with the potential for more than minimal harm.
Part B
Refer to F609
On 09/01/22 at 11:32 AM, the surveyor observed Resident #191 reclining back in his/her reclining chair in their room. The surveyor attempted to interview the resident. The resident was able to communicate his/her name to the surveyor.
The surveyor reviewed the medical record for Resident #191.
A review of the resident's admission Record, reflected that the resident had resided at the facility for about a year and had diagnoses which included but were not limited to; cerebral palsy (a congenital disorder that affects movement, muscle tone and posture due to abnormal brain development before birth), lobar pneumonia, unspecified organism, unspecified severe protein calorie malnutrition, schizophrenia, major depressive disorder, anxiety, unspecified intellectual disabilities, essential hypertension, and gastro-esophageal reflux disease without esophagitis (inflammation that damages the tube running from the throat to the stomach).
A review of the resident's quarterly Minimum Data Set (MDS), an assessment tool used to facilitate the management of care dated 03/24/22, reflected that the resident had a Brief Interview for Mental Status score of 6 out of 15, which indicated the resident had moderately impaired cognition. A further review of the resident's MDS, Section G - Functional Status for activities of daily living reflected that the resident required supervision and setup for eating and drinking.
A review of the resident's Order Audit Report, throughout Resident's #191's stays at the facility, revealed a Physicians Order (PO) dated 05/27/2022, and timed at 10:37 AM, for regular diet puree texture, honey thickened liquid consistency.
According to a review of an incident investigation dated 06/08/22, completed by the facility's DON indicated on 05/27/22 at 2:30 PM Resident #191 was in the 2D dayroom during snack time. The resident's (Licensed Practical Nurse) LPN was informed by an activity aide that Resident #191 was choking and vomiting. The resident had a PO for honey thickened liquids and was provided thin whole milk by his/her primary CNA2. The resident was immediately evaluated by the LPN. Upon evaluation, the LPN heard crackles throughout the resident's lungs and determined the resident's vital signs were abnormal. The LPN notified the residents (Primary Care Physician) PCP who gave physician orders for the administration of oxygen and nebulizer treatments, quickly came to the unit, assessed the resident, and sent the resident to the hospital for an evaluation. Resident #191 was admitted with aspiration pneumonia and required placement of a peg-tube (a creation of an artificial external opening in the stomach for nutritional support) in the hospital.
A further review of the incident investigation dated 06/08/22, revealed Resident #191 was incorrectly provided regular thin liquids during snack time when his/her current diet order indicated honey thick liquids. The DON further concluded that the incident most likely occurred due to lack of knowledge regarding proper protocols in verifying fluid consistencies.
A review of a Progress Note (PN) dated 5/27/22, and timed at 14:30 (2:30 PM), indicated that while Resident #191 was in the dayroom during snack time, staff informed nursing that the resident was choking and vomiting. The PN further explained that the resident had a PO for honey thickened liquids and was given thin milk by an unknown staff member. The PN revealed that the resident was evaluated by the LPN. Upon evaluation, the LPN heard crackles throughout the resident's lungs, the resident's vital signs were abnormal, and the resident's physician was notified immediately. Upon notification of the physician, the physician provided the LPN with physician orders for the resident to be administered oxygen and a nebulizer treatment. The PN further indicated that the physician came to the unit, assessed the resident, and decided to send the resident to the hospital.
A further review of the resident's PN, dated 5/27/22, and timed at 22:35 (10:25 PM), reflected that the resident was admitted to the hospital with possible aspiration pneumonia.
A review of the resident's hospital discharge paperwork from 05/27/22 through 06/09/22, reflected a discharge diagnosis of aspiration which was identified on a chest x-ray. A further review of the resident's hospital paperwork indicated that the resident required placement of a peg-tube. The hospital discharge paperwork dated 06/08/22, by the Speech Language Pathologist (SLP) at the hospital indicated, [Resident arrives via ambulance from [facility] with [blood pressure] 70/40. The hospital discharge paperwork further indicated as per Emergency Medical Services the resident was normally on a thickened liquid but was administered unthickened milk at some point, aspirated on it.
A review of the facility's Investigation of the incident that took place on 05/27/22 was dated, 06/08/22 and signed by the DON. The investigation indicated that video surveillance dated 05/27/22 and timed at 1426 (2:26 PM), shows [CNA2] passing out snacks in the dayroom. He opens and places what appears to be a milk carton in from of [Resident #191]. [Resident #191] is seen sitting at the table drinking milk. Three other employees are present in the dayroom. [Activity aide] appears to be checking on [Resident #191], leaves the dayroom and returns with [LPN] (pulling the vital sign machine).
The Investigation revealed that the DON interviewed the staff members that were present in the dayroom. A review of the interview with the resident's LPN revealed that a staff member saw the resident drinking milk and then start coughing. The LPN went into the dayroom, evaluated the resident, and observed that the resident was coughing and spitting up. The LPN told the DON that she auscultated (listened to the resident's lungs with a stethoscope) and heard crackles. The LPN then notified the resident's PCP who gave her physician orders for oxygen and nebulizer treatments. The LPN interview indicated that the resident's PCP came to the unit and decided to call 911 because the resident's vital signs were abnormal.
A review of the interview with the resident's CNA2 indicated that he did not recall passing out the milk to Resident #191 but recalled seeing the resident drinking the milk and being surprised that the resident was on regular milk fluid consistency. The investigative report revealed that the DON asked the CNA2 the process for identifying residents on alternative fluid consistencies, the CNA2 responded that he knew by the dots by the resident's bedroom doors.
A review of the interview with the activity aide indicated that she saw the resident drinking milk out of a red carton. The activity aide told the DON that she did not know who gave the resident the milk and the resident was spitting up liquid and coughing. When the DON asked the activity aide the process for identifying residents on alternative fluid consistencies the activity aide stated that she did not know.
A review of the interview with the facility's Corporate Food Service Director revealed that on 05/27/22 at 10:31AM, the kitchen received a PO for honey thick liquids for the resident.
A review of the Investigation conclusion indicated the resident was provided regular thin liquids when his/her current diet indicated honey thickened liquids. A further review of the Investigation revealed the DON concluded Resident #191 received the incorrect fluid consistency during snack time and the incident most likely occurred due to lack of knowledge by staff regarding proper protocols in verifying fluid consistencies.
A review of Nurse Staffing for the 2D unit on 05/27/22, revealed that the CNA2 that provided Resident #191 with the thin whole milk was the resident's primary care CNA for that day.
A review of the CNA2's personnel file revealed that on 05/27/22, the CNA2 who provided the resident with thin whole milk received a verbal warning by the facility's DON. The verbal warning indicated that the CNA2 failed to follow instructions. Incorrect Diet was documented on the verbal warning work rule violation. Additionally, a Dietary Inservice was provided to the CNA2 by the DON. The Dietary Inservice indicated, Explained DOT system and importance of checking dietary restrictions prior to feeding. DOT system hanging in nurses station and dayroom. Specific colored DOT placed near resident's name plate by room door. No fluids left at bedside of residents on a tube feeding and with Blue Dot. Residents requiring thickened liquids will receive tray with empty mug and coffee thickener packet. Dietary will send up carafe of hot water for staff to use to make the coffee. Demonstrated how to use Coffee thickener packets- Nectar and Honey thick. Jello and ice cream are considered thin liquids. When unsure- STOP! And ask nurse before giving anything.
A further review of the CNA2's personnel file indicated that on 06/07/22, the CNA2 was terminated due to performance issues, absenteeism, and poor work quality.
A review of the resident's Care Plan, revised 07/26/22, reflected a focus area for nutrition. The goal of the resident's Care Plan was that the resident would follow diet as ordered. Interventions in Resident #191's Nutrition Care Plan included; provide me my diet as ordered and provide me with my supplements as ordered.
On 09/09/22 at 11:42 AM, the surveyor interviewed the facility's Registered Dietician (RD) who stated that a resident was placed on an altered diet or liquid consistency after being evaluated by the SLP. The RD stated that she observed resident's during mealtimes and if she noticed that a resident was having difficulty swallowing or suspected weight loss due to swallowing difficul[TRUNCATED]
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
Based on observation, interview, and review of other facility documentation, it was determined that the facility failed to maintain the facility in a clean and sanitary environment. This deficient pra...
Read full inspector narrative →
Based on observation, interview, and review of other facility documentation, it was determined that the facility failed to maintain the facility in a clean and sanitary environment. This deficient practice was identified for 2 of 6 units, (Unit 1 D and 2 A) and was evidenced by the following:
1. On the 1 D unit the surveyor observed the following:
- On 9/9/22 at 10:53 AM, the surveyor observed on 1 D unit hallway (that covered both the high and low side), black colored stains on the floor and on the walls.
- On 9/9/22 at 11:00 AM, the surveyor observed missing wall tiles in multiple areas of the 1-D hallway.
- On 9/9/22 at 11:15 AM, the surveyor observed the unit D shower area (the only available shower room on 1-D) and observed the shower head on the shower stall floor.
- On 9/9/22 at 11:15 AM, the surveyor observed a large dark stain on the tile floor of the 1-D shower stall.
- On 09/09/22 at 11:17 AM, the surveyor observed the ceiling of the main shower room with rust marks and chipped paint that was right above where the residents' shower.
- On 09/09/22 at 11:20 AM, the surveyor observed some dark stains on the wall tiles in the shower room.
- On 09/09 22 at 12:00 PM, the surveyor observed a fish tank in the 1 D dining/activity room with dirty water inside the tank. The surveyor observed no fish inside the tank.
- On 09/12/22 at 11:25 AM, the surveyor observed a few residents' rooms with chipped paint on their exterior door frame.
On 9/15/22 at 10:36 AM, during the Resident Council meeting, five of five residents discussed facility environmental concerns on unit 1-D with a surveyor. The five residents told the surveyor that the game room which is also the 1 D dining room was not cleaned regularly, broken blinds in the game room and the facility was painting ceiling tiles instead of replacing aluminum tiles in the game room. In addition, the 1 D shower room had no light, broken shower heads, and the facility staff placed a blanket on the floor to prevent water from flowing into the hallway.
A review of the housekeeping schedule from 8/31/22 through 9/15/22, provided by the Director of Nursing revealed that only one housekeeper was assigned on the 1-D nursing unit.
On 9/9/22 at 11:20 AM, the surveyor interviewed the Housekeeper (HK) on unit 1-D who stated that the HK's responsibility was to sweep and wash the 1-D unit floors that included the floors inside the residents' rooms and in the hallways. The HK also stated she cleaned the bathrooms and all the high touch areas. She further stated that the 1-D high-side shower room was being renovated and that all the residents are using the low-side shower room. When the surveyor asked the HK when was the last time the Unit 1-D hallway floors and walls had a deep cleaning, the HK laughed and stated that she can't remember the last time the floors were stripped and waxed.
On 9/15/22 at 12:30 PM, the surveyor interviewed the Director of Housekeeping stated that there were usually two housekeepers who worked on the 1 D unit. The Director pf Housekeeping also stated that there was only one housekeeper for the past few days because of staff shortages and that the facility was unable to do a deep cleaning on the 1-D nursing unit because they don't have enough overnight staff to strip and wax the unit 1 D hallway. The Director of Housekeeping further stated that stripping and waxing can only happen at night because the residents are sleeping and that this process was not done because of staff shortages. The Director of Housekeeping also stated that they were not able to buff the floor until the floors are stripped and waxed and buffing the residents' rooms are possible, but the hallways and the bathrooms are another challenge. The Director of Housekeeping acknowledged that the 1-D unit had one working shower room and the second shower room was being renovated.
2. On the 2 A unit the surveyor observed the following:
On 9/09/22 at 11:13 AM, the surveyor observed water leaking from the ceiling that was dripping onto the nursing station. It was leaking next to a computer which was in use by the unit 2 A nursing staff.
At that same time, the surveyor interviewed the Director of Medical Records (DMR) who stated that the leak had been fixed on multiple occasions but tends to return once it rains. The DMR also stated that it rained days ago but because it was a very hard rain, water must have accumulated which caused the current leak.
On 9/15/22 at 1:30 PM, the surveyor discussed the above observations and concerns with the administrative staff.
There was no additional information provided.
NJAC 8:39-31.4 (a)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Grievances
(Tag F0585)
Could have caused harm · This affected 1 resident
Based on interview and record review, it was determined that the facility failed to provide information and educate residents on the Grievance process. This deficient practice was identified for 5 of ...
Read full inspector narrative →
Based on interview and record review, it was determined that the facility failed to provide information and educate residents on the Grievance process. This deficient practice was identified for 5 of 5 residents (Residents #44, #51, #67, #150, and #15) interviewed for the grievance process at the Resident Council meeting conducted on 9/15/22 at 10:30 AM and was evidenced by the following:
On 9/15/22 at 10:40 AM, during the resident council meeting with five alert and oriented residents, the surveyor asked the residents if they were aware of what a grievance was and how to file a grievance with the facility if necessary. Five of the five residents present during the meeting told the surveyor they did not know the definition of a grievance or how to file a grievance. When the surveyor reviewed the resident council meeting minutes for June, July, and August 2022, prior to having the resident council meeting, the facility did not provide information regarding grievances.
On 9/15/22 at 3 PM, the surveyor reviewed the Resident admission Packet which did not contain any information explaining a grievance or instructing residents how to file a grievance. At the same time, the surveyor discussed the concern with the Licensed Nursing Home Administrator (LNHA) and the Director of Nursing (DON).
On 9/19/22 at 2:20 PM, the LNHA provided the surveyor with a weekly hand out that was given to each resident. On the back of the first page was a note to educate residents on the grievance process. The surveyor asked the LNHA if that was always in the weekly packet and the LNHA stated, no, it was added Friday which was after the surveyor's inquiry.
On 9/20/22 at 12:34 PM, the surveyor reviewed the facility grievance book which included grievances from February 2022 through July 2022, there were none for August 2022. Review of the September 2022 grievances included clothing issues for 4 of the 5 resident council members, all filed by the facility on 9/15/22 after the surveyor's inquiry.
On 9/21/22 at 10:24 AM, the surveyor reviewed the Patient Concern/Grievance policy. The policy was updated 9/22, after the surveyor's inquiry on the grievance process. The facility did not provide the policy that was in place prior to the Resident council meeting.
On 9/21/22 at 10:54 AM, the surveyor interviewed the Social Worker (SW) regarding the grievance process. The SW told the surveyor SW she was a traveling Social Worker, meaning going from facility to facility for the corporation. The SW had been at the facility one week. The surveyor asked what the grievance process was, and the social worker was unsure how they were completed at the facility, but told the surveyor that the other facilities educate residents on admission. The SW could not speak to what process the previous social worker had in place. The SW stated she would bring the surveyor the social work admission's packet that usually has the grievance process information included.
On 9/21/22 at 11:40 AM, the surveyor reviewed an undated packet titled Your Rights and Protections as a Nursing Home Resident provided by the SW. The sixth bullet on page one was titled Make Complaints, which indicated the residents have the right to make a complaint to the staff at the nursing home. It did not include the grievance process or instructions on how to file a grievance.
NJAC 8:39-4.1 (a) 35; 13.2 (c)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 9/14/22 at 11:45 AM, during the Resident Council meeting Resident #150 told the surveyor that he/she had never received a ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 9/14/22 at 11:45 AM, during the Resident Council meeting Resident #150 told the surveyor that he/she had never received a shower at the facility.
On 9/16/22 at 11:21 AM, the surveyor observed Resident #150 lying in bed awake and alert watching television. There was a basin filled with water and a washcloth was on resident's bedside table. Resident #150 stated that he/she gets a bed bath daily. He/she was able to wash most of his/her body and then the Certified Nursing Assistant (CNA) would assist and finish washing the area on his/her body that he/she couldn't reach. Resident #150 stated that he/she washes his/her own hair in bed and added, but it would feel so good to have my hair washed in the shower. The resident further stated that he/she was only offered a shower once since he/she arrived at the facility. The resident stated that he/she would prefer a shower but had not been offered a shower since that one time.
The surveyor reviewed Resident #150's medical records:
A review of the admission Record (admission summary), indicated that the resident had diagnoses that included but not limited to morbid obesity due to excess calories, iron deficiency anemia(too little iron in the body), drug-induced polyneuropathy(malfunction of many peripheral nerves in the body), major depressive disorder, neuromuscular dysfunction of bladder (lack of bladder control due to due to brain spinal cord, or nerve problems), heart failure, acquired absence of left leg above knee, acquired absence of left hip joint, and cellulitis (bacterial skin infection) of unspecified part of limb.
A review of the annual MDS dated [DATE], reflected the resident had a BIMS score of 11 out of 15, which indicated that the resident had a moderately impaired cognition. Review of Section G for Functional Status indicated the resident was totally dependent on staff with personal hygiene and bathing requiring one person assistance and totally dependent with transfers requiring two person assistance.
A review of the Physician's Order (PO) dated 7/2/22, indicated weekly showers every Wednesday, 7-3 shift. Complete skin observation tool; everyday shift and every Wednesday for hygiene.
A review of the September 2022 Treatment Administration Record (TAR) reflected the above corresponding PO's. Further review of the TAR indicated a check mark with staff initials indicating that the resident received a shower on 9/7/22 and 9/14/22.
A review of the Tasks section in the Electronic Medical Record (EMR) reflected that there were no check marks under the sections titled, ADL (activities of daily living) Bathing and/or Resident Refused that would indicate bathing was performed. There was no documented evidence of the resident's refusal of ADL/Bathing/shower weekly on Wednesdays for the month of September 2022.
A review of the Care Plan (CP) indicated a Focus area initiated on 7/28/20 and revised on 4/19/22, for ADL's which indicated the resident had decreased function in all areas of ADL's due to: Balance problems, debility, Missing limb, weakness, deconditioning, and morbid obesity. The CP goals indicated that the resident will maintain/improve ADL's and functional mobility through the next review date. The CP interventions/tasks indicated to assist with baths and showers. There were no CP interventions reflecting the 7/2/22 PO's for weekly showers every Wednesday. In addition, there was no documented evidence in the CP indicating the resident's preference for a shower or that the resident refused showers when offered.
On 9/16/22 at 11:26 AM, the surveyor interviewed the Licensed Practical Nurse Unit Manager (LPN/UM) on unit 1-D who stated that the resident was offered a shower weekly on Wednesdays during the 7-3 PM shift, but the resident always refused the shower. She further stated that the resident never requested a shower and that the resident was certainly able to have a shower. The LPN/UM stated that the resident was obese but the unit had a trolley device to transfer the resident into the shower. The LPN/UM stated that there was no shower binder on the unit. There was no documented evidence that the resident refused showers on Wednesdays.
On 9/16/22 at 1:51 PM, the surveyor interviewed the resident's assigned CNA who stated that the resident was offered a shower every Wednesday on the 7-3 PM shift but the resident always refused the shower. The CNA stated that the staff encouraged the resident to take a shower and to maintain his/her hygiene. She further stated that the resident receives a bed bath daily and would also sometimes refuse the bed bath. The CNA stated that she did not document the resident's refusal of showers or bed baths.
On 9/19/22 at 1:51 PM, the surveyor in the presence of the LPN/UM reviewed the resident's September 2022 TAR. The LPN/UM stated that the check marks on 9/7/22 and 9/14/22, indicated that the resident was bathed but not necessarily showered. The LPN/UM stated that if the resident preferred a shower, or refused a shower, bed bath, or any hygiene, then that concern should have been included in the resident's care plan.
On 9/19/22 at 2:19 PM, the surveyor in the presence of the survey team interviewed the DON who provided the surveyor with documentation that the resident refused bathing on 8/24/22 and 8/31/22. The DON stated that if a resident had behaviors of refusing showers then it should be care planned. There was no additional information provided.
NJAC 8 39-11.2(f)
Based on observation, interview, and record review, it was determined that the facility failed a.) to implement a comprehensive person-centered care plan intervention with regard to communication and b.) to develop a comprehensive person-centered care plan to address a behavior. The deficient practice was identified for 2 of 39 residents reviewed for care plans, (Residents #102 and #150), and evidenced by the following:
1. On 8/31/22 at 11:02 AM, the surveyor observed Resident#102 laying on the bed with the responsible party (RP) at the bedside. The RP stated that Resident#102 was cognitively intact, unable to speak appropriately but able to utilize the personal computer for communication. The RP further stated that he/she had a concern that the 11-7 staff think Resident#102 was cognitively impaired because Resident#102 was unable to talk properly due to ALS (Amyotrophic lateral sclerosis is a rare neurological disease that primarily affects the nerve cells responsible for controlling voluntary muscle movement like chewing, walking, and talking).
On 9/02/22 at 10:40 AM, the surveyor observed Resident#102 was laying on the bed with RP at the bedside. The RP showed the surveyor Resident#102's call bell. The RP stated that the flat call bell was specific for Resident#102 because Resident#102 was quadriplegic due to ALS and that the call bell should be placed just below Resident#102's chin for Resident#102 to be able to push the bell with his/her chin when needed. The RP stated that there was an incident a while ago that the RP was told by a Certified Nursing Aide (CNA) that Resident#102's call bell was not placed appropriately during the 11-7 shift. The RP was unable to remember the exact date and the name of the CNA but stated that he/she had immediately reported the incident to the management and the Social Worker (SW).
Furthermore, the RP stated that the same problem happened again a week ago, but was unable to remember the exact date and the name of the 11-7 shift CNA. The RP further stated that it was Resident#102 who informed the RP of the concern with the call bell that was not placed where Resident#102 would be able to use it. The RP added that the recent incident was reported to the SW.
On 9/02/22 at 11:18 AM, the surveyor interviewed the Registered Nurse/Unit Manager (RN/UM) regarding Resident#102's call bell. The RN/UM stated that the call bell should be placed within Resident#102's chest. Then the surveyor asked the RN/UM if RN/UM was aware that according to the RP, Resident#102's call bell should not be placed on the chest because it would not be accessible to Resident#102. The RN/UM stated that I have to get back to you about it. The RN/UM further stated that the call bell and the interventions should be in the Care Plan (CP) to follow.
The surveyor reviewed Resident #102's medical records:
The admission Record (admission summary), indicated that the resident had diagnoses that included but not limited to ALS, quadriplegia (a symptom of paralysis that affects all limbs and body from the neck down), anemia (low blood count), dysarthria, and anarthria (anarthria is a severe form of dysarthria. Dysarthria is a motor speech disorder that occurs when someone can not coordinate or control the muscles used for speaking).
Resident#102's person-centered focus care plan for communication showed has communication deficit due dysarthria r/t (related to) dx (diagnosis) of ALS; he/she can speak slowly but his/her voice is very soft; he/she communicates with an electronic device (computer) via a sensor at the tip of his/her nose (initiated on 6/27/17 and revision date of 11/24/21) with interventions that included to ensure that resident's personal computer for communication is functioning (date initiated 6/25/18 and revision date on 7/13/21) and provide a chin tuck call bell in reach at all times (initiated on 6/27/17 and revision date on 7/13/21).
According to the Investigation report of 11/11/21 and 11/18/21 claims that was provided by the Director of Nursing (DON), showed that on the day of 11/19/21, the RP came to the nursing office to discuss two areas of recent concern of the RP and Resident#102. Included in the 11/11/21 concern was CNA#1 placed Resident#102's call bell on top of Resident#102's chest instead of near the chin where Resident#102 can use the call bell to call for help. The investigation revealed that CNA#1 denied Resident#102's claim and CNA#1 was removed from Resident#102's assignment.
The 8/26/22 Grievance/Concern Form that was provided by the Licensed Nursing Home Administrator (LNHA) showed that Resident#102 emailed the SW about an incident on 8/26/22 at 5:00 AM when the 11-7 shift CNA#2 moved Resident#102's call bell away where Resident#102 was unable to reach it.
On 9/8/22 at 6:21 AM, the surveyors interviewed CNA#2. CNA#2 stated that Resident #102 is cognitively intact with difficulty talking. The surveyor asked CNA#2 if Resident#102's personal computer was being utilized when communicating with Resident#102. CNA#2 responded that CNA#2 was aware of Resident#102's computer and not sure about using the computer as a means of communication because CNA#2 followed the paper instruction that was posted in Resident#102's room for the list of Resident#102's questions when Resident#102 uses the call bell.
During an interview on 9/12/22 at 9:30 AM with the surveyor to the SW, the SW stated that SW was unaware that Resident #102 was able to communicate via computer until SW had received an email on 8/26/22 about the CNA#1 who had moved the resident's call bell away.
On 9/12/22 at 11:11 AM, the surveyor interviewed the Assistant Director of Nursing (ADON) who signed the Investigation of 11/11/21 and 11/18/21 claims of Resident #102. The surveyor asked the ADON if ADON asked Resident#102 to respond to ADON's interview about the 11/11/21 and 11/18/21 investigations with the use of Resident#102's computer. The ADON responded I don't recall utilizing the computer for an interview.
On 9/13/22 at 11:39 AM, the surveyor interviewed CNA#3. CNA#3 stated that Resident#102 was cognitively intact, unable to talk, and uses the call bell. CNA#3 further stated that Resident#102 was able to communicate through facial gestures and nodding. The surveyor asked CNA#3 if CNA#3 was aware that Resident#102 was able to communicate with the use of Resident#102's personal computer and CNA#3 stated I'm not sure.
On 9/15/22 at 02:19 PM, the survey team met with the LNHA, Chief Nursing Officer (CNO), and DON and were made aware of the above concerns.
On 9/20/22 at 10:23 AM, the surveyor called CNA#4 for the second time concerning the 8/26/22, Grievance concern and there was no callback.
On 9/20/22 at 01:56 PM, the survey team met with the LNHA, DON, and Assistant Nursing Home Administrator. There was no additional information provided.
NJAC 8:39-11.2(f)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on observation, interview, and review of pertinent facility documentation, it was determined that the facility failed to update and revise an Interdisciplinary Comprehensive Care Plan (IDCCP) to...
Read full inspector narrative →
Based on observation, interview, and review of pertinent facility documentation, it was determined that the facility failed to update and revise an Interdisciplinary Comprehensive Care Plan (IDCCP) to include interventions for 1 of 11 residents, (Resident #121), reviewed for accidents.
This deficient practice was evidenced by the following:
On 9/13/22 at 11:10 AM, the surveyor observed Resident #121 who was alert, oriented, and seated in a wheelchair watching television.
The surveyor reviewed the medical record for Resident #121.
The admission Record reflected that Resident #121 was admitted to the facility with diagnoses that included but not limited to schizophrenia (a disorder that affects a person's ability to think, feel and behave clearly), bi-Polar illness (condition of mood swing from depressive lows to manic highs), major depressive disorder (long term loss of pleasure and interest) and anxiety disorder (disorder of feeling worried and fear).
A review of the Annual Minimum Data Set (MDS), an assessment tool used to facilitate the management of care dated 6/30/22, revealed that Resident #121 had a Brief Interview Mental Status (BIMS) score of 15 out of 15 which indicated that the resident had an intact cognition.
A review of Resident #121's progress notes (PN) dated 6/22/22 at 21:14 (9:14 PM) revealed a nurses note: Resident discovered by orientee nurse in the bathroom smoking a cigarette. The nurse went into room and found a cigarette in the toilet. The nurse could not locate alleged matches or possible lighter. Resident #121 continues to exhibit behaviors out of baseline. The nurse has attempted to collect UA/CNS multiple times to no affect. Resident #121 continues to throw away what left in toilet. Replaced 4 times. Resident #121 awaiting Psych consult. Labs to be drawn in the morning. Supervisor made aware. Education rendered to Resident #121. Monitoring in progress.
A review of the Facility's investigation dated 6/22/22 revealed that Resident #121 was discovered smoking in the bathroom while a staff member was conducting rounds on the evening of 6/21/21. The staff member entered the room and smelled cigarette smoke. The staff member asked Resident #121 if they were smoking. Resident #121 stated that Resident #121 was smoking a cigarette that Resident #121 had left over from the previous smoke break. Resident #121 stated that they used a match from a match box. Resident #121 had two matches left and that they flushed the match book down the toilet. Resident #121 allowed the nurse and the night supervisor to inspect Resident #121's room for cigarettes and a lighter/matches. The nurse and the night supervisor were unable to find anything. Resident #121 was educated about the facility smoking policy and that smoking inside the facility was prohibited.
The investigational report also had an interview from the Assistant Administrator (AA) who met with Resident #121 on 6/22/22. Resident #121 was re-educated regarding the facility's smoking policy. Resident #121 was also warned that if they were caught smoking inside the facility that Resident #121 will lose their smoking privileges. The AA and the Administrator (Admin) also conducted another search of Resident #121's room. The facility conducted two more searches and was unable to find any cigarettes or lighters.
A review of Smoking Assessments dated 12/30/21, 03/31/22 and 6/30/22 revealed that Resident #121 is a safe smoker and that Resident #121 are safe to smoke unsupervised.
A review of Resident #121's Care Plan (CP) was revealed there was no documentation in CP regarding Resident #121 smoking in their room on 6/22/22 with no interventions preventing this from happening again. The Care Plan Reflected the following:
They were a focus area for Smoking with an initiation date of 1/12/22, and a revision date of 4/07/22, which had a goal that Resident #121 will not suffer injury through the next review date. The Smoking care plan revealed the following interventions:
-Assist resident with set up as needed.
-Educate about smoking risk/hazards and about the availability for cessation.
-Educate resident about the facility policy on smoking: appropriate places to smoke, times, concerns, facility rules and regulations.
-Resident can smoke unsupervised
-Monitor resident to ensure continued safety while smoking. Observe clothing and skin for signs of cigarette burns.
-Notify MD and family of any injury related to smoking
-Smoking supplies are stored according to facility policy: Staff hold and distribute.
On 9/20/22 at 12:45 PM, the surveyor interviewed Resident #121 who stated that after the smoking incident on 6/22/22, that Resident #121 was re-educated about the facility smoking policy and that if Resident #121 broke the rules again that Resident #121 will lose their smoking privileges. Resident #121 stated that they will never smoke inside the facility again.
On 9/20/22 at 1:10 PM, the surveyor interviewed Resident #121's Certified Nursing Assistant (CNA) who stated that Resident #121's behaviors have been good the past few months. The CNA also stated that at the time of the smoking incident Resident #121 was experiencing a lot of behaviors including being agitated and combative. The CNA noted that they never saw Resident #121 smoking or even smelled smoke in Resident #121's room but heard that another staff member found a cigarette in Resident #121's toilet.
On 9/20/22 at 1:15 PM, the surveyor interviewed the 2 A Unit Manager (UM) who stated that UM remembered Resident #121's smoking incident and it occurred at a time when Resident #121 was experiencing a lot of behaviors. UM also noted that the facility already notified the psychiatrist regarding Resident #121's behaviors and that Resident #121 was being monitored. UM also stated that when Resident #121 was caught smoking the facility in-serviced Resident #121 regarding the facility smoking policy and Resident #121 was warned if Resident #121 smoked again in their room that Resident #121 will lose their smoking privileges. The facility also did room checks and found no smoking material inside Resident #121's room. When the surveyor asked the UM if the facility should have implemented a CP for this incident, the UM stated that UM didn't feel that Resident #121 should be CP for a one time incident.
On 9/20/22 at 2:30 PM, the surveyor interviewed the Recreation Director (RD) regarding the facility's smoking program. The RD stated that the recreation department are responsible for supervising the smoking activity during the 9:30 AM, 1:30 PM, and the 3 PM smoke times. The recreation department will bring a locked cart that contain the residents' cigarettes. The recreation department will distribute the cigarettes to the residents', and they will only give out two at a time. The recreation department have no lighters or matches, the residents light their cigarettes from a lighter that's mounted on the exterior wall. Recreation staff will also observe to make sure that residents are smoking safely, don't have their own lighters or matches and that they are not bringing cigarettes back into the facility. If the recreation department catches a resident with their own lighter, the facility will confiscate the lighter and re-educate that resident regarding the facility smoking policy. RD that the facility policy was to warn on the first incident and if it happened again that resident would either lose their smoking privileges or they will be discharged from the facility. RD further stated that Resident #121 only had one incident and that if a resident is caught breaking the smoking policy RD's department will either be notified in the morning meeting or through email.
On 9/21/22 at 9:30 AM, the surveyor observed the smoking activity and observed recreation staff members distributed cigarettes to the residents. Inside the smoking cart contained individual boxes that were locked and contained the cigarettes for specific residents. The surveyor observed staff give out no more than two cigarettes. The residents were observed lighting their cigarettes from an exterior wall mounted lighter.
On 9/21/22 at 9:40 AM, the surveyor interviewed a Recreation staff member who stated that at the start of the smoking activity that resident's will line up and that staff will distribute their cigarettes. The smoking cart contained no lighters or matches. Resident must light their cigarettes from the wall mounted lighter. The recreation staff will observe the residents, to make sure that they are smoking safely and if they were observed using a lighter or matches the facility will confiscate and re-educate the resident regarding the facility's smoking policy.
On 9/21/22 at 10:57 AM, the surveyor interviewed the Licensed Nursing Home Administrator (LNHA) who stated that Resident #121 was re-educated regarding the facility smoking policy and the facility conducted three room checks to make sure that Resident #121 was compliant with the facility smoking policy. LNHA did state that a CP could have been updated to reflect this incident.
On 9/21/22 at 11:08 AM, the surveyor interviewed the AA who stated that both the AA and the LNHA at the time of the incident met with the resident the day after the smoking incident. AA stated that Resident #121 was re-educated and that Resident #121 allowed them to do a room check and they found no cigarettes or lighters/matches. The AA and LNHA advised Resident #121 that if they broke the facility's smoking policy again that Resident #121 could lose their smoking privileges. The AA acknowledged that AA doesn't know much about care planning and that a CP was created and updated by either the UM or the Director of Nursing (DON). AA stated that they probably didn't update the CP because it was a one time incident.
On 9/21/22 at 1:30 PM, the surveyor met with the DON and the LNHA and no further information was provided by the facility.
A review of the facility's policy titled Smoking Policy-Residents that was dated 8/31/22 and was provided by the DON included the following:
Under Policy Interpretation and Implementation.
7. Any smoking-related privileges, restrictions and concerns shall be noted on the care plan, IDT note in the resident medical record, and all personnel caring for the resident shall be aware of these issues.
11. Smoking articles for residents with or without independent smoking privileges:
e. Smoking shall not be permitted in bed or the facility, at any time.
13. The facility staff will check periodically to determine if residents have any smoking articles among their possessions or on their person in violation of our smoking policies. Staff shall confiscate any such articles and shall notify the Charge Nurse/Unit Manager that they have done so, and the IDT will meet with the resident and document in the IDT section of the medical record. The Administrator and Director of Nursing will be made aware of any infractions of the smoking policy.
NJAC 8:39-11.2 (1), (2), 12.1, 27.1 (a)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, interviews, and record review, it was determined that the facility failed to accurately transcribe a physician's order for a wound treatment to a stage 4 sacral pressure ulcer on...
Read full inspector narrative →
Based on observation, interviews, and record review, it was determined that the facility failed to accurately transcribe a physician's order for a wound treatment to a stage 4 sacral pressure ulcer onto the Treatment Administration Record (TAR) for 1 of 4 residents (Resident #181) reviewed for wound care.
The deficient practice was evidenced by the following:
On 9/09/22 at 11:13 AM, the surveyor observed Resident #181 lying in bed with head of bed elevated and bed covers on and up to Resident #181's waist. Resident#181 was awake and watching television.
A review of Resident #181's Electronic Medical Record (EMR) indicated that Resident #181 was admitted to the facility with a diagnosis that included, but not limited to, multiple sclerosis (a disease in which the insulating covers of nerve cells in the brain and spinal cord are damaged. This damage can result in decreased vision, muscle weakness, and trouble with sensation and coordination.), peripheral vascular disease (a condition in which narrowed blood vessels reduce blood flow to limbs), neuromuscular dysfunction of bladder (a lack of bladder control due to brain, spinal cord or nerve problems), atherosclerotic heart disease (the build-up of fats, cholesterol, and other substances in and on the artery walls), and dementia (impairment of memory and judgement).
A review of Resident #181's quarterly Significant Change Minimum Data Set (MDS), an assessment tool used to facilitate the management of care dated 7/19/2022, reflected Resident #181 had a Brief Interview for Mental Status (BIMS) score of 03 out of 15, indicating Resident #181's cognition was severely impaired. Review of Section G for , Functional Status indicated Resident #181 did not ambulate, and was totally dependent for eating, bathing, dressing, toileting, and transfers. Section M of the MDS for Skin Conditions indicated that Resident #181 had a stage 4 (full thickness tissue loss with exposed bone, tendon, or muscle) pressure ulcer.
A review of Resident # 181's current Physician orders (PO) indicated a PO dated 9/01/2022, for calcium alginate miscellaneous: Apply to sacral wound topically every day shift for wound care. Cleanse NSS [normal saline solution], pat dry. Apply collagen powder to wound base, and cover with calcium alginate. Place a silicone foam dressing over. Change BID [twice a day] and when soiled.
A review of the Wound Care Nurse Practitioner progress notes titled, Physician Recommendation Details/Wound Orders and Treatment Recommendations, dated 9/07/2022, indicated to change sacral dressing twice daily or when soiled.
A review of the September 2022 Treatment Administration Record (TAR) revealed that the sacral wound treatment was plotted for once daily on the day shift.
During an interview with the surveyor on 9/13/2022 at 10:36 AM, Resident #181's assigned Licensed Practical Nurse (LPN#1) employed at the facility since 2/2022, reviewed Resident #181's wound care orders with the surveyor. The surveyor asked the LPN, how often was the resident's sacral wound treatment being administered and the dressing changed? The LPN stated, twice a day or when soiled. The surveyor showed the LPN that Resident #181's TAR indicated that the sacral wound treatment was signed as administered once daily on the 7-3 shift. The LPN stated that Resident #181 is incontinent of stool, so the sacral dressing is probably changed more than once a day.
During an interview with the surveyor on 9/15/2022 at 11:10 AM, Resident #181's assigned LPN#2 reviewed the PO's order for Resident #181's sacral wound treatment. The LPN#2 stated that the PO indicated to change the dressing BID (2 times a day) and when soiled. The LPN#2 then reviewed Resident#181's TAR in the EMR (electronic medical record) and stated that Resident #181's sacral wound order was transcribed to be done once daily on the 7-3 shift. The LPN#2 further stated that Resident #181's TAR should have indicated that the sacral wound treatment to be administered twice a day as per the physician's ordered. The surveyor asked LPN#2 what were the times for a BID wound treatment? The LPN#2 stated she would have to clarify Resident #181's PO for the sacral wound, and also clarify with the Unit Manager (UM) about the correct times to put in the TAR for BID treatments.
On 9/15/22 at 11:21 AM, the surveyor interviewed the Unit Manager (UM) on unit 1-B who stated that the resident's sacral wound care was done daily. The surveyor asked the UM to review Resident #181's PO and TAR for the sacral wound treatment in the presence of the surveyor. The UM read the PO and stated that the order indicated to change sacral wound BID (twice a day) and when soiled. The UM then reviewed the TAR and stated that it indicated to change the sacral wound once daily on the 7-3 shift. The UM further stated that the TAR indicated that the sacral wound care was done once during the 7-3 shift, but the resident was incontinent of stool and was sure the sacral dressing was changed a second time during the day due to being soiled from stool. The UM stated that the resident's sacral wound order was changed to daily and/or when soiled, and she forgot to change the verbiage in the order details when transcribing the PO onto the TAR. The UM further stated that if a physician ordered a resident's wound dressing to be changed BID (2 times a day), he/she would transcribe the physician's wound care order in the TAR to be done daily on the 7AM-3 PM day shift and the 3 PM-11 PM evening shift.
On 9/16/22 at 11:47 AM, in the presence of the survey team, the Director of Nursing (DON) stated that the resident's 9/1/22, PO indicated the sacral wound to be changed BID and when soiled. The Licensed Nursing Home Administrator (LNHA) and DON acknowledged that the sacral wound care treatment was not transcribed onto the September 2022 TAR according to the 9/1/22 physician's order.
NJAC 8:39-27.1 (a)
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 9/1/22 at 10:50 AM., the surveyor observed Resident #177 in his/her room out of bed and sitting on his/her wheelchair, awa...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. On 9/1/22 at 10:50 AM., the surveyor observed Resident #177 in his/her room out of bed and sitting on his/her wheelchair, awake, alert, and appropriately responded to the surveyor's inquiry.
A review of the admission Record (an admission summary) revealed that Resident #177 was admitted to the facility on [DATE], with diagnoses that included but not limited to Type 2 Diabetes Mellitus with Mild Nonproliferative Diabetic Retinopathy without Macular Edema, Bilateral (high blood sugar that affected the eyes) and Major Depressive Disorder, Recurrent, Unspecified.
A review of the admission MDS with an Assessment Reference Date (ARD) of 7/21/22, reflected that the resident had a BIMS score of 14 out of 15, which indicated that the resident was cognitively intact.
A review of Resident #177's hybrid (paper and electronic) medical records reflected no available progress notes from the attending physician. The EMR reflected Physician's Progress Notes all written by the APN.
On 9/14/22 at 9:45 a.m., the surveyor asked the DON to provide all the resident's physician progress notes for July 2022 through the most current in September 2022.
On 9/15/22 at 9:35 a.m., the surveyor interviewed the DON regarding Resident #177's physician visits and documentation. The DON was informed that the surveyor could not find the attending physician's notes in the resident's hybrid medical records.
During the interview, the surveyor reviewed the electronic Physician's Progress Notes with the DON. The DON acknowledged that there was no documentation written by the resident's attending physician. She further acknowledged that the attending physician's progress notes should be readily accessible in the resident's medical records.
On the same day at 2:19 p.m., the survey team met with the LNHA, DON, and the Chief Nursing officer and they were made aware of the above concerns. There was no additional information provided.
On 9/19/22 at 3:05 p.m., the surveyor interviewed Resident #177's attending physician regarding his resident visits and documentation records. The primary physician stated that he saw Resident #177 and had the progress notes in his possession. He further stated that he was going to put his documentation in the resident's electronic medical record but was not a good typist.
During an interview with the DON on 9/20/22 at 9:54 AM, she stated that she had not received the progress notes from the resident's attending physician. The surveyor asked the DON who was responsible for overseeing to ensure that the physicians were documenting on the resident's medical records. The DON stated that she did not know but she would double check who's responsible.
On 9/21/22 at 12:36 p.m., the Licensed Nursing Home Administrator (LNHA) and DON met with the survey team. The DON was asked if the facility received progress notes from the attending physician. The DON stated that they have not received progress notes from him. There was no additional information provided by the facility.
A review of the facility policies titled Physician Visits and regarding the protection of all the facility's medical records. However, both did not speak of medical records accessibility.
NJAC 8:39-35.2 (d)(5), (g)
Based on observation, interview and record review, it was determined the facility failed to maintain complete and readily accessible medical records. This deficient practice was identified for 2 of 39 residents, (Resident #159 and Resident #177), and was evidenced by the following:
1. On 9/13/22 at 11:00 AM, the surveyor reviewed Resident #159 physician progress notes in the electronic medical record (EMR). In review of the physician notes the surveyor noted that all the resident's progress notes were written by an Advanced Practice Nurse (APN). The surveyor could not locate any notes written by the attending physician within the medical record. The surveyor then asked the Director of Nursing (DON) to provide all the resident's physician progress notes for July and August.
The surveyor reviewed the admission Minimum Data Set (MDS), an assessment tool dated 7/13/22. Medical diagnoses included cancer, chronic obstructive pulmonary disease (COPD, a condition involving constrictions of the airways and difficulty or discomfort breathing which sometimes requires supplemental oxygen), hypertension (high blood pressure). Review of the Brief Interview of Mental Status (BIMS) indicated the resident had a BIMS of 14 out of 15, which indicated the resident was cognitively intact. Review of section G showed the resident had a functional status of 2-person assist for transfer and toileting and a one-person assist for dressing eating and hygiene
On 9/15/22 at 11:15 AM, the surveyor reviewed the resident's progress notes for July and August 2022. Resident #159 was admitted to the facility on [DATE], the first progress note was the admission note dated 7/8/22 written by the APN. The resident had physician progress notes for 14 more visits in July and all visits were submitted by the APN. Review of the August progress notes showed that the resident was seen 14 times in August 2022 and all notes were submitted by the APN. The surveyor could not locate any progress notes completed by the attending physician.
On 09/19/22 at 1:30 PM, surveyor placed calls to the attending physician and the APN.
On 09/19/22 at 2:15 PM, the surveyor asked the DON if the attending physician of Resident #159 provided documentation of visits to the facility for the months of July and August and the DON stated I have a call out to the doctor.
On 09/19/22 at 3:05 PM, the surveyor received a call back from the attending physician for Resident #159 regarding visits and documentation of progress notes. The physician told the surveyor he saw the patient and had the documentation and was going to put it in the (EMR) but was not a good typist. The physician had not given the surveyor an exact date of when he last rounded in the facility to see his residents.
On 09/20/22 at 2:30 PM, the DON was asked if any progress notes from the attending physician were received by the facility, and the DON said she needed to place another call out to the physician.
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, interview, and record review, it was determined that the facility failed to: a.) ensure that appropriate hand hygiene was performed by 2 of 13 staff observed during dining and wo...
Read full inspector narrative →
Based on observation, interview, and record review, it was determined that the facility failed to: a.) ensure that appropriate hand hygiene was performed by 2 of 13 staff observed during dining and wound care observation, and b.) disinfect the table for 1 of 2 staff observed for wound treatment in accordance with the Centers for Disease Control and Prevention (CDC) guidelines for infection control and facility policies.
This deficient practice was evidenced by the following:
According to the U.S. CDC guidelines Hand Hygiene Recommendations, Guidance for Healthcare Providers for Hand Hygiene and COVID-19, page last reviewed 1/8/2021 included, When to Perform Hand Hygiene? Multiple opportunities for hand hygiene may occur during a single care episode. Following are the clinical indications for hand hygiene: Use an Alcohol-Based Hand Sanitizer: Immediately before touching a patient .Hands should be washed with soap and water for at least 20 seconds when visibly soiled, before eating, and after using the restroom. Immediately after glove removal .
1. On 9/9/22 at 12:29 PM, the surveyor observed that there were 8 (eight) residents and one Certified Nursing Aide#1 (CNA#1) inside the 2 A dining area. The CNA#1 provided a plastic bib (an item of clothing tied around the neck to protect clothes from getting dirty when eating) to four out of eight residents. The CNA#1 had direct contact with four residents while applying the bib and then immediately donned (applied) a new pair of gloves without performing hand hygiene.
On that same date and time, CNA#1 used the hand wipes to help Resident#162 in performing hand hygiene by holding the resident's both hands and wiping back and forth, discarded the used hand wipes to the plastic cup that the CNA#1 was also holding on her right hand, then immediately went to Resident#804 without removing the used gloves and without performing hand hygiene in between residents, used another piece of hand wipes to help the resident perform hand hygiene by directly touching the resident's both hands. When the CNA#1 was about to do the same thing to Resident #231, the surveyor called the attention of the CNA#1 to the side while two other staff entered the 2 A dining room.
At that time, the surveyor interviewed CNA#1 about hand hygiene. The CNA#1 informed the surveyor that hand hygiene should be performed before and after direct contact with the residents, before and after applying gloves and PPE (personal protective equipment). Then the surveyor asked the CNA#1 if she had direct contact with the residents in the dining area and what she should have done at that time. The CNA#1 stated, yes, and I should have performed hand hygiene before putting on my gloves. Afterward, the surveyor asked the CNA#1 if she did change her gloves in between direct contact with the residents and if should she perform hand hygiene between direct contact with Residents#162 and #804. The CNA#1 responded no, and that she stated that should have removed the used gloves, performed handwashing, and applied a new pair of gloves before going to the next resident.
Furthermore, the surveyor asked CNA#1 why she did not perform hand hygiene, and the CNA#1 had no answer. The CNA#1 indicated that she's been working in the facility for two and half years and was educated about hand hygiene by the Infection Preventionist Nurse (IPN).
2. During an observation on 8/31/22 at 10:54 AM by the surveyor, CNA#2 was inside the resident's room while providing morning care to the resident.
The surveyor reviewed the medical records of Resident #69.
The admission Record (admission summary) reflected that the resident was admitted to the facility with diagnoses that included Paraplegia unspecified (paralysis that affects all or part of the trunk, legs, and pelvic organs) and Multiple sclerosis (a neurological disease that causes dizziness, mobility problems, numbness, and fatigue.)
The Quarterly Minimum Data Set (QMDS) ARD 6/23/22, an assessment tool used to facilitate the management of care, indicated a Brief Interview for Mental Status (BIMS) score of 15 out of 15, which reflected that the resident's cognition was intact.
The Order Summary Report (OSR) for September 202 included the following wound care orders:
- Start Date (SD) 7/15/22 Cleanse bilateral toes with NSS (normal saline solution) apply Bacitracin (an antibiotic used to prevent wound infections) OTA (open to air) alternating or every other day one time a day every two days.
- SD 9/2/22 Lotrisone Cream 1-0.05% (is a prescription medication used on the skin) apply to left buttock topically every day and evening shift for wound care cleanse with NSS pat dry.
- SD 9/2/22 Lotrisone Cream 1-0.05% apply to left gluteal fold topically every day and evening shift for fungal rash cleanse NSS, pat dry.
- SD 7/28/22 Zinc Oxide ointment (skincare and preventative medicine) 10% apply to BL (bilateral) buttocks topically every day and evening shift for a skin condition. Apply following all care/incontinence opportunities PRN (as needed).
A review of the Progress Notes showed an 8/31/22, Skin/Wound (S/W) Note signed by a Registered Nurse (RN) that indicated that the resident was seen for a weekly wound visit by NP (Nurse Practitioner). The 8/31/22 S/W Note reflected that there was a left buttock MASD (moisture-associated skin damage) and left gluteal fold fungal dermatitis with an order of cleansing with NSS and applying Lotrisone cream BID (twice a day).
On 9/2/22 at 10:32 AM, the surveyor observed the resident laying in bed while watching television. The resident stated that the wounds on their back were getting better, the nurse does wound care every day and there was no concern.
On 9/9/22 at 11:22 AM, the surveyor observed CNA#2 and Licensed Practical Nurse (LPN) during wound treatment observation. The side table that was used for wound care was not disinfected as evidenced by a white spot and a liquid on some part of the table with no barrier used when the Zinc oxide skin protectant container, a box of gloves, a tube of Bacitracin, foam dressing were found on top of the table. There were also resident's personal belongings on top of the table which included drinking cups and papers.
On that same date and time, the surveyor observed the LPN removing gloves and performing handwashing for 11 seconds after the wound care treatment. The LPN informed the surveyor that handwashing and scrubbing hands should be at least 20 seconds. The surveyor asked the LPN if she washed her hands for 20 seconds and the LPN stated, I think so, then the surveyor told the LPN that the surveyor observed the LPN scrubbing her hands for 11 seconds and the LPN responded, Oh, I am sorry.
Furthermore, during an interview with the surveyor, the LPN stated that she did not disinfect the table because I know it was being clean in the morning. Afterward, the LPN further stated that she should have disinfected the table before putting the supplies.
On 9/9/22 at 11:41 AM, the surveyor interviewed the Registered Nurse/Unit Manager (RN/UM) regarding the above concern. The RN/UM stated that the LPN should have washed her hands for 20 seconds and that she was educated by the IPN on hand hygiene.
On 9/15/22 at 11:53 AM, the surveyor interviewed and asked the IPN who is responsible for hand hygiene, PPE, and wound treatment competencies in the facility. The IPN stated that she was responsible for hand hygiene and PPE competencies. She further stated that I think it was the Unit Manager who's responsible for the wound treatment competency, but I will get back to you with that.
At that time, the surveyor asked the IPN about the wound treatment process and hand hygiene. The IPN informed the surveyor that the staff should use the purple sani wipes (disinfecting wipes) in wiping the table before setting up we want to make sure that nothing on the table come in to contact dirty area, that it was a nonsterile procedure but want to maintain as clean as possible. She further stated that handwashing should be scrubbing for 20 seconds. The IPN indicated that when staff had direct contact with residents, staff should change gloves and perform hand hygiene.
On that same date and time, the surveyor informed the IPN of the above concerns with CNA#1 and the LPN. The IPN acknowledged that the LPN should have washed her hands for 20 seconds, must disinfect the table before use, and should have followed the facility policy about putting a liner on top of a clean table before placing the wound care products and supplies. She further stated that CNA#1 should have changed gloves and performed hand hygiene in direct contact with a resident in the dining area. The IPN stated that she will re-educate the LPN and CNA#1.
On 9/15/22 at 02:19 PM, the survey team met with the Licensed Nursing Home Administrator (LNHA), Corporate Chief Nurse, and the Director of Nursing (DON) and discussed the above concerns.
On 9/20/22 at 12:44 PM, the DON informed the surveyor that there was no negative effect on the resident's buttocks.
A review of the facility's Handwashing/Hand Hygiene Policy that was provided by the DON with a reviewed/revised date of 8/2022 included Policy Statement: This facility considers hand hygiene the primary means to prevent the spread of infections. Policy Interpretation and Implementation: 7. Use an alcohol-based hand rub containing at least 62% alcohol; or , alternatively, soap (antimicrobial or non-antimicrobial) and water for the following situations: .b. Before and after direct contact with residents; i. After contact with with a resident's intact skin; .Washing Hands 1. Vigorously lather hands with soap and rub them together, creating friction to all surfaces, for a minimum of 20 seconds (or longer) under a moderate stream of running water, at a comfortable temperature .
A review of the Wound Care policy that was provided by the DON with a reviewed/revised date of 12/2021 included Purpose: The purpose of this procedure is to provide guidelines for the care of wounds to promote healing Steps in the Procedure: 1. Use disposable cloth (paper towel is adequate) to establish clean field on resident's overbed table. Place all items to be used during procedure on the clean field .
On 9/20/22 at 01:56 PM, the survey team met with the LNHA, DON, and Assistant Nursing Home Administrator and there was no additional information from the facility.
NJAC: 8:39-19.4(a)(b)(l)(n)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** REFER TO F610
REFER TO F609
Based on observation, interview, and record review, it was identified that the facility failed to re...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** REFER TO F610
REFER TO F609
Based on observation, interview, and record review, it was identified that the facility failed to report to the New Jersey Department of Health (NJDOH) and follow facility policy and procedures for reporting: a.) an unwitnessed event which resulted in a major injury for Resident #75, b.) an allegation and investigation of a resident to resident altercation, for Residents #27 and #228, c.) an allegation of abuse made by a resident representative for Resident #99, d.) an injury of unknown origin for Resident #99, and e.) an observed incident and investigation in which serious bodily injury occurred to Resident #191. The deficient practice was identified for five (5) of six (6) residents reviewed for alleged violations, (Resident #27, #75, #99, #191, and #228) and was evidenced by the following:
1. On 9/08/22 at 11:28 AM, the surveyor interviewed the responsible party (RP) for Resident #75 in the presence of a second surveyor. The RP informed the surveyors that Resident #75 sustained a right hip fracture which required surgery. The RP also stated that this occurred the day after the resident had an incident whereby his/her finger got caught in the bed frame which Emergency Services (ES) were required to release by cutting the metal bed frame. The RP stated that Resident #75 was sent to the hospital for evaluation of the finger and that the resident complained of pain the next day at the facility. The RP further stated that the Assistant Administrator stated that the hip fracture could have occurred when ES was moving the resident and that no further information was provided.
On 9/09/22 at 11:07 AM, the surveyor interviewed Resident #75's regular assigned Certified Nursing Assistant (CNA#1) who stated that the resident required total care although the resident could feed hem/herself. She further stated that the resident was confused and could answer simple questions.
On 9/09/22 at 11:39 AM, the surveyor observed Resident #75 in the day room wearing a mask and seated in high back wheelchair.
The surveyor reviewed the electronic medical record (EMR) for Resident #75.
Review of the residents admission Record (an admission summary) reflected that the resident had diagnoses which included but were not limited to: Alzheimer's Disease, repeated falls and fracture of unspecified part of the neck of the right femur (hip).
Review of the annual Minimum Data Set (MDS), an assessment tool used to facilitate the management of care, dated 12/9/21, reflected the resident had a Brief Interview for Mental Status (BIMS) score of 6 out of 15, which indicated that the resident had a severe impaired cognition. Further review of the MDS reflected that the resident required limited assistance (resident highly involved with activity; staff provide guided maneuvering of limbs or other non-weight-bearing assistance) with the physical assistance of two people.
Review of the Individual Comprehensive Care Plan (ICCP) reflected a focus area for pain initiated on 12/4/20 and revised on 3/9/22, which indicated that the resident had potential for pain related to impaired mobility and frequent falls. The ICCP also reflected that on 1/19/22, the resident had Right Leg/hip pain (Right hip fracture). Interventions initiated on 12/4/20, included Monitor/record/report to nurse any s/s (signs/symptoms) of non-verbal pain . vocalizations (grunting, moans, yelling out, silence, as well as Monitor/record/report to nurse, residents' complaints of pain .
Review of Resident #75's Progress Notes reflected the following:
On 1/18/22 at 7:32 AM, a Nurses' Note reflected that at 5:45 am nurse on unit called the undersigned supervisor and notified that Resident #75 got finger stuck in (a hole) the bed frame and Resident #75 was unable to get his/her finger out. Undersigned went to the unit to assess, finger swollen and not able to get out. Resident #75 doesn't know how his/her finger got in the hole. Resident #75 was sleeping and when Resident #75 woke up, Resident #75's finger was stuck. 911 was called, requested for the fire department to come. Fire department, EMT [emergency medical transport] and police arrived, they had to cut the frame of the bed to release Resident #75's finger. The finger was assessed and noted as bruised, swollen, and painful. [Physician] notified, order to transport to emergency room (ER) for further evaluation. Spouse [name redacted] notified. Resident #75 left the facility at 7:18 AM, all pertinent paperwork was sent with the resident to the ER.
On 1/18/22 at 12:19 PM, a Nurses' Note reflected that the Resident returned from hospital from jammed right finger of the right hand .no c/o (complaint of) pain or discomfort, head to toe completed. Redness and swelling to right hand finger closest to pinky finger, abrasion noted, X-ray 3 views done, negative .New order 600 mg (milligrams) Ibuprofen Q (every) 6 hrs. PRN (as needed) .
On 1/18/22 at 2:52 PM, Resident #75's primary physician saw and examined Resident #75 and there was no notation of any pain or discomfort to the finger or any other area of the body.
On 1/19/22 at 9:19 AM, a Nurses' Note reflected that Nurse notified by [agency] CNA resident c/o rt (right) leg and rt hip pain during AM care, nurse assessed Resident #75 and notified MD (physician), MD rx (prescribed) x-ray; 2 view for rt [right] hip and rt [right] leg will fu [follow up] with results.
On 1/19/22 at 9:25 AM, there was an Orders-Administration Note which reflected that Resident #75 was administered 600 mg of Ibuprofen due to complaint of pain in the lower extremity.
On 1/19/22 at 12:25 PM, a Nurses' Note reflected that the x-ray results showed a subcapital fracture to the right hip and that the physician and the RP were made aware.
On 1/19/22 at 2:40 PM, a Nurses' Note reflected that the resident was transported to the hospital and that the RP was present.
On 1/26/22 at 7:06 PM, a Nurses' Note reflected that the Resident returned to facility at approximately 5:45 PM . resident underwent operative procedure of the right hip, post op-site has approximately 30-40 staples .
A review of the investigation signed and dated on 1/19/22 by the Director of Nursing (DON) as Investigation summary completed was provided by the Regional Registered Nurse, reflected that it was an Injury of unknown origin for a Right hip fracture. There was no documented evidence of staff or ES personnel statements. The timeline did not include staff names for identification, nor specific time stamped accounts. The conclusions were indicated as follows: Investigation and interviews revealed that the injury most likely occurred during the incident and transfer which occurred on 1/18/22. There was no evidence to conclude that [resident] had a fall which resulted in a fracture of his/her right hip. The incident on 1/18/22 that involved the EMS/Local fire department to break his/her bed frame, release his/her finger and transfer him/her to the ER for evaluation may have possibly caused this injury. There was also no evidence of incidents (per hospital records) that may have occurred while at the hospital.
On 9/15/22 at 11:45 AM, the surveyor interviewed the resident's assigned Licensed Practical Nurse/Unit Manager (LPN/UM#1) who stated that the intermittent confusion and was at high risk for falls. LPN/UM#1 stated that the resident had an incident that his/her finger got stuck in the bed side rail and ES had to be called to remove it. LPN/UM#1 stated that the way ES positioned the resident may have caused the fracture but that LPN/UM#1 was not there at the time. She also stated that LPN/UM#1 did not conduct the investigation and that the hospital was trying to figure that out; the facility did not come up with this. LPN/UM#1 also stated that because they figured out what happened this was not considered an injury of unknown origin.
At 12:21 PM, the surveyor interviewed the DON and the Chief Nursing Officer (CNO) in the presence of two surveyors. They stated that an injury of unknown origin would prompt an investigation of abuse.
At 1:15 PM, the DON acknowledged that the investigation was an injury of unknown origin for a right hip fracture. The DON stated that the morning after the resident's finger got stuck in the bed frame and was sent to hospital, he/she complained of hip pain. The DON acknowledged there were no statements available within the investigation. The DON stated that the conclusion after the investigation and interviews was that the fracture most likely occurred upon Resident #75's transfer on 1/18/22. The DON stated that the transfer, may have possibly caused injury. The DON acknowledged that there was no documented evidence of interviews with the EMS personnel. In addition, the DON stated that she did not report this incident and could not speak to the rationale.
At 1:22 PM, the DON stated that the conclusion was not put together. The DON stated that she would try to document interviews depending on if she spoke with the person while in the car or in person. The DON stated that interviews could have been conducted by phone or written as well. The DON acknowledged that there was no documented evidence within the investigation of interviews conducted. The DON stated that the occurrence was probably related to and most likely occurred during Resident #75's transfer. She could not produce documented evidence that led to this conclusion.
On 9/16/22 at 12:23 PM, the DON provided the requested medical record information for Resident #75, however, she did not provide any further information related to the investigation.
On 9/20/22 at 11:38 AM, the surveyor conducted a phone interview with the resident's assigned 11-7 CNA#2. The CNA#2 stated that she attempted to perform incontinence care for the resident when she noticed that the resident could not move well and was screaming in pain. The CNA#2 stated that the resident implied the pain was in his/her hands. The CNA#2 stated that she requested assistance from two other male aides to change the resident's brief. The CNA#2 added that Resident #75 was of large stature and that CNA#2 could not have hurt him/her. The CNA#2 stated that Resident #75 was resistant to care at times and difficult to move. The CNA#2 further stated that the resident was confused and had a history of falls and so she checked on Resident #75 often. The CNA#2 stated that the resident did not have a fall on her shift. She could not recall if she reported this to the nurse and stated that she did not see any bodily injuries on Resident #75. The CNA#2 also stated that she had been educated on abuse and in that event, she should report abuse to her supervisor or an administrator staff member. She stated that if a resident had an injury that could not be explained that the facility should have investigated it.
On that same date at 11:47 AM, the Licensed Nursing Home Administrator (LNHA) stated that an injury of unknown origin should have been reported if it occurred in the facility. After reviewing the facility's policy in the presence of the surveyor, the LNHA stated that the facility's policy for reporting should have occurred within 24 hours of the event.
REFER to F689
5. On 9/01/22 at 11:32 AM, the surveyor observed Resident #191 reclining back in his/her geri-chair in their room. The surveyor attempted to interview the resident. The resident was able to communicate his/her name to the surveyor.
The surveyor reviewed the medical record for Resident #191.
A review of the resident's admission Record reflected that Resident #191 had resided at the facility for about a year and had diagnoses which included but were not limited to cerebral palsy (a congenital disorder that affects movement, muscle tone and posture due to abnormal brain development before birth), lobar pneumonia, unspecified organism, unspecified severe protein calorie malnutrition, schizophrenia, major depressive disorder, anxiety, unspecified intellectual disabilities, essential hypertension, and gastro-esophageal reflux disease without esophagitis (inflammation that damages the tube running from the throat to the stomach).
A review of the resident's quarterly Minimum Data Set (MDS), an assessment tool used to facilitate the management of care dated 3/24/2022, reflected that Resident #191 had a Brief Interview for Mental Status score of 6 out of 15, which indicated Resident #191 had moderately impaired cognition. Further review of Resident #191's MDS, Section K - Swallowing/Nutritional Status did not indicate that Resident #191 was on a mechanically altered diet that would require a change in texture of foods or liquids.
A review of a Progress Note (PN) dated 5/27/2022, and timed at 14:30 (2:30 PM) indicated that while Resident #191 was in the dayroom during snack time, staff informed nursing that Resident #191 was choking and vomiting. The PN further explained that Resident #191 had a Physician's Order (PO) for honey thickened liquids and was given thin milk by an unknown staff member. The PN revealed that Resident #191 was evaluated by the Licensed Practical Nurse (LPN#3). Upon evaluation, the LPN#3 heard crackles throughout the resident's lungs, the resident's vital signs were abnormal, and the resident's physician was notified immediately. Upon notification of the physician, the physician provided the LPN#3 with physician orders for Resident #191 to be administered oxygen and a nebulizer treatment. The PN further indicated that the physician came to the unit, assessed Resident #191 and decided to send Resident #191 to the hospital.
A further review of Resident #191's PN dated 5/27/2022, and timed at 22:35 (10:25 PM) reflected that Resident #191 was admitted to the hospital with possible aspiration pneumonia (occurs when food or liquid is breathed into the airway of the lungs, instead of being swallowed).
A review of the resident's hospital discharge paperwork from 5/27/2022 through 6/09/2022, reflected a discharge diagnosis of aspiration which was identified on a chest x-ray. A further review of Resident #191's hospital paperwork indicated that Resident #191 required placement of a peg-tube (a creation of an artificial external opening in the stomach for nutritional support).
A review of Resident #191's Order Audit Report throughout Resident's #191's stays at the facility revealed a PO dated 5/27/2022, and timed at 10:37 AM for regular diet puree texture, honey thickened liquid consistency.
A review of Resident #191's Diet Order Timeline indicated that on 5/27/2022, the Speech Language Pathologist (SLP) recommended downgrading Resident #191's diet to puree texture, honey thick liquid consistency. Upon the SLP recommendation, the order was approved by the physician.
A review of the facility's Investigation of the incident dated 6/08/2022, and signed by the DON indicated that in conclusion Resident #191 was provided regular thin liquids when his/her current diet indicated honey thickened liquids. The investigation revealed Resident #191 received the incorrect fluid consistency during snack time and the incident most likely occurred due to lack of knowledge by staff regarding proper protocols in verifying fluid consistencies.
On 9/15/22 at 11:30 AM, the surveyor interviewed Resident #191's Registered Nurse (RN) who stated anything that resembles abuse should be reported immediately to supervisory staff. The RN was unsure of time frames for reporting abuse and incidents and accidents that resulted in physical harm to a resident.
On 9/15/22 at 11:52 AM, the surveyor interviewed the Licensed Practical Nurse/Unit Manager (LPN/UM#2) who stated that abuses needed to be reported and investigated immediately. The LPN/UM#2 further stated that an incident or accident that occurred that caused a resident distress and required hospitalization would be reported to the facility management immediately by LPN/UM and LPN/UM would in-service staff on the event to prevent further incidents from occurring. The LPN/UM#2 could not speak to time frames for reporting to the NJDOH.
On 9/15/22 at 12:57 PM, the surveyors interviewed the CNO and the DON and asked the question, How long after a serious bodily injury occurred to a resident would it be reported? The CNO and DON did not know and stated that they would have to get back to the surveyors with that answer. The surveyors never received a response from the CNO and DON. The DON stated that DON did not report the incident for Resident #191 because the incident involved one Certified Nursing Assistant (CNA#4), an investigation was initiated and the staff member was re-educated that day.
On 9/20/22 at 11:28 AM, the surveyor interviewed the facility's Administrator (Admin) who stated the DON was the head abuse investigator at the facility and was in charge.
At 11:50 AM, the Admin stated that if Resident #191 had serious bodily injury due to abuse, then it would be reported to the NJDOH within two hours according to the facility's abuse policy and procedure. The Admin told the surveyor that Resident #191 was harmed and had an adverse reaction due to being administered whole thin milk, but it was not based off carelessness or lack of education because the CNA#4 was educated prior to the event. The Admin stated that the incident occurred due to, human error. The Admin did not speak to the proper procedure the CNA#4 should have performed based off the prior education the CNA#4 received.
A review of the facility's Abuse Investigating and Reporting Policy and Procedure revised 05/2022 included, All reports of resident abuse, neglect, exploitation, misappropriation of resident property, mistreatment, and/or injuries of unknown source (abuse) shall be promptly reported to local state and federal agencies (as defined by current regulations) and thoroughly investigated by facility management. Findings of abuse investigations will also be reported.
In addition, the facility's Abuse Investigating and Reporting Policy and Procedure revised 05/2022 indicated, 1. All alleged violations involving abuse, neglect, exploitation, or mistreatment, including injuries of an unknown source and misappropriation of property will be reported to the facility Administrator, or his/her designee, to the following persons or agencies: a. State licensing certification agency responsible for surveying/licensing the facility; b. The local/State Ombudsman; c. The Resident Representative (Sponsor) of Record; d. Law enforcement officials; The resident's Attending Physician 2. An alleged violation of abuse, neglect, exploitation or mistreatment (including injuries of unknown source and misappropriation of resident property) will be reported immediately, but no later than: a. Two (2) hours if the alleged violation involves abuse or has resulted in serious bodily injury; or b. Twenty-four (24) hours if the alleged violation does not involve abuse and has not resulted serious bodily injury.
NJAC 8:39-9.4(e)(f)
2. On 8/31/22 at 11:02 AM, the surveyor observed Resident #228 in the hallway self-propelling a wheelchair. The resident said hello to the surveyor and stated that he/she would be willing to talk to the surveyor at another time.
On 9/1/22 at 11:09 AM, the surveyor interviewed Resident #228 in their room. The resident stated that he/she has lived in the facility approximately two years and was unable to care for him/herself and that the staff had done a good job caring for him/her.
The surveyor reviewed the medical record for Resident #228.
A review of the resident's admission Record reflected that the resident had diagnoses which included but were not limited to morbid (severe) obesity, diabetes, and major depressive disorder.
A review of the resident's quarterly Minimum Data Set (MDS), an assessment tool used to facilitate the management of care dated 8/11/2022, reflected that the resident had a Brief Interview for Mental Status (BIMS) score of 11 out of 15, which indicated the resident had moderately intact cognition.
A review of the resident's interdisciplinary care plan revealed a focus area dated 7/5/22, for an actual fall with no injury related to alcohol intoxication with interventions dated 7/3/22, sent out via 911 for evaluation.
A review of the facility's investigation Unwitnessed fall dated 7/3/2022, was provided by the Director of Nursing (DON) and prepared by the Licensed Practical Nurse (LPN#1) and signed by the Assistant Director of Nursing (ADON). The Incident Description indicated that At 7:00 PM, certified nursing aide reported to the nurse that resident was yelling and cursing at other resident. Nurse went to resident and asked what was happening. Resident was very loud, disrespectful, cursing, throwing things, punching at the wall, and threatening to punch somebody. Nurse tried to calm him/her down but resident refused to calm down. He/she continue to wheel around the hallways threatening to hit somebody, throwing things. He/she wheeled himself to room [ROOM NUMBER], one of the patient in that room tried to ask him/her to calm down, he/she tried to hit the resident and the resident ran inside his/her room. A certified nursing aide who was taking care of another resident in that room closed the door to stop him/her from going inside, he/she tried to push the door open, banging on the door, threw him/her self on the floor, rolling on the floor and cursing.
In addition, the attached nursing progress note dated 7/3/22, at 11:43 PM, was included which indicated, Resident refused to be redirected or listen to anybody. Supervisor called police, telehealth and the family. The police came and helped get resident up from the floor back to his/her wheelchair. He/she was sent out to hospital for psych evaluation at 9:40 PM.
On 9/12/22 at 11:15 AM, the surveyor interviewed the DON who stated that investigations were discussed with a compliance team which usually consisted of the Licensed Nursing Home Administrator (LNHA), herself and other staff members depending on the individual case such as including the social worker or speech therapist. The DON added that the team discusses whether there was a need to report to the New Jersey Department of Health (NJDOH) which was based on the regulations. The DON explained that the meetings were not documented and the decision whether to report or not was not documented either.
On 9/15/22 at 12:57 PM, the surveyor, in the presence of two other surveyors, interviewed the CNO and the DON regarding the investigation dated 7/3/22, for Resident #228. The DON stated that she did not report the incident for Resident #228 because the compliance team had not felt that the incident was required to be reported to the NJDOH. The CNO stated that Resident #228 was not intentionally directing his/her actions towards another resident. The DON added that the compliance team had not felt that the incident was a resident-to-resident altercation. The DON stated that she thought the aggression of Resident #228 was more directed at the staff members that were trying to calm the resident down and not toward any other resident. The DON explained that she based whether to report immediately on a discussion with whoever was describing the situation and if it fell within guidelines would report immediately. The DON added that the Administrator could report, or she would instruct a supervisor to report to the NJDOH immediately.
At that time, the surveyor read out loud the Nursing Description from the Witnessed Fall investigation form which included, He/she wheeled him/herself to room [ROOM NUMBER], one of the patient in that room tried to ask him/her to calm down, he/she tried to hit the resident and the resident ran inside his/her room. The CNO then acknowledged that the situation could be interpreted differently.
On 9/15/22 at 2:19 PM, the survey team met with the LNHA and the DON. The LNHA stated that he had become the facility administrator on 9/5/22, and after reviewing the incident for Resident #228, acknowledged that the incident should have been reported and had the DON send a Reportable Event Record/Report to the NJDOH on 9/15/22, at 2:17 PM.
On 9/19/22 at 10:05 AM, the surveyor attempted to conduct a telephone with LPN#1 who had completed the Witnessed Fall form and was unsuccessful.
3. On 9/9/22 at 11:30 AM, the surveyor observed Resident #99 being wheeled by a Certified Nursing Aide (CNA#3) who stated to the resident that she was taking him/her to his/her room for changing before he/she was to go out with a resident representative.
The surveyor reviewed the medical record for Resident #99.
A review of the resident's admission Record revealed diagnoses which included hypertension (high blood pressure), major depressive disorder (mood disorder), cerebral palsy (a group of disorders that affect a person's ability to move and maintain posture), and schizophrenia (a disorder that affects a person's ability to think, feel and behave clearly).
A review of the quarterly Minimum Data Set (MDS), an assessment tool used to facilitate the management of care dated 7/30/22, reflected the resident had a BIMS score of 12 out of 15, indicating that the resident had a moderately intact cognition. In addition, the MDS Section B completed for Hearing, Speech and Vision reflected that the resident was usually able to make themselves understood and was usually able to understand others.
A review of the resident's interdisciplinary care plan (IDCP) revealed a Focus dated as initiated 6/19/2014, and revision on 1/4/2022, for Cognition. Resident #99 is alert & oriented to self, place, familiar faces. He/she has a flat affect. He/she has a diagnosis of schizophrenia. He/she has been noted as forgetful. The Interventions/Tasks included Communicate with the resident/family/caregivers regarding residents capabilities and needs.
Further review of the IDCP revealed a Focus dated as initiated 5/23/2019, and revision on 1/4/2022, for Resident has a communication problem, able to verbalize basic needs but has difficulty understanding others, this is due to diagnosis of dev[developmental] delayed, mental issues.
A review of a Grievance/Concern Form dated 3/30/22 provided by the DON for Resident #99 revealed [Resident representative (RR)] reported that Resident #99 has scratches -he/she said staff scratch his/her legs. In addition, an Unknown investigation dated 3/21/22, was provided by the DON which was completed by the Licensed Practical Nurse/Unit Manager (LPN/UM#1) included an Incident Description which indicated, While resident on home visit, resident representative noticed scratch marks on left lower extremity. RR stated, when he/she asked Resident #99 stated, while dressing him/her they scratch his/her legs. When nurse spoke with Resident #99, he/she stated, sometimes when he/she feels itchy, he/she does scratch him/herself. Head to assessment completed no other changes in skin, skin intact. Vital signs blood pressure 128/89 heart rate 75 respirations 19 temperature 97.2 no pain or discomfort noted. Physician made aware, bacitracin to left lower extremity for 5 days. Will continue to monitor.
On 9/12/22 at 11:15 AM, the surveyor interviewed the DON who stated that investigations were discussed with a compliance team which usually consisted of the LNHA, herself and other staff members depending on the individual case such as including the social worker or speech therapist. The DON added that the team discusses whether there was a need to report to the NJDOH that was based on the regulations. The DON explained that the meetings were not documented and the decision whether to report or not was not documented either.
On 9/15/22 at 11:30 AM, the surveyor attempted to interview Resident #99 who answered yes and no to questions and would not elaborate and preferred to not answer any more questions. The resident answered no when asked if he/she had any issues or concerns with the staff, medications or living at the facility.
On 9/15/22 at 11:40 AM, the surveyor interviewed the LPN/UM#1 who stated that she had completed the Unknown investigation dated 3/31/22, and gave it to the DON and the DON completed the Grievance/Concern Form dated 3/30/22. The LPN/UM#1 added that the resident was not comfortable speaking with people he/she doesn't know and would get annoyed and doesn't like being bothered. The LPN/UM#1 stated that she was unsure if an investigation with statements was needed because it was known that the incident was related to the resident. The LPN/UM#1 stated that the resident can tell you if something was bothering him/her. The LPN/UM#1 stated that when she asked the resident what had happened, the resident told her that he/she felt itchy and scratched his/her legs, so she didn't think that statements from staff were needed. The LPN/UM#1 then stated that the resident was not confused but very forgetful and was fairly reliable. The LPN/UM#1 could not speak to reporting abuse.
On 9/15/22 at 12:57 PM, the surveyor, in the presence of two other surveyors, interviewed the CNO and the DON regarding the Grievance /Concern Form dated 3/30/22, and investigation dated 3/31/22, for Resident #99. The DON stated she was involved in reporting to the NJDOH and would initiate an investigation of abuse for any resident concern that falls under the abuse policy and any and all allegations of abuse or injury of unknown origin. The DON added that the process for an allegation of abuse was if reportable then assess if resident safe in immediate moment, do an investigation and speak with the person or resident, take staff off assignment depending on the allegation. The CNO stated that Resident #99 was able to articulate what had happened then it was not an allegation of abuse. The DON added that she felt the resident could speak for themselves. The DON explained that she based whether to report immediately on a discussion with whoever was describing the situation and if it fell within guidelines would report immediately. The DON added that the Administrator could report, or she would instruct a supervisor to report to the NJDOH immediately if needed. The CNO and DON would not speak to the RR statement that he/she was told by Resident #99 that the scratches were from staff.
4. On 9/9/22 at 11:30 AM, the surveyor observed Resident #99 being wheeled by a CNA#3 who stated to the resident that she was taking him/her to his/her room for changing before he/she was to go out with a resident representative.
The surveyor reviewed the medical record for Resident #99.
A review of the resident's admission Record revealed diagnoses which included hypertension (high blood pressure), major depressive disorder (mood disorder), cerebral palsy(a group of disorders that affect a person's ability to move and maintain posture), and schizophrenia (a disorder that affects a person's ability to think, feel and behave clearly).
A review of the quarterly Minimum Data Set (MDS), an assessment tool used to facilitate the management of care dated 7/30/22, reflected the resident had a BIMS score of 12 out of 15, indicating that the resident had a moderately intact cognition. In addition, the MDS Section B completed for Hearing, Speech and Vision reflected that the resident was usually able to make themself understood and was usually able to understand others.
A review of the resident's IDCP revealed a Focus dated as initiated 6/19/2014, and revision on 1/4/2022, for Cognition indicated Resident #99 is alert & oriented to self, place, familiar faces. He/she has a flat affect. He/she has a diagnosis of schizophrenia. He/she has been noted as forgetful. The Interventions/Tasks included Communicate with the resident/f[TRUNCATED]
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Investigate Abuse
(Tag F0610)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** REFER to 609
Based on interview, observation, and record review, it was determined that facility failed to conduct a timely and ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** REFER to 609
Based on interview, observation, and record review, it was determined that facility failed to conduct a timely and through investigation, as well as, follow their own facility policy on Abuse Investigation and Reporting was consistently implemented for five (5) of six (6) residents (Resident #27, #75, #99, #102 and #228) reviewed for alleged violation investigations.
This deficient practice was evidenced by the following:
1. On [DATE] at 11:28 AM, the surveyor interviewed the responsible party (RP) for Resident #75 in the presence of a second surveyor. The RP informed the surveyors that Resident #75 sustained a right hip fracture which required surgery. The RP stated that this occurred the day after Resident #75 had an incident whereby his/her finger got caught in the bed frame which Emergency Services (ES) were required to release by cutting the metal bed frame. The RP stated that Resident #75 was sent to the hospital for evaluation of the finger and that the resident complained of pain the next day at the facility. The RP further stated that the Assistant Administrator (AA) stated that the hip fracture could have occurred when ES was moving the resident and that no further information was provided.
On [DATE] at 11:07 AM, the surveyor interviewed the resident's regular assigned Certified Nursing Assistant (CNA#1) who stated that Resident #75 required total care although the resident could feed him/herself. She further stated that the resident was confused and could answer simple questions.
On [DATE] at 11:39 AM, the surveyor observed Resident #75 in the day room wearing a mask and was seated in a high back wheelchair.
The surveyor reviewed the electronic medical record (eMAR) for Resident #75.
Review of the admission Record (an admission summary) reflected that the resident had diagnoses which included but were not limited to Alzheimer's Disease, repeated falls and fracture of unspecified part of the neck of the right femur (hip).
Review of the annual Minimum Data Set (MDS), an assessment tool used to facilitate the management of care, dated [DATE], reflected that the resident had a Brief Interview for Mental Status (BIMS) score of 6 out of 15, which indicated that the resident had severe cognitive impairment. Further review of the MDS reflected that the resident required limited assistance (resident highly involved with activity; staff provide guided maneuvering of limbs or other non-weight-bearing assistance) with the physical assistance of two people.
Review of the Individual Comprehensive Care Plan (ICCP) reflected a focus area for pain initiated on [DATE] and revised on [DATE], which indicated that the resident had potential for pain related to impaired mobility and frequent falls. It also reflected that on [DATE], the resident had Right leg/hip pain (Right hip fracture). Interventions initiated on [DATE], included Monitor/record/report to nurse any s/s (signs/symptoms) of non-verbal pain . vocalizations (grunting, moans, yelling out, silence, and Monitor/record/report to nurse, residents' complaints of pain .
Review of Resident #75's Progress Notes reflected the following:
On [DATE] at 7:32 AM, a Nurses' Note reflected that at 5:45 am nurse on unit called the undersigned supervisor notifying that patient got [resident] finger stuck in the bed frame (a hole) in the bed frame and [resident] is unable to get his finger out. Undersigned went to the unit to assess, finger swollen and not able to get out. Patient report [resident] doesn't know how [resident] finger got in the hole [resident] was sleeping and when [resident] woke up, [resident] finger was stuck. 911 called, requested for the fire department to come. Fire department, EMT (emergency medical transport) and police arrived, they had to cut the frame of the bed to release [resident] finger, finger noted bruised and swollen and painful. [Physician] notified, order to transport to ER (emergency room) for further evaluation. Spouse [name redacted] notified. All pertinent paperwork sent with patient to ER left facility at 7:18 am.
On [DATE] at 12:19 PM, a Nurses' Note reflected that Resident returned from hospital from jammed right finger of the right hand .no c/o (complaint of) pain or discomfort, head to toe completed. Redness and swelling to right hand finger closest to pinky finger, abrasion noted, X-ray 3 views done, negative .New order 600 mg (milligrams) Ibuprofen Q (every) 6 hrs. PRN (as needed) .
On [DATE] at 2:52 PM, Resident #75's primary physician saw and examined Resident #75 related to Resident #75's finger and there was no notation of any pain or discomfort to the finger or any other area of the body.
On [DATE] at 9:19 AM, a Nurses' Note reflected that Nurse notified by [agency] CNA resident c/o rt (right) leg and rt hip pain during AM care, nurse assessed Resident #75 and notified MD (physician), MD rx (prescribed) xray 2 view for rt hip and rt leg will fu (follow up) with results.
On [DATE] at 9:25 AM, there was an Orders-Administration Note which reflected that Resident #75 was administered 600 mg of Ibuprofen due to Resident #75's complaint of pain in the lower extremity.
On [DATE] at 12:25 PM, a Nurses' Note reflected that the x-ray results showed a subcapital fracture to the right hip and that the physician and the RP was made aware.
On [DATE] at 2:40 PM, a Nurses' Note reflected that Resident #75 was transported to the hospital and that the RP was present.
On [DATE] at 7:06 PM, a Nurses' Note reflected that Resident returned to facility approximately at 5:45 PM . resident underwent operative procedure of the right hip, post op site has approximately 30-40 staples .
Review of the investigation provided by the Regional Registered Nurse (RRN) on [DATE] at 12:56 PM, reflected that it was an Injury of unknown origin for a Right hip fracture. There was no documented evidence of staff or ES personnel statements. The timeline did not include staff names for identification, nor specific time stamped accounts. The conclusions were indicated as follows: Investigation and interviews reveal that the injury most likely occurred during the incident and transfer which occurred on [DATE]. There is no evidence to conclude that [resident] had a fall which resulted in a fracture of his/her right hip. The incident on [DATE] that involved the EMS/Local fire department to break his/her bed frame, release his/her finger and transferred him/her to ER for evaluation may have possibly caused this injury. There was also no documented evidence of incidents (per hospital records) that may have occurred while at the hospital. This was signed and dated by the Director of Nursing (DON) as Investigation summary completed on [DATE].
On [DATE] at 11:45 AM, the surveyor interviewed Resident #75's assigned Licensed Practical Nurse/Unit Manager (LPN/UM). She stated Resident #75 had intermittent confusion and was at high risk for falls. The LPN/UM stated that Resident #75 had an incident that his/her finger got stuck in the bed side rail and the ES had to be called to remove it. The LPN/UM also stated that the way ES positioned Resident #75 may have caused the fracture but that the LPN/UM was not there at the time. The LPN/UM further stated that LPN/UM did not conduct the investigation and that the hospital was trying to figure that out; the facility did not come up with this. The LPN/UM stated that because they figured out what happened this was not considered an injury of unknown origin.
On that same date at 12:21 PM, the surveyor interviewed the DON and the Chief Nursing Officer (CNO) in the presence of two additional surveyors. They stated that an injury of unknown origin would prompt an investigation of abuse.
On that same date at 1:15 PM, the DON acknowledged that the investigation was an injury of unknown origin for a right hip fracture. The DON stated that the morning after Resident #75's finger got stuck in the bed frame and was sent to hospital, he/she complained of hip pain. The DON acknowledged there were no statements available within the investigation. The DON stated that the conclusion after the investigation and interviews was that the fracture most likely occurred upon Resident #75's transfer on [DATE]. The DON stated that the transfer, may have possibly caused injury. The DON acknowledged that there was no documented evidence of interviews with the EMS personnel.
On that same date at 1:22 PM, the DON stated that the conclusion was not put together. The DON stated that she would try to document interviews depending on if she spoke with the person while in the car or in person. The DON stated that interviews could have been conducted by phone or in person. The DON acknowledged that there was no documented evidence within the investigation that interviews were conducted. The DON stated that the occurrence was probably related to and most likely occurred during Resident #75's transfer. The DON could not provide any documented evidence that led to this conclusion. She further stated, I would have to check that.
On [DATE] at 12:23 PM, the DON provided the requested medical record information for Resident #75, however, she did not provide any further information related to the investigation.
On [DATE] at 11:38 AM, the surveyor conducted a phone interview with Resident #75's 11-7 assigned Certified Nursing Assistant (CNA#2). The CNA#2 stated that she attempted to perform incontinence care for Resident #75 when she noticed that Resident #75 could not move well and was screaming in pain. The CNA#2 stated that Resident #75 implied the pain was in his/her hands. The CNA#2 stated that she requested assistance from two other male aides to change Resident #75's briefs. The CNA#2 added that Resident #75 was of large stature and that she could not have hurt him/her. The CNA#2 stated that Resident #75 was resistant to care at times and difficult to move. The CNA#2 further stated that Resident #75 was confused and had a history of falls and so she checked on Resident #75 often. The CNA#2 stated that Resident #75 did not have a fall on CNA#2's shift. She could not recall if she reported this to the nurse and stated that she did not see any bodily injuries on Resident #75. The CNA#2 also stated that she had been educated on abuse and in that event she should report abuse to her supervisor or an Administrative staff member. She stated that if a resident had an injury that could not be explained that the facility should have investigated it.
At 12:32 PM, the surveyor interviewed the AA who stated that he interviewed Resident #75 and the RP but could not speak to any other aspect of the investigation.
5. On [DATE] at 11:02 AM, the surveyor observed Resident#102 laying on the bed with the responsible party (RP) at the bedside. The RP stated that Resident#102 was cognitively intact, unable to speak appropriately but able to utilize the personal computer for communication. The RP further stated that at times the concern was with the 11-7 shift staff who think Resident#102 is cognitively impaired because Resident#102 is unable to talk properly due to ALS (Amyotrophic lateral sclerosis is a rare neurological disease that primarily affects the nerve cells responsible for controlling voluntary muscle movement like chewing, walking, and talking).
On [DATE] at 10:40 AM, the surveyor observed Resident#102 laying on the bed with the RP at the bedside. The RP showed the surveyor Resident#102's call bell. The RP stated that the flat call bell was specific for Resident#102 because Resident#102 was a quadriplegic due to ALS and that the call bell should be placed just below Resident#102's chin for Resident#102 to be able to call when needed. The RP further stated that there was an incident a while ago. The RP was unable to remember the exact date and the name of the Certified Nursing Aide (CNA) involved. The RP stated that the unknown CNA told the RP that Resident#102's call bell was not placed appropriately during the 11-7 shift. The RP told the surveyor this was immediately reported to the facility's management and the social worker.
Furthermore, the RP stated that the problem did not arise not until a week ago and was unable to remember the exact date and the name of the 11-7 shift CNA. The RP further stated that it was Resident#102 who informed the RP that the call bell was not placed where the resident would be able to use it. The RP indicated that it was reported to the SW.
On [DATE] at 11:18 AM, the surveyor asked the Registered Nurse/Unit Manager (RN/UM) for a copy of the resident's grievance reports and the RN/UM stated that she would get back to the surveyor.
The surveyor reviewed Resident #102's medical records:
The admission Record (an admission summary), indicated that Resident#102 had diagnoses that included ALS, quadriplegia (a symptom of paralysis that affects all limbs and body from the neck down), anemia (low blood count), dysarthria, and anarthria (anarthria is a severe form of dysarthria. Dysarthria is a motor speech disorder that occurs when someone can not coordinate or control the muscles used for speaking).
A review of Resident # 102's IDCP revealed a focus area for communication initiated on [DATE], and revised on [DATE], which indicated has communication deficit due dysarthria r/t (related to) dx (diagnosis) of ALS; she can speak slowly but his/her voice is very soft; he/she communicates with an electronic device (computer) via a sensor at the tip of his/her nose. The interventions included to ensure that Resident#102's personal computer for communication is functioning initiated on [DATE], and revised on [DATE], and and provide a chin tuck call bell in reach at all times initiated on [DATE], and revised on [DATE].
The [DATE], Quarterly Minimum Data Set (MDS), an assessment tool used to facilitate the management of care, indicated a BIMS score of 15 out of 15, which reflected that Resident#102's cognition was intact.
According to the [DATE], Grievance/Concern Form (G/C Form) that was provided by the LNHA showed that Resident#102 emailed the SW about the incident on [DATE] at 5:00 AM when the 11-7 shift CNA moved Resident#102's call bell away where Resident#102 was unable to reach it.
The [DATE] G/C Form included a list of attempts made to resolve the problem as follows:
-Met with RP/resident
-Trial specialty breath-bell (stationary difficult to move)
-Right side preferred for chin tuck call bell
-Stat in-service
On [DATE], G/C Form showed that the For Social Work Department Completion: information below was left blank that was signed by the SW:
Resolved:
Unresolved:
Date:
The [DATE] G/C Form attachments included the following:
a. [DATE] Nurses' Notes about UM (Unit Manager) discussed with RP that the preferred placement of the chin tuck call bell is the right side of the chin and the breath-activated call device trial was conducted and ineffective.
b. Communication care plan intervention for right side preferred for chin tuck call bell was initiated on [DATE].
c. In-service Sign-in Sheet dated [DATE] with Topic about Resident#102's call bell placement. There was 8 staff from the 7-3 shift and one who worked the 7-3 and 3-11 shift signed the in-service.
d. Patient Concern/Grievance Policy copy that was updated on 1/2022.
e. Grievance/Concern Form copy (blank form).
Further review of the [DATE] G/C Form revealed the following:
- The CNA's name was not able to be identified and there was no statement from the alleged CNA.
- The In-service Sign-in Sheet did not include the 11-7 shift staff when the alleged violation was concerning the 5 AM CNA.
- The part where the SW should complete was blank.
On [DATE] at 1:28 PM, the surveyor interviewed the DON and discussed the above concerns. The DON acknowledged that the [DATE], G/C Form and the investigation were incomplete.
On [DATE] at 9:30 AM, the surveyor interviewed the SW who stated that in the grievance process, the facility uses the Grievance/Concern Form that anyone can fill out the form and submit to the SW, then the SW will forward it to the involved department like if a broken TV, the form will be given to the Maintenance Department, then once completed, it will be returned to the SW for filing.
On that same date and time, the SW stated that in the area where the Social Work Department Completion, I put a checkmark to the resolved item and it was not necessary to put additional notes. When the surveyor asked the SW why the [DATE], G/C Form was not completed and there was no checkmark to indicate it was resolved, the SW stated, I don't know.
At that same time, the surveyor asked the SW who was the alleged CNA on the [DATE], grievance and the SW responded that she did not know who the CNA was. The SW further stated that she did not know why there was no statement from the CNA when the grievance form was sent back to the SW for filing.
Furthermore, the SW stated that she was not aware of what happened to the alleged CNA on the [DATE] grievance. She further stated, They do not share that piece of information with me. The surveyor then asked the SW if the social worker department was part of the ID (Interdisciplinary) team and if grievances were being discussed as part of the ID team meeting. The SW stated, yes, and the ID team never discussed the investigation with me with regard to staff, they keep it very private here for the privacy of the employees.
On [DATE] at 10:43 AM and 2:15 PM, the surveyor asked the DON for the name of the CNA from the [DATE] grievance. The DON stated that she would get back to the surveyor.
On [DATE] at 8:45 AM, the DON provided CNA's name and phone number on the [DATE] grievance.
On [DATE] at 11:44 AM, the surveyor interviewed the RN/UM regarding the [DATE] grievance report. The RN/UM informed the surveyor that on [DATE], the SW received an email that an incident occurred at 5:00 AM regarding a CNA who went to Resident#102's room and moved the call bell away from Resident#102. The RN/UM indicated that the SW sent an email to the DON and stated,I think the LNHA was included in the email regarding the incident.
On that same date and time, the RN/UM informed the surveyor that she was off on [DATE], and when she came back to work on [DATE], she immediately talked to Resident#102 and the RP about the [DATE] incident. The surveyor asked the RN/UM if she was able to identify the alleged CNA and the RN/UM stated, no, I asked all of the staff on that date and no one admitted to it. The surveyor asked the RN/UM if she documented the conclusion of the investigation and the RN/UM stated it was not documented and there were no written statements obtained from the staff.
On [DATE] at 9:17 AM, the surveyor informed the DON regarding the above concerns with the [DATE] investigation. The surveyor asked the DON how she was able to identify the CNA's name when the RN/UM indicated that the conclusion of the investigation did not specify who the alleged CNA was. The surveyor asked the DON why there were only eight (8) 7-3 shift staff who were given an in-service about the placement of the call bell when the incident happened on the 11-7 shift. The DON stated that she would get back to the surveyor.
On [DATE] at 2:19 PM, the survey team met with the LNHA, CNO, and DON and they were made aware of the above concerns.
On [DATE] at 10:23 AM, the surveyor attempted to conduct a telephone interview with the alleged CNA for the second time but was unable to.
On [DATE] at 11:59 AM, the surveyor interviewed the DON in the presence of the Assistant Nursing Home Administrator (ADON). The DON stated that on [DATE], the alleged CNA was in-serviced via telephone on call bell placement and confirmed that the alleged CNA was the assigned CNA for Resident #102 on the 11-7 shift.
On [DATE] at 1:56 PM, the survey team met with the LNHA, DON, and ADON and discussed the above concerns. There was no additional information provided.
A review of the Grievances & Patient Concern Policy that was provided by the DON with a revised date of [DATE] included Policy: This policy is to ensure that concerns are properly communicated and reported to the proper department in a timely fashion by streamlining the investigation process. Procedure: 1. If a resident/family member has a concern they can approach/contact any facility staff member or a resident concern form can be filled out. The concern will then be forwarded to social services. 2. Social Services will give each concern a number for reference and log each one for investigation in the Grievance Log kept in the Social Services office and follow up .4. At Morning Meeting/Department Head meeting, Social Services will discuss all outstanding concerns and/or resolutions. 5. At the completion of each concern investigation, Social Services will enter the resolution into the concern log
A review of the facility policy dated as revised 5/2022 for Abuse Prevention Program provided by the CNO and DON included that as part of the resident abuse prevention, the administration will: Identify and assess all possible incidents of abuse; and Investigate and report any allegations of abuse within timeframe's as required by federal requirements;
A review of the facility policy dates as revised 5/2022 for Abuse Investigation and Reporting provided by the CNO and DON included that All reports of resident abuse, neglect, exploitation, misappropriation of resident property, mistreatment, and/or injuries of unknown source (abuse) shall be promptly reported to local state and federal agencies (as defined by current regulations) and thoroughly investigated by facility management.
In addition, the Abuse Investigation and Reporting policy included that the individual conducting the investigation will, as a minimum: Interview any witnesses to the incident; Interview staff members (on all shifts) who have had contact with the resident during the period of the alleged incident; Interview the resident's roommate; Review all events leading up to the alleged incident. Also, Witness reports will be obtained in writing. Either the witness will write his/her statement and sign and date it, or the investigator may obtain a statement, read it back to the member, and have him/her sign and date it.
NJAC 8:39-4.1(a)(5), 27.1(a)
2. On [DATE] at 11:02 AM, the surveyor observed Resident #228 in the hallway self-propelling a wheelchair. Resident #228 said hello to the surveyor and stated that he/she would be willing to talk to the surveyor at another time.
On [DATE] at 11:09 AM, the surveyor interviewed Resident #228 in their room. Resident #228 stated that he/she has lived in the facility approximately two years and was unable to care for him/herself and that the staff has done a good job caring for him/her.
The surveyor reviewed the medical record for Resident #228.
A review of Resident #228's admission Record reflected that Resident #228 had diagnoses which included but were not limited to morbid (severe) obesity, diabetes, and major depressive disorder.
A review of Resident #228's quarterly Minimum Data Set (MDS), an assessment tool used to facilitate the management of care dated [DATE] reflected that Resident #228 had a Brief Interview for Mental Status (BIMS) score of 11 out of 15 which indicated Resident #228 had a moderately intact cognition.
A review of Resident #228's Interdisciplinary Care Plan (IDCP) dated [DATE], included an actual fall with no injury related to alcohol intoxication with interventions dated [DATE], sent out via 911 for evaluation.
A review of the facility's investigation Unwitnessed fall dated [DATE] was provided by the Director of Nursing (DON) and prepared by the Licensed Practical Nurse (LPN#1) and signed by the Assistant Director of Nursing (ADON). The Incident Description indicated that At 7:00 PM, certified nursing aide reported to the nurse that Resident #228 was yelling and cursing at other resident. Nurse went to Resident #228 and asked what was happening. Resident #228 was very loud, disrespectful, cursing, throwing things, punching at the wall, and threatening to punch somebody. Nurse tried to calm him/her down but Resident #228 refused to calm down. He/she continue to wheel around the hallways threatening to hit somebody, throwing things. He/she wheeled himself to room [ROOM NUMBER], one of the patients in that room tried to ask him/her to calm down, he/she tried to hit the resident and the resident ran inside his/her room. A certified nursing aide who was taking care of another resident in that room closed the door to stop him/her from going inside, he/she tried to push the door open, banging on the door, threw him/her self on the floor, rolling on the floor and cursing.
Included in the investigation was a statement from a Certified Nursing Aide (CNA#3) which reflected At 7 PM, I was in room [ROOM NUMBER] putting patient to bed, Resident #228 was at the door hitting the door and cursing patient. I ask Resident #228 to go to his/her room, he/she refused to leave. I call the nurse and the nurse call the supervisor. A fall risk evaluation, an updated IDCP, and a Possession, Consumption, or Intent to sell unauthorized or illegal substances policy and signature of the resident accepting and agreeing to the policy were also included in the investigation report. In addition, the nursing progress notes dated [DATE] at 11:43 PM were included with additional information that reflected Resident refused to be redirected or listen to anybody. Supervisor called police, telehealth, and the family. The police came and helped get Resident #228 up from the floor back to his/her wheelchair. He/she was sent out to hospital for psychiatric evaluation at 9:40 PM.
On [DATE] at 11:00 AM, the surveyor interviewed Resident #228 who stated that he/she would rather not discuss the incident that occurred on [DATE]. Resident #228 stated that the incident was all his/her fault and that the facility staff responded appropriately and that he/she was very embarrassed.
On [DATE] at 11:08 AM, the surveyor interviewed the Licensed Practical Nurse/Unit Manager (LPN/UM) who stated that LPN/UM was not working on the day of the incident but had heard that Resident #228 was verbally abusive and had a fall. The LPN/UM stated that when Resident #228 returned from the hospital with a diagnosis of alcohol intoxication that LPN/UM and the social worker (SW) had spoken to Resident #228 and he/she admitted to being intoxicated and agreed to sign the facility policy. The LPN/UM stated that LPN/UM did not know how Resident #228 obtained the alcohol because Resident #228 had not left the facility and thought an investigation was performed. The LPN/UM added that Resident #228 was embarrassed and had not discussed again with Resident #228 because he/she was very apologetic and had been compliant. The LPN/UM stated that LPN/UM could not speak to how the investigation was completed. The LPN/UM then stated that the investigation report goes to the DON.
On [DATE] at 11:24 AM, based on the room number indicated on the facility investigation report dated [DATE], the surveyor interviewed Resident #27 who stated that he/she remembered an incident that had occurred and had given a statement to the police that day. Resident #27 stated that Resident #27 had not spoken to any other staff member about the incident except the CNA#3 that was in his/her room and was seen after that day by his/her psychiatrist for a regular visit. Resident #27 also stated that he/she had a roommate on that day but that the roommate had since expired. Resident #27 explained that there was a resident who was in the hallway yelling and he/she had heard a lot of noise coming from the hallway. Then, Resident #27 added that he/she was in his/her room with a CNA#3 who protected him/her by keeping the door closed because Resident #228 was in the hallway and kept banging on the door so hard that the door was shaking. Resident #27 stated He/she scared the hell out of me. when speaking about Resident #228 banging on the door. Resident #27 stated that he/she was thankful that there was CNA#3 in the room with him/her. Resident #27 added that he/she was fine when it was all over and felt protected and was able to self-propel through the hallways by him/herself.
The surveyor reviewed the medical record for Resident #27.
A review of the resident's quarterly Minimum Data Set (MDS), an assessment tool used to facilitate the management of care dated [DATE] reflected that Resident #27 had a Brief Interview for Mental Status (BIMS) score of 14 out of 15 which indicated Resident #27 had an intact cognition.
There was no progress note for Resident #27 indicating that Resident #27 was involved in any incident or was spoken to by any staff member.
On [DATE] at 12:57 PM, the surveyor in the presence of two other surveyors, interviewed the CNO and the DON regarding the investigation dated [DATE] for Resident #228. The DON stated that DON thought the aggression of Resident #228 was more directed at the staff members that were trying to calm Resident #228 down and not toward any other resident. The DON acknowledged that the investigation was not completed and had not included a statement from the residents' in the room where the CNA#3 had kept the door closed, CNA statements who cared for Resident #228 that day, any staff that had observed the incident, the police report, or the hospital report.
On [DATE] at 11:47 AM, the survey team met with the LNHA and DON. The LNHA stated that he became the facility administrator on [DATE] and after reviewing the incident for Resident #228, had the DON send a Reportable Event Record/Report to the NJDOH on [DATE] at 2:17 PM, which included additional investigation information such as statements from Resident #27 and a SW's statement which was not included in the [DATE], Witnessed Fall investigation. The DON acknowledged that the investigation was incomplete and in addition had not included how Resident #228 obtained the alcohol.
On [DATE] at 10:05 AM, the surveyor attempted to conduct a telephone interview with the LPN#1 who had completed the Witnessed Fall form and was unsuccessful.
On [DATE] at 11:25 AM, the surveyor was provided by the DON additional investigation information dated [DATE] for the incident which occurred on [DATE] which included CNA statements, police report information, the hospital report, and a conclusion as to how Resident #228 obtained alcohol and a plan for follow-up. The DON acknowledged that the additional information should have been completed in the investigation dated [DATE].
On [DATE] at 9:56 AM, the surveyor interviewed the CNA#3 via telephone who stated that CNA#3 worked for an agency and had not worked at the facility since the beginning of July. The CNA#3 recalled that CNA#3 had seen Resident #228 going crazy in the hallway and explained that Resident #228 was wheeling him/herself around hitting things, pushing things over and tipped over the linen cart. The CNA#3 added that CNA#3 was assigned Resident #27 and was taking care of Resident #27. The CNA#3 stated I had to lock the door so Resident #228 would not come inside and hurt my resident. The CNA#3 also stated that Resident #27 was scared and that after the incident spoke with the police. The CNA#3 then said that CNA#3 had to write a statement. The CNA#3 added that Resident #228 was not on Resident #228's assignment and lived far down the hallway. The CNA#3 was unsure if there were any other residents [TRUNCATED]
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected multiple residents
3. On 9/9/22 at 12:25 PM, the surveyor observed Resident #177 in his/her room out of bed and sitting on his/her wheelchair, awake, alert, and appropriately responded to the surveyor's inquiry.
The su...
Read full inspector narrative →
3. On 9/9/22 at 12:25 PM, the surveyor observed Resident #177 in his/her room out of bed and sitting on his/her wheelchair, awake, alert, and appropriately responded to the surveyor's inquiry.
The surveyor reviewed the medical records of Resident #177.
The admission Record revealed that Resident #177 was admitted to the facility with diagnoses that included but not limited to Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema, bilateral (high blood sugar that affected the eyes) and major depressive disorder, recurrent, unspecified.
The admission MDS (AMDS) with an ARD date of 7/21/22, indicated a BIMS score of 14 out of 15 under Section C, which indicated that the resident had an intact cognition.
Review of the 7/15/22, BIMS assessment section in the Assessment tab of the electronic medical record reflected a BIMS score of 13, which did not accurately reflect the coding in the 7/21/22, AMDS under Section C.
The surveyor could not locate a BIMS interview that supported the coding under Section C in the 7/21/22 AMDS, within the look-back period in the resident's electronic medical records (EMR).
4. On 9/1/22 at 10:54 a.m., the surveyor observed Resident #206 sitting in his/her wheelchair in the hallway in front of his/her room door awake, alert, calm, and appropriately responded to the surveyor's inquiry during a unit tour.
The surveyor reviewed the medical records of Resident #206.
The admission Record reflected that Resident #206 was admitted to the facility with diagnoses that included but were not limited to epilepsy, unspecified, not intractable, without status epilepticus (a disorder of the brain causing temporary and uncontrolled abnormalities in muscle movements) and unspecified dementia, unspecified severity, without behavioral disturbance, psychotic disturbance, mood disturbance, and anxiety (a brain disorder that causes problems with thinking, memory, and behavior).
The quarterly MDS ARD dated 8/4/22, indicated a BIMS score of 8 out of 15, which reflected that the resident's cognition was moderately impaired. Section C 0100 was coded 1. Yes and was signed by the SW#1 on 8/13/22.
The above 8/4/22, quarterly MDS was signed by SW#1, 9 days after the ARD.
Review of the 8/4/22, quarterly Assessment in the Assessment tab of the EMR reflected that Section C for the BIMS was not completed.
Review of the PN for SSN in the EMR reflected that the last documented note was dated 10/29/21. The quarterly MDS ARD date of 2/3/22, indicated a BIMS score of 7 out of 15, which indicated that the resident had moderately impaired cognition. Section C 0100 was coded 1, yes, and signed by the SW#3 on 2/24/22.
The above 2/3/22, quarterly MDS was signed by the DSW, 21 days after the ARD.
Review of the 2/3/22 quarterly assessment in the Assessment tab of the EMR reflected that section C for the BIMS was not completed.
Review of the annual MDS ARD dated 11/4/21, indicated a BIMS score of 7 out of 15, which indicated that the resident had moderately impaired cognition. Section C 0100 was coded 1. yes, and signed by the SW#3 on 2/24/22.
On 9/8/22 at 10:12 AM, two surveyors interviewed MDS Coordinator. The surveyor asked the MDS Coordinator if she checked for coding accuracy entered in the MDS within the ARD period before locking the MDS assessment for submission. The MDS Coordinator could not provide an answer and stated, It is the best we can do.
Furthermore, the MDS Coordinator stated that she was aware that the BIMS in the Assessment tab in EMR was not being completed. The surveyor asked the MDS Coordinator who was responsible for checking if the BIMS interviews in the Assessment tab were completed. The MDS Coordinator stated, we were in the middle of figuring that out. she acknowledged that all interview sections in the MDS assessments should have been conducted and completed within the ARD look-back period, not after the ARD.
On 9/15/22 at 2:19 p.m., the survey team met with the LNHA, DON, and CNO and discussed the above MDS findings. There was no additional information provided.
Based on observation, interview, and record review, it was determined that the facility failed to accurately assess and properly code residents' status in the Minimum Data Set (MDS), an assessment tool used to facilitate the management of care. This deficient practice was identified for 7 of 39 residents (Residents #13, #69, #102, #106, #177, #198 and #206) reviewed under Section C for cognition.
This deficient practice was evidenced by the following:
According to the CMS's (Centers for Medicare & Medicaid Services) RAI (Resident Assessment Instrument) Version 3.0 Manual dated October 2019 Section C: Cognitive Patterns included Coding Tips .If the resident interview was not conducted within the look-back period (preferably the day before or the day of) the ARD (Assessment Reference Date), item C 0100 must be coded 1, Yes, and the standard no information code (a dash -) entered in the resident interview items.
1. During an observation on 8/31/22 at 10:54 AM by the surveyor, the Certified Nursing Aide (CNA) was inside the resident's room while providing morning care to the resident.
The surveyor reviewed the medical records of Resident #69.
The admission Record (admission summary) reflected that Resident #69 was admitted to the facility with diagnoses that included but were not limited to paraplegia unspecified (paralysis that affects all or part of the trunk, legs, and pelvic organs) and multiple sclerosis (a neurological disease that causes dizziness, mobility problems, numbness, and fatigue.)
The quarterly MDS (MDS) ARD 6/23/22, indicated a Brief Interview for Mental Status (BIMS) score of 15 out of 15, which reflected that Resident #69's cognition was intact. The C 0100 was coded 1, yes, and signed by Social Worker #1 (SW#1) on 6/04/22.
The above 6/23/22, MDS was signed by SW#1, 19 days before the ARD.
The 6/23/22, Quarterly Assessment in the Assessment tab of the electronic medical record showed that Section C for the BIMS was not completed.
Review of the Progress Notes (PN) for Social Service Note (SSN) in the electronic medical record showed that the last documented note was dated 4/19/22.
2. On 8/31/22 at 11:02 AM, the surveyor observed Resident#102 laying on the bed with the responsible party (RP) at the bedside. The RP stated that the resident is cognitively intact, unable to speak appropriately but able to utilize the personal computer for communication. The RP further stated that Resident#102 was unable to talk properly due to ALS (Amyotrophic lateral sclerosis is a rare neurological disease that primarily affects the nerve cells responsible for controlling voluntary muscle movements like chewing, walking, and talking).
The surveyor reviewed the medical records of Resident #102.
The admission Record reflected that Resident#102 was admitted to the facility with diagnoses that included but were not limited to ALS, quadriplegia (a symptom of paralysis that affects all limbs and body from the neck down), anemia (low blood count), dysarthria, and anarthria (anarthria is a severe form of dysarthria. Dysarthria is a motor speech disorder that occurs when someone can not coordinate or control the muscles used for speaking).
The MDS ARD dated 8/18/22, indicated a BIMS score of 15 out of 15, which reflected that the resident's cognition was intact. The C 0100 was coded 1, yes, and signed by SW#2 on 8/29/22.
The above 8/18/22, MDS was signed by SW#2, 11 days after the ARD.
The 8/11/22, quarterly Assessment in the Assessment tab of the electronic medical record showed that Section C for the BIMS was not completed.
Review of the PN for SSN in the electronic medical record showed that the last documented note was dated 3/10/22.
On 9/7/22 at 12:53 PM, two surveyors interviewed the Director of Social Worker (DSW). The DSW stated that the initial assessment was being documented in the electronic medical record in the Assessment tab and that all notes were in the electronic medical record and nothing was on paper. The DSW further stated that the quarterly assessments were exactly the same as MDS. The DSW indicated that it was the MDS Coordinator (MDSC) who initiates the MDS assessment in the Assessment tab and the SW is responsible for sections A, C, D, and Q. Furthermore, the DSW stated that DSW had been doing the MDS for over 10 years.
On that same date and time, the DSW informed the surveyors that assessments are due on Thursdays and the expectation was for the DSW to finish by Friday. The surveyor asked the DSW why the assessments were not completed accordingly and accurately. The DSW stated that before the pandemic, there were three and a half full-time Social workers in the facility and then, after the pandemic, the DSW was the only one who worked full time as a SW and the two other staff were part-time and per diem. The DSW acknowledged that the look-back period of Section C was seven days and should have been followed. The DSW stated, I feel bad that the assessment was not getting done.
On 9/8/22 at 10:12 AM, two surveyors interviewed MDS Coordinator. The surveyor asked the MDS Coordinator if she checked for the coding accuracy entered in the MDS within the ARD period before locking the MDS assessment for submission. The MDS Coordinator could not provide an answer and stated, It is the best we can do.
On 9/15/22 at 2:19 PM, the survey team met with the Licensed Nursing Home Administrator (LNHA), Director of Nursing (DON), Chief Nursing Officer (CNO), and discussed the above findings. There was no additional information provided.
5. On 9/01/22 at 11:56 AM, the surveyor observed Resident #198 who was alert and oriented and self-propelling in his/her wheelchair.
The surveyor reviewed the Medical Records for Resident #198.
The admission Record reflected that Resident #198 was admitted to the facility with diagnoses that included but not limited to anxiety disorder (a disorder that make you worry, nervous and uneased), osteoarthritis (disorder where the bones become brittle and fragile from loss of tissue), and cervicalgia (neck and shoulder pain).
A review of the quarterly MDS ARD dated 8/04/22, indicated a BIMS score of 12 out of 15, which indicated that the resident had moderately impaired cognition. Section C 0100 was coded 1. yes, and signed by SW#1 on 8/10/22.
The above 8/4/22, quarterly MDS was signed by SW#1 six (6) days after the ARD.
Review of the 8/4/22, quarterly Assessment in the Assessment tab of the electronic medical record showed that Section C for the BIMS was not completed.
Review of the PN for SSN in the electronic medical record showed the last documented note was on 2/3/22.
6. On 9/01/22 at 12:03 PM, the surveyor observed Resident #106 sitting in an electric wheelchair watching television.
The surveyor reviewed the Medical Records for Resident #106.
The admission Record reflected that the resident was admitted to the facility with diagnoses that included and not limited to chronic kidney disease (Long standing disease of the kidneys), Hypertension (high blood pressure) and Congestive Heart Failure (condition in which the heart doesn't pump blood well).
A review of the QMDS ARD dated 6/09/22, indicated a BIMS score of 15 out of 15, which indicated that the resident had an intact cognition. Section C 0100 was coded 1. yes, and signed by SW#1 on 7/05/22.
The above 6/09/22, QMDS was signed by SW#1 twenty nine (29) days after the ARD.
Review of the 6/09/22, quarterly Assessment in the Assessment tab of the electronic medical record showed that Section C for the BIMS was not completed.
Review of the PN for SSN in the electronic medical record showed the last documented note was dated 5/13/22.
7. On 9/01/22 at 12:10 PM, the surveyor observed Resident #13 in bed sleeping.
The surveyor reviewed the Medical Records for Resident #13.
The admission Record reflected that the resident was admitted to the facility with diagnoses that included and not limited to multiple sclerosis (progressive disease of the nerves, spinal cord, and brain), hypertension (high blood pressure) and hyperlipidemia (high cholesterol).
A review of the quarterly MDS ARD dated 8/26/22, indicated a BIMS score of 1 out of 15, which indicated that the resident had severe cognitive impairment. Section C 0100 was coded 1, yes, and signed by SW#1 on 9/06/22.
The above 6/09/22, quarterly MDS was signed by SW#1, eleven (11) days after the ARD.
A Review of the electronic medical record showed that there were no quarterly Assessments completed on 8/26/22.
Review of the PN for SSN in the electronic medical record showed the last documented note was dated 6/16/21.
NJAC 8:39-11.1
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record review, and review of pertinent facility documentation it was identified that the facili...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record review, and review of pertinent facility documentation it was identified that the facility failed to: a.) follow the Physician's Order (PO) for the use of oxygen equipment b.) appropriately store portable oxygen tank to the back of resident wheelchair and c.) store respiratory equipment in a way to prevent the spread of infection. This deficient practice was identified for three of three residents' reviewed for respiratory care, (Resident #111, #159 and #191) and was evidenced by the following:
The surveyor observed Resident #111.
1. On 9/01/22 at 11:32 AM, the surveyor observed the resident sitting in their high back wheelchair in their room watching TV. The surveyor observed an Oxygen (O2) concentrator in Resident #111's room next to Resident #111's bed. The O2 concentrator was running and set at two (2) Liters and Resident #111 was wearing their nasal cannula. The nasal cannula and humidification bottle were not labeled and dated. The surveyor also observed a portable O2 tank hanging from the wheelchair handle on the back of Resident #111's high back wheelchair. The concentrator was not in a holder or attached to the wheelchair with a strap. It was hanging freely by a green handle approximately 18 inches off the ground.
On 9/07/22 at 01:12 PM, the surveyor observed the resident in their room sleeping in their high back wheelchair. The surveyor observed the O2 concentrator in front of the wheelchair. The O2 concentrator was running and set at two (2) Liters and the resident was wearing their nasal cannula. The nasal cannula and humidification bottle were not labeled and dated. The surveyor also observed a portable O2 tank hanging from the wheelchair handle on the back of the resident high back wheelchair. The concentrator was not in a holder or attached to the wheelchair with a strap. It was hanging freely by a green handle approximately 18 inches off the ground.
On 9/19/22 at 11:32 AM, the surveyor observed the resident sitting in their high back wheelchair in their room getting ready to eat lunch. Again, the surveyor observed the O2 concentrator in Resident #111's room next to the residents bed. The O2 concentrator was running and set at two (2) Liters and the resident was wearing their nasal cannula (device used to deliver supplemental oxygen via a plastic tubing through the nostrils). The nasal cannula did not have a label or date on it. The surveyor also observed a portable O2 tank hanging from the wheelchair handle on the back of the residents high back wheelchair with a nasal cannula attached to it. The nasal cannula was not dated or in a bag. It was wrapped around Resident #111's wheelchair handle open to the environment. The portable O2 tank was not in a holder or attached to the wheelchair with a strap. It was hanging freely by a green handle approximately 18 inches off the ground.
On 09/15/22 11:52 AM, the surveyor interviewed the Certified Nursing Aide (CNA#1) who stated, I receive report from the nurses for my assignment in the morning. When I have a resident with O2, I make sure air is flowing from the tubing, The nurses do the vital signs and check the orders.
On 09/15/22 11:52 AM, the surveyor interviewed the Registered Nurse (RN#1) who stated, I make sure and check the order, check on the patient to make sure they are wearing their nasal cannula and check that the concentrator is on the correct setting of O2 liters.
On 09/19/22 11:56 AM, the surveyor interviewed the Licensed Practical Nurse/Unit Manger (LPN/UM) who was also the staff nurse caring for Resident #111 on this day. The LPN/UM stated that Resident #111 had COPD and was on continuous O2. He/She was forgetful but easily redirected and removed his/her nasal cannula at times. The LPN/UM explained that when Resident #111 wore his/her O2, their O2 saturation (the percentage of oxygen in a person's blood) was 96% and when the O2 was removed the O2 saturation dropped to 93%. The LPN/UM further stated that the nightshift nurses performed the humidification and tubing change with labeling on Wednesdays. The surveyor and LPN/UM proceeded to go in Resident #111's room. The surveyor asked the LPN/UM if the portable O2 tank and tubing should be hanging on the back of the chair with the tubing exposed and wrapped around the handle? The LPN/UM stated, No, this should be in a portable cart or attached to [the residents] wheelchair and the tubing should be in labeled and dated in a patient bag. The surveyor proceeded to ask the LPN/UM to show the surveyor where the PO was for the O2, the LPN/UM was unable to find the PO and stated that it had been discontinued in June 2022. The LPN/UM stated, That is funny because [the resident] has been on O2 since I started working here in March of 2021.
The surveyor reviewed the medical record for Resident #111.
A review of the resident's admission Record reflected that they had resided at the facility since 2015 and had diagnoses which included but were not limited to chronic obstructive pulmonary disease (a chronic inflammatory lung disease that causes obstructed airflow from the lungs), chronic congestive heart failure (blood often backs up and fluid can build up in the lungs, causing shortness of breath.), anemia (a condition in which you lack enough healthy red blood cells to carry adequate oxygen to your body's tissues), chronic kidney disease (a condition in which the kidneys are damaged and cannot filter blood as well as they should), and obesity (is a complex disease involving an excessive amount of body fat).
A review of the residents most recent significant change Minimum Data Set (MDS), an assessment tool used to facilitate the management of care, dated July 8, 2022, reflected that the resident had a Brief Interview for Mental Status (BIMS) score of 12 out of 15, which indicated the resident had moderately impaired cognition.
A review of the resident May through September 2022 Order Recap Report (ORR) revealed a PO dated 6/24/2022, to give two (2) liters of O2 to maintain O2 saturation of 92% or above as needed for supplemental oxygen. It showed discontinuation under order status.
A review of the residents Active Orders as of 9/15/2022, on the Order Summary Report (OSR) revealed no active or current orders for continuous or PRN (as needed) oxygen for the resident .
A review of the facility's Oxygen Administration Policy and Procedure revised 01/2022, included under Preparation, Verify that there is a physician's order for this procedure. Review the physician's orders or facility protocol for oxygen administration.
Further review of the facility's Oxygen Administration Policy and Procedure revised 01/2022, included under equipment and supplies that the portable O2 cylinder should be stored in a secured container, Strapped to the stand.
2. On 08/31/22 at 10:25 AM, during the initial tour of the facility Resident #159 was out of bed in a wheelchair. Resident #159 could not be interviewed due to a language barrier. The resident was wearing O2 via nasal cannula connected to a portable O2 tank on the back of the wheelchair. There was also a concentrator in the room, but the nasal cannula tubing was not connected to Resident #159 at the time of the observation.
A review of the resident's admission Record reflected that Resident # 159 was admitted to the facility on [DATE], with diagnoses which included but not limited to cancer, chronic obstructive pulmonary disease and hypertension (high blood pressure).
A review of the admission MDS dated [DATE], reflected the resident had a BIMS score of 14 out of 15, indicating that the resident had intact cognition. Review of Section G, for functional status, indicated that Resident #159 had a functional status of a 2-person assistance for transfer and toileting and a one-person assistance for dressing, eating, and hygiene.
A review of the September 2022 PO's revealed an active PO for O2 dated 8/04/22. The PO was for O2 at two liters/minute via nasal cannula every shift for COPD if oxygen level less than 92%, meaning the oxygen level would be checked every shift for Resident #159 and if the reading was less than 92% the oxygen would then be applied.
A review of the September 2022 Medication Administration Record (MAR) indicated the above corresponding PO for the use of O2. The MAR reflected that the staff signed every shift that Resident #159 was wearing O2.
On 9/02/22 at 10:00 AM, the surveyor reviewed the vital signs/graphic section of the Electronic Medical Record (EMR) which showed the following pulse oximetry (noninvasive monitoring of oxygen saturation) documentation. After review of the documented pulse oximetry levels, the resident was never below 92%, and the oxygen was still applied to the resident.
9/2/2022 12:11 PM
97.0 %
Oxygen via Nasal Cannula
9/1/2022 06:14 PM
95.0 %
Room Air
9/1/2022 04:52 PM
96.0 %
Oxygen via Nasal Cannula
9/1/2022 08:18 AM
96.0 %
Oxygen via Nasal Cannula
9/1/2022 08:17 AM
96.0 %
Oxygen via Nasal Cannula
9/1/2022 02:18 AM
98.0 %
Oxygen via Nasal Cannula
8/31/2022 07:15 PM
96.0 %
Room Air
8/31/2022 05:19 PM
97.0 %
Oxygen via Nasal Cannula
8/31/2022 02:15 PM
94.0 %
Room Air
8/31/2022 03:06 AM
98.0 %
Oxygen via Nasal Cannula
A review of the resident's Care Plan (CP) initiated on 9/02/22, indicated a focus area for oxygen therapy related to medical diagnosis Chronic Obstructive Pulmonary Disease (COPD) The goal was to have no signs and symptoms of poor oxygen levels and the interventions implemented included changing positions, administering oxygen and medications as ordered by physician and to monitor for side effects.
On 9/08/22 at 11:10 AM, the surveyor observed Resident #159 in bed with eyes closed. Resident #159 was wearing O2 via nasal cannula connected to an O2 concentrator and it was set at two liters.
0 9/09/22 at 11:55 AM, the surveyor observed Resident #159 in the room in a wheelchair. Resident #159 was wearing O2 at two liters via nasal cannula via a compressor.
On 9/15/22 at 12:45 PM, Resident #159 was in the bed wearing O2 via nasal cannula at two liters. The surveyor interviewed the unit Licensed Practical Nurse (LPN) who was taking care of Resident #159 and asked what the orders for the oxygen were. The LPN told the surveyor that Resident #159 was ordered to wear two liters of O2 via nasal cannula continuously (meaning the resident wore the oxygen all the time). The surveyor then interviewed the Registered Nurse/Unit Manager (RN/UM) who stated that the resident wears O2 continuously.
On 9/15/22 at 2:20 PM, the surveyor presented the O2 concern to the Director of Nursing (DON), and the DON acknowledged that the PO for the use of the O2 needed to be clarified with Resident #159's physician.
9/21/22 at 11:00 AM, the surveyor reviewed the Oxygen Administration Policy and Procedure dated 1/2022, which included to verify that there was a physician order for the oxygen and to review the physicians' orders or facility protocol for oxygen administration.
3. On 9/01/22 at 11:32 AM, the surveyor observed Resident #191 reclining back in his/her geri-chair in their room. The surveyor attempted to interview Resident #191. Resident #191 was able to communicate his/her name to the surveyor. The surveyor observed an O2 concentrator in Resident #191's room next to Resident #191's bed. The O2 concentrator was not running at the time of the surveyor observation. The surveyor observed the nasal cannula tubing laying on the floor next to the O2 concentrator and further observed the nasal cannula tubing draped over the O2 concentrator with the prongs of the nasal cannula tubing in direct contact with the back of the O2 concentrator. The surveyor saw that Resident #191 had two nebulizer masks. One of the nebulizer masks was placed on top of the nebulizer machine and the other nebulizer mask was on top of the O2 concentrator. The surveyor saw a Yankauer suction wand in direct contact with the windowsill. None of the respiratory equipment was stored in a plastic bag.
On 9/02/22 at 10:00 AM, the surveyor entered Resident #191's unoccupied room and observed the O2 concentrator in the room. The nasal cannula tubing was stored in a plastic bag and attached to the O2 concentrator. The surveyor further observed a nebulizer mask not stored in a plastic bag and in direct contact with windowsill. The surveyor saw the Yankauer suction wand not placed in plastic bag and in direct contact with the windowsill.
On 9/09/22 at 11:32 AM, the surveyor interviewed CNA#2 who stated that CNA#2 took care of Resident #191, Resident #191 was alert to self, and was able to verbalize simple needs. The CNA#2 told the surveyor that Resident #191 received O2 and Resident #191 never touched the O2 concentrator. The CNA#2 further stated that CNA#2 did not touch the O2 concentrator because it was the primary nurse's responsibility.
On 9/09/22 at 11:35 AM, the surveyor interviewed Resident #191's RN#2 who stated Resident #191 was confused and needed total care with activities of daily living. RN#2 further stated that Resident #191 had received O2 on an as needed basis and received nebulizer treatments if he/she was short of breath or congested. RN#2 stated that the O2 equipment should have been stored in a plastic bag for infection control purposes.
On 9/09/22 at 11:55 AM, the surveyor interviewed the LPN/UM who stated Resident #191's O2 equipment should have been stored in a plastic bag to keep it sanitary.
The surveyor reviewed the medical record for Resident #191.
A review of the resident's admission Record reflected that Resident #191 had resided at the facility for about a year and had diagnoses which included but were not limited to cerebral palsy (a congenital disorder that affects movement, muscle tone and posture due to abnormal brain development before birth), lobar pneumonia, unspecified organism, unspecified severe protein calorie malnutrition, schizophrenia, major depressive disorder, anxiety, unspecified intellectual disabilities, essential hypertension, and gastro-esophageal reflux disease without esophagitis (inflammation that damages the tube running from the throat to the stomach).
A review of Resident #191's most recent significant change Minimum Data Set (MDS), an assessment tool used to facilitate the management of care dated 7/21/2022, reflected that Resident #191 had a BIMS score of 4 out of 15 which indicated Resident #191 had severely impaired cognition.
A review of Resident #191's September 2022 Order Summary Report (OSR) revealed a PO dated 7/08/2022, to give two (2) liters of oxygen to maintain oxygen saturation of 94% or above as needed for supplemental oxygen. A further review of the September 2022, OSR revealed a PO dated 6/28/2022, for Ipratropium-Albuterol Solution 0.5-2.5 (3) milligrams (MG)/(3) milliliter (ML) inhale orally via nebulizer every four hours for wheezing and shortness of breath.
A review of Resident #191's September 2022 Treatment Administration Record (TAR) reflected a PO dated 7/08/2022, to give two (2) liters of oxygen to maintain oxygen saturation of 94% or above as needed for supplemental oxygen. A review of the September 2022 Medication Administration Record (MAR) reflected a PO dated 6/28/2022, for Ipratropium-Albuterol Solution 0.5-2.5 (3) milligrams (MG)/(3) milliliter (ML) inhale orally via nebulizer every four hours for wheezing and shortness of breath. A further review of the September 2022 MAR indicated that the nurses were signing at 0000 (12:00 AM), 0400 (4:00 AM), 0800 (8:00 AM), 1200 (12:00 PM), 1600 (4:00 PM), and 2000 (8:00 PM) that the resident was administered the nebulizer treatment.
A review of Resident #191's Care Plan (CP) revised 7/26/2022, did not reflect a focus area for the use of as needed O2 or for the care of O2 equipment.
A review of the facility's Oxygen Administration Policy and Procedure revised 01/2022 indicated to, replace entire set-up every seven days. Date and store in treatment bag when not in use.
NJAC 8:39-27.1(a)
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected multiple residents
3. On 8/31/22 at 10:43 AM, the surveyor interviewed the Registered Nurse/Unit Manager (RN/UM). The RN/UM stated that I am not sure if the 2 A unit had residents with facility-acquired wounds.
During a...
Read full inspector narrative →
3. On 8/31/22 at 10:43 AM, the surveyor interviewed the Registered Nurse/Unit Manager (RN/UM). The RN/UM stated that I am not sure if the 2 A unit had residents with facility-acquired wounds.
During an observation on 8/31/22 at 10:54 AM by the surveyor, the Certified Nursing Aide (CNA#2) was inside the resident's room with a privacy curtain in use while providing morning care. The surveyor observed the resident with an indwelling catheter.
The surveyor reviewed the medical records of Resident #69.
The admission Record (admission summary) reflected that the resident was admitted to the facility with diagnoses that included but were not limited to Paraplegia unspecified (paralysis that affects all or part of the trunk, legs, and pelvic organs) and Multiple sclerosis (a neurological disease that causes dizziness, mobility problems, numbness, and fatigue.)
The 6/23/22 Quarterly Minimum Data Set (QMDS), an assessment tool used to facilitate the management of care, indicated a brief interview for mental status (BIMS) score of 15 out of 15, which reflected that the resident's cognition was intact.
The Order Summary Report (OSR) for September 202 included the following wound care orders:
Start Date (SD) 7/15/22 Cleanse bilateral toes with NSS (normal saline solution) apply Bacitracin (an antibiotic ointment used to prevent wound infections) OTA (open to air) alternating or every other day one time a day every two days.
SD 9/2/22 Lotrisone Cream 1-0.05% (an antifungal/steroid combination cream used on the skin) apply to left buttock topically every day and evening shift for wound care cleanse with NSS pat dry.
SD 9/2/22 Lotrisone Cream 1-0.05% apply to left gluteal fold topically every day and evening shift for fungal rash cleanse NSS, pat dry.
SD 7/28/22 Zinc Oxide ointment (a skincare and preventative medicine) 10% apply to BL (bilateral) buttocks topically every day and evening shift for a skin condition. Apply following all care/incontinence opportunities PRN (as needed).
A review of the Progress Notes showed an 8/31/22 Skin/Wound (S/W) Note signed by a Registered Nurse (RN) that indicated that the resident was seen for a weekly wound visit by NP (Nurse Practitioner). The 8/31/22 S/W Note reflected that there was a left buttock MASD (moisture-associated skin damage) and left gluteal fold fungal dermatitis with an order of cleansing with NSS and applying Lotrisone cream BID (twice a day).
On 9/2/22 at 10:32 AM, the surveyor observed the resident laying in bed while watching television. The resident stated that the wounds on their back were getting better, the nurse does wound care every day and there was no concern.
On 9/9/22 at 11:05 AM, the surveyor observed the CNA#2 providing morning care to the resident with a privacy curtain in use. There was a quarter strength 475 milliliters (mls) bottle of Dakin's solution (a broad-spectrum antimicrobial cleanser that is gentle to the skin) with approximately 100 mls left inside the bottle that was on top of the resident's nightstand. The CNA#2 stated that she did not know who left the bottle of Dakin's solution in the resident's room. There was no other resident at that time inside the room except for Resident #69. Then the CNA#2 called the nurse.
On 9/9/22 at 11:22 AM, the surveyor interviewed the Licensed Practical Nurse (LPN#2). The LPN#2 stated that she was not sure who left Dakin's solution inside the resident's room. The LPN#2 further stated that the medication should have been stored inside the treatment cart.
On 9/9/22 at 11:41 AM, the surveyor interviewed the RN/UM and made her aware of the above concern. The RN/UM stated that Dakin's solution should not be in the resident's room and should be stored inside the treatment cart. The surveyor asked the RN/UM if the resident had an order for Dakin's solution and the RN/UM stated that she will get back to the surveyor.
On 9/15/22 at 9:17 AM, the surveyor informed the DON of the above concern with Dakin's solution that was left in the resident's room and that the resident had no order for the medication. The DON stated that she will get back to the surveyor.
On 9/15/22 at 02:19 PM, the survey team met with the LNHA, Chief Nursing Officer, and DON and were made aware of the above concerns.
On 9/16/22 at 9:55 AM, the surveyor interviewed the Consultant Pharmacist (CP) who stated that the nurses should know that medications should not be left at a resident's bedside and that was part of her in-service when she does medication pass observations.
On 9/20/22 at 12:44 PM, the DON acknowledged that there was no order for Dakin's solution for Resident #69 and the medication should have been stored inside the treatment cart.
On 9/20/22 at 01:56 PM, the survey team met with the LNHA, DON, and Assistant Nursing Home Administrator. The facility administrative team had no additional information provided.
A review of the facility's Storage of Medications Policy that was provided by the LNHA with a reviewed/revised date of 1/2022 included Policy Statement: The facility shall store all drugs and biologicals in a safe, secure, and orderly manner. Policy Interpretation and Implementation: .2. The nursing staff shall be responsible for maintaining medication storage and preparation areas in a clean, safe, and sanitary manner .8. Drugs shall be stored in an orderly manner in cabinets, drawers, carts, or automatic dispensing systems. Each resident's medications shall be assigned to an individual cubicle, drawer, or other holding area to prevent the possibility of mixing medications of several residents
NJAC 8:39-11.2(b), 27.1(a), 29.2(d), 29.4(g)(h)
2. On 9/13/22 at 11:10 AM, the surveyor observed Resident #121 who was alert and oriented seated in a wheelchair watching television. The surveyor observed a medication cup on the resident's overbed table that contained two (2) pills. The surveyor interviewed the resident who stated that the two (2) medications in the cup were Metformin (medication to treat high blood sugar) and Buspar and that she/he was allowed to take it when they were ready.
On 9/13/22 at 11:20 AM, the surveyor showed the 2 A unit Registered Nurse/Unit Manager (RN/UM) the medication cup that contained the two (2) pills. The RN/UM stated that no medication should have been left for the resident to take and that the medications should have been administered in the presence of a nurse. The RN/UM took the medication cup that contained the two pills and brought it back to the medication room to be destroyed in a drug disposal system. The RN/UM stated that the medication nurse was on break and would have to re-educate the nurse regarding the facility medication administration policy.
On 9/13/22 at 12:00 PM, the surveyor interviewed the the Licensed Practical Nurse (LPN#1) who was Resident #121's medication nurse. LPN #1 stated that medications should never be left with a resident unattended and that residents should only be administered their medications in the presence of a nurse. The LPN#1 stated that she administered the medications to Resident #121, but failed to make sure that the resident swallowed their pills. She stated that she would have to make sure that her residents swallowed their pills by asking them to open their mouth after she had given the resident their medications.
The surveyor reviewed the medical record for Resident #121.
The admission Record reflected that the resident was admitted to the facility with diagnoses that included but were not limited to Schizophrenia (a disorder that affects a person's ability to think, feel and behave clearly), bi-polar illness (condition of mood swing from depressive lows to manic highs), major depressive disorder (long term loss of pleasure and interest) and anxiety disorder (disorder of feeling worry and fear).
A review of the annual Minimum Data Set (MDS), an assessment tool used to facilitate the management of care, dated 6/30/22, reflected that the resident had a brief interview for mental status (BIMS) score of 15 out of 15, indicating that the resident had an intact cognition.
A review of the interdisciplinary care plan revealed that there was no focus area that indicated that the resident could self-administer their medications.
A review of the Order Summary Report (OSR), dated 9/13/22, had not included a PO that the resident was able to self-administer medications. The OSR revealed a PO dated 3/20/22 for Buspirone (Buspar) 10 milligram (MG) tablet to give one tablet in the morning for anxiety and a PO dated 4/18/22 for Metformin ER (Extended Release) 750 MG to give one tablet two times daily for Diabetes.
A review of the September 2022 Electronic Medication Administration Record (EMAR) revealed a PO dated 3/20/22 for Buspirone (Buspar) 10 MG tablet to give 1 tablet by mouth in the morning with an administration time of 9 AM. The administration time of 9 AM on 9/13/22 for the Buspirone was signed by the LPN as being administered.
In addition, the EMAR also revealed a PO dated 4/18/22 for Metformin ER 750 MG 1 tablet by mouth twice daily with administration times of 8 AM and 5 PM. The administration time of 8 AM on 9/13/22 for the Metformin ER was signed by the LPN as being administered.
On 9/15/22 at 2:00 PM, the survey team met with the LNHA, Chief Nursing Officer and DON and no further information was provided by the facility.
On 9/16/22 at 9:55 AM, the surveyor interviewed the Consultant Pharmacist (CP) who stated that she would make recommendations that Metformin ER be given at 8 AM with food and that nurses should be aware that medications should not be left at a resident's bedside, and this is part of her in-service when she does medication pass observations.
On 9/16/22 at 10:24 AM, the CP provided the surveyor with a Medication Pass Observation Worksheet dated 9/15/22 which she stated she had just completed yesterday with another nurse. The CP added that she used this form when performing a medication administration observation and also to educate the nurses. The surveyor with the CP reviewed the worksheet which had criteria she used to evaluate the medication observation which included Resident observed to ensure medication is swallowed. In addition, the worksheet indicated Medications administered at correct time.
On 9/21/22 at 9:58 AM, the surveyor interviewed the CP who stated that she had done a medication observation in-service in July but was unable to find the sign in sheet for attendance. The CP added that she used the Medication Pass Observation Worksheet as a guide for the inservice. The CP added that she does frequent medication observations for the facility and medications being left at the bedside was not allowed.
A review of the facility's policy for Administering Medications that was dated 12/21 and was provided by the DON indicated the following:
Policy Statement- Medications shall be administered in a safe and timely manner, and as prescribed.
Under Policies Interpretation and Implementation.
3. Medications must be administered in accordance with the orders, including any required time frame.
24. Residents may self-administer their own medications only if the attending physician, in conjunction with the interdisciplinary Care planning team, has determined that they have the decision-making capacity to so safely.
Based on observation, interview and record review, it was determined that the facility failed to provide pharmaceutical services in accordance with professional standards to ensure that a.) medications that were ordered by the physician were available for administration during the months of April, May, and July 2022 for one (1) of 18 residents, (Resident #99) reviewed for medication management, b.) medications were observed as accurately and timely administered to one (1) of seven (7) residents, (Resident #121) reviewed for medication administration, and c.) a treatment medication was accurately administered and properly stored for one (1) of two (2) residents, Resident #69, reviewed for treatment medications.
The deficient practices were evidenced by the following:
Reference: New Jersey Statutes Annotated, Title 45. Chapter 11. Nursing Board. The Nurse Practice Act for the State of New Jersey states: The practice of nursing as a registered professional nurse is defined as diagnosing and treating human responses to actual and potential physical and emotional health problems, through such services as case finding, health teaching, health counseling, and provision of care supportive to or restorative of life and wellbeing, and executing medical regimens as prescribed by a licensed or otherwise legally authorized physician or dentist.
Reference: New Jersey Statutes Annotated, Title 45, Chapter 11. Nursing Board. The Nurse Practice Act for the State of New Jersey states: The practice of nursing as a licensed practical nurse is defined as performing tasks and responsibilities within the framework of case finding; reinforcing the patient and family teaching program through health teaching, health counseling and provision of supportive and restorative care, under the direction of a registered nurse or licensed or otherwise legally authorized physician or dentist.
1. On 9/9/22 at 11:30 AM, the surveyor observed Resident #99 being wheeled by a Certified Nurses Aide (CNA#1) who stated to the resident that she was taking him/her to his/her room for changing before he/she was to go out with a resident representative.
The surveyor reviewed the medical record for Resident #99.
A review of the resident's admission Record revealed diagnoses which included hypertension (high blood pressure), major depressive disorder (mood disorder), cerebral palsy(a group of disorders that affect a person's ability to move and maintain posture), schizophrenia (a disorder that affects a person's ability to think, feel and behave clearly) and intestinal obstruction (a mechanical or functional obstruction of the intestines that prevents normal movement of the products of digestion).
A review of the quarterly Minimum Data Set (MDS), an assessment tool used to facilitate the management of care dated 7/30/22, reflected the resident had a brief interview for mental status (BIMS) score of 12 out of 15, indicating that the resident had a moderately intact cognition. In addition, the MDS included in Section B, completed for Hearing, Speech and Vision that the resident was usually able to make themself understood and was usually able to understand others.
A review of the July 2022 EMAR revealed a physician's order (PO) dated 7/16/2022 for Amitiza (a medication used to relieve constipation) capsule 24 micrograms (MCG), give one capsule by mouth two times a day for constipation. The Amitiza PO had an entry of 9 for administration which corresponded to the chart code of other/see nurses notes on 7/16/22 at 6 PM, 7/17/2022 at 9 AM and 7/18/22 at 9 AM
A review of the corresponding nursing progress notes were as follows:
-dated 7/16/22 at 8:14 PM revealed that for Amitiza, pharmacy called, awaiting pharmacy delivery. Patient made aware.
-dated 7/17/22 at 10:08 AM revealed for Amitiza, Prior authorization in progress, MD and family aware.
-dated 7/17/22 at 8:05 PM revealed for Amitiza, Awaiting delivery from pharmacy.
-dated 7/18/22 at 9:39 AM revealed for Amitiza, Prior authorization in progress, medication administered from back up supply.
On 9/13/22 at 12:09 PM, the surveyor interviewed the Licensed Practical Nurse/Unit Manager (LPN/UM) who stated that Resident #99 had a resident representative that was very involved in the resident's care. The LPN/UM added that the resident had been on Linzess for constipation and the resident's representative had spoken with the physician to try Amitiza instead of Linzess. The LPN/UM stated that there was an insurance issue with obtaining Amitiza but thought that the resident was receiving Linzess until the Amitiza was delivered by pharmacy. The LPN/UM stated that if a medication was not available the nurse should call the pharmacy, check the back up supply and if needed call the physician for follow up orders if the medication was not available.
Further review of the July EMAR revealed a PO dated 6/14/22 with a discontinue order of 7/16/22 for Linzess capsule 290 MCG, give one capsule by mouth one time a day for irritable bowel syndrome. The Linzess was discontinued after the 7/16/22 morning dose.
On 9/15/22 at 11:30 AM, the surveyor attempted to interview Resident #99 who answered yes and no to questions and would not elaborate and preferred to not answer any more questions. The resident answered no when asked if he/she had any issues or concerns with the staff, medications or living at the facility.
The surveyor further reviewed the medical record for Resident #99.
A review of the April 2022 EMAR revealed a physician's order (PO) dated 4/13/2022 for Hydralazine (a medication used to lower blood pressure) hydrochloride tablet 50 milligrams (MG), give one tablet by mouth every eight hours for hypertension. On 4/16/22 at 2 PM, and 4/18/22 at 2 PM the Hydralazine PO had an entry of 9 for administration which corresponded to the chart code of other/see nurses notes.
A review of the following corresponding nursing progress notes revealed:
-dated 4/16/22 at 2:42 PM due meds were given as ordered
-dated 4/16/22 at 2:44 PM for Hydralazine, resident out on pass with family member.
-dated 4/30/22 at 3:04 PM for Hydralazine, out on pass with family member, will return 6:00 PM.
-dated 4/30/22 at 3:33 PM all due meds were given as ordered.
A review of the May 2022 EMAR revealed a PO dated 4/13/2022 for Hydralazine hydrochloride tablet 50 MG, give one tablet by mouth every eight hours for hypertension. On 5/18/22 at 2 PM the Hydralazine PO had an entry of 9 for administration which corresponded to the chart code of other/see nurses notes.
A review of the corresponding nursing progress notes dated 5/18/22 at 3:27 PM revealed out on pass with family member.
Further review of the May 2022 EMAR revealed a PO dated 4/14/2022 for Cymbalta (a medication used for depression) capsule delayed release particles 60 MG, (Duloxetine hydrochloride), give one capsule by mouth one time a day for depression. On 5/16/22 at 9 AM the Cymbalta PO had an entry 9 for administration which corresponded to the chart code of other/see nurses notes.
A review of the nursing progress note dated 5/16/22 at 12:48 PM revealed that for Cymbalta, resident's family member took resident prior to medication administration.
On 9/16/22 at 9:55 AM, the surveyor interviewed the Consultant Pharmacist (CP) who stated that there have been issues with medications not being available. The CP stated that she recently had done an inservice and there were medications that were not available and was told by the nurses that there was an issue with the pharmacy delivering. The CP stated that the Director of Nursing (DON) was aware and that there may be an issue with the provider pharmacy. The CP added that she has told the nurses that they should check the back up supply first and if the medication was not there then call the pharmacy for a STAT (immediate) delivery and also to call the physician to make them aware if the time needed to be changed or follow up orders. The CP added that the nurses should not enter in the EMAR that a medication was not administered without documentation as to why and the follow-up from a physician.
On 9/16/22 at10:24 AM, the CP provided the surveyor with a Medication Pass Observation Worksheet dated 9/15/22 which she stated she had just completed yesterday and had an issue with medications not being available. The CP added that she uses this form when performing a medication administration observation and also to educate the nurses when she does inservices. The surveyor with the CP reviewed the worksheet which reflected criteria that was to be observed during the medication observation which included Resident observed to ensure medication is swallowed, Medications administered at correct time, and No medications omitted.
On 9/19/22 at 11:25 AM, the surveyor was provided a list by the Director of Nursing (DON) regarding the dates and reasons for the above medications not being administered to Resident # 99. The list indicated that the #9 entered on the EMAR for the Hydralazine, and Cymbalta was indicated in nursing notes that the resident was out on pass. In addition, the list indicated that Linzess was discontinued on 7/16, Amitiza started on 7/16, Amitiza discontinued 7/29 and Linzess started 7/29/22.
On 9/19/22 at 11:45 AM, the surveyor interviewed the LPN/UM who stated that the resident representative for Resident #99 usually came the same time every day and that the nurses were aware that the resident's medications were to be administered before leaving or upon return to the facility. The LPN/UM added that if the timing of the medication administration was going to be greater than one hour before or one hour after the time of administration noted on the EMAR then the physician was to be called for follow up instructions as to whether to administer the medication or hold it.
On 9/19/22 at 2:08 PM, the survey team met with the Licensed Nursing Home Administrator (LNHA) and DON. The DON stated that when a resident goes out on pass the medications that were to be administered during that time should be worked out by nursing or the physician should be notified for follow up. The DON added that she thought the resident representative for Resident #99 was very involved and was well aware of the resident's medications and usually would have the resident back before medications were needed or had them administered before leaving. The DON was unable to speak to why the medications were not administered. In addition, the DON was unable to speak to the discrepancy of the Amitiza not being administered and would have to check further.
On 9/21/22 at 9:58 AM, the surveyor interviewed the CP who stated that she had done a medication observation inservice in July but was unable to find the sign in sheet for attendance. The CP added that she uses the Medication Pass Observation Worksheet as a guide for the inservice.
On 9/21/22 at 12:35 PM the survey team met with the LNHA and DON who both stated that they had nothing further to present for the medications not being administered.
A review of the facility policy dated as revised 12/2021 for Administering medications reflected that Medications shall be administered in a safe and timely manner, and as prescribed. In addition, Medications must be administered in accordance with the orders, including any required time frame.
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
Based on observation, interview and record review, it was determined that the facility failed to document non-drug interventions that were attempted and the need for an as needed psychoactive medicati...
Read full inspector narrative →
Based on observation, interview and record review, it was determined that the facility failed to document non-drug interventions that were attempted and the need for an as needed psychoactive medication (Ativan) to be administered according to documented behaviors from April, May, June and July. The deficient practice was identified for one (1) of five (5) residents (Resident #101) reviewed for unnecessary medications, and was evidenced by the following:
On 9/1/22 at 11:24 AM, the surveyor observed Resident #101 in a wheelchair in the Day Room. The resident waved the surveyor over to him/her. The resident stated that he/she wanted to get up and would then be able to walk out of the room.
At that time, a Certified Nursing Aide (CNA) came over to the resident and asked if the resident would like to be taken somewhere else.
On 9/1/22 at 11:26 AM, the CNA stated that the resident was confused and unable to stand on their own and often asked to be taken home. The CNA added that the resident had a behavior of yelling and does get anxious but was able to redirect the resident.
On 9/2/22 at 11:12 AM, the surveyor observed Resident #101 in the Day Room sitting at a table with a group of other residents coloring a picture.
On 9/9/22 at 12:48 PM, the surveyor observed Resident #101 in his/her room in bed with an already eaten lunch tray on the overbed table in front of the resident. The resident stated that lunch was good. The resident was pleasant but was unable to answer any other questions because the resident had rambling thoughts expressed.
On 9/13/22 at 11:26 AM, the surveyor interviewed the Licensed Practical Nursing (LPN#1) who stated that she was familiar with Resident #101. The LPN#1 stated that she had not administered any as needed (PRN) psychoactive medication for behaviors but thought the resident had a current physician's order because the resident's husband had passed away recently the beginning of September. The LPN#1 added that the resident usually had no behaviors requiring a PRN medication but does need a lot of explanation as to what was happening. The LPN#1 explained that today the resident had to have blood drawn and was nervous so she had stayed with the resident to keep him/her calm. The LPN#1 also explained that she would have to write a progress note if the resident was having behaviors to explain what the behaviors were and what had happened and in the behavior monitoring section on the electronic medication administration record (EMAR) she would indicate a number of how many times the resident had the identified behaviors during her shift. The LPN#1 added that she would document the behaviors in progress notes whether she administered a PRN medication or not. The LPN#1 also stated that the facility had a Psychiatric Nurse Practitioner who came to the facility and reviewed the behavior notes to assess how the residents were doing.
On 9/13/22 at 12:09 PM, the surveyor interviewed the Licensed Practical Nurse/Unit Manager (LPN/UM) who stated that the facility had a Psychiatric group who came in on a regular basis to review all residents on a psychoactive medication. The LPN/UM added that the group reviewed the behavior monitoring and asked the nurses how the resident was doing. The LPN/UM stated that there were no monthly summaries regarding the resident's behaviors or to indicate the number of times a PRN psychoactive medication was used. The LPN/UM added that the EMAR had the behaviors described and did not think the nurses had to write progress notes when the behaviors occurred. The LPN/UM also stated that if the physician's order (PO) indicated to administer when the resident had anxiety, she did not think the nurses would have to describe what the anxiety behaviors were in the progress notes because the PO indicated anxiety.
On 9/15/22 at 2:19 PM, the surveyor team met with the Licensed Nursing Home Administrator (LNHA), Director of Nursing (DON) and Chief Nursing Officer (CNO). The DON stated that for behavior monitoring charting in the EMAR a Y meant that the resident was monitored for a behavior and an N meant that a behavior was observed and would expect to see a progress note describing the behavior. The DON could not speak to why numbers were entered for behavior monitoring. The CNO stated that she would expect to see a progress note if there were behaviors. In addition, the LNHA stated that if a PRN psychoactive medication was used for a behavior, then there should be a progress note explaining.
The surveyor reviewed the medical record for Resident #101.
A review of the resident's admission Record revealed diagnoses which included transient cerebral ischemic attack (a mini stroke), anxiety disorder, dementia with behavioral disturbance, major depressive disorder.
A review of the quarterly Minimum Data Set (MDS), an assessment tool used to facilitate the management of care dated 8/29/22, reflected that the resident had a brief interview for mental status (BIMS) score of 6 out of 15, indicating that the resident had a severely impaired cognition.
A review of Individual Patient's Controlled Drug Record (IPCDR) for Ativan 0.5 milligram (MG) tablets dated as received 3/21/22, revealed that one tablet of Ativan had been removed from inventory on the following dates and times and was administered to Resident #101 by the following nurses:
-on 4/22/22 at 10:14 AM by LPN #2.
-on 4/23/22 at 6:18 PM by RN#2.
-on 5/5/22 at 9 PM by LPN#3.
-on 6/29/22 at 8 PM by RN#1.
-on 7/2/22 at 9 AM by RN#1.
-on 7/2/22 at 8 PM by RN#1.
-on 7/3/22 at 10 AM by RN#1.
-on 7/3/22 at 7 PM by RN#1.
A review of the April and May 2022 EMAR had a PO dated 4/22/22, for Ativan 0.5 milligram (MG), give one tablet by mouth every 12 hours as needed (PRN) for anxiety. The PO had a discontinue date of 5/10/22. In addition, there was the Ativan administration documentation that corresponded with the IPCDR for the dates of 4/22, 4/23 and 5/5.
A review of the corresponding nursing progress notes for the April and May 2022 dates of the Ativan administration on the IPCDR revealed the following:
-on 4/22/22 at 10:49 AM LPN#2 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every 12 hours as needed for anxiety.
- on 4/22/22 at 3:28 PM LPN#2 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every 12 hours as needed for anxiety. PRN administration was: Effective.
-on 4/23/22 at 6:25 PM RN #2 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every 12 hours as needed for anxiety, given at 6:25 PM for anxiety.
- on 4/23/22 at 7:53 PM RN #2 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every 12 hours as needed for anxiety, given at 6:25 PM for anxiety. PRN administration was: Effective
-on 5/5/22 at 5:39 PM by LPN#3 indicated an administration note Behaviors-monitoring for the following (specify) itching, picking at skin, restlessness, (agitation), hitting, increase in complaints, biting, kicking, spitting, cussing, racial slurs, elopement, stealing, delusions, hallucinations, psychosis, aggression, refusing care. Every shift for monitoring document Y if any of the above observed, specify behavior in progress notes. Document N if no behaviors observed. Cursing and increase in complaints.
-on 5/5/22 at 8:53 PM by LPN#3 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every 12 hours as needed for anxiety.
-On 5/5/22 at 9:30 PM by LPN#3 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every 12 hours as needed for anxiety. PRN administration was: Effective.
A review of the June and July 2022 EMAR had a PO dated 6/24/22 for Ativan 0.5 MG, give one tablet by mouth every 8 hours PRN for anxiety for 14 days. In addition, there was the Ativan administration documentation that corresponded with the IPCDR for the dates of 6/29, 7/2 and 7/3.
A review of the corresponding nursing progress notes for the June and July 2022 dates of the Ativan administration on the IPCDR revealed the following:
-on 6/29/22 at 6:00 PM by RN#1 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every eight (8) hours as needed for anxiety for 14 days.
- on 6/29/22 at 6:39 PM by RN#1 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every eight (8) hours as needed for anxiety for 14 days. PRN administration was: Effective.
-on 7/2/22 at 8:44 AM by RN#1 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every eight (8) hours as needed for anxiety for 14 days.
- on 7/2/22 at 11:26 AM by RN#1 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every eight (8) hours as needed for anxiety. PRN administration was: Effective.
-on 7/2/22 at 5:38 PM by RN#1 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every eight (8) hours as needed for anxiety for 14 days.
- on 7/2/22 at 6:35 PM by RN#1 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every eight (8) hours as needed for anxiety for 14 days. PRN administration was: Effective.
-on 7/3/22 at 10:11 AM by RN#1 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every eight (8) hours as needed for anxiety for 14 days.
- on 7/3/22 at 11:04 AM by RN#1 there were two entries that indicated an administration note Was a behavior observed: YES.
- on 7/3/22 at 11:05 AM by RN#1 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every eight (8) hours as needed for anxiety for 14 days. PRN administration was: Effective.
-on 7/3/22 at 6:18 PM by RN#1 indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every eight (8) hours as needed for anxiety for 14 days.
- on 7/3/22 at 6:18 PM by RN#1 9:15 PM indicated an administration note Ativan tablet 0.5 MG, give one tablet by mouth every eight (8) hours as needed for anxiety for 14 days. PRN administration was: Effective.
A review of the April and May 2022 EMAR's revealed a behavior monitoring entry dated 3/35/33 with a discontinue date of 5/17/22 for Behaviors-Monitor for the following: itching, picking at skin, restlessness, (agitation), hitting, increase in complaints, biting, kicking, spitting, cussing, racial slurs, elopement, stealing, delusions, hallucinations, psychosis, aggression, refusing care. Every shift for monitoring document Y if any of the above observed, specify behavior in progress notes. Document N if no behaviors observed. The following entries were noted on the corresponding dates of PRN Ativan administration:
-for 4/22/22 and 4/23/22 there was zero 0 entered for the day, evening and night shifts.
-for 5/5/22 there was zero 0 entered for the day, evening and night shifts.
A review of the June and July 2022 EMAR's revealed a behavior monitoring entry dated 6/17/22 for Behaviors-Monitor for the following: itching, picking at skin, restlessness, (agitation), hitting, increase in complaints, biting, kicking, spitting, cussing, racial slurs, elopement, stealing, delusions, hallucinations, psychosis, aggression, refusing care. Every shift for monitoring document Y if any of the above observed, specify behavior in progress notes. Document N if no behaviors observed. The following entries were noted on the corresponding dates of PRN Ativan administration:
-for 6/29/22 there was zero 0 entered for the day, evening and night shifts.
- for 7/2/22 there was zero 0 entered for the day, evening and night shifts.
-for 7/3/22 there was 3 entered for the day shift, 2 entered for the evening shift and zero 0 entered for the night shift.
There was no progress note indicating as to which behaviors were exhibited on 7/3/22 with the entry 3 for the day sift.
On 9/16/22 at 9:55 AM, the surveyor interviewed the Consultant Pharmacist (CP) who stated that the facility had a Psychiatric group that came to the facility frequently and reviewed all the psychoactive medications and has seen that they do gradual dosage reductions and had diagnoses which warranted the use of the psychoactive medications. The CP added that the EMAR had the behaviors that were being monitored and those were decided upon by nursing. The CP stated that if a resident had behaviors during a nurses shift then there would be a number in the behavior monitoring on the EMAR and a corresponding progress note describing the behaviors. The CP was unsure if a progress note was needed for the use of a PRN Ativan for anxiety. The CP added that if a PRN Ativan was administered then the EMAR behavior monitoring should correspond for that day and time. The CP also stated that non-drug interventions should be attempted before administering the PRN psychoactive medication and thought that would be in the progress notes. The surveyor reviewed with the CP the PRN Ativan for Resident #101 and the CP stated that she would have to review further.
On 9/19/22 at 9:36 AM, the surveyor interviewed the Registered Nurse (RN #1) via telephone who stated that she worked as an agency nurse per diem (when needed) approximately two days a week at the facility and was familiar with Resident #101. The RN#1 stated that she had administered PRN Ativan to the resident. The RN#1 stated that the resident had anxiety and would fight with his/her spouse who resided in the facility. The RN#1 added that the resident would yell and want someone to stay with them all the time and would request to go home frequently. The RN#1 stated that there should be a progress note describing the resident's behavior and thought that maybe she missed writing the progress note. The RN#1 stated that there was a lot happening and working at the facility was very busy and may not have completed a progress note. The RN#1 stated that she had tried non-drug interventions such as distracting the resident, offering a snack, reassuring the resident and talking calmly. The RN#1 added that she would document the number of behaviors in the EMAR and that should correlate with the PRN Ativan that was administered.
On 9/19/22 at 1:38 PM, the surveyor interviewed the LPN#2 who stated that she had administered Ativan on 4/22/22, because the resident was anxious over being administered a blood transfusion. The LPN#2 stated that the resident had not received a blood transfusion on 4/22/22, because there was a problem, and the transfusion was done on 4/23/22. The LPN#2 stated that she had not written a progress note because the Ativan was to calm the resident for a blood transfusion and had not thought she needed to write a progress note.
On 9/19/22 at 2:08 PM, the survey team met with the LNHA and DON. The DON acknowledged that the behavior monitoring was inconsistent, and the documentation had not correlated with the use of PRN Ativan. The DON stated that she had no further information for the use of the PRN Ativan. The DON added that the use of a PRN medication should have a progress note that would indicate the need for use and if the medication was being used for behaviors, then the behavior monitoring should also correlate with the administration of the medication.
On 9/20/22 at 11:49 AM, the surveyor interviewed the RN#2 via the telephone who stated that she had administered the PRN Ativan to Resident #101 on 4/23/22. The RN#2 stated that she was told by the technician who was going to be doing the blood transfusion to administer the Ativan because the resident was anxious. The RN#2 stated that she thought she had written a progress note and that the resident was always nervous. The RN#2 added that she had to stay with the resident during the blood transfusion to keep the resident calm. The RN#2 stated that she thought that she had written a progress note.
On 9/20/22 at 12:24 PM, the surveyor interviewed LPN#3 who stated that she had administered the PRN Ativan on 5/5/22. The LPN#3 stated that the resident was frequently screaming and agitated with his/her spouse. The LPN#3 also stated that she was an agency nurse and would ask other staff who were familiar with the resident before administering a PRN medication. The LPN#3 added that she tried to change the resident's environment, offered a snack and tried to distract the resident before administering a medication. The LPN#3 stated that she documented the occurrence in the computerized communication log which does not remain for more than 2 days. The LPN#3 could not speak to documentation in the progress notes.
On 9/21/22 at 9:58 AM, the CP stated that she was unable to speak to the process of behavior monitoring and documentation because that was the responsibility of the CNO. The CP added that she had not done any in services on behavior monitoring or documentation since she was not involved in that process.
A review of the facility policy Behavior Assessment, Intervention and Monitoring dated as revised 1/2022 provided by the DON reflected that the General Guidelines included 1. Behavior is the response of the individual to a wide variety of factors. These factors may include medical, physical, functional, psychosocial, emotional, psychiatric or environmental causes. 2. Behavior is regulated by the brain and is influenced by past experiences , personality traits, environment, and interactions with other people. Behavior can be a way for an individual in distress to communicate unmet needs, indicate discomfort, or express thoughts that cannot be articulated. 4. Appropriate assessment and treatment of behavioral symptoms requires differentiating between behavioral symptoms that can be managed by treating underlying factors, and those that cannot. 5. Current guidelines recommend the use of non-pharmacological interventions for behavioral or psychological symptoms of dementia. In addition, for Monitoring the policy reflected that If the resident is being treated for altered behavior or mood, any improvements or worsening in the individual's behavior, mood, function will be documented in the clinical record. In addition, The IDT will monitor the progress of individuals with impaired cognition and behavior until stable. New or emergent symptoms will be documented and reported.
NJAC 8:39-27.1(a), 29.2 (d)