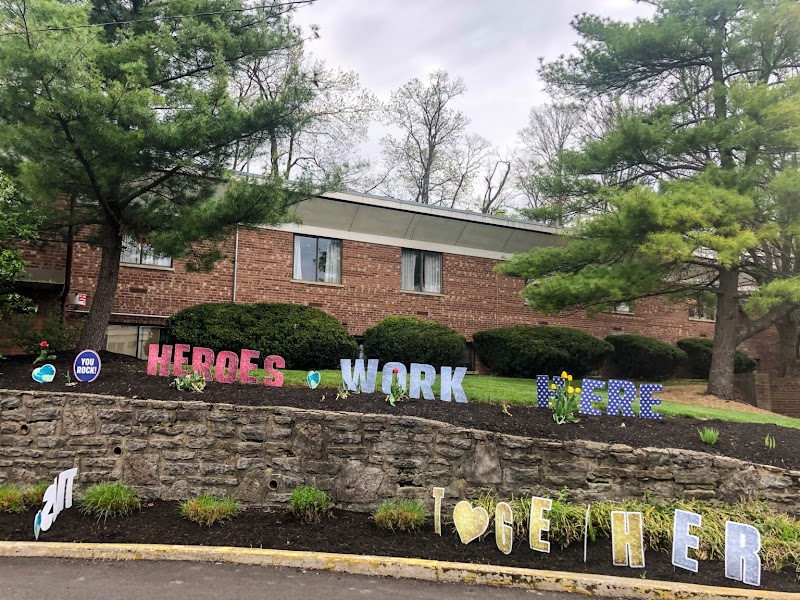
THE CHATEAU AT MOUNTAIN CREST NURSING & REHAB CTR



Within standard 12-15 month inspection cycle. Federal law requires annual inspections.
The Chateau at Mountain Crest Nursing & Rehab Center has received a Trust Grade of F, indicating significant concerns and poor overall performance. Ranking #793 out of 913 in Ohio places it in the bottom half of facilities in the state, and #60 out of 70 in Hamilton County means there are only nine local options that are worse. The facility's trend is worsening, as the number of reported issues increased from 12 in 2024 to 17 in 2025. Staffing is rated as average with a turnover rate of 59%, which is higher than the state average, while RN coverage is also average. However, the facility has been fined a concerning $297,729, which is higher than 95% of Ohio facilities, suggesting ongoing compliance issues. Specific incidents include serious failures in resident care, such as a resident developing severe pressure ulcers due to inadequate assessments and interventions, and another instance where a resident was injured in a wheelchair collision with an aggressive peer. Additionally, there was a case where a resident fell and sustained a head injury due to improper transfer assistance by staff. While there are some strengths, such as a 5-star quality measures rating, the numerous deficiencies and serious incidents raise significant red flags for families considering this facility.
- Trust Score
- F
- In Ohio
- #793/913
- Safety Record
- High Risk
- Inspections
- Getting Worse
- Staff Stability ⚠ Watch
- 59% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $297,729 in fines. Lower than most Ohio facilities. Relatively clean record.
- Skilled Nurses ○ Average
- Each resident gets 32 minutes of Registered Nurse (RN) attention daily — about average for Ohio. RNs are the most trained staff who monitor for health changes.
- Violations ⚠ Watch
- 74 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Below Ohio average (3.2)
Below average - review inspection findings carefully
13pts above Ohio avg (46%)
Frequent staff changes - ask about care continuity
Well above median ($33,413)
Significant penalties indicating serious issues
11 points above Ohio average of 48%
The Ugly 74 deficiencies on record
Jun 2025
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record reviews, observation, staff interviews, and policy review, the facility failed to ensure residents were ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, staff interviews, and review of a facility policy, the facility failed to ensure re...
Read full inspector narrative →
Apr 2025
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, staff interview, and facility policy review, the facility failed to notify the phys...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0685
(Tag F0685)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, resident and staff interview, and review of resident lists, the facility failed to ensure reside...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review, staff interview, interview with local health clinic staff, review of hospital docum...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, medical record review, staff interview, and facility policy review, the facility failed to provide timely ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, staff interview, and facility policy review, the facility failed to monitor weights...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0773
(Tag F0773)
Could have caused harm · This affected 1 resident
3. Review of the medical record for Resident #118 revealed an admission date of 08/13/24 with diagnoses of extradural and subdural abscess, osteomyelitis, and Arnold Chiari Syndrome.
Review of a phys...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0805
(Tag F0805)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident and staff interview, and medical record review, the facility failed to serve food in a form to to...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, medical record review, and policy review, the facility failed to ensure staff wore approp...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident and staff interviews, medical record review, review of service reports, and policy review, the fa...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, resident and resident family interview, staff interview, review of incident reports, and policy ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
Based on observation and staff interview, the facility failed to ensure medications were secure and inaccessible to unauthorized staff and residents. This had the potential to affect five (#31, #54, #...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, resident and staff interview, medical record review, and review of a facility policy, the facility failed ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
Based on observation and staff interview, the facility failed to store foods in a manner to prevent spoilage and failed to ensure kitchen staff appropriately wore hair restraints while in the kitchen....
Read full inspector narrative →
Jan 2025
2 deficiencies
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, resident and staff interviews and review of facility policy, the facility failed to maintain comfortable air temperatures and failed to provide a homelike environment. This affec...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0914
(Tag F0914)
Could have caused harm · This affected multiple residents
Based on observation, resident interview, and staff interview, the facility failed to ensure residents had full visual privacy as required. This affected nine (#01, #02, #03, #04, #05, #06, #08, #09, ...
Read full inspector narrative →
Oct 2024
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0678
(Tag F0678)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, staff interview, review of the facility policy, and review of online guidelines per the American...
Read full inspector narrative →
Oct 2024
3 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on review of the medical record, staff interview, and review of the facility policy, the facility failed to implement time...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on review of the medical record, staff interview, and review of the facility policy, the facility failed to implement timely care and treatment for pressure ulcers. This affected one (Resident #...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on medical record review, observation, staff interview, and review of the facility policy, the facility failed to ensure the medication error rate was below five percent. The medication error wa...
Read full inspector narrative →
Sept 2024
5 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Pressure Ulcer Prevention
(Tag F0686)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, staff interview, observation, and review of the facility policy, the facility failed to adequate...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected 1 resident
THE FOLLOWING DEFICIENCY REPRESENTS AN INCIDENT OF PAST NON-COMPLIANCE THAT WAS SUBSEQUENTLY CORRECTED PRIOR TO THIS SURVEY.
Based on record review, staff interview, review of facility Self-Reported I...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Incontinence Care
(Tag F0690)
Could have caused harm · This affected 1 resident
Based on medical record review, resident interview, staff interview, and review of the facility policy, the facility failed to provide adequate catheter care for residents with an indwelling urinary c...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, review of hospital discharge record, observation, resident interviews and staff interview the fa...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected 1 resident
Based on record review, observation, resident interview, and staff interview, the facility failed to provide an operational call light system which would allow for residents to alert staff of their in...
Read full inspector narrative →
Jun 2024
2 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, staff interview, review of the facility's investigation, review of witness statements, review of...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0825
(Tag F0825)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure a resident received therapy services as evaluated by the the...
Read full inspector narrative →
Jan 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation, interview,record review,review of the weather via website www.timeanddate.com, and facilities policy review, the facility failed to maintain a comfortable environment for 40 Resi...
Read full inspector narrative →
Sept 2023
1 deficiency
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0576
(Tag F0576)
Could have caused harm · This affected 1 resident
Based on observation, record review, resident interview, staff interview, and review of the facility policy, the facility failed to ensure residents had the right to have use of a telephone where call...
Read full inspector narrative →
May 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
Based on record review, staff interview, and policy review, the facility failed to ensure residents and resident representatives were provided with a care conference to provide input into the developm...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected 1 resident
Based on record review, staff interview, and review of the controlled substance sheets, the facility failed to administer as needed psychotropic medications for an appropriate indication and failed to...
Read full inspector narrative →
May 2023
2 deficiencies
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, staff interviews, review of facilities Self-Reported Incidents (SRIs), review of facilities inve...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, staff interviews, review of the facility's investigation, review of the facility's self-reported inciden...
Read full inspector narrative →
Apr 2023
1 deficiency
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Accident Prevention
(Tag F0689)
A resident was harmed · This affected 1 resident
Based on record review, observation, resident interview, staff interview, review of hospital reports, and review of facility policy, the facility failed to ensure staff safely assisted residents with ...
Read full inspector narrative →
Dec 2022
18 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Free from Abuse/Neglect
(Tag F0600)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, review of facility self-reported incident (SRI), review of facility investigations, observations...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Resident Rights
(Tag F0550)
Could have caused harm · This affected 1 resident
Based on medical record review, observation, staff interview and policy review, the facility failed to ensure privacy was provided during perineal care. This affected one (#97) of one resident reviewe...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 3. Medical record review for Resident #117 revealed an admission date of 07/08/22. Diagnoses include dementia with behaviors chr...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and staff interview, the facility failed to provide medications to residents when they are on a leave of ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0849
(Tag F0849)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on medical record review, observation, interview, hospice staff interview, review of the hospice contract, and review of t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, resident and staff interviews, the facility failed to provide a safe, clean comfortable and homelike envi...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Medical record review for Resident #57 revealed an admission date of 12/08/17 with diagnoses including but not limited to anx...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected multiple residents
Based on observations, staff interviews and review of the facility policy, the facility failed to ensure hazardous chemicals were securely stored out of the reach of confused and independently mobile ...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Medication Errors
(Tag F0758)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, staff interviews and policy review, the facility failed to ensure residents taking psychotropic medicati...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, record review, and policy review, the facility failed to ensure medications were prepared prope...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0919
(Tag F0919)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation and staff interview, the facility failed to ensure the call system was functioning on a secured unit to all...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0730
(Tag F0730)
Could have caused harm · This affected most or all residents
Based on employee record review and staff interview, the facility failed to provide annual evaluations to State Tested Nursing Assistants (STNA's). Additionally, the facility failed to provide the ann...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected most or all residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, staff interview, and policy/procedure review, the facility failed to label, date, and discard expired food...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0574
(Tag F0574)
Minor procedural issue · This affected most or all residents
Based on observations, resident interviews, staff interviews, and policy review, the facility failed to ensure information was available on how to contact the Ombudsman. This had the potential to affe...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0576
(Tag F0576)
Minor procedural issue · This affected most or all residents
Based on resident and staff interviews and review of the local post office business hours, the facility failed to ensure residents will have access to mail service on Saturdays. This affected six (#16...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Deficiency F0577
(Tag F0577)
Minor procedural issue · This affected most or all residents
Based on observation, resident and staff interviews, the facility failed to display the state agency survey results, where residents and visitors could visibly access them. This directly affected six ...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Grievances
(Tag F0585)
Minor procedural issue · This affected most or all residents
Based on observation, resident and staff interview, review of resident council minutes, the facility failed to ensure information was posted for residents and their representatives on how to file a gr...
Read full inspector narrative →
MINOR
(C)
Minor Issue - procedural, no safety impact
Abuse Prevention Policies
(Tag F0607)
Minor procedural issue · This affected most or all residents
Based on review employee personal files, staff interview, and policy review, the facility failed to implement their abuse policy by not doing the required reference checks on employee prior to hiring....
Read full inspector narrative →
Oct 2019
21 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0558
(Tag F0558)
Could have caused harm · This affected 1 resident
Based on record review, observation, resident and staff interview, and review of facility policy, the facility failed to ensure resident's were provided with water pitchers in their rooms in accordanc...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Notification of Changes
(Tag F0580)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation, and physician and staff interview, the facility failed to notify the doctor of a change in ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Abuse Prevention Policies
(Tag F0607)
Could have caused harm · This affected 1 resident
Based on record review, review of facility's Self-Reported Incidents, resident and staff interviews and review of facility policy, the facility failed to implement their policy when they did not repor...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected 1 resident
Based on resident and staff interviews, observation, record review, review of facility's Self-Reported Incidents and review of facility policy, the facility failed to report an allegation of misapprop...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, and resident and staff interview, the facility failed to complete Minimum Data Set (MDS) assessments whi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
Based on observation, staff interview and record review, the facility failed to implement comprehensive person-centered care plans. This affected one (#80) of 26 residents reviewed for care plans. The...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Quality of Care
(Tag F0684)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation and staff interview, the facility failed to provide professional standards of care for wound...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Pressure Ulcer Prevention
(Tag F0686)
Could have caused harm · This affected 1 resident
Based on observation, physician and staff interviews, and record review the facility failed to timely assess a pressure wound. This affected one (#110) of 28 residents reviewed for orders in the initi...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0687
(Tag F0687)
Could have caused harm · This affected 1 resident
Based on observation, record review and resident and staff interviews, the facility failed to provide ongoing podiatry care for residents. This affected one (#117) of one resident reviewed for foot ca...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, record review and staff interview, the facility failed to administer resident's medications with a medication error rate less than five percent. There were two medication errors ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected 1 resident
Based on observation, staff interview, and facility policy review, the facility failed to ensure infection control was maintained during medication administration. This affected two residents (#17 and...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0582
(Tag F0582)
Could have caused harm · This affected multiple residents
Based on record review and staff interview, the facility failed to issue the Notice to Medicare Provider Non-coverage (NOMNC) form and Skilled Nursing Facility Advanced Beneficiary Notice (SNFABN) for...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Transfer Notice
(Tag F0623)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 6. Review of Resident #40's medical records revealed an admission date of 04/16/12. Diagnoses included atherosclerotic heart dis...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0625
(Tag F0625)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 6. Review of Resident #40's medical records revealed an admission date of 04/16/12. Diagnoses included atherosclerotic heart dis...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Respiratory Care
(Tag F0695)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 4. Review of the medical record for the Resident #45 revealed an admission date of 05/15/15. Diagnoses included atrial fibrillat...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected multiple residents
3. Review of the medical record for the Resident #2 revealed an admission date of 12/31/18. Diagnoses included conversion disorder, mood disorder, anxiety and major depressive disorder.
Review of the...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, staff interview, and review of facility policy, the facility failed to ensure that food and beverage items were stored in the resident's snack and beverage utility rooms and in t...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0921)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Observation of residents smoking outside leisure unit on 10/22/19 at 11:30 A.M. revealed a large limb lying next to sidewalk ...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Social Worker
(Tag F0850)
Could have caused harm · This affected most or all residents
Based on review of personnel files, review of job description and staff interview, the facility failed to have a Licensed Social Worker (LSW) employed on a full-time basis. This had the potential to a...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
QAPI Program
(Tag F0867)
Could have caused harm · This affected most or all residents
Based on review of the Quality Assurance Performance Improvement (QAPI) meeting minutes and staff interview, the facility failed to ensure appropriate plans of action were in place to correct any iden...
Read full inspector narrative →
CONCERN
(F)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0868
(Tag F0868)
Could have caused harm · This affected most or all residents
Based on review of the Quality Assurance Performance Improvement (QAPI) meeting minutes and staff interview, the facility failed to ensure quarterly QAPI meetings were being conducted. This had the po...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "Why is there high staff turnover? How do you retain staff?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 4 harm violation(s), $297,729 in fines, Payment denial on record. Review inspection reports carefully.
- • 74 deficiencies on record, including 4 serious (caused harm) violations. Ask about corrective actions taken.
- • $297,729 in fines. Extremely high, among the most fined facilities in Ohio. Major compliance failures.
- • Grade F (10/100). Below average facility with significant concerns.
About This Facility
What is The Chateau At Mountain Crest Nursing & Rehab Ctr's CMS Rating?
CMS assigns THE CHATEAU AT MOUNTAIN CREST NURSING & REHAB CTR an overall rating of 2 out of 5 stars, which is considered below average nationally. Within Ohio, this rating places the facility higher than 0% of the state's 100 nursing homes. A rating at this level reflects concerns identified through health inspections, staffing assessments, or quality measures that families should carefully consider.
How is The Chateau At Mountain Crest Nursing & Rehab Ctr Staffed?
CMS rates THE CHATEAU AT MOUNTAIN CREST NURSING & REHAB CTR's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 59%, which is 13 percentage points above the Ohio average of 46%. High turnover can affect care consistency as new staff learn residents' individual needs.
What Have Inspectors Found at The Chateau At Mountain Crest Nursing & Rehab Ctr?
State health inspectors documented 74 deficiencies at THE CHATEAU AT MOUNTAIN CREST NURSING & REHAB CTR during 2019 to 2025. These included: 4 that caused actual resident harm, 65 with potential for harm, and 5 minor or isolated issues. Deficiencies causing actual harm indicate documented cases where residents experienced negative health consequences.
Who Owns and Operates The Chateau At Mountain Crest Nursing & Rehab Ctr?
THE CHATEAU AT MOUNTAIN CREST NURSING & REHAB CTR is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility operates independently rather than as part of a larger chain. With 167 certified beds and approximately 118 residents (about 71% occupancy), it is a mid-sized facility located in CINCINNATI, Ohio.
How Does The Chateau At Mountain Crest Nursing & Rehab Ctr Compare to Other Ohio Nursing Homes?
Compared to the 100 nursing homes in Ohio, THE CHATEAU AT MOUNTAIN CREST NURSING & REHAB CTR's overall rating (2 stars) is below the state average of 3.2, staff turnover (59%) is significantly higher than the state average of 46%, and health inspection rating (1 stars) is much below the national benchmark.
What Should Families Ask When Visiting The Chateau At Mountain Crest Nursing & Rehab Ctr?
Based on this facility's data, families visiting should ask: "How do you ensure continuity of care given staff turnover, and what is your staff retention strategy?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's high staff turnover rate.
Is The Chateau At Mountain Crest Nursing & Rehab Ctr Safe?
Based on CMS inspection data, THE CHATEAU AT MOUNTAIN CREST NURSING & REHAB CTR has a clean safety record: no substantiated abuse findings (meaning no confirmed cases of resident harm), no Immediate Jeopardy citations (the most serious violation level indicating risk of serious injury or death), and is not on the Special Focus Facility watch list (a federal program monitoring the lowest-performing 1% of nursing homes). The facility has a 2-star overall rating and ranks #100 of 100 nursing homes in Ohio. While no facility is perfect, families should still ask about staff-to-resident ratios and recent inspection results during their visit.
Do Nurses at The Chateau At Mountain Crest Nursing & Rehab Ctr Stick Around?
Staff turnover at THE CHATEAU AT MOUNTAIN CREST NURSING & REHAB CTR is high. At 59%, the facility is 13 percentage points above the Ohio average of 46%. High turnover means new staff may not know residents' individual needs, medications, or preferences. It can also be disorienting for residents, especially those with dementia who rely on familiar faces. Families should ask: What is causing the turnover? What retention programs are in place? How do you ensure care continuity during staff transitions?
Was The Chateau At Mountain Crest Nursing & Rehab Ctr Ever Fined?
THE CHATEAU AT MOUNTAIN CREST NURSING & REHAB CTR has been fined $297,729 across 4 penalty actions. This is 8.3x the Ohio average of $36,056. Fines at this level are uncommon and typically indicate a pattern of serious deficiencies, repeated violations, or failure to correct problems promptly. CMS reserves penalties of this magnitude for facilities that pose significant, documented risk to resident health or safety. Families should request specific documentation of what issues led to these fines and what systemic changes have been implemented.
Is The Chateau At Mountain Crest Nursing & Rehab Ctr on Any Federal Watch List?
THE CHATEAU AT MOUNTAIN CREST NURSING & REHAB CTR is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.