RAINBOW HEALTH CARE COMMUNITY AND RAINBOW ASSISTED




Inspected within the last 6 months. Data reflects current conditions.
Rainbow Health Care Community and Rainbow Assisted in Bristow, Oklahoma, has received a Trust Grade of F, indicating significant concerns about the quality of care provided. Ranking #127 out of 282 facilities in Oklahoma places them in the top half, while being #3 out of 7 in Creek County means only two local options are better. The facility is showing signs of improvement, reducing issues from 16 in 2024 to just 2 in 2025, which is encouraging. Staffing is average with a turnover rate of 49%, which is better than the state average of 55%. However, the facility has incurred $53,804 in fines, higher than 84% of facilities in the state, reflecting repeated compliance problems. There have been several concerning incidents, including a critical situation where a resident slid out of their wheelchair during transport and was left on the floor of the van for approximately 30 miles. Additionally, there was a serious issue involving a resident who developed sepsis due to inadequate monitoring of a surgical wound. Furthermore, the facility failed to ensure proper hand hygiene practices during care, which puts residents at risk for infection. While there are some strengths, such as the facility's ongoing improvement and average staffing levels, these serious deficiencies raise important questions about the care quality at this facility.
- Trust Score
- F
- In Oklahoma
- #127/282
- Safety Record
- High Risk
- Inspections
- Getting Better
- Staff Stability ⚠ Watch
- 49% turnover. Above average. Higher turnover means staff may not know residents' routines.
- Penalties ✓ Good
- $53,804 in fines. Lower than most Oklahoma facilities. Relatively clean record.
- Skilled Nurses ⚠ Watch
- Each resident gets only 22 minutes of Registered Nurse (RN) attention daily — below average for Oklahoma. Fewer RN minutes means fewer trained eyes watching for problems.
- Violations ⚠ Watch
- 25 deficiencies on record. Higher than average. Multiple issues found across inspections.
The Good
-
5-Star Quality Measures · Strong clinical quality outcomes
-
Full Sprinkler Coverage · Fire safety systems throughout facility
-
No fines on record
Facility shows strength in quality measures, fire safety.
The Bad
Near Oklahoma average (2.6)
Meets federal standards, typical of most facilities
Near Oklahoma avg (46%)
Higher turnover may affect care consistency
Above median ($33,413)
Moderate penalties - review what triggered them
Part of a multi-facility chain
Ask about local staffing decisions and management
The Ugly 25 deficiencies on record
Jul 2025
2 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0577
(Tag F0577)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to ensure the most recent survey results of the facility were posted in a place readily accessible to residents, family members and legal repres...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0761
(Tag F0761)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure a controlled medication was secured in a locked container that was permanently affixed to the building for 1 (#14) of ...
Read full inspector narrative →
Nov 2024
2 deficiencies
1 IJ
CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
On 11/07/24, an IJ situation was determined to exist related to the facilities failure to ensure staff were aware of proper transportation after a resident slid out of a wheelchair during a transport....
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure proper handwashing was conducted during incontinent care, between residents, and/or a roll gauze that was dropped on t...
Read full inspector narrative →
Mar 2024
13 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0578
(Tag F0578)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure residents were offered the opportunity to formulate an advance directive for one (#31) of three sampled residents who were reviewed ...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** 2. Res #16 had diagnoses that included abnormalities of gait and mobility, muscle wasting, lack of coordination, generalized wea...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Accident Prevention
(Tag F0689)
Could have caused harm · This affected 1 resident
Based on observation, record review and interview, the facility failed to ensure fall mats were properly placed for two (#43 and #10) of two resident who were reviewed for accident hazards.
The DON id...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
Based on record review and interview the facility failed to ensure nutritional supplements were provided as ordered for one (#73) of seven residents who were reviewed for nutrition.
The DON identified...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0700
(Tag F0700)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review, observation, and interview, the facility failed to assess the resident for risk of entrapment from bed r...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure side effect monitoring was implemented for anticoagulant medications for two (#3 and #129) of six sampled residents whose medication...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected 1 resident
Based on observation, record review, and interview, the facility failed to ensure the medication error rate was below five percent. A total of 28 opportunities were observed with two medication errors...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0848
(Tag F0848)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure arbitration agreements provided for the selection of a neutr...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Safe Environment
(Tag F0584)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure a sanitary environment in the shower rooms.
The DON identified 76 residents who reside at the facility.
Findings:
A Quality of Life-Ho...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0698
(Tag F0698)
Could have caused harm · This affected multiple residents
2. Res #25 had diagnoses that included end-stage renal disease, dependence on renal dialysis, and hypertension.
A physician order, dated 11/26/22, documented remove dressing to fistula to LUE six hour...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0809
(Tag F0809)
Could have caused harm · This affected multiple residents
Based on observation, interview, and record review, the facility failed to offer the residents an HS snack and ensure snacks were served to the residents in accordance with the facility policy, for th...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation, record review and interview, the facility failed to ensure the ice machine was clean.
The DON identified # residents ate from the kitchen.
Findings:
A Nutritional Services Sanita...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Infection Control
(Tag F0880)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure staff followed infection control protocols while delivering meals to residents in the dining room.
The administrator identified 76 res...
Read full inspector narrative →
Jan 2024
1 deficiency
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0604
(Tag F0604)
Could have caused harm · This affected multiple residents
Based on observation, record review, and interview, the facility failed to ensure residents were free from physical restraints which were not required to treat the resident's medical symptoms for one ...
Read full inspector narrative →
Jan 2023
4 deficiencies
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Staffing Information
(Tag F0732)
Could have caused harm · This affected 1 resident
Based on observation and interview, the facility failed to post nurse staffing information daily, which included all of the required components.
The Resident Census and Conditions of Residents form do...
Read full inspector narrative →
CONCERN
(D)
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
Based on record review and interview, it was determined the facility failed to ensure residents were free of duplicate medication dosage for one (#16) of five residents reviewed for unnecessary medica...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Unnecessary Medications
(Tag F0759)
Could have caused harm · This affected multiple residents
Based on record review, observation, and interview, the facility failed to ensure a medication administration error rate was less than five percent for two (#13 and #70) of five sampled residents obse...
Read full inspector narrative →
CONCERN
(E)
Potential for Harm - no one hurt, but risky conditions existed
Food Safety
(Tag F0812)
Could have caused harm · This affected multiple residents
Based on observation and interview, the facility failed to ensure:
a. the kitchen was maintained clean and in good repair, and;
b. staff did not handle foods with their bare hands.
The dietary manag...
Read full inspector narrative →
Nov 2022
3 deficiencies
1 Harm
SERIOUS
(G)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Actual Harm - a resident was hurt due to facility failures
Quality of Care
(Tag F0684)
A resident was harmed · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to assess and monitor a surgical site and failed to follow physician's...
Read full inspector narrative →
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0887
(Tag F0887)
Could have caused harm · This affected 1 resident
Based on record review and interview, the facility failed to ensure staff signed a consent indicating they had been educated on risks, benefits, and potential side effects of the COVID-19 vaccination ...
Read full inspector narrative →
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure resident records were complete, accurate, and readily access...
Read full inspector narrative →
Understanding Severity Codes (click to expand)
Questions to Ask on Your Visit
- "What changes have you made since the serious inspection findings?"
- "Can I speak with families of current residents?"
- "What's your RN coverage like on weekends and overnight?"
Our Honest Assessment
- • Licensed and certified facility. Meets minimum state requirements.
- • Multiple safety concerns identified: 1 life-threatening violation(s), 1 harm violation(s), $53,804 in fines. Review inspection reports carefully.
- • 25 deficiencies on record, including 1 critical (life-threatening) violation. These warrant careful review before choosing this facility.
- • $53,804 in fines. Extremely high, among the most fined facilities in Oklahoma. Major compliance failures.
- • Grade F (33/100). Below average facility with significant concerns.
About This Facility
What is Rainbow Health Care Community And Rainbow Assisted's CMS Rating?
CMS assigns RAINBOW HEALTH CARE COMMUNITY AND RAINBOW ASSISTED an overall rating of 3 out of 5 stars, which is considered average nationally. Within Oklahoma, this rating places the facility higher than 99% of the state's 100 nursing homes. This mid-range rating indicates the facility meets federal standards but may have areas for improvement.
How is Rainbow Health Care Community And Rainbow Assisted Staffed?
CMS rates RAINBOW HEALTH CARE COMMUNITY AND RAINBOW ASSISTED's staffing level at 3 out of 5 stars, which is average compared to other nursing homes. Staff turnover is 49%, compared to the Oklahoma average of 46%.
What Have Inspectors Found at Rainbow Health Care Community And Rainbow Assisted?
State health inspectors documented 25 deficiencies at RAINBOW HEALTH CARE COMMUNITY AND RAINBOW ASSISTED during 2022 to 2025. These included: 1 Immediate Jeopardy (the most serious level, indicating potential for serious harm or death), 1 that caused actual resident harm, and 23 with potential for harm. Immediate Jeopardy findings are rare and represent the most serious regulatory concerns. They require immediate corrective action.
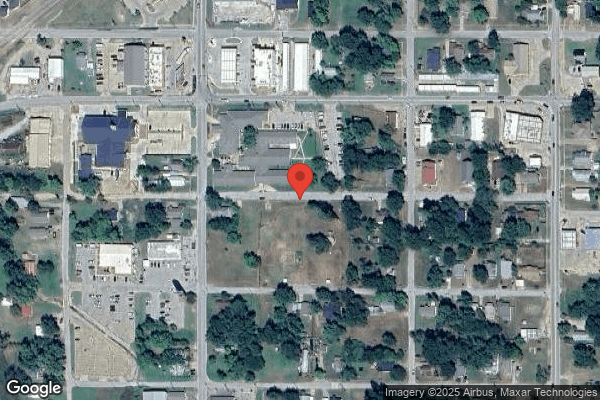
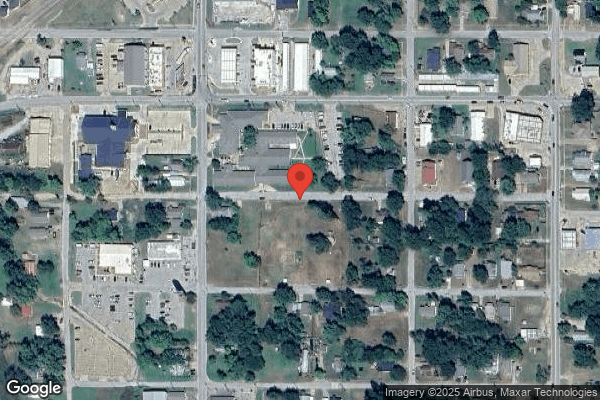
Who Owns and Operates Rainbow Health Care Community And Rainbow Assisted?
RAINBOW HEALTH CARE COMMUNITY AND RAINBOW ASSISTED is owned by a for-profit company. For-profit facilities operate as businesses with obligations to shareholders or private owners. The facility is operated by MGM HEALTHCARE, a chain that manages multiple nursing homes. With 106 certified beds and approximately 75 residents (about 71% occupancy), it is a mid-sized facility located in BRISTOW, Oklahoma.
How Does Rainbow Health Care Community And Rainbow Assisted Compare to Other Oklahoma Nursing Homes?
Compared to the 100 nursing homes in Oklahoma, RAINBOW HEALTH CARE COMMUNITY AND RAINBOW ASSISTED's overall rating (3 stars) is above the state average of 2.6, staff turnover (49%) is near the state average of 46%, and health inspection rating (2 stars) is below the national benchmark.
What Should Families Ask When Visiting Rainbow Health Care Community And Rainbow Assisted?
Based on this facility's data, families visiting should ask: "What changes have been made since the serious inspection findings, and how are you preventing similar issues?" "Can I visit during a mealtime to observe dining assistance and food quality?" "How do you handle medical emergencies, and what is your hospital transfer rate?" "Can I speak with family members of current residents about their experience?" These questions are particularly relevant given the facility's Immediate Jeopardy citations.
Is Rainbow Health Care Community And Rainbow Assisted Safe?
Based on CMS inspection data, RAINBOW HEALTH CARE COMMUNITY AND RAINBOW ASSISTED has documented safety concerns. Inspectors have issued 1 Immediate Jeopardy citation (the most serious violation level indicating risk of serious injury or death). The facility has a 3-star overall rating and ranks #1 of 100 nursing homes in Oklahoma. Families considering this facility should ask detailed questions about what corrective actions have been taken since these incidents.
Do Nurses at Rainbow Health Care Community And Rainbow Assisted Stick Around?
RAINBOW HEALTH CARE COMMUNITY AND RAINBOW ASSISTED has a staff turnover rate of 49%, which is about average for Oklahoma nursing homes (state average: 46%). Moderate turnover is common in nursing homes, but families should still ask about staff tenure and how the facility maintains care continuity when employees leave.
Was Rainbow Health Care Community And Rainbow Assisted Ever Fined?
RAINBOW HEALTH CARE COMMUNITY AND RAINBOW ASSISTED has been fined $53,804 across 1 penalty action. This is above the Oklahoma average of $33,617. Fines in this range indicate compliance issues significant enough for CMS to impose meaningful financial consequences. Common causes include delayed correction of deficiencies, repeat violations, or care failures affecting resident safety. Families should ask facility leadership what changes have been made since these penalties.
Is Rainbow Health Care Community And Rainbow Assisted on Any Federal Watch List?
RAINBOW HEALTH CARE COMMUNITY AND RAINBOW ASSISTED is not on any federal watch list. The most significant is the Special Focus Facility (SFF) program, which identifies the bottom 1% of nursing homes nationally based on persistent, serious quality problems. Not being on this list means the facility has avoided the pattern of deficiencies that triggers enhanced federal oversight. This is a positive indicator, though families should still review the facility's inspection history directly.