CRITICAL
(J)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Immediate Jeopardy (IJ) - the most serious Medicare violation
Accident Prevention
(Tag F0689)
Someone could have died · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure residents remained free from accidents, haza...
Read full inspector narrative →
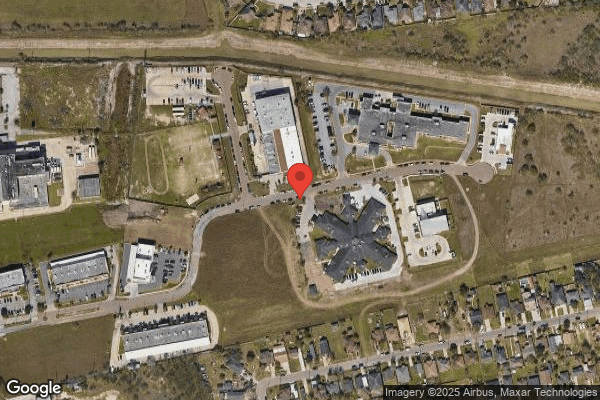
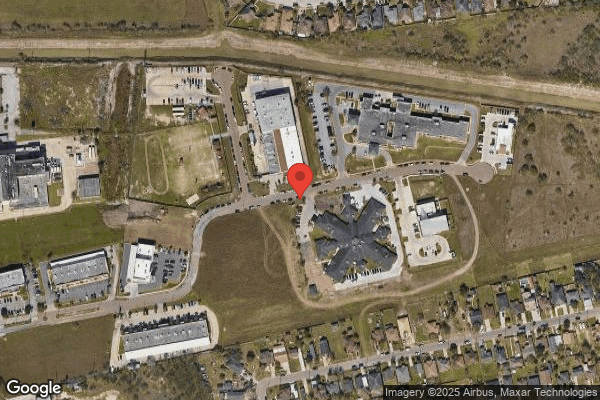
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure residents remained free from accidents, hazards and each resident received adequate supervision and assistance while providing care for 1 of 5 residents (Resident #1) reviewed for accidents and supervision. The facility failed to ensure Resident #1 received supervision when outside in his wheelchair. Resident #1 wheeled his way down the parking lot to the road, flipping his wheelchair where the parking lot met the roadway pinning Resident #1 on the roadway where he was unable to get up. The non-compliance was identified as past non-compliance. The Immediate jeopardy began on 12/31/2024 and ended on 01/02/2025. The facility had corrected the noncompliance before the survey began. This deficient practice has the potential to affect all residents in the building by causing resident injuries, such as falls, fractures, and even death due to improper supervision. The findings included: Record review of Resident #1's admission record dated 06/17/2025 revealed he was a [AGE] year-old male with an admission date of 12/27/2024. Diagnoses included dementia (the loss of cognitive functioning - thinking, remembering, and reasoning - to such an extent that it interferes with a person's daily life and activities), and osteoarthritis (a degenerative joint disease, in which the tissues in the joint break down over time). Record review of Resident #1's Care Plan dated 12/31/2024 revealed: FOCUS: o CANCELLED: Resident #1 is an elopement risk/wanderer r/t Dementia Date Initiated: 01/02/2025 Revision on: 01/31/2025 Cancelled Date: 01/31/2025 GOALS: o CANCELLED: The resident's safety will be maintained through the review date. Date Initiated: 12/31/2024 Revision on: 01/31/2025 Target Date: 01/15/2025 Cancelled Date: 01/31/2025 INTERVENTIONS/TASKS: o CANCELLED: Distract resident from wandering by offering pleasant diversions, structured activities, food, conversation, television, book. Resident prefers: Date Initiated: 12/31/2024 Revision on: 01/31/2025 Cancelled Date: 01/31/2025 ACTA CNA LN RN SS 01/31/2025 o CANCELLED: Provide structured activities: toileting, walking inside and outside, reorientation strategies including signs, pictures and memory boxes. Date Initiated: 12/31/2024 Revision on: 01/31/2025 Cancelled Date: 01/31/2025 ACTA CNA 01/31/2025 o CANCELLED: Pt Wandering seeking to exit. Wander guard placed for safety and monitoring. Date Initiated: 12/31/2024 Revision on: 01/31/2025 Cancelled Date: 01/31/2025 LN RN SS 01/31/2025. Record review of Resident #1's admission MDS dated [DATE] revealed Resident #1 had severe cognitive impairment with a BIMS of 03. Wandering impact was blank. Resident #1 was substantial/maximal assistance (Helper does more than half the effort) for ADLs. Record review of Resident #1's Wandering Evaluation dated 12/27/2024 revealed Resident #1 was not a wandering risk. Record review of Resident #1's Progress Notes revealed on 12/31/24 at 01:15 PM, Resident #1 had an unwitnessed fall from his wheelchair outside the facility. Record review of 12/31/24 at 03:45 PM Progress Notes for Resident #1 revealed on assessment, Resident #1 sustained a 1-inch abrasion to his right elbow when he fell. Observation on 06/19/25 at 08:15 AM revealed from the front door of the facility to the road in front of the facility where Resident #1 fell out of his wheelchair, while unsupervised on 12/31/24 at 01:15 PM, is approximately 150 feet. The road outside the facility is a busy road with a hospital across the street with cars parked on both sides of the roadway making visibility difficult for oncoming cars. Review of the weather on 12/31/24 at 01:15 PM revealed it was 72 degrees and clear. Record review of Resident #1's Progress Notes dated 12/31/24 at 03:45 PM written by LVN F revealed Resident #1 had an unwitnessed fall outside. Resident #1 was assessed. The Doctor and RP were notified. The Doctor ordered STAT x-ray of skull, shoulders bilaterally, femur bilateral, hip bilaterally, humerus bilaterally, ankles bilaterally, elbows bilaterally, and wrist bilaterally. Results negative for fracture or injury. Resident #1 had no complaints of pain and verbalized refusal to take pain medication. Record review of Resident #1's Progress Notes dated 01/01/2025 at 05:55 AM written by LVN C revealed LVN C reported x-ray results to doctor. LVN C notes there were no new orders given. Record review of Resident #1's Progress Notes dated 12/31/2024 at 08:29 PM written by LVN C revealed S/P Fall 24 hours: Resident in his bedroom without complain of pain or discomfort. Resident continues with wander guard placed on the right ankle. No seeking behaviors noted at this time. Record review revealed between 12/31/2024 - 01/02/2025, staff and residents were interviewed, in-services on Abuse/Neglect, Elopement, Notifying Nurses of Residents Going Outside re-education for all staff was initiated and ongoing. Record review of Resident #1's Care Plan was updated on 01//02/2024 to include elopement risk/wanderer/ related to dementia with intervention of a wander guard. Record review of Resident #1's Progress Notes dated 01/06/2025 at 02/27 PM written by LVN W revealed Resident #1's wander guard to his right ankle was removed due to resident was not exit seeking. Resident #1's wander guard was removed, and a nonskid placement pad applied to the resident's wheelchair. Record review on 06/20/2025 revealed Receptionist JJ was not trained on Notifying Nurses of Residents Going Outside prior to the incident on 12/31/2024. In an interview on 06/1920/25 at 11:24 AM a visitor stated on 12/31/24 around 01:15 PM she was arriving at the facility to visit another resident. She said she was trying to find a parking spot when she noticed a resident in a wheelchair trying to escape down the parking lot. The visitor stated the resident reached the road, and his wheelchair hit the pothole between the parking lot and the road. She said the wheelchair tipped over and threw the resident out of the wheelchair, and it landed on top of him. She said she ran to him and took the wheelchair off him and helped him back into his wheelchair. The visitor stated she asked the resident where he was going, and he told her he was going downtown. She said at that time staff started coming down to help the resident. She did not know how the staff found out the resident had fallen. In an interview on 06/19/2025 at 01:08 PM BOM G stated the receptionist was the one who told her a resident had fallen outside. BOM G stated she when she went out, Resident #1 was on the ground with his wheelchair next to him. She said at the time, the visitor, the receptionist, ADON H, ADON I, and the Interim Administrator were there. BOM G stated Resident #1 said he was moving, tripped, and he was fine. In an interview on 06/19/2025 at 01:15 PM LVN F stated on 12/31/2024 he was at the nurse's station when he was told Resident #1 had fallen outside. LVN F stated he stayed at the nurse's station when the other nurses ran outside. LVN F stated he remembers when the resident came back in, and LVN F stated the resident was assessed by him and ADON I who was no longer working at the facility. LVN F stated he thinks he remembers a skin tear, but he was unsure. LVN F stated if a resident had a BIMS of 13 or more, they could sign themselves out of the building, but if the BIMS was less than 13, a family member, nurse, or CNA had to sign or take them out. He said sometimes Activities would take a resident out, but they had to clear it with the nurse before they would take them out. In an interview on 06/19/25 at 09:35 AM The DON stated Receptionist JJ was terminated on 01/14/2025 for taking Resident #1 outside and leaving him unsupervised. Termination papers along with file reviewed by surveyor. In an interview on 06/19/2025 at 04:55 PM, the DON stated if a resident wanted to go outside, the DON could take the resident outside. He said if a family member, with the RP's permission, could take their resident outside, or a CNA could, or a nurse could. The DON stated if the resident had a good BIMS of 13 or above, they could go outside alone and if the BIMS is less than 13, they would have to be supervised. The DON stated the door at the front was always locked so the receptionist had to screen before opening the door. The DON stated Code Yellow was announced for missing residents. He said the last in-services on elopement, residents going outside were last Monday (06/16/25) and they are on-going. In an interview on 06/19/2025 at 05:17 PM The Administrator stated a resident could go outside by themselves would depend on their BIMS. He said for a BIMS of 13 or above they can sign themselves out. If their BIMS was 13 or below, they cannot go outside unsupervised. The Administrator stated they had to be signed out by a family member, but the RP had to agree to a family member signing the resident out, by a nurse. The Administrator stated Code Yellow was announced to the facility if a resident was missing. He said they had monthly drills on elopement so everyone would know what to do in the event a resident was missing. The Administrator stated last Friday, 06/13/2025, he had an all staff meeting and went over elopements, residents going out by themselves (who can and who cannot), and abuse/neglect. The facility had corrected the noncompliance before the survey began as followed: Record review of the following interventions put into place: 1. Record review of Resident #1's medical record revealed Resident #1 was assessed by the nurse, findings reported to doctor, and x-rays ordered. 2. Record review of Resident #1's Wandering Evaluation dated 12/31/2024 revealed he was a wander risk. 3. Record review of Resident #1's skin assessment dated [DATE] revealed abrasion to right elbow with slight bleeding and a skin tear to his left knee details. 4. Record review of Resident #1's neurological checks dated 12/31/2024 revealed were started at 01:20 PM. 5. Record review of Resident #1's medical record showed wander guard was placed on 12/31/2024. 4. Record review of in-service education dated 12/31/2024-01/02/25 revealed all staff including direct care staff were in-serviced on Abuse/Neglect, Elopement, and Notifying Nurses of Residents Going Outside. 5. Record review of questionnaires dated 12/31/2024-01/02/2025 reflected all staff were quizzed on Abuse/Neglect, Elopement, and Notifying Nurses of Residents Going Outside. 6. Record review of Resident #1's Care Plan was updated to include wandering risk, wander guard, and injuries sustained with interventions. 7. Record review of revealed the facility investigated the incident and Receptionist JJ was terminated for taking and leaving Resident #1 outside unsupervised. 8. Record review revealed facility reported the incident to State within the correct timeframe. On 06/19/2025, 2 Receptionists, 1 Activity Aide and 1 Activity Director, 1 Human Resource Coordinator, 1 Housekeeper, 1 Medication Aide, 1 Hospitality Aide, 9 CNAs, 1 MDS LVN, 12 LVNs, 1 RN, the DON, and the Administrator were interviewed on policy/procedures on Abuse/Neglect, Elopement, and for residents going outside supervised and unsupervised, Code Yellow for missing residents, and in-services. All staff were able to state the correct policy/procedures. In an interview on 06/19/25 at 05:17 PM the Administrator stated they had an all staff meeting on Friday, 06/13/25, in-servicing on Abuse/Neglect, Elopement, and Notifying Nurses of Residents Going outside and the in-services were ongoing. He said they had monthly Elopement Drills with the staff. Record review of facility's policy titled Going Outside Policy undated, revealed The resident's stay with the facility is voluntary. The resident may leave the facility temporarily on therapeutic leave at any time. The resident or responsible party shall follow the facility rules regarding signing in and out of the facility whenever he or she leaves the facility. Record review of facility's policy Elopements and Wandering Residents dated 11/21/2022 revealed: Policy: This facility ensures that residents who exhibit wandering behavior and/or are at risk for elopement receive adequate supervision to prevent accidents and receive care in accordance with their person-centered plan of care addressing the unique factors contributing to wandering or elopement risk. Policy Explanation and Compliance Guidelines: 1.The facility may be equipped with door locks/alarms to help avoid elopements. 2. Alarms are not a replacement for necessary supervision. Staff are to be vigilant in responding to alarms in a timely manner. 4.Monitoring and Managing Residents at Risk for Elopement or Unsafe Wandering d. Adequate supervision will be provided to help prevent accidents or elopements.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0552
(Tag F0552)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, and record reviews the facility failed to ensure the residents right to be informed of the risks and benefi...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, and record reviews the facility failed to ensure the residents right to be informed of the risks and benefits of proposed care, of treatment and treatment alternatives or treatment options and to choose the alternative or option he or she prefers, for 1 of 5 residents (Resident #3, Resident #6 ) reviewed for consent for antipsychotic medications in that:
1. Resident #3 was prescribed and administered Haldol (an antipsychotic) without prior consent based on information of the benefits, risks, and options available.
2. The facility failed to ensure psychoactive medication consents for Resident #6's were signed and dated by his guardian for the use of Zyprexa (antipsychotic medication), Buspirone (anxiolytic medication), lorazepam (benzodiazepine medication), and Risperidone (antipsychotic medication).
These failures could affect the right to self-determination of all facility residents who receive medication by allowing them to receive medication without their prior knowledge or consent, or that of their responsible party or emergency contacts.
The findings included:
1. Record review of Resident #3's admission record dated 06/17/2025, revealed an admission date of 08/15/2024, and a re-admission date on 11/25/2024, with a diagnoses which included dementia (a group of thinking and social symptoms that interferes with daily functioning) without behavioral disturbance, psychotic disturbance (delusions and hallucinations), mood disturbance, and anxiety, and traumatic subdural hemorrhage (a type of bleeding near the brain that can happen after a head injury) with loss of consciousness of 30 minutes or less.
Record review of Resident #3's admission MDS, dated [DATE], revealed a BIMS of 01, indicating severe cognitive impairment. There were no potential indicators of psychosis, and no behavioral symptoms were indicated. Active diagnoses included: traumatic brain dysfunction (an impairment in the normal functioning of the brain caused by an outside force, usually a violent blow to the head), and dementia. Resident #3 was not receiving an antipsychotic.Record review of Resident #3's Progress Note written by LVN J, dated 10/28/2024 at 11:18 AM revealed, As per NP (S), new order for Haldol Deconate 50mg IM Q month for aggression behavior.
Record review of Resident #3's Progress Note Orders - Administration Note on 10/28/2024 written by LVN J revealed This order is outside of the recommended dose or frequency. Haldol Decanoate Intramuscular Solution 50 MG/ML (Haloperidol Decanoate) Inject 50 mg intramuscularly one time a day every 1 month(s) starting on the 28th for 1 day(s) for 50mg IM Q month - The frequency of monthly is below the usual frequency of every 28 days.Record review of Resident #3's Progress Note dated 10/29/2024 at 08:18 PM written by LVN K, revealed Administered monthly haloperidol.Record review of resident #3's care plan, dated 11/19/2024, revealed:FOCUS: The resident uses antipsychotic medications (HALDOL) r/t AGITATION Date Initiated: 11/19/2024 Revision on: 11/19/2024.GOALS: Resident will have no injuries related to medication usage Date Initiated: 11/19/2024 Target Date: 12/31/2024.INTERVENTIONS/TASKS: o psych consult Date Initiated: 11/19/2024 Revision on: 11/19/2024 LN o Discuss side effects of medications with resident/RP Date Initiated: 11/19/2024 LN o Keep environment free of clutter and safety hazards Date Initiated: 11/19/2024 LN o Monitor behaviors. Notify MD of new or worsening behaviors Date Initiated: 11/19/2024 LN SS o Monitor vital signs as ordered by MD and PRN Date Initiated: 11/19/2024 LN o Monitor/document/report PRN any adverse reactions of antipsychotic medications: unsteady gait, tardive dyskinesia, EPS (shuffling gait, rigid muscles, shaking), frequent falls, refusal to eat, difficulty swallowing, dry mouth, depression, suicidal ideations, social isolation, blurred vision, diarrhea, fatigue, insomnia, loss of appetite, weight loss, muscle cramps nausea, vomiting, behavior symptoms not usual to the person. Date Initiated: 11/19/2024 LN.
Record review of Resident #3's medical record did not reveal consent for the antipsychotic Haldol until 02/22/2025.During an interview on 06/25/2025 at 03:38 PM Resident #3's RP stated she had gone to the facility sometime around February to sign a consent for a medication they wanted to give Resident #3. The RP stated she could not remember the name of the medication. She said they told her it was for sleep because he woke up in the night and because he walked around.
During an interview on 06/26/2025 at 01:14 PM LVN P stated for an antipsychotic to be given to a resident, the LVN needed to make sure she had a consent form, the correct diagnosis, the right reason, the right time, the right route, the right patient, and the right documentation.
During an interview on 06/26/2025 at 01:48 PM LVN K stated he could not recall if he had administered the Haldol injection to Resident #3 on 10/29/2024 or not. He stated he had just started working as a nurse at the facility (October 2024). LVN K stated Resident #3 did not have behavior.
In an interview on 06/26/25 at 05:33 PM the DON stated to administer an antipsychotic; consent must be signed prior to giving an antipsychotic. The DON stated he had seen the consent for the Haldol for Resident #3 had been signed in February 2025. The DON stated the consent should have been signed by the RP and checked by the nurse before the Haldol was administered.
2. Record review of Resident #6’s admission record dated 09/06/24, revealed a [AGE] year-old male with diagnoses which included: Alzheimer’s disease, unspecified dementia, unspecified severity, without behavioral disturbance, psychotic disturbance, mood disturbance, anxiety and cognitive communication deficit.
Record review of Resident #6’s quarterly MDS assessment dated [DATE] revealed resident had a BIMS score of 6 indicating moderately impaired cognition and that Resident #6 was taking antipsychotic and antianxiety medications.
Record review of Resident #6’s physician orders revealed orders which included the following:
Zyprexa 2.5MG tablet Give 1 tablet by mouth two times a day for mood disorder effective 09/14/24; Zyprexa 5MG tablet Give 1 tablet by mouth three times a day for agitation effective 12/17/24; Buspirone 5MG tablet Give 1 tablet by mouth two times a day for mood disorder effective 03/19/25;
Lorazepam 0.5MG tablet Give 1 tablet by mouth every 12 hours as needed for mood disorder effective 01/08/25; Risperidone 0.25MG tablet Give 1 tablet by mouth one time a day for mood disorder effective 04/04/25.
Record review of Resident #6’s MAR revealed Zyprexa, Buspirone, and Lorazepam had been administered on dates prior to have received the signed consents.
Record review of Resident #6’s “Informed Consent for Psychoactive Medications” for Zyprexa 2.5MG and Zyprexa 5MG revealed both forms were signed and dated by the doctor and resident’s RP on 05/22/25.
Record review of Resident #6’s “Informed Consent for Psychoactive Medications” for Buspirone revealed the form was signed by the doctor but was not dated. The same form revealed resident’s RP signed and dated on 05/21/25.
Record review of Resident #6’s “Informed Consent for Psychoactive Medications” for Buspirone revealed a second consent form was signed and dated by the doctor and resident’s RP on 06/25/25.
Record review of Resident #6’s “Informed Consent for Psychoactive Medications” for lorazepam revealed the form was signed and dated by the doctor and resident’s RP on 06/27/25.
Record review of informed consents revealed there was no actual consent form for Risperidone.
Interview was attempted with Resident #6 on 07/14/25 at 9:35 am but resident was unable to answer any medication questions.
During an interview on 07/14/25 at 10:28 am, LVN F stated that when a doctor gave an order for an antipsychotic medication, the nurse was to verify the order and make sure it was correct. Once the order was verified that it was correct, then the consent is needed from the family, either verbally or signed on paper. LVN F stated that verbal orders that were obtained by the phone, were to be verified with another nurse present during the phone call. Once the family gave consent, LVN F stated both nurses were to sign the form and then hand the form off to the medical records office. LVN F stated that the ADON H, ADON I, or the DON were
responsible for reviewing the consents that were submitted for the new orders that were received.
During an interview on 07/14/25 at 3:37 pm, MDS D stated that when a psychotropic medication was ordered by a doctor, the nurse that received the order had to obtain the family’s consent before the medication was given. MDS D stated that consents, either verbal or in person, are signed off on a paper form. MDS D verified which one of Resident #6’s medications needed a consent. MDS D stated that Zyprexa 2.5MG and Zyprexa 5MG, Buspirone, Lorazepam, and Risperidone all needed consents. The consents for Zyprexa, Buspirone and lorazepam had been uploaded to their computer system however the consent form for Risperidone was not found. MDS D stated those were the only consents she was able to find in the system for Resident #6.
During an interview on 07/15/25 at 10:39 am, the DON stated that when a doctor gave an order for an antipsychotic, consent from the family was required. The DON stated that the family was informed of the new order and the family was allowed to give consent or refuse. If the family gave consent over the phone, then two nurses received the verbal consent and both nurses signed the actual consent form. The DON stated that consents were monitored every morning during the reports from the morning meeting. The DON stated that new medications or new orders were discussed in every morning meeting. The DON stated that ADON H, ADON I, or he himself would review that the forms have been signed correctly. If the consent had not been done, there would be a hold on medication administration and notify the doctor that the medication was not administered. The DON reviewed Resident #6’s medication administration record and stated the medications had been administered on dates prior to have received the written consent forms. The DON states he was unaware the consent forms had not been signed by RP nor by the doctor.
A record review of the facility's policy Nursing Facility Residents' Rights, dated November 2021, revealed, Participation in Your Care
You have the right to:
-Have any psychoactive medications prescribed and administered in a responsible manner as mandated by the Texas Health and Safety Code, 242.505, and refuse to consent to the prescription of psychoactive medications.
A record review of the facility's policy Use of Psychotropic Medication(s), dated 03/05/25, revealed, Policy Explanation and Compliance Guidelines:
9. Prior to initiating or increasing a psychotropic medication, the resident, family, and/or resident representative must be informed of the benefits, risks, and alternatives for the medication, including any black box warnings for antipsychotic medications, in advance of such initiation or increase.
10. The resident has the right to accept or decline the initiation or increase of psychotropic medication.
11. The facility will document that the resident or resident representative was informed in advance of the risks and benefits of the proposed care, the treatment alternatives or other options and the preferred option to accept or decline in a format the facility deems to use (e.g., written consent form, narrative note, etc.).
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Assessment Accuracy
(Tag F0641)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, and record review, the facility failed to ensure the assessment accurately reflected the resident's status ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, and record review, the facility failed to ensure the assessment accurately reflected the resident's status for 1 (Resident #3) of 5 residents reviewed for accuracy of assessments.
The facility failed to ensure Resident #3 was evaluated before administering an antipsychotic (Haldol).
This failure could place residents at risk of receiving care and services to meet their needs.
The findings included:
Record review of Resident #3's admission record dated 06/17/2025, revealed an admission date of 08/15/2024, and a re-admission date on 11/25/2024, with a diagnoses which included dementia (a group of thinking and social symptoms that interferes with daily functioning) without behavioral disturbance, psychotic disturbance (delusions and hallucinations), mood disturbance, and anxiety, and traumatic subdural hemorrhage (a type of bleeding near the brain that can happen after a head injury) with loss of consciousness of 30 minutes or less.
Record review of Resident #3's admission MDS, dated [DATE], revealed a BIMS of 01, indicating severe cognitive impairment. There were no potential indicators of psychosis, and no behavioral symptoms were indicated. Active diagnoses included: traumatic brain dysfunction (an impairment in the normal functioning of the brain caused by an outside force, usually a violent blow to the head), and dementia. Resident #3 was not receiving an antipsychotic.
Record review of Resident #3's chart 10/25/2024 through 06/26/2025, revealed no evaluations were completed prior to Haldol being administered.
Record review of Resident #3's Progress Note written by LVN J, dated 10/28/2024 at 11:18 AM revealed, As per NP (NP S), new order for Haldol Decanoate 50mg IM Q month for aggression behavior.
Record review of Resident #3's Progress Note on 10/28/2024 at 11:19 AM written by LVN J revealed, Orders - Administration Note: This order is outside of the recommended dose or frequency. Haldol Decanoate Intramuscular Solution 50 MG/ML (Haloperidol Decanoate) Inject 50 mg intramuscularly one time a day every 1 month(s) starting on the 28th for 1 day(s) for 50mg IM Q month - The frequency of monthly is below the usual frequency of every 28 days.
Record review of Resident #3's Progress Note dated 10/29/2024 at 08:18 PM written by LVN K, revealed Administered monthly haloperidol.
Record review of resident #3's care plan, dated 11/19/2024, revealed:
FOCUS: o The resident uses antipsychotic medications (HALDOL) r/t AGITATION Date Initiated: 11/19/2024 Revision on: 11/19/2024.
GOALS: o Resident will have no injuries related to medication usage Date Initiated: 11/19/2024 Target Date: 12/31/2024.
INTERVENTIONS/TASKS: o psych consult Date Initiated: 11/19/2024 Revision on: 11/19/2024 LN o Discuss side effects of medications with resident/RP Date Initiated: 11/19/2024 LN o Keep environment free of clutter and safety hazards Date Initiated: 11/19/2024 LN o Monitor behaviors. Notify MD of new or worsening behaviors Date Initiated: 11/19/2024 LN SS o Monitor vital signs as ordered by MD and PRN Date Initiated: 11/19/2024 LN o Monitor/document/report PRN any adverse reactions of antipsychotic medications: unsteady gait, tardive dyskinesia, EPS (shuffling gait, rigid muscles, shaking), frequent falls, refusal to eat, difficulty swallowing, dry mouth, depression, suicidal ideations, social isolation, blurred vision, diarrhea, fatigue, insomnia, loss of appetite, weight loss, muscle cramps nausea, vomiting, behavior symptoms not usual to the person. Date Initiated: 11/19/2024 LN.
In an interview on 06/26/25 at 10:25 AM PA N stated she was the one who discontinued Resident #3's Haldol order on 06/19/2025. She said she spoke to MD O about the Haldol order for Resident #3, and they decided they wanted Resident #3 to evaluated by psychiatric services. PA N stated she did not see on the notes where Resident #3 had been evaluated. PA N stated before giving Haldol a resident would have to be evaluated by psych first.
In an interview on 06/26/25 at 02:16 AM LVN Q stated she called PA N to have Resident #3's Haldol discontinued on 06/19/2025 due to checking the chart with resident had no behaviors and no evaluation. LVN Q stated she received an order for psychiatric services to come evaluate Resident #3.
In an interview on 06/26/2025 at 05:33 PM, the DON stated to administer an antipsychotic, an evaluation needed to be done prior to giving the antipsychotic.
A record review of the facility's policy Use of Psychotropic Medication(s), dated 03/05/25, revealed,
Policy Explanation and Compliance Guidelines:
5.The indications for initiating, maintaining, or discontinuing medication(s), as well as the use of nonpharmacological approaches, will be determined by evaluating the resident's physical, behavioral, mental, and psychosocial signs and symptoms in order to identify and rule out any underlying medical conditions, including the assessment of relative benefits and risks, and the preferences and goals for treatment.
7. The resident's medical record shall include documentation of this evaluation and the rationale for chosen treatment options.
13.Residents who receive an antipsychotic medication will have an Abnormal Involuntary Movement Scale (AIMS) test performed on admission, every six months, with a significant change in condition, change in antipsychotic medication, PRN or as per facility policy.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Comprehensive Care Plan
(Tag F0656)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, and record review the facility failed to develop and implement a comprehensive person-centered care plan fo...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interviews, and record review the facility failed to develop and implement a comprehensive person-centered care plan for each resident, consistent with the resident rights, that included measurable objectives and timeframes to meet a resident's medical, nursing, and mental and psychosocial need that were identified in the comprehensive assessment for 1 of 5 residents (Resident #2) reviewed for comprehensive person-centered care plans.The facility failed to develop interventions in a comprehensive person-centered care plan for Resident #2 to address his behavior of putting small items in his mouth such as crayons.This deficient practice could place residents at risk of not being provided with the necessary care or services and not having personalized plans developed to address their specific needs.The Findings include: Record review of Resident #2's admission record dated , revealed a [AGE] year-old male with an admission date of 07/06/2021,with a diagnoses which included Alzheimer's Disease (a progressive disease that destroys memory and other important mental functions), dementia (a group of thinking and social symptoms that interferes with daily functioning) without behavioral disturbance, psychotic disturbance (delusions and hallucinations), mood disturbance, and anxiety. Record review of Resident #3's quarterly MDS assessment dated [DATE] reflected a blank BIMS score, which indicated a severe cognitive impairment. There were no potential indicators of psychosis, verbal behavioral symptoms occurred 1 - 3 days, and other behavioral symptoms not directed toward others (e.g., physical symptoms such as hitting or scratching self, pacing, rummaging, public sexual acts, disrobing in public, throwing, or smearing food or bodily waste, or verbal/vocal symptoms like screaming, disruptive sounds) occurred 1 - 3 days. Record review of Resident #2's quarterly care plan dated 06/13/2025 reflected the following: Problem: Resident #2 has a behavior problem r/t vascular dementia, mood disorder, delusional disorder:RP refuses psychiatric services. Only wants primary MD (Medical Doctor) to follow up with behaviors (no date); Resident #2 noted eating crayons during activity time. Apt to put activity objects in mouth (no date),Goal: Resident #8 will have fewer episodes by review date (date initiated 07/09/2021, revision on 12/26/2024, target date 09/16/2025).Interventions: no interventions noted for Resident #2's behavior of eating crayons. During an observation on 07/11/2025 at 10:07 p.m., Resident #2 was observed pacing back and forth down the memory unit's hall. His steps were balanced and steady. He was not interviewable. In an interview on 07/11/2025 at 10:15 p.m., CNA KK said she had worked with Resident #2 for over 2 years. She said Resident #2 kept to himself and walked repeatedly down the memory unit hall. She said at times he had been physically combative with staff and other residents. She said there had been times in which he had refused care but was easily redirected. She said Resident #2 liked to put small objects in his mouth and/or lick them. CNA KK said staff in the memory unit know Resident #2's behavior of trying to take small objects from them so as soon as they see Resident #2 approach them, they will hide those small objects and redirect him. In an interview on 07/11/2025 at 1:45 p.m., the MDS D said it was her responsibility to ensure a resident's MDS, and care plan were accurate and updated. She said if a resident had a problem related to behaviors and continued with the same behavior(s) at the next assessment, she would not update it. She said if the resident displayed a new behavior problem(s), she would simply add to the existing problem (behavior) listed on their previous care plan assessment. MDS D said her office was housed in the memory unit and for the most part would spend her time out in the memory unit's hall while she worked. She said this allowed her to become familiar with the residents. MDS D said Resident #2's behavior problems included, banging on doors, wandered into other residents' rooms and went through their closet/drawers, took small objects they had, and being aggressive with staff and other residents. She said Resident #2's behavior problems were a weekly occurrence and needed constant redirection. She said she remembered a time when the Activity Aide mentioned to her look [Resident #2] tried to eat crayons while he participated in an activity. She said she immediately cared for his behavior but forgot to include an initiation date for that behavior. She said she had also failed to include intervention(s) for that behavior. MDS D said in hindsight, she should have not been so specific but rather entered a general statement that read, Resident #2 likes to put small objects in his mouth and/or lick them. She said an interventionshe could have entered was to keep small objects away from his reach and to redirect him. The MDS D said there were no negative outcomes to Resident #2 for not having any interventions in place for his behavior of eating crayons. She said the staff that worked in the memory unit were aware of his behavior and would keep a close eye on him and knew not to give him any small objects.In an interview on 07/15/2025 at 10:15 a.m., the Activity Aide said she was housed in the memory unit Monday through Friday from 9:00 a.m. to 4:00 p.m. and her partner would work the same hours on the weekends. She said Resident #2 participated in activities but would not stay the entire time as he preferred walking back and forth down the hall. She said she was aware Resident #2 had behavior problems and recalled a time in which he tried to put crayons in his mouth. She said she could not give a date when that happened. She said she had informed MDS D because she was in the unit. She said she was pretty sure they told the Charge Nurse but did not remember. The Activity Aide said she knows not to give or leave any small objects accessible to Resident #2 because he liked to place them in his mouth. She said whenever he is participating, she would use a beach ball or music activities. In an interview on 07/15/2025 at 11:36 a.m., the DON said the facility's MDS nurse was responsible for ensuring residents' care plans were accurate and updated. He said a resident's behaviors should be care planned, and interventions set in place to prevent future occurrences. The DON said there were no negative outcomes to Resident #2 not having any interventions for his behavior (eating crayons) because staff in the memory unit knew his behaviors and there were always plenty of staff to redirect him. Record review of the facility's Comprehensive Care Policy dated 10/24/2022 reflected the following:Policy:It is a policy of this facility to develop and implement A comprehensive person-centered care plan for each resident, consistent with a resident right, that includes measurable objectives and time frames to lead in residence medical, nursing, and mental and psychosocial needs that are identified in the residence comprehensive assessment. Policy Explanation and Compliance Guidelines:The care planning the process will include an assessment of the residents' strengths and the needs and will be and will incorporate the president's personal and cultural preferences and developing goals of care period services provided or arranged by the facility, as outlined by the comprehensive care, shall be culturally competent and trauma informed.The comprehensive care plan will describe, at a minimum, the following:a. The services that are to be furnished to attain or maintain the resident's highest practicable physical, mental, and psychosocial well-being.5.The comprehensive care plan will be reviewed and revised by the interdisciplinary team after each comprehensive and quarterly MDS assessment.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0657
(Tag F0657)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record reviews, the facility failed to review and revise comprehensive care plans for 4 res...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interviews and record reviews, the facility failed to review and revise comprehensive care plans for 4 residents (Residents, #1, #2, #7, and #6) of 10 residents reviewed comprehensive care plan revisions. 1.The facility failed to review and revise Resident #1's comprehensive person-centered care plan from Full Code Status to DNR Status when ordered DNR was dated [DATE]. 2.The facility failed to review and revise Resident #7's comprehensive person-centered care plan when he had a resident-to-resident altercation with Resident #6 when she grabbed his left forearm and pierced skin with her fingernails which caused multiple skin tears on [DATE] at 5:30 p.m., 3. The facility failed to review and revise Resident #2's comprehensive person-centered care plan when he had a resident-to-resident altercation with Resident #7 when he striked her on the face with a closed hand on [DATE] at 3:00 p.m. 4.The facility failed to review and revise Resident #6's comprehensive person-centered care plan when he had a resident-to-resident altercation with: Resident #9 when he striked her left upper arm with a closed hand on [DATE] at 2:30 p.m. Resident #10 when he pushed his wheelchair toward her left knee which caused a skin tear on [DATE] at 3:15 p.m. Resident #7 when he grabbed her by the hair and her arm on [DATE] at 12:25 p.m. These failures could affect residents and place them at risk of not receiving appropriate interventions to meet their current needs. The findings included:: 1.Record review of Resident #1's admission record dated [DATE] revealed he was a [AGE] year-old male with an admission date of [DATE]. Diagnoses included dementia (the loss of cognitive functioning - thinking, remembering, and reasoning - to such an extent that it interferes with a person's daily life and activities), and osteoarthritis (a degenerative joint disease, in which the tissues in the joint break down over time). Record review of Resident #1's Care Plan dated [DATE] revealed the following:FOCUS: RESOLVED: Resident #1 is a full code Date Initiated: [DATE] Revision on: [DATE] Resolved Date: [DATE]GOALS: RESOLVED: Facility will comply with resident/family wishes Date Initiated: [DATE] Revision on: [DATE] Target Date: [DATE] Resolved Date: [DATE] INTERVENTIONS/TASKS: RESOLVED: If a resident has a cardiac arrest, initiate CPR and call 911. Notify MD/RP and follow MD orders after notification. Date Initiated: [DATE] Revision on: [DATE] Resolved Date: [DATE] LN [DATE] o RESOLVED: Keep emergency cart well supplied and ready for use at all times Date Initiated: [DATE] Revision on: [DATE] Resolved Date: [DATE] LN [DATE] o RESOLVED: [NAME] chart and all pertinent documents with FULL CODE Date Initiated: [DATE] Revision on: [DATE] Resolved Date: [DATE] LN SS [DATE]. FOCUS: CANCELLED: Resident #1 is a DNR Date Initiated: [DATE] Revision on: [DATE] Cancelled Date: [DATE]GOALS: CANCELLED: Facility will comply with resident/family wishes Date Initiated: [DATE] Revision on: [DATE] Target Date: [DATE] Cancelled Date: [DATE]INTERVENTIONS/TASKS: CANCELLED: Ensure signed DNR is in medical record Date Initiated: [DATE] Revision on: [DATE] Cancelled Date: [DATE] LN SS [DATE] CANCELLED: If resident has a cardiac arrest, do not call 911 or initiate CPR. Notify MD/RP and follow instructions after notification Date Initiated: [DATE] Revision on: [DATE] Cancelled Date: [DATE] LN [DATE] CANCELLED: Keep resident as comfortable as possible at all times Date Initiated: [DATE] Revision on: [DATE] Cancelled Date: [DATE] LN [DATE] o CANCELLED: [NAME] chart and all pertinent documents with DNR status Date Initiated: [DATE] Revision on: [DATE] Cancelled Date: [DATE] LN [DATE] CANCELLED: Send copy of DNR paperwork upon transfer from facility Date Initiated: [DATE] Revision on: [DATE] Cancelled Date: [DATE] LN [DATE] CANCELLED: Social services consult if resident/family want to change code status Date Initiated: [DATE] Revision on: [DATE] Cancelled Date: [DATE] SS [DATE].Record review of Resident #1's Facility Internal Patient Self-Determination Checklist Texas dated [DATE] revealed the Full Code status box checked. Record review of Resident #1's OOH-DNR signed by RP and witnesses on [DATE] and the physician signed on [DATE]. Record review of Resident #1's Physician's Order for DNR dated [DATE]. In an interview on [DATE] at 06:42 PM, the Administrator stated Resident #1 was a full code when he first came in, but the RP signed the DNR after he had been admitted . The nurses can see the code status on their computers on the first page. It would have been updated when his code status changed. 2. Record review of Resident #2's admission record dated , revealed a [AGE] year-old male with an admission date of [DATE],with a diagnoses which included Alzheimer's Disease (a progressive disease that destroys memory and other important mental functions), dementia (a group of thinking and social symptoms that interferes with daily functioning) without behavioral disturbance, psychotic disturbance (delusions and hallucinations), mood disturbance, and anxiety. Record review of Resident #2's quarterly MDS assessment dated [DATE] reflected his BIMS score was left blank, which indicated his cognition was severely impaired. Further review indicated no behavioral symptoms. Record review of the facility's incident by incident report from [DATE] to [DATE] reflected:Resident #2 had a resident-to-resident altercation with Resident # 7 on [DATE] at 3:00 p.m. Record review of Resident #2's quarterly care plan dated [DATE] reflected a problem the resident has a behavior problem related to vascular dementia, mood disorder, delusional disorder. Resident #2's resident-to-resident altercation with Resident #7 on [DATE] had not been care planned and no interventions were set in place. 3.Record review of Resident #6's admission record dated [DATE] reflected a [AGE] year-old-male with an admission date of [DATE]. His relevant diagnoses included Alzheimer's disease (a progressive disease that destroys memory and other important mental functions), dementia (a group of thinking and social symptoms that interferes with daily functioning), unspecified mood (affective) disorder (a serious mental illness that causes persistent and intense changes in a person's mood, energy, and behavior) , and cognitive communication deficit ( difficulties in communication that arise from impairments in cognitive processes like attention, memory, problem-solving, and executive functions). Record review of Resident #6's quarterly assessment dated [DATE] reflected a BIMS score of 06, which indicated his cognition was severely impaired. Further review reflected Resident #6 had behavioral problems with physical behavioral symptoms directed towards others (e.g., hitting kicking, pushing, scratching, grabbing, abusing others sexually) that occurred 1 to 3 days. Verbal behavioral symptoms directed towards others (e.g., threatening others, screaming at others, cursing at others) that occurred 4 to 6 days, but less than daily. Record review of the facility's incident by incident report from [DATE] to [DATE] reflected: Resident #6 had a resident-to-resident altercation with Resident #9 on [DATE] at 2:30 p.m. Resident #6 had a resident-to-resident altercation with Resident #8 on [DATE] at 3:15 p.m. Resident #6 had a resident-to-resident altercation with Resident #7 on [DATE] at 12:25 p.m. Record review of Resident #6's quarterly care plan dated [DATE] reflected:Problem: [Resident #6] gets physically/verbally aggressive in activities at times and isn't easily redirected (date initiated/revised on [DATE]). Further review of Resident #6's care plan reflected his resident-to-resident altercations he had with Residents #7, #9, and #10 had not been care planned and no interventions were set in place. In an interview and observation on [DATE] at 4:49 p.m., MDS D said it was her responsibility to ensure a resident' care plan was accurate and updated. She said Resident #7, #2, and #6 all had behavior problems related to being physically and verbally aggressive towards staff and other residents. She said all resident-to-resident altercations needed to be care planned and some type of intervention set in place. The MDS D was observed as she reviewed Resident #7, #2, and #6's care plans on their electronic medical record and said the resident-to-resident altercations Residents #7, #2, and #6 had not been care planned. She said there were no negative outcomes for either resident for not having interventions in place as their behavior of being aggressive had been care planned and they were being monitored closely by staff in case they needed to be redirected. In an interview on [DATE] at 11:36 a.m., the DON who said it was facility's MDS nurse responsibility to a residents' care plan were accurate and updated. He said a resident's behaviors should be care planned, and interventions set in place to prevent future occurrences. The DON said all resident-to-resident altercations should be care planned for the resident who was the aggressor. The DON said Resident #7, #2, and #6's had no negative outcomes due to their resident-to-resident altercations not care planned. He said all three residents' behaviors of being physically and verbally aggressive towards staff and other residents had been care planned and staff kept a close eye on them in case they needed to be redirected. Record review of facility's policy Communication of Code Status dated [DATE] revealed:Policy:It is the policy of this facility to adhere to residents' rights to formulate advance directives. In accordance to these rights, this facility will implement procedures to communicate a resident's code status to those individuals who need to know this information. Policy Explanation and Compliance Guidelines:2.When an order is written pertaining to a resident's presence or absence of an Advance Directive, the directions will be clearly documented in the physician orders section of the medical record. Examples of directions to be documented include, but are not limited to: a. Full Code b. Do Not Resuscitate3.The nurse who notates the physician order is responsible for documenting the directions in all relevant sections of the medical record. Record review of facility's policy Baseline Care Plan dated [DATE] revealed:Policy:The facility will develop and implement a baseline care plan for each resident that includes the instructions needed to provide effective and person-centered care of the resident that meets professional standards of quality care.Policy Explanation and Compliance Guidelines:1.The baseline care plan will: a. Be developed within 48 hours of a resident's admission. b. Include the minimum healthcare information necessary to properly care for a resident including, but not limited to: i. Initial goals based on admission orders. ii. Physician orders. iii. Dietary orders. iv. Therapy services. v. social services. vi. PASARR recommendation, if applicable. Record review of facility's policy Comprehensive Care Plans dated [DATE] revealed:Policy: It is the policy of this facility to develop and implement a comprehensive person-centered care plan for each resident, consistent with resident rights, that includes measurable objectives and timeframes to meet a resident's medical, nursing, and mental and psychosocial needs that are identified in the resident's comprehensive assessment.Policy Explanation and Compliance Guidelines:8.Qualified staff responsible for carrying out interventions specified in the care plan will be notified of their roles and responsibilities for carrying out the interventions, initially and when changes are made.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0692
(Tag F0692)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents received therapeutic diets that were...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview, and record review, the facility failed to ensure residents received therapeutic diets that were prescribed by the attending physician for 1 of 4 residents (Resident #8) reviewed for therapeutic diets.The facility failed to ensure Resident #8 received a house shake on 07/14/2025 with his breakfast tray as ordered by his physician with orders dated 07/11/2025 for a house shake with meals for malnutrition and a revised order effective 07/14/2025 for a house shake with meals for supplement.This failure could place residents at risk for poor intake, weight loss, unmet nutritional needs, and a loss of dignity.Findings Included:Record review of Resident #8's admission sheet dated 07/14/2025, reflected a [AGE] year-old male with an admission date of 01/14/2020, with a diagnoses which included vascular dementia (brain damage caused by multiple strokes), cognitive communication deficit (deficits in communication skills resulting from cognitive impairments like attention, memory, problem-solving, and sequencing), need for assistance with personal care, and age-related physical debility (decline in physical function and strength that commonly occurs with aging).Record review of Resident #8's quarterly MDS assessment dated [DATE] reflected a BIMS score of 04, which indicated his cognition was severely impaired.Record review of Resident #8's quarterly care plan dated 06/12/2025 reflected a nutritional problem related to current diet: regular diet, mechanical soft texture, regular liquids consistency, add fortified foods with all meals (date initiated 01/28/2020 and revised on 02/26/2024). His goal was to maintain adequate nutritional status as evidenced by maintaining weight through review date (date initiated 01/28/2020 and revised on 01/20/2025). Resident #8's interventions in part included, provide, and serve supplements as ordered: Med Plus 2.0 (date initiated/revised 07/10/2025).Record review on 07/15/2025 of Resident #8's weight history reflected07/04/2025 146.6 lbs.07/05/2025 136.0 lbs.06/05/2025 136.0 lbs.05/03/2025 144.2 lbs.Record review of Resident #8's order summary dated 07/15/2025 reflected an active order effective 07/11/2025 for a house shake with meals for malnutrition and a revised order effective 07/15/2025 for a house shake with meals for supplement.During an observation on 07/15/2025 at 10:25 a.m., this Surveyor, while observing residents in the memory unit, noticed a meal tray on the dining room counter. As per the meal ticket on the meal tray, it belonged to resident #8. The food and drinks on the tray seemed untouched. His meal ticket dated 07/15/2025, breakfast reflected the following:Texture: mech softSpecial diets: regular diet, fluids-thinNotes: milk of choice- 8 oz, juice of choice- 4 oz, water-8 oz. (ounces)Standing orders: fortified foodIn an interview on 07/15/20/2025 at 10:30 a.m., CNA KK said Resident #8 had refused his breakfast and she had placed it on the dining room counter in case he requests it later.In an interview on 07/15/2025 at 10:35 a.m., the DM said she was responsible for ensuring all residents' meals were served according to their physician's orders. She said each resident had a meal ticket which indicated their diet, texture, allergies, dislikes, and any standing order(s). She said she would print the meal tickets on a daily basis, and that was how the dietary aides would know what to serve each resident. The DM said there were several ways in which she would know if a resident received a new dietary order for a house shake. She said one way would be for the nursing staff that received the order to complete a dietary slip which indicated the new order and given to her. Another way would be if the nursing staff noticed the house shake was not included in the resident's meal tray, they would let her know, and the last way was when she did her weekly thorough checks on any new orders for that week. The DM said if the resident's meal ticket did not indicate a house shake, the dietary aides would not place one on their tray. The DM said the facility had been out of house shakes for about a month. She said they were substituting the house shakes with fortified milk. The DM said the way the dietary aides would identify a fortified milk glass from a regular milk glass was they would write an F on the fortified milk covers. The DM was observed as she inspected Resident #8's breakfast tray. She said, unfortunately the milk does not have an F therefore he was served regular milk and Resident #8's milk ticket did not indicate house shake. She said she was not given a dietary slip from the nurse that reflected Resident #8's order for a house shake.In an interview on 07/15/2025 at 11:00 a.m., LVN F said he had notified Resident #8's NP that on 07/11/2025, he had refused his breakfast and only eaten 30 % of his lunch. He said the NP gave an order for a house shake with each meal. LVN F said he did not remember if he had completed a dietary slip for Resident #8's house shake order nor did her remember if he had notified the DM. LVN F said he had corrected Resident #8's order on 07/15/2025 to reflect house shake for supplement. He said on 07/11/2025, he had indicated the house shake for malnutrition, and Resident #8 was not malnourished. LVN F said he was not aware the facility was out of house shakes. He said if a resident had an order for a house to shake, the Charge Nurse would have to sign off on it. He said since the facility was out of house shakes, they would still sign off on it but enter a code 9 which indicated other/see progress notes.In an interview on 07/15/2025 at 11:15 a.m., Resident #8 refused to be weighed. He said he had already weighed himself.Record review on 07/15/2025 at 11:25 a.m., of facility's purchase order from 06/16/2025 to 07/14/2025 reflected house shakes (strawberry, vanilla, chocolate) were out of stock.In an interview on 07/15/2025 at 11:36 a.m., the DON said on 07/11/2025, Resident #8's NP ordered a house shake with each meal because on same day he had refused breakfast. The DON said he was not aware the facility was out of house shakes. He said he had known the facility was out of house shakes, he would have updated Resident #8's order to reflect fortified milk. He said he would be calling the facility's Dietician to verify if the fortified milk the residents were being given equated the same nutrients as a house shake before he was able to say if Resident #8 had any negative effects due been given fortified milk instead of a house shake. This surveyor requested the facility's physician's orders policy but was given physician visits and physician delegation instead. The DON said that was the only policy related to following physician orders they had.Record review on 07/15/2025 of the facility's Supplement Conversion Table (undated) reflected:House shake conversion:House shake-1 carton converted to 8 oz. (ounces of fortified milk.In an interview on 07/15/2025 at 11:47 a.m., the Administrator said he had not been informed the facility was out of house shakes but knew the house shakes had been replaced with fortified milk. He said ideally, best practice the environment. He should have been informed the facility was out of house shakes. He said the management team, which included DM, met twice a day (9:00 am and 4:00 pm) and that is where they discuss any issues/concerns of the day. The Administrator said, we need to get better with communication and if there's an issue, we need to find out the root cause. The Administrator said there were no negative outcomes to Resident #8 for not being served a house shake because it was substituted with fortified milk.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Pharmacy Services
(Tag F0755)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the accurate acquiring, receiving, dispensing, ...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observation, interview and record review, the facility failed to ensure the accurate acquiring, receiving, dispensing, and administering of all drugs and biologicals to meet the needs of each resident for 1 (Resident #3) of 5 residents reviewed for pharmacy services.
The facility failed to verify there was a physician's order for Haldol (an antipsychotic) and to ensure the order had an indication of its use.
This failure could place residents at risk for receiving an antipsychotic medication without a physician's order or an indication for use resulting in a resident receiving a medication which could cause a decline in health status.
The findings included:
Record review of Resident #3's admission record dated 06/17/2025, revealed an admission date of 08/15/2024, and a re-admission date on 11/25/2024, with a diagnoses which included dementia (a group of thinking and social symptoms that interferes with daily functioning) without behavioral disturbance, psychotic disturbance (delusions and hallucinations), mood disturbance, and anxiety, and traumatic subdural hemorrhage (a type of bleeding near the brain that can happen after a head injury) with loss of consciousness of 30 minutes or less.
Record review of Resident #3's admission MDS, dated [DATE], revealed a BIMS of 01, indicating severe cognitive impairment. There were no potential indicators of psychosis, and no behavioral symptoms were indicated. Active diagnoses included: traumatic brain dysfunction (an impairment in the normal functioning of the brain caused by an outside force, usually a violent blow to the head), and dementia. Resident #3 was not receiving an antipsychotic.
Record review of Resident #3's Progress Note written by LVN J, dated 10/28/2024 at 11:18 AM revealed, As per NP (NP S), new order for Haldol Decanoate 50mg IM Q month for aggression behavior.
Record review of Resident #3's Progress Note on 10/28/2024 at 11:19 AM written by LVN J revealed, Orders - Administration Note: This order is outside of the recommended dose or frequency. Haldol Decanoate Intramuscular Solution 50 MG/ML (Haloperidol Decanoate) Inject 50 mg intramuscularly one time a day every 1 month(s) starting on the 28th for 1 day(s) for 50mg IM Q month - The frequency of monthly is below the usual frequency of every 28 days. No indication for use on the physician's order.
Record review of Resident #3's Progress Note dated 10/29/2024 at 08:18 PM written by LVN K, revealed Administered monthly haloperidol.
Record review of Resident #3's October 2024 MAR revealed there was no physician's order for Haldol Decanoate Intramuscular Solution 50 MG/ML (Haloperidol Decanoate) Inject 50 mg intramuscularly one time a day every 1 month(s) starting on the 28th for 1 day(s) for 50mg IM Q month - The frequency of monthly is below the usual frequency of every 28 days, nor was there an indication for use on the order.
Record review of resident #3's care plan, dated 11/19/2024, revealed:
FOCUS: o The resident uses antipsychotic medications (HALDOL) r/t AGITATION Date Initiated: 11/19/2024 Revision on: 11/19/2024.
GOALS: o Resident will have no injuries related to medication usage Date Initiated: 11/19/2024 Target Date: 12/31/2024.
INTERVENTIONS/TASKS: o psych consult Date Initiated: 11/19/2024 Revision on: 11/19/2024 LN o Discuss side effects of medications with resident/RP Date Initiated: 11/19/2024 LN o Keep environment free of clutter and safety hazards Date Initiated: 11/19/2024 LN o Monitor behaviors. Notify MD of new or worsening behaviors Date Initiated: 11/19/2024 LN SS o Monitor vital signs as ordered by MD and PRN Date Initiated: 11/19/2024 LN o Monitor/document/report PRN any adverse reactions of antipsychotic medications: unsteady gait, tardive dyskinesia, EPS (shuffling gait, rigid muscles, shaking), frequent falls, refusal to eat, difficulty swallowing, dry mouth, depression, suicidal ideations, social isolation, blurred vision, diarrhea, fatigue, insomnia, loss of appetite, weight loss, muscle cramps nausea, vomiting, behavior symptoms not usual to the person. Date Initiated: 11/19/2024 LN.
During an interview on 06/26/2025 at 10:25 AM PA N stated when she talked with MD O about Resident #3 and the Haldol order, MD O said he was not familiar with the Haldol order for Resident #3, and he would not have ordered Haldol to him. PA N stated NP S (the one who ordered Haldol for Resident #3, was no longer working at the doctor's office).
During an interview on 06/26/2025 at 01:14 PM LVN P stated for an antipsychotic to be given to a resident, the LVN needed to make sure she had a consent form, the correct diagnosis, the right reason, the right time, the right route, the right patient, and the right documentation. She stated if all those were not checked, a medication error could happen.
During an interview on 06/26/2025 at 01:48 PM LVN K stated he could not recall if he had administered the Haldol injection to Resident #3 on 10/29/2024 or not. He stated he had just started working as a nurse and at the facility (October 2024). LVN K stated Resident #3 did not have behaviors.
In an interview on 06/26/25 at 05:33 PM, the DON stated all orders must be complete. If the orders were not complete, they needed to be fixed by confirming with the doctor. The DON stated he had seen Resident #3's Haldol order had been given by NP S to LVN J on 10/28/2024, (LVN J no longer worked at the facility), and LVN K had written in the Progress Notes he had administered the Haldol on 10/29/2024 although the order was not on the MAR so it could not be checked off on the MAR. The DON stated the order should be checked by the nurse before the Haldol was administered.
A review of the facility's policy Medication Administration dated 10/24/2022 revealed the following:
Policy Explanation and Compliance Guidelines:
10. Review MAR to identify medication to be administered.
11. Compare medication source (bubble pack, vial, etc.) with MAR to verify resident name, medication name, form, dose, route, and time.
17. Sign MAR after administered.
18. If medication is a controlled substance, sign narcotic book.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Drug Regimen Review
(Tag F0756)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure any drug regimen irregularities reported by the Pharmacist C...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on record review and interview, the facility failed to ensure any drug regimen irregularities reported by the Pharmacist Consultant were acted upon, for 1 (Resident #3) of 5 residents whose medications were reviewed.
The facility failed to act on the facility's Pharmacy Consultant recommendations for Resident #3 ' s Haldol order for 1. An approved psychiatric diagnosis and 2. To have an informed consent on file.
This failure could place residents receiving antipsychotic medications at risk for adverse consequences and could cause a decline in their physical, mental, and psychosocial condition.
The findings were:
Record review of Resident #3's admission record dated 06/17/2025, revealed an admission date of 08/15/2024, and a re-admission date on 11/25/2024, with a diagnoses which included dementia (a group of thinking and social symptoms that interferes with daily functioning) without behavioral disturbance, psychotic disturbance (delusions and hallucinations), mood disturbance, and anxiety, and traumatic subdural hemorrhage (a type of bleeding near the brain that can happen after a head injury) with loss of consciousness of 30 minutes or less.
Record review of Resident #3's admission MDS, dated [DATE], revealed a BIMS of 01, indicating severe cognitive impairment. There were no potential indicators of psychosis, and no behavioral symptoms were indicated. Active diagnoses included: traumatic brain dysfunction (an impairment in the normal functioning of the brain caused by an outside force, usually a violent blow to the head), and dementia. Resident #3 was not receiving an antipsychotic.
Record review of the Pharmacy Consultant letter titled All Recommendations dated between 01/25/2025 and 02/27/2025 for Resident #3 revealed:
Recommendations By Routing:
Nursing
Please ensure approved psych diagnosis has been documented to support continued use.
Record review of the Pharmacy Consultant letter titled All Recommendations dated between 01/29/2025 and 01/30/2025 for Resident #3 revealed:
Recommendations By Routing:
Nursing
An informed consent was not found in resident medical record for:
Haldol – requires standardized antipsychotic consent form.
Record review on 06/17/2025 of Resident #3's medical record did not reveal a consent for the antipsychotic Haldol (ordered 10/28/2024) until 02/22/2025.
Record review on 06/17/2025 of Resident #3 ' s medical record revealed there had been no evaluations completed for the administration of Haldol (an antipsychotic) from 10/28/2024 through 06/17/2025.
In an interview on 06/25/2025 at 03:38 PM Resident #3's RP stated she had gone to the facility sometime around February to sign a consent for a medication they wanted to give Resident #3. She said they told her it was for sleep because he woke up in the night and because he walked around.
In an interview on 06/26/25 at 10:25 AM PA N stated she was the one who discontinued Resident #3 ' s Haldol order on 06/19/2025. She said she spoke to MD O about the Haldol order for Resident #3, and they wanted Resident #3 to evaluated by psychiatric services. PA N stated she did not see on the notes where Resident #3 had been evaluated. PA N stated before giving Haldol a resident would have to be evaluated by psych first.
In an interview on 06/26/2025 at 01:14 PM LVN P stated for an antipsychotic to be given to a resident, the LVN needed to make sure she had a consent form (signed), the correct diagnosis, the right reason, the right time, the right route, the right patient, and the right documentation.
In an interview on 06/26/25 at 02:16 PM LVN Q stated she called PA N (on 06/18/2025) to have Resident #3 ' s Haldol discontinued on 06/19/2025 due to checking the chart with resident had no behaviors and no evaluation. LVN Q stated she received an order for psychiatric services to come evaluate Resident #3.
In an interview on 06/26/25 at 05:33 PM the DON stated, to administer an antipsychotic, an evaluation needed to be done, and a consent must be signed prior to giving the antipsychotic. The DON stated he had seen the consent for the Haldol for Resident #3 had been signed in February 2025 and the order had been given by NP S to LVN J on 10/28/2024, (LVN J no longer worked at the facility). The DON stated the consent should have been signed by the RP.
Record review of facility ' s policy General Policy & Procedures, Subsection: Consultant Pharmacist Service Requirements dated 10/01/2019, revealed:
Procedure
B. Communicating to the responsible prescriber and the facility leadership potential or actual problems detected and other findings relating to medication therapy orders as well as recommendations for changes in medication therapy and monitoring of medication therapy at least monthly.
7.A. A written or electronic report of findings and recommendations resulting from the activities as described above is given to the administrator and/or director of nursing at least monthly.
Record review of facility's policy Use of Psychotropic Medication(s) dated 03/05/1025 revealed:
Policy:
It is the intent of this policy to ensure that residents only receive psychotropic medications when other nonpharmacological interventions are clinically contraindicated.
Policy Explanation and Compliance Guidelines:
5.The indications for initiating, maintaining, or discontinuing medication(s), as well as the use of nonpharmacological approaches, will be determined by evaluating the resident ' s physical, behavioral, mental, and psychosocial signs and symptoms in order to identify and rule out any underlying medical conditions, including the assessment of relative benefits and risks, and the preferences and goals for treatment.
7. The resident ' s medical record shall include documentation of this evaluation and the rationale for chosen treatment options.
13.Residents who receive an antipsychotic medication will have an Abnormal Involuntary Movement Scale (AIMS) test performed on admission, every six months, with a significant change in condition, change in antipsychotic medication, PRN or as per facility policy.
Record review of the facility's policy Nursing Facility Residents' Rights, dated November 2021, revealed,
Participation in Your Care
You have the right to:
-Have any psychoactive medications prescribed and administered in a responsible manner as mandated by the Texas Health and Safety Code, 242.505, and to refuse to consent to the prescription of psychoactive medications.
CONCERN
(D)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Deficiency F0757
(Tag F0757)
Could have caused harm · This affected 1 resident
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure each resident's drug regimen was free of unnecessary drugs f...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on interview and record review, the facility failed to ensure each resident's drug regimen was free of unnecessary drugs for 1 (Resident #3) of 5 residents reviewed for medications.
The facility failed to have an adequate indication for the use of the medication Haldol (an antipsychotic) for Resident #3 before administering the medication with a black box warning.
This failure could put residents at risk of harm from adverse reactions or harmful side effects.
The findings included:
Record review of Resident #3's admission record dated 06/17/2025, revealed an admission date of 08/15/2024, and a re-admission date on 11/25/2024, with a diagnoses which included dementia (a group of thinking and social symptoms that interferes with daily functioning) without behavioral disturbance, psychotic disturbance (delusions and hallucinations), mood disturbance, and anxiety, and traumatic subdural hemorrhage (a type of bleeding near the brain that can happen after a head injury) with loss of consciousness of 30 minutes or less.
Record review of Resident #3's admission MDS, dated [DATE], revealed a BIMS of 01, indicating severe cognitive impairment. There were no potential indicators of psychosis, and no behavioral symptoms were indicated. Active diagnoses included: traumatic brain dysfunction (an impairment in the normal functioning of the brain caused by an outside force, usually a violent blow to the head), and dementia. Resident #3 was not receiving an antipsychotic.
Record review of Resident #3's Progress Note written by LVN J, dated 10/28/2024 at 11:18 AM revealed, As per NP (S), new order for Haldol Deconate 50mg IM Q month for aggression behavior.
Record review of Resident #3's Progress Note Orders - Administration Note on 10/28/2024 written by LVN J revealed This order is outside of the recommended dose or frequency. Haldol Decanoate Intramuscular Solution 50 MG/ML (Haloperidol Decanoate) Inject 50 mg intramuscularly one time a day every 1 month(s) starting on the 28th for 1 day(s) for 50mg IM Q month - The frequency of monthly is below the usual frequency of every 28 days.
Record review of Resident #3's October 2024 MAR revealed no order for Haldol Decanoate Intramuscular Solution 50 MG/ML (Haloperidol Decanoate) Inject 50 mg intramuscularly one time a day every 1 month(s) starting on the 28th for 1 day(s) for 50mg IM Q month - The frequency of monthly is below the usual frequency of every 28 days.
Record review of Resident #3's Progress Note dated 10/29/2024 at 08:18 PM written by LVN K, revealed Administered monthly haloperidol.
Record review of Resident #3's Order Summary dated 11/01/2024 revealed an order for Haldol Decanoate Intramuscular Solution 50 MG/ML (Haloperidol Decanoate) Inject 50 mg intramuscularly one time a day every 1 month(s) starting on the 28th for 1 day(s) for 50mg IM Q month - The frequency of monthly is below the usual frequency of every 28 days with an order date of 10/28/2024 and a start date of 12/15/2024.
Record review of resident #3's care plan, dated 11/19/2024, revealed:
FOCUS: o The resident uses antipsychotic medications (HALDOL) r/t AGITATION Date Initiated: 11/19/2024 Revision on: 11/19/2024.
GOALS: o Resident will have no injuries related to medication usage Date Initiated: 11/19/2024 Target Date: 12/31/2024.
INTERVENTIONS/TASKS: o psych consult Date Initiated: 11/19/2024 Revision on: 11/19/2024 LN o Discuss side effects of medications with resident/RP Date Initiated: 11/19/2024 LN o Keep environment free of clutter and safety hazards Date Initiated: 11/19/2024 LN o Monitor behaviors. Notify MD of new or worsening behaviors Date Initiated: 11/19/2024 LN SS o Monitor vital signs as ordered by MD and PRN Date Initiated: 11/19/2024 LN o Monitor/document/report PRN any adverse reactions of antipsychotic medications: unsteady gait, tardive dyskinesia, EPS (shuffling gait, rigid muscles, shaking), frequent falls, refusal to eat, difficulty swallowing, dry mouth, depression, suicidal ideations, social isolation, blurred vision, diarrhea, fatigue, insomnia, loss of appetite, weight loss, muscle cramps nausea, vomiting, behavior symptoms not usual to the person. Date Initiated: 11/19/2024 LN.
Record review of Resident #3's December 2024 MAR revealed an order for Haldol Decanoate Intramuscular Solution 50 MG/ML (Haloperidol Decanoate) Inject 50 mg intramuscularly one time a day every 1 month(s) starting on the 28th for 1 day(s) for 50mg IM Q month and checked off as administered on 12/19/2024.
Record review of Resident #3's physician's orders revealed no indication for use for the antipsychotic Haldol from 10/28/2024 through 06/18/2025.
Record review of Resident #3's physician's order for Haldol dated 11/25/2024 written by MD O revealed a black box warning Increased mortality of elderly patients with dementia-related psychosis. Haloperidol is not approved for the treatment of dementia-related psychosis.
During an interview on 06/25/25 at 02:25 PM CNA R stated when he first met Resident #3, he was walking and walking. CNA R stated now, Resident #3 was very calm. CNA R stated he did not know what happened to make Resident #3 calm.
During an interview on 06/25/2025 at 03:38 PM Resident #3's RP stated she had gone to the facility sometime around February to sign a consent for a medication they wanted to give Resident #3. She said they told her it was for sleep because he woke up in the night and because he walked around.
During an interview on 06/26/2025 at 10:25 AM PA N stated she discontinued the order for Haldol on 06/19/2025 for Resident #3. She said she had spoken to MD O about it, and they decided they wanted Resident #3 to be evaluated by psych. PA N stated she had not seen in the notes where Resident #3 had been evaluated. PA O stated when she talked with MD O about Resident #3 and the Haldol order, MD O said he was not familiar with the Haldol order for Resident #3, and he would not have ordered Haldol to him. PA N stated NP S (the one who ordered Haldol for Resident #3, was no longer working at the doctor's office).
During an interview on 06/26/25 at 03:40 PM MD O stated he did not know where that order (Resident #3's order for Haldol) came from. He said it did not come from him. He said he would not give Haldol to a nursing home patient, and he definitely would not give it once a month. MD O stated he thought there was probably an error in communication and he thought it was just nonsensical.
During an interview on 06/26/2025 at 01:14 PM LVN P stated for an antipsychotic to be given to a resident, the LVN needed to make sure she had a consent form, the correct diagnosis, the right reason, the right time, the right route, the right patient, and the right documentation.
During an interview on 06/26/2025 at 01:48 PM LVN K stated he could not recall if he had administered the Haldol injection to Resident #3 on 10/29/2024 or not. He stated he had just started working as a nurse, and at the facility (October 2024). LVN K stated Resident #3 did not have behaviors.
In an interview on 06/26/25 at 02:16 AM, LVN Q stated she called PA N to have Resident #3's Haldol order discontinued on 06/19/2025. LVN Q stated she had checked Resident #3's chart, and he had no behaviors. She said the staff were interviewed about behaviors with Resident #3 and none were reported. LVN Q stated she received an order for psych to come evaluate Resident #3.
In an interview on 06/26/25 at 03:40 PM MD O stated he did not know where that order for Haldol came from for Resident #3. He said it had not come from him. He said he would not give Haldol to a nursing home patient, and he definitely would not order for it to be given once a month. MD O stated he thought there was probably an error in communication, and he thought it was just nonsensical.
In an interview on 06/26/25 at 05:33 PM, the DON stated all orders must be complete. If the orders are not complete, they need to be fixed by confirming with the doctor. To administer an antipsychotic, an evaluation needed to be done, and a consent must be signed prior to giving the antipsychotic. The DON stated he had seen the consent for the Haldol for Resident #3 had been signed in February 2025 and the order had been given by NP S to LVN J on 10/28/2024, (LVN J no longer worked at the facility), and LVN K had written in the Progress Notes he had administered the Haldol on 10/29/2024 although the order was not on the MAR so it could not be checked off on the MAR. The DON stated the consent should have been signed by the RP and checked and the order should be checked by the nurse before the Haldol was administered. The DON stated he started working at the facility two months ago.
A record review of the facility's policy Use of Psychotropic Medication(s), dated 03/05/25, revealed,
Policy Explanation and Compliance Guidelines:
9.Prior to initiating or increasing a psychotropic medication, the resident, family, and/or resident representative must be informed of the benefits, risks, and alternatives for the medication, including any black box warnings for antipsychotic medications, in advance of such initiation or increase.
10. The resident has the right to accept or decline the initiation or increase of a psychotropic medication.
11.The facility will document that the resident or resident representative was informed in advance of the risks and benefits of the proposed care, the treatment alternatives or other options and the preferred option to accept or decline in a format the facility deems to use (e.g., written consent form, narrative note, etc.).
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Free from Abuse/Neglect
(Tag F0600)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record review, the facility failed to ensure the residents had the right to be free from a...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record review, the facility failed to ensure the residents had the right to be free from abuse, neglect, and misappropriation of property for 6 of 8 residents (Residents #6, #9, #7, and R#10) reviewed for abuse. 1.The facility failed to ensure Resident #6 was free from abuse when Resident #7 dug her nails on Resident #6's left forearm that resulted with multiple skin tears with serosanguineous drainage on 01/02/2025. 2.The facility failed to ensure Resident #9 was free from abuse when Resident #6 hit Resident 9 on her upper left arm with a closed hand on 03/25/2025.3.The facility failed to ensure Resident #7 was free from abuse when Resident #2 slapped Resident #7 on the left side of the face with a closed hand on 03/25/2025. 4.The facility failed to ensure Resident #7 was free from abuse when Resident #6 grabbed Resident #7 by the hair and arm on 04/11/2025. 5.The facility failed to ensure Resident #10 was free from abuse when Resident #6 rolled his wheelchair towards her and hit her left knee and caused a skin tear on 03/28/2025. The findings included: Resident #6Record review of Resident #6's admission record dated 07/15/2025 reflected a [AGE] year-old-male with an admission date of 09/06/2024. His relevant diagnoses included Alzheimer's disease (a progressive disease that destroys memory and other important mental functions), dementia (a group of thinking and social symptoms that interferes with daily functioning), unspecified mood (affective) disorder (a serious mental illness that causes persistent and intense changes in a person's mood, energy, and behavior) , and cognitive communication deficit ( difficulties in communication that arise from impairments in cognitive processes like attention, memory, problem-solving, and executive functions). Record review of Resident #6's quarterly assessment dated [DATE] reflected a BIMS score of 06, which indicated his cognition was severely impaired. Further review reflected Resident #6 had behavioral problems with physical behavioral symptoms directed towards others (e.g., hitting kicking, pushing, scratching, grabbing, abusing others sexually) that occurred 1 to 3 days. Verbal behavioral symptoms directed towards others (e.g., threatening others, screaming at others, cursing at others) that occurred 4 to 6 days, but less than daily. Record review of Resident #6's quarterly care plan dated 05/12/2025 reflected the following: Problem: [Resident #6] is/has potential to be physically aggressive r/t dementia (date initiated 04/21/2025 and revised on 07/11/2025). Goal: [Resident #6] will not harm self or others through the review date (date initiated 04/21/2025). Interventions: Administer medications as ordered, monitor/document for side effects and effectiveness (date initiated: 04/21/2025), communication, provide physical and verbal cues to alleviate anxiety; give positive feedback, assist verbalization of source of agitation, assist to set goals for more pleasant behavior, encourage seeking out of staff member when agitated (date Initiated 04/21/2025), give the resident as many choices as possible about care and activities (date initiated 04/21/2025), monitor/document/report PRN any s/sx (signs and symptoms) of resident posing danger to self and others (date initiated 04/21/2025) Resident #9Record review on 07/12/2025 of Resident #9's admission sheet dated 07/14/2025 reflected an [AGE] year-old female with an admission date of 08/14/2023 and an original admit date of 02/06/2023. Her relevant diagnoses included Alzheimer's disease (a progressive disease that destroys memory and other important mental functions), dementia (a group of thinking and social symptoms that interferes with daily functioning), mood disorder, and obsessive-compulsive personality disorder (a personality disorder characterized by an intense focus on order, perfectionism, and control).Record review on 07/12/2025 of Resident #9's change of condition MDS assessment dated [DATE] reflected a BIMS score of 06, which reflected her cognition was severely impaired. Record review on 07/12/2025 of Resident 9's quarterly care plan dated 05/22/2025 reflected no behavioral problems and the resident to resident on 03/25/2025 had not been care planned. Resident #7Record review of Resident #7's face sheet dated 07/14/2025 reflected a [AGE] year-old-female with an admission date of 09/16/2019. Her relevant diagnoses included Alzheimer's disease (a progressive disease that destroys memory and other important mental functions), emotional lability (a sign or symptom exaggerated changes in mood or affect in quick secession), mood disorder, and dementia(a group of thinking and social symptoms that interferes with daily functioning) . Record review of Resident #7's annual MDS assessment dated [DATE] reflected a BIMS score of 03, which reflected her cognition was severely impaired. Record review of Resident #7's comprehensive care plan dated 06/19/2025 reflected:Problem: [Resident #7] does tend to get verbally/physically abusive with staff and residents. She isn't easily redirected at time. Resident #10Record review of Resident #10's admission sheet dated 07/14/2025 reflected a [AGE] year-old-female with an admission date of 03/25/2025 and a discharge date of 04/16/2025. Her relevant diagnoses included chronic kidney disease (longstanding disease of the kidneys leading to renal failure), anemia (a condition in which the blood doesn't have enough healthy red blood cells and hemoglobin), unsteadiness on feet, and diabetes (too much sugar in the blood). Record review of Resident #10's admission MDS dated [DATE] reflected a BIMS score of 08, which reflected her cognition was moderately intact. Record review of Resident #10's comprehensive care plan dated 03/25/2025 reflected no behavior problems and resident-to-resident on 04/11/2025 had not been care planned. Resident #2Record review of Resident #2's admission sheet dated 07/14/2025, reflected [AGE] year-old male with an admission date of 07/06/2021. His relevant diagnoses w included Alzheimer's Disease (a progressive disease that destroys memory and other important mental functions), dementia (a group of thinking and social symptoms that interferes with daily functioning) without behavioral disturbance, psychotic disturbance (delusions and hallucinations), mood disturbance, and anxiety (feelings of worry, nervousness, or unease, often about an anticipated event. Record review on 07/12/2025 of Resident #2's quarterly MDS, dated [DATE], revealed a blank BIMS, which indicated his cognition was severely impaired. Record review on 07/12/2025 of Resident #2's quarterly care plan dated 06/13/2025 reflected a problem the resident has a behavior problem related to vascular dementia, mood disorder, delusional disorder. Resident #2's resident-to-resident altercation with Resident #7 on 03/25/2025 had not been care planned and no interventions were set in place. Record review on 07/11/2025 of the facility's incident reports from 01/02/2025 through 07/11/2025 reflected the following: Resident #6 had a resident-to-resident altercation (victim) on 01/02/2025 with Resident #7. 1. Record review of Resident #6's progress note dated 01/02/2025 at 6:19 p.m. authored by LVN P reflected sn (skilled nurse) noted resident trying to get passed another resident and bumped her chair and they exchanged words asking female resident to move and that is when the female resident responded and grabbed resident l fa and pierced the skin and caused multiple skin tears. SN (skilled nurse) witnessed and intervened immediately. SN (skilled nurse) assessed resident and noted serosanguineous drainage coming from site. SN (skilled nurse) cleansed sited with n/s (normal saline) and pat dried and applied steri-strips. Resident denies any discomfort at this time. Up to w/c (wheelchair) waiting for dinner. SN (skilled nurse) continues to monitor resident for any type of changes in condition.NP, RP and administrator made aware. Plan of care ongoingRecord review of Resident #6's change in condition dated 01/02/2025 at 5:30 p.m., reflected:Signs/symptoms details: skin tears to left forearm, started 01/02/2025, since started it has gotten stayed the same.Assessment/suggestion: cleanse with normal saline, pat dry and apply steri strips.Notifications: RP on 01/02/2025 at 5:35 p.m., NP on 01/02/2025 at 5:30 p.m. Record review on 07/11/2025 of Resident #6's skin and wound-total body skin assessment dated [DATE] at 5:09 p.m. Authored by LVN P reflected the following:Turgor: good elasticitySkin color: normal for ethic groupTemperature: warm (normal)Moisture: normalCondition: normalEnter the # of new wounds: 1 Record review of the facility's incident reports from 01/02/2025 through 07/11/2025 reflected the following: Resident #6 had the following resident-to-resident altercations (aggressor) on 03/25/2025 with Resident #9. 2. Record review on 07/11/2025 of Resident #9 progress note dated 03/25/2025 at 5:07 p.m., authored by LVN K reflected: resident (Resident #9) sitting at dining room table interacting with other residents when male resident (Resident #6) at sitti8ng [sitting] at the [NAME] [corner] of the dining room table attempts to take a jacket away from resident. Resident able to stay with a jacket. at this point sn (skilled nurse) noted male resident strike resident on left upper arm with closed hand. Sn (skilled nurse) immediatly [immediately]removed resident. SN (skilled nurse) assessed resident and no discoloration or erythema noted to site. v/s (vital signs) 126/74, 78,98%ra,18,97.8. resident stating that has discomfort to l upper extremity. resident noted with same rom (range of motion) as per baseline. When asked what happened, the resident stated [NAME] el [NAME] me golpio. (the man hit me) contacted dr pending callback with any new orders. administered prn (as needed). contacted rp and understanding verbalized. don made aware.Record review on 07/11/2025 of Resident #9's skin and wound-total body skin assessment dated [DATE] at 7:08 p.m., by LVN P reflected no new wounds.Record review of the facility's incident reports from 01/02/2025 through 07/11/2025 reflected the following: Resident #2 had the following resident-to-resident altercations (aggressor) on 03/25/2025 with Resident #7. 3. Record review on 07/11/2025 of Resident #7 progress note dated, authored by LVN P reflected: resident (Resident #7) in the middle of the hallway when cna (no name) was trying to move her out of the way from the exit door. as cna is maneuvering the resident out of the way of the exit door entrance a male resident (Resident #2) noted to close hand and strike resident in the face on the left cheek. Residentnoted to yell and attempt to strike back. sn intervene immediatly. sn assessed resident noted with no discoloration or erythema to left cheek. resident (Resident #7) denies any discomfort at this time. v/s (vital signs) 128/72,70,98%ra,18,97.3 resident (Resident #7) stating i don't know why he did that. contacted np (nurse practitioner) n/o (new orders) for xr t(x-ray) to left mandible, nasal and nose. RP made aware understanding verbalized. DON made aware. Record review of Resident #7's skin and wound-total body assessment dated [DATE] at 5:26 p.m., authored by LVN P reflected no new wounds. Record review of Resident #7's x-ray results reflected no fractures or other bony abnormalities. Record review of the facility's incident reports from 01/02/2025 through 07/11/2025 reflected the following: Resident #6 had the following resident-to-resident altercations (aggressor) on 04/11/2025 with Resident #7 at 3:15 p.m 4. Record review on 07/11/2025 of Resident #7's progress notes dated 04/11/2025 at 4:50 p.m., authored by LVN K reflected Upon my rounds CNA (no name) notified me of an altercation that occurred between this resident and other resident having her hair pulled and grabbed on her arm. Upon arriving to wandering unit both residents were already separated and performed whole body assessment resident finding no abnormalities. resident complained of no pain VS (vital signs) 123/89 BP, P 89, T 97.6, O297, RR 18. Neuro checks normal notified family and practitioner. Will continue to monitor for deviations of baseline and separate residents in facility.Record review of the facility's risk management report dated 04/11/2025 at 12:25 p.m., authored by LVN K reflected :Incident description: Upon my rounds CNA (no name) notified me of an altercation that occurred between this resident and other resident having her hair pulled and grabbed on her arm. Upon arriving to wandering unit both residents were already separated and performed whole body assessment resident finding no abnormalities. resident complained of no pain VS (vital signs) 123/89 BP, P 89, T 97.6, O297, RR 18. Neuro checks normal notified family and practitioner. Will continue to monitor for deviations of baseline and separate residents in facility. Injury type: no injuries observed at time of incidentLevel of pain: 0Resident description: Resident unable to answer Record review on 07/11/2025 of the Resident #7 skin and wound-total body skin assessment dated [DATE] at 3:18 p.m. reflected no new wounds.Record review of the facility's incident reports from 01/02/2025 through 07/11/2025 reflected the following: Resident #6 had the following resident-to-resident altercations (aggressor) on 03/28/2025 with Resident #10 at 3:15 p.m 5. Record review on 07/11/2025 of the facility's risk management report for Resident #6 (altercation with Resident #10) dated 03/28/2025 at 3:15 p.m., authored by LVN A reflected: aides reported to this nurse resident was hit with a wheelchair in the left knee by [Resident #6], resident has a small skin tear noted to left knee, wound care nurse assessed and treated skin tear, admin and don notified and aware, md at 1546 tx [treatment] order for , Rp notified at 1545. Immediate action taken: resident has small skin tear to left knee that was assessed and treated by wound care nurse. Left skin tear: clean with wound cleanser, pat dry; apply clean gauze dssg [dressing] and monitor for s/s infection. MD notified and tx[treatment] order for. no pain or discomfort noted, resident got herself up and started walking around hallway. Record review on 07/11/2025 of Resident #10's progress notes dated 03/28/2025 at 4:21 p.m., authored by LVN A reflected: aides reported to this nurse resident was hit with a wheelchair in the left knee by [Resident #6], resident has a small skin tear noted to left knee, wound care nurse assessed and treated skin tear, admin and DON notified and aware, md at 13:46 tx [treatment] order for , Rp notified .Record review on 07/11/2025 of Resident #10's change in condition dated 03/25/2025 at 4:26 p.m., reflected the following: The change in condition, symptom, or signs to report: resident was hit with a wheelchair in the left knee by [Resident #6], small skin tear noted to left knee, wound care nurse skin tear.In an interview on 07/11/2025 at 1:00 p.m., CNA KK said Resident #6 for the past couple of months had not displayed any aggressiveness towards staff or residents. She said he was much calmer and would spend more time in his room. She said his health had declined, and he was under palliative care. She said she had been present during his altercation with Resident #7 on 01/02/2025. She said LVN P was sitting in the nurse station facing both residents; she was in the hallway in proximity of where the altercation had taken place. She said Resident #6 had not shown any aggression prior to striking Resident #6 on her face. She said both she and LVN P immediately intervened and separated them. She said she removed Resident #6 while LVN P assessed Resident #6. She said all residents in the memory unit need constant redirecting. She said out of the 21 residents in the memory unit only 3 are bedbound, and the rest are able to ambulate on their own or wheelchairs. She said the unit had enough staff to monitor and redirect residents when needed. She said she was regularly trained in the topics of abuse, neglect, and exploitation. An interview on 07/14/2025 at 4:05 p.m., LVN P said she was the charge nurse in the memory unit during the resident-to-resident involving Resident #6 with Resident #7, and Resident #9. LVN P said on 01/02/2025 (day shift), Resident #7's wheelchair was parked in the middle of the entry of the dining room when Resident #6's wheelchair accidentally bumped into Resident #7's wheelchair. She said, as soon as he bumped her, Resident #7 started making a motion to grab his arm and that's when she immediately went towards them and removed Resident #7's hand from Resident #6's wrist. She said both Resident #6 and Resident #7 have dementia, and they have good and bad days and can be both physically and verbally aggressive. She said Resident #6 sustained multiple skin tears. She said she had immediately cleansed his wounds and notified his NP and RP. She said she was sitting at the nurse's station and always had eyes on them, that's why she was able to immediately intervene. She said Resident #6 and Resident #7 both resumed their normal activities.LVN P said on 03/25/2025 at 2:30 p.m., she was sitting in the nurse's station and had full visual of all the residents in the dining room. She said she saw Resident #7 sitting in the dining room and was approached by Resident #2. She said as Resident #2 tried to remove Resident #7's jacket that was in the back of her wheelchair, Resident #7 quickly grabbed it preventing him from taking it. She said at that time Resident #6 got upset and immediately striked her on her arm. She said she witnessed the entire incident and as soon as Resident #2 raised his hand, she quickly walked towards them, but he still managed to hit Resident #7. She said she and other staff quickly approached both residents and separated them. She said she assessed Resident #7 and saw no injuries. She said she notified their RP's, NP's, and the DON. LVN P said on 03/25/2025 at 3:00 p.m., while sitting in the nurse's station and having full visual of the dining room and hallway, she observed Resident #7 sitting on her wheelchair close to the exit door. She said she then saw Resident #2 walking in the same direction and as a CNA (no name given) tried to move Resident #7 out of the way, Resident #2 was seen closing his hand and what appeared to have striked Resident #7 on her left cheek. She said both were immediately separated and she rendered care to Resident #7. She said she notified her NP (nurse practitioner) who ordered an x-ray of her face area. She said Resident #7 had no visible marks after her skin assessment and denied any pain. LVN P said she was regularly in-service on the topic of abuse and neglect. She said Resident #6, #7, #9 and #2 all had behavior problems related to their diagnoses of Alzheimer's. She said the unit had enough staff to care for all 21 residents. She said Resident #6's resident-to-resident altercations would be considered abuse. She said the Administrator had always been notified of all the resident-to-resident altercations.In an interview on 07/11/2025 at 2:30 p.m., the DON said he was informed of all resident-to-resident altercations. He said all resident-to-resident altercations needed to be care planned and interventions set in place. He said the Administrator was also notified al all resident-to-resident altercations as he was the Abuse Coordinator. He said he was responsible for reporting to the state. The DON said the memory unit had enough staff to care for all 21 residents. He said there were always a minimum of 2 CNAs, 1 charge nurse, 1 activity aide, and the MDS nurse was housed in the unit. He said if a resident needed to be on a 1:1 then they would get another staff member from the facility to cover. The DON said all staff were in-service on the topic of abuse, neglect, and exploitation regularly. The DON could not say if Residents # 2, #6, #7, #9, and #10 had any negative outcomes due to the resident-to-resident altercations they had. In an interview on 07/11/2025 at 2:45 p.m., the Administrator said he would be notified of all resident-to-resident altercations. He said he did not consider the resident-to-resident altercations in the memory unit as abuse because of their mental status. He said all suffered from dementia and to him there was no ill intent when they would strike another resident. He said that was the reason he had not reported the resident-to-resident altercations. Record review of the facility's Abuse, Neglect and Exploitation policy dated 07/11/25 reflected the following:Policy:It is the policy of this facility to provide protections for the health, welfare, and rights of each resident by developing and implementing written policies and procedures that prohibit and prevent abuse, neglect, exploitation, and misappropriation of resident property. Definitions: Physical abuse includes, but is not limited to hitting, slapping, punching, biting, and kicking. It also includes controlling behavior through corporal punishment. III. Prevention of Abuse, Neglect, and Exploitation:The facility will implement policies and procedures to prevent and prohibit all types of abuse, neglect, misappropriation of resident property, and exploitation that achieves: B. Identifying, correcting and intervening in situations in which abuse, neglect, exploitation, and/or misappropriation of resident property is more likely to occur with the deployment of trained and qualified, registered, licensed, and certified staff on each shift in sufficient numbers to meet the needs of the resident, and assure that the staff assigned have knowledge of the individual residents' care needs and behavioral symptoms. D. The identification, ongoing assessment, care planning for appropriate interventions, and monitoring of residents with needs and behaviors which might lead to a conflict or neglect. IV: Identification of abuse, neglect, and exploitationB. Possible indicator of abuse includes, but are not limited to: 6. physical abuse of a resident observed
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Report Alleged Abuse
(Tag F0609)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure that all alleged violations involving abuse,...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews, and record review, the facility failed to ensure that all alleged violations involving abuse, neglect, or mistreatment, were reported immediately to the State Survey Agency, within two hours if the events that cause the allegation involve abuse or result in serious bodily injury, or not later than 24 hours if the events that cause the allegation do not involve abuse and do not result in serious bodily injury, for 3 (Resident #5, Resident #3, and Resident #2) of 4 residents reviewed for neglect.
The facility failed to report allegations of resident neglect for Resident #5 to the State Survey Agency within the allotted time frame of 2 hours on 05/24/25 when Resident #5 had a fall at around 7:30 AM and sustained a serious bodily injury (distal fibular diametaphyseal fracture).
The facility failed to report two Resident – to – Resident altercations. One on 11/15/24 between Resident #3 and Resident #2. The other occurred on 03/25/25 with Resident #2 and an unknown resident.
The facility failed to report unwitnessed injury for Resident #2 on 11/11/24, 11/13/24, 12/17/24, 01/07/25, 02/04/2025, and 03/19/25.
The facility failed to report an unwitnessed fall with skin tear to Resident #2 ' s nose.
These failures could place all residents at increased risk for potential abuse/neglect due to unreported allegations of abuse and neglect.
The findings included:
1.Record review of Resident #5 ' s admission sheet reflected a [AGE] year-old female with an admission date of 03/18/25 and an original admission date of 03/02/24 and a discharge date of 03/22/25). Her relevant diagnoses included dementia (a group of symptoms affecting memory, thinking, and social abilities, which interfere with daily life), abnormalities of gait and mobility (any deviations from typing walking pattern, often indicating underlying neurological, musculoskeletal, or other medical conditions), unsteadiness on feet.
Record review of Resident #5 ' s quarterly MDS assessment dated [DATE] reflected she had a BIMS score of 12, which indicated her cognition was moderately intact.
Record review of Resident #5 ' s quarterly care plan dated 03/04/24 reflected Resident #5 was at risk for falls related to impaired mobility and history of falls. Her interventions in part included to anticipate and meet her needs, call light within reach, and to ensure [Resident #5] wore appropriate footwear (when ambulating or mobilizing in wheelchair.
Record review on 06/17/25 of Resident #5 ' s progress note dated 01/18/25 at 11:09 a.m., authored by LVN T reflected reported to NP purple skin discoloration to right dorsal foot and right inner extremity .Order x-ray, arterial scan to extremity and consult with Dr. Orders in place.
Record review on 06/17/25 of Resident #5 ' s radiology result report dated 01/18/25 signed at 6:52 p.m., reflected Resident #5 had an acute distal fibular diametaphyseal fracture with soft tissue swelling.
Record review on 06/17/25 of Resident #5 ' s progress note dated 01/18/25 at 10:50 p.m., authored by LVN C reflected charge nurse reported .foot right 2 views results serviced 01/18/25 to NP T. As per NP T repeat foot 2 views x-ray, tibia-fibula right 2 views x-ray .
Record review on 06/17/25 of Resident #5 ' s intake reflected the facility reported her injury on 01/19/25 at 3:57 p.m.
In a telephone interview on 06/17/25 at 02:45 p.m., LVN C said he did not remember much of Resident #5 ' s 01/18/25 incident. He said the only thing he remembered was that he had been given report by the outgoing nurse that Resident #5 had complained her ankle being discolored.
An interview on 06/19/25 at 10:30 a.m., LVN U said on 01/18/25 (did not remember the time), Resident #5 had complained to her of having purple skin discoloration to her lower right inner extremity. She said while she assessed her, Resident #5 had voiced that she had not fallen or injured her right leg in any way. LVN U said she immediately notified Resident 4 ' s NP and received order for a scan and x-ray.
In an interview on 06/19/25 at 10:55 p.m., the DON said Resident #5 had complained her lower right leg was discolored, purple in color on 01/18/25 around 11:00 a.m. He said the charge nurse had conducted a head-to-toe assessment and notified Resident #5 ' s NP. He said NP ordered a duplex and an x-ray to right tibia-fibula and to right foot. The DON said the facility had received confirmation from the mobile X-ray company on 01/18/25 at 6:52 p.m. that Resident #5 had a fracture. He said staff must have not read the report until 10:48 p.m. He said Resident #5 ' s NP was notified, and he had ordered a repeat x-ray to confirm fracture. The DON said the reason the NP had ordered a repeat x-ray was because Resident #5 had not complained of pain or reported any injury. The DON said Resident #5 had a repeated x-ray on 01/19/25 and the findings confirmed Resident #5 had an acute distal fibular diametaphyseal fracture. The DON said since Resident#4 ' s NP had requested a repeated x-ray; they did not considered Resident #5 having a fracture until the results from the second x-ray came in. He said Resident #5 ' s NP had not deemed it a fracture yet because he had ordered a second x-ray that was the reason the facility had reported the incident to state on 01/19/25 after the results from the second x-ray confirmed the findings from the first x-ray taken on 01/18/25. The DON said the facility would not call a fracture, until the NP/Dr. called it a fracture.
An interview on 06/19/25 at 11:00 a.m., the Administrator the facility had received Resident #4 ' s x-ray results of a fracture on 01/18/25 at 7:00 p.m., but her NP had ordered a repeat to confirm the finding. The Administrator said the repeated x-ray was done and confirmed on 01/19/25 that Resident #4 had sustained an acute right distal fibular diametaphyseal fracture. He said he reported the fracture within 2 hours of confirming fracture. The Administrator said he did not report the fracture to state on 01/18/25 because Resident #4 ' s NP had not confirmed the fracture.
A telephone interview on 06/19/25 at 12:48 p.m., NP T said he had ordered a repeated x-ray for Resident #4 to confirm the findings of the first x-ray which indicated she had a distal fibular diametaphyseal fracture. He said the second x-ray would serve as a confirmation only and he would go with the first x-ray findings to diagnose her as having a fracture.
2. Record review of Resident #3's admission record dated 06/17/2025, revealed an [AGE] year old male with an admission date of 08/15/2024, and a re-admission date on 11/25/2024, with a diagnoses which included dementia (a group of thinking and social symptoms that interferes with daily functioning) without behavioral disturbance, psychotic disturbance (delusions and hallucinations), mood disturbance, and anxiety, and traumatic subdural hemorrhage (a type of bleeding near the brain that can happen after a head injury) with loss of consciousness of 30 minutes or less.
Record review of Resident #3's admission MDS, dated [DATE], revealed a BIMS of 01, indicating severe cognitive impairment. There were no potential indicators of psychosis, and no behavioral symptoms were indicated. Active diagnoses included: traumatic brain dysfunction (an impairment in the normal functioning of the brain caused by an outside force, usually a violent blow to the head), and dementia.
3. Record review of Resident #2's admission record dated 06/17/2025, revealed a [AGE] year old male with an admission date of 07/06/2021,with a diagnoses which included Alzheimer ' s Disease (a progressive disease that destroys memory and other important mental functions), dementia (a group of thinking and social symptoms that interferes with daily functioning) without behavioral disturbance, psychotic disturbance (delusions and hallucinations), mood disturbance, and anxiety.
Record review of Resident #2's Change in Condition MDS, dated [DATE], revealed a blank BIMS, indicating severe cognitive impairment. There were no potential indicators of psychosis, verbal behavioral symptoms occurred 1 – 3 days, and other behavioral symptoms not directed toward others (e.g., physical symptoms such as hitting or scratching self, pacing, rummaging, public sexual acts, disrobing in public, throwing or smearing food or bodily waste, or verbal/vocal symptoms like screaming, disruptive sounds) occurred 1 – 3 days. Active diagnoses included: Alzheimer ' s Disease and dementia.
Record review of Resident #2 ' s Care Plan dated 04/02/2025 revealed:
FOCUS:
·
The resident is potential to be physically aggressive with staff when redirected. Physically aggresive with staff during showers, dressing, adl care UPSET WHEN REDIRECTED FROM OTHER PATIENTS BED. APT TO SLEEP IN OTHER'S ROOMS. AND ON SOFA. Date Initiated: 09/09/2021 Revision on: 11/11/2024
GOALS:
·
The resident will not harm self or others through the review date. Date Initiated: 09/09/2021 Revision on: 12/26/2024 Target Date: 07/01/2025
INTERVENTIONS/TASKS:
·
Administer medications as ordered. Monitor/document for side effects and effectiveness. Date Initiated: 11/11/2024 LN RN
·
COMMUNICATION: provide physical and verbal cues to alleviate anxiety; give positive feedback, assist verbalization of source of agitation, assist to set goals for more pleasant behavior, encourage seeking out of staff member when agitated. Date Initiated: 09/09/2021 CNA LN RN SS
·
Monitor/document/report PRN any s/sx of resident posing danger to self and others. Date Initiated: 09/09/2021 CNA LN RN SS
·
When the resident becomes agitated: Intervene before agitation escalates; Guide away from source of distress; Engage calmly in conversation; If response is aggressive, staff to walk calmly away, and approach later. Date Initiated: 11/11/2024 CNA LN RN
FOCUS:
·
The resident has a behavior problem r/t Vascular Dementia, Mood disorder, Delusional disorder: RP REFUSES PSCHIATRIC SERVICES. ONLY WANTS PRIMARY MD TO FOLLOW UP WITH BEHAVIORS. Bangs on exit doors Wanders into other residents rooms Rummages through other residents personal belongings Takes other residents seeing eye glasses and puts them on Removes nurses items behind nurses station Urinates in trash cans, hallway, other residents rooms Defecates in trash cans urinates in closets at times likes to eat meals on sofa with bedside table 4/9/24 combative during adl care causing skin tear. RESIDENT NOTED EATING CRAYONS DURING ACTIITY TIME. APT TO PUT ACTIVITY OBJECTS IN MOUTH 9/3/24 ALTERCATION WITH ANOTHER RESDIENT punches, scratches, kicks staff during care Date Initiated: 07/09/2021 Revision on: 11/11/2024
GOALS:
·
The resident will have fewer episodes by review date. Date Initiated: 07/09/2021 Revision on: 12/26/2024 Target Date: 07/01/2025
INTERVENTIONS/TASKS:
·
4/9/24 Administer wound care to skin tear as ordered-patient removes dressing Date Initiated: 04/11/2024 Revision on: 04/11/2024 LN RN
·
9/3/24 MEDICATON REVIEW Date Initiated: 09/04/2024 Revision on: 09/04/2024 LN RN SS
·
Anticipate and meet The resident's needs. Psychiatric consult 12/15/21 with medication recommendations- RP refused. Date Initiated: 07/09/2021 Revision on: 12/30/2021 CNA LN RN
·
Caregivers to provided opportunity for positive interaction, attention. Stop and talk with him/her as passing by. Date Initiated: 07/09/2021 CNA LN RN SS
·
Explain all procedures to the resident before starting and allow the resident to adjust to changes. Date Initiated: 03/17/2022 Revision on: 03/17/2022 CNA LN RN
·
If reasonable, discuss The resident's behavior. Explain/reinforce why behavior is inappropriate and/or unacceptable to the resident. Date Initiated: 07/09/2021 CNA LN RN SS
·
Intervene as necessary to protect the rights and safety of others. Approach/Speak in a calm manner. Divert attention. Remove from situation and take to alternate location as needed. Date Initiated: 07/09/2021 CNA LN RN SS
·
Praise any indication of The resident's progress/improvement in behavior. Date Initiated: 03/17/2022 CNA LN RN SS
·
Reward the resident for appropriate behavior by (OFFERINC SNACKS, ICE ACTACREAM-PER FAMILY REQUEST)- ATTEMPTED FOOD, SNACKS AND ICE CREAM. Date Initiated: 04/11/2024 Revision on: 04/11/2024 CNA LN RN SS.
Record review of Resident #2 ' s CPS Report dated 11/11/2024 revealed Today is 11/11/24. 77 yo has significant injuries to his face that may have been caused by another resident. There are concerns about the level of care that 77yo is receiving if another resident has assaulted him and caused these injuries. 77 yo has an injury to his mouth and was described as having a swollen lip. 77 yo has a bruise near his eye. Staff are unable to explain how this occurred. Staff did not seem to be aware of the injuries until concerns were voiced to them. There was not believed to be physical abuse by staff personnel at the facility.
Record review of Resident #2 ' s Progress Notes dated 11/11/2024 at 11:25 AM written by LVN W revealed, head to toe assessment performed. residents affected areas measured. purplish discoloration to left forearm measured at 2cm (0.787 inches) in length and 2cm (0.787 inches) in in height. purplish discoloration to left side of 52w9chin measured at 1/2 cm in height. resident denies any pain when affected areas are assessed. no skin tears or abnormal skin breakage noted.
Record review of Resident #2 ' s Progress Notes dated 11/13/2024 at 09:06 AM written by LVN P revealed LVN P assessed Resident #3 with reddened discoloration to bilateral (left and right) forearms.
Record review of Resident #3 ' s Progress Notes on 11/15/24 at 12:06 PM written by LVN W revealed Resident #3 displayed physical behaviors toward Resident #2. Verbal comments were made by Resident #3 to Resident #2. Resident #3 pushed Resident #2 away from him.
Record review of Resident #3 ' s Progress Notes on 11/15/24 at 12:07 PM written by LVN W revealed the interaction between both residents was stopped by staff. Residents were separated from each other. Residents PCP made aware of the incident. Order received to increase clonazepam 1mg BID scheduled (Resident #3), and psych consult. orders carried out. The residents ' behavior was to be monitored continuously.
Record review of Resident #2 ' s Progress Notes on 11/15/2024 at 12:26 PM written by LVN W revealed Resident #2 was seen interacting with Resident #3. Resident #2 approached Resident #3 in their face. Resident #3 struck Resident #2 which caused Resident #2 to stumble back. Resident #2 proceeded to push Resident #3.
Record review of Resident #2 ' s Progress Notes on 11/15/2024 at 12:26 PM written by LVN W revealed Resident #2 and Resident #3 were separated immediately by nursing staff. Resident #2 continued walking down the hallway. Resident #2 ' s behavior was to be monitored continuously.
Record review of Resident #2 ' s Progress Notes dated 12/17/2024 at 09:06 AM written by LVN X revealed Monitor discoloration to the left arm and to the left side of the chin. every shift.
Record review of Resident #2 ' s Progress Notes dated 01/07/2025 at 12:00 PM written by LVN J revealed CNA alerted this SN of resident having discoloration to bilateral upper extremities (left arm and right arm) and discoloration to right side of scalp. Upon assessment, red discoloration to bilateral arms noted, no skin tears to bilateral arms noted, and no swelling to bilateral arms noted. Purplish discoloration to scalp noted, approximately 2x2cm.
Record review of Resident #2 ' s Change in Condition Note dated 02/04/2025 at 04:28 PM written by LVN J revealed Resident observed with a bump to forehead and was reported to physician. A new order was given to monitor Resident #2 for 24 hours for any changes.
Record review of Resident #2 ' s Progress Note dated 03/10/2025 at 09:30 PM written by LVN B revealed LVN B was made aware by CNA that Resident #2 was found in supine position next to the bed. Resident #2 was assessed, and a skin tear was noted to bridge of his nose.
Record review of Resident #2 ' s Change in Condition Note dated 03/10/2025 at 09:33 PM written by LVN B revealed Type: Change of Condition Signs/Symptoms Details: unwitnessed fall, started 03/10/2025.
Record review of Resident #2 ' s Orders - Administration Note dated 03/19/2025 at 10:01 AM written by RN V revealed Monitor discoloration to the left arm and to the left side of the chin. every shift.
Record review of Resident #2 ' s Progress Note dated 03/25/2025 at 08:48 PM written by LVN C revealed S/P 1/3 Resident to Resident, Vital signs BP 124/68, pulse 67, Respiration 18, oxygen saturation 97 Room air and temperature 97.8F.
Record review of Resident #2 ' s Progress Note dated 03/25/2025 at 11:52 AM written by LVN J revealed Resident (#2) is S/P Day 2/3 of Resident to Resident.
Interview on 06/16/2025 at 02:30 PM Resident #2 ' s FM stated Resident #2 always had bruises, but it was nothing like what it was that time with a swollen lip and bruised eye in November 2024. He said the facility told him it was unwitnessed, and they did not know what happened. He said he had not heard anything back from the facility.
Interview on 06/18/2025 at 02:10 PM CNA Z stated she had been a CNA since August 2024 and had worked at the facility the entire time. She said if she would see a resident fall or found a resident on the floor, she would tell the nurse right away. CNA Z stated she would not move or leave the resident until the nurse said they could get them up. CNA Z stated she would stay with the resident until the nurse said it was ok to leave. CNA Z stated they try to keep the residents busy. They offer snacks, puzzles, and some watch television. CNA Z stated if there was a resident-to-resident altercation, they try to separate residents, and they call for the nurse. She said there was a nurse in the unit at all times. CNA Z stated CNAs reported any changes to a resident immediately to the nurse. CNA Z stated she would abuse/neglect the administrator because he is the Abuse Coordinator.
Interview on 06/25/2025 at 04:00 PM LVN X stated he had not worked at the facility for over two months. LVN X stated he could not remember the progress note he wrote on 12/17/2024 which said, Monitor discoloration to left arm and left side of chin. He said he thought it was already reported by the prior shift.
Interview on 06/26/2025 at 01:14 PM LVN P stated she could not remember why she completed a Skin and Wound Assessment on Resident #2 on 03/25/2025. LVN P stated Resident #2 was not a faller. She said he paced the hall and has Alzheimer/Dementia. LVN P stated Resident #2 self-ambulated and was an assisted feeding. LVN P stated Resident #2 had unexplained bruising and they did not know why. LVN P stated for discoloration out of nowhere, it should be reported to the doctor, RP, and DON. LVN P stated for changes of a resident either a CNA reported or assessed by the nurse, the doctor would be notified, she would follow through with orders, notify family, complete a Change in Condition form, and let all the team members know what was going on including the DON. LVN P stated if a CNA told her a resident had fallen or was on the floor or if she saw a resident on the floor or a resident fell she would assess the resident, make sure they were safe, contact doctor, follow through with orders, contact family, notify DON, and put in Incident Report. LVN P stated if there was a Resident – to – Resident altercation (verbally or physically) she would immediately separate residents, assess the residents, contact doctor, make sure residents were safe, contact family, complete an Incident /accident report, monitor for 72 hours, and notify DON.
Interview on 06/26/2025 at 05:33 PM the DON stated he would have to look at Resident #2 ' s chart to know if he fell a lot because he had not been at the facility long and did not know all the residents yet. The DON stated he was not sure if Resident #2 had a history of a lot of unexplained bruising. He said all incidents are reported to the doctor (bruising, skin tears, change in condition, etc.). The DON stated all changes a CNA would report or if he would see to a resident are reported. He said if a CNA would tell him a resident had fallen or was on the floor or if he saw a resident on the floor or he had seen the resident fall, he would assess, notify doctor and RP, and follow all orders given. He said if it was safe to put the resident in bed, he would help put them in bed. He said if the fall were unwitnessed, he would get an x-ray, and report to State if needed. The DON stated if there were a Resident – to – Resident altercation (verbally or physically), first thing would be to separate them, safety first, assess, notify doctor and RP. He said if orders were given, he would follow through with the orders.
Interview on 06/26/2025 at 06:42 PM the Administrator stated Resident #2 had a few falls since he had been at the facility. He said he had been at the facility since 02/03/2025. He said he was not aware of any unexplained bruising on Resident #2. He stated that no one had reported any unexplained bruising on Resident #2 to him. The Administrator stated abuse/neglect, injuries of unknown origin, and falls with major injuries were to be reported to State.
Record review of the facility ' s Abuse, Neglect and Exploitation policy dated 08/15/22 reflected:
Policy:
It is a policy of this facility to provide protections for the health, welfare, and rights of each resident by developing and implementing policies and procedures that prohibit and prevent, neglect, exploitation, and misappropriation of property.
IV. Identification of Abuse, Neglect and Exploitation
A. The facility will have written procedures to assist staff in identifying the different types of abuse – mental/verbal abuse, sexual abuse, physical abuse, and the deprivation by an individual of goods and services. This includes staff to resident abuse and certain resident to resident altercations.
B. Possible indicators of abuse include, but are not limited to:
2. Physical marks such as bruises or patterned appearances such as a handprint, belt or ring mark on a resident ' s body.
3. Physical injury of a resident, of unknown source.
VII. Reporting/Response:
The facility will have written procedures that include:
Reporting of all alleged violations to the Administrator, state agency, adult protective services and to all other required agencies (e.g., law enforcement when applicable) within specified timeframes:
Immediately, but no later than 2 hours after the allegation is made, if the events that cause the allegation involve abuse or result in serious bodily injury, or
Not later than 24 hours if the events that cause the allegation do not involve abuse and do not result in serious bodily injury.
CONCERN
(E)
📢 Someone Reported This
A family member, employee, or ombudsman was alarmed enough to file a formal complaint
Potential for Harm - no one hurt, but risky conditions existed
Medical Records
(Tag F0842)
Could have caused harm · This affected multiple residents
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record review, the facility failed to maintain clinical records on each resident that were...
Read full inspector narrative →
**NOTE- TERMS IN BRACKETS HAVE BEEN EDITED TO PROTECT CONFIDENTIALITY** Based on observations, interviews and record review, the facility failed to maintain clinical records on each resident that were complete and accurately documented in accordance with accepted professional standards and practices for 3 (Resident #2, Resident#3, Resident #4) of 5 residents reviewed for accuracy and completeness of clinical records. 1.The facility failed to ensure LVN A and LVN F correctly completed Resident #4's neuro checks between 05/24/25 and 05/27/25. 2. The facility failed to ensure LVN A documented on Resident #4's electronic medical record; he had a nosebleed after the fall he sustained on 05/24/25. 3. The facility failed to ensure Resident #4's left inferior orbital wall fracture was documented on his electronic medical record. 4. The facility failed to ensure two Resident-to-Resident altercations were documented thoroughly. One altercation between residents on 11/15/2024 between Resident #3 and Resident #2, and the other altercation occurred on 03/25/2025 with Resident #2 and Resident #6.5. The facility failed to ensure the bruising of unknown origin for Resident #2 on 11/11/2024, 11/13/2024, 12/17/2024, 01/07/2025, 02/04/2025, and 03/19/2025 was thoroughly documented in the Progress Notes.6. The facility failed to ensure the unwitnessed fall on 03/10/2025 with skin tear to the bridge of Resident #2's nose was thoroughly documented.These failures could place residents at risk of not receiving adequate care and services due to inaccurate reflection of the care provided. Findings included: Record review of Resident #4's admission sheet dated 06/18/25 reflected an [AGE] year-old male with an admission date of 04/19/23 with pertinent diagnoses that included dementia (a group of symptoms affecting memory, thinking, and social abilities, which interfere with daily life), history of falling, difficulty walking, abnormalities of gait and mobility, and presence of intraocular (anything that is situated within the eyeball) lens . Record review of Resident #4's quarterly MDS assessment dated [DATE] reflected a BIMS score of 04, which indicated his cognition was severely impaired. Record review of Resident #4's quarterly care plan dated 05/26/25 reflected he was at risk for falls related to confusion and poor safety awareness (date initiated 04/19/23 and revised on 05/26/23). Resident #4's interventions in part included a safe environment with even floors free from spills and/or clutter, adequate flare free light, a working and reachable call light, and personal items within reach. Record review of Resident #4's progress notes on his electronic medical record dated 05/24/25 at 7:35 a.m., authored by LVN C reflected aide reported to this nurse resident had fell lying on left side on the floor in hallway. resident has redness to left side of cheek and skin tear to left hand. resident stated his foot caught his other foot while walking pushing wheelchair and fell. redness noted to left side of cheek, skin tear noted to back of left hand, NP notified. vs 130/74, 77, 18, 97.4 at time of assisting resident. skin tear cleansed with wound cleanser, and dry dressing applied. Record review of Resident #4's progress notes on his electronic medical record dated 05/24/25 at 9:12 a.m., authored by LVN C reflected NP gave order to send to ER for CT of head to rule out brain bleed from fall, EMS notified at 9:01 a.m. called ER and gave report to RN at 9:08 a.m. Record review on 06/19/25 of Resident #4's hospital record dated 05/24/25 reflected, he had presented to their emergency room via EMS due to a fall. His stated complaint: fall/nosebleed/left hand skin tear. The impression of cat scan performed on 05/24/25 was a left maxillary sinus anterior, medial, and lateral walls, and a left inferior orbital wall fracture which is minimally to nondisplaced. Record review of Resident #4's neuro checks on her electronic medical record reflected they were done from 05/24/25 to 05/26/25. Record review of Resident #4, 13th neuro checks on his electronic medical record were not dated, or time stamped by LVN C. Record review of Resident #4's, 16th and 17th neuro check was left blank by LVN F. In an observation and interview on 06/18/25 at 9:00 a.m., Resident #4 was observed sitting in his wheelchair in the memory unit's dining room. He did not have any visible bruising or any facial grimacing. Resident #4 closed his eyes when this surveyor started speaking to him. An interview on 06/18/25 at 9:15 a.m., LVN A said Resident #4 had sustained a fall on 05/24/25 at around 7:35 a.m., while walking down the hall of the memory unit. She said she was also in the hallway when a nurse aide reported to her Resident #4 had fallen. She said she found Resident #4 lying on his left side. She said she had immediately assessed him and the only injuries he had were a red mark on his cheek and a skin tear to his left hand. LVN A said Resident #4 told her, his foot caught his other foot while walking pushing his wheelchair and fell. She said she immediately notified his NP (no new order given) and proceeded to cleanse his wounds. She said she then proceeded to cleanse his wounds and checked his vitals. She said after his vitals were checked; she initiated the neuro checks. LVN A said during one of the 30-minute neuro checks, she noticed Resident #4 had a nosebleed. She said she called his NP again at 9:12 a.m., to let him know of the nosebleed and gave ordered for Resident #4 to be sent out to the ER to rule out brain bleed from the fall. LVN A said Resident #4 came back the same day with a diagnosis of a left sinus fracture. LVN A said she had contacted Resident #4's NP twice the morning of 05/24/25. She said she had documented Resident #4's fall and nosebleed on his electronic medical record under progress notes and on the neuro check where his nosebleed had been noticed. In an interview on 06/19/25 at 2:00 p.m., LVN A said she had completed Resident #4's neuro check #13. She said she had forgotten to enter the date and time but had answered the rest of the questions. LVN A said she thought she had documented Resident #4's nosebleed on the neuro check but did not know why there was no record of it. She said there were no negative outcomes to Resident #4 not having his neuro check #13th dated/timed, or his nosebleed documented on his electronic medical record. In an interview on 06/19/25 at 2:45 p.m., LVN F said he was supposed to complete Resident #4's neuro checks # 16 and 17 on 05/26/25. He said he did not remember why neuro checks #16 and #17 were blank. He said he did not remember if it was because Resident #4 had refused or if it had been a computer error that the information had not populated. This surveyor asked him what he meant by a computer error and his response was band width issues. LVN F said there were no negative outcomes to Resident #4 not having neuro checks #16 and #17 completed because Resident #4 had been stable that night. An interview on 06/19/25 at 3:00 p.m., the DON said on 05/24/25, Resident #4 had reported he was walking towards the dining area in the memory unit when he fell. The DON said Resident #4 was found lying to his left side in the hallway, he had redness to the left side of the cheek and a skin tear to left hand. He said Resident #4 had given a description of how he had fallen. The DON said after he had been assessed head-to-toe, his NP had been notified. The DON said what he thought had happened was that the NP had not answered the first time, and he later called back and had given orders to send to the ER for treatment, evaluation, and a CT scan. He said the neuro checks were initiated at 7:10 am on 05/24/25 and continued after Resident #4 returned from the hospital. He said neuro check #13, was not dated or timed on 05/25/25 and neuro checks #16 and #17 had been left blank. The DON said it was his responsibility to check on a daily basis any assessments to include neuro checks were done by his nursing staff to ensure they were completed correctly. The DON said when he checked any assessment and did any corrections, his name populated as signed by. He said he missed Resident #4's neuro check 13th had not been dated or signed by LVN C. The DON said on 05/26/25 which he checked Resident #4's neuro checks completed on 05/26/25, he noticed neuro check #16 and #17 had been left blank by LVN F. The DON said he ensured, Resident #4 had his vitals checked on 05/26/25 and that they were within normal range. The DON said no negative outcome to Resident #4 for not having his neuro checks #13, #16, and #17 completed correctly. This Surveyor read LVN A's interview back to the DON. He said he was not aware that LVN C had gotten a hold of Resident #4's NP the first time she called him on 05/24/24, that during a neuro check, Resident #4 had a nosebleed, or that the NP had been called a second time and given orders to send to the ER. The DON said he did not find that information on Resident #4's electronic medical records (progress notes or neuro checks). The DON said Resident #4 had sustained a fracture to the left maxillary sinus. This Surveyor asked the DON to review Resident #4's page 3 of his discharge form from the ER department where it reflected, he had sustained a fracture to the left maxillary sinus anterior, medial, and lateral walls and a left inferior orbital wall fracture which was minimally to nondisplaced. The DON said he had not read about the fracture to the left inferior orbital wall but that it did not matter because it was all the same area. He said both fractures would heal on their own therefore, there were no negative outcome to Resident #4 not having his second fracture (left inferior orbital wall) documented on his electronic medical record. Record review of the facility's Documentation in Medical Record policy dated 10/24/22 reflected: Policy: Each resident's medical record shall contain an accurate representation of the actual experiences of the resident and include enough information to provide a picture of the resident's progress through complete, accurate, and doing documentation. Record review of Resident #2's admission record dated 06/17/2025, revealed a [AGE] year old male with an admission date of 07/06/2021, with a diagnoses which included Alzheimer's Disease (a progressive disease that destroys memory and other important mental functions), dementia (a group of thinking and social symptoms that interferes with daily functioning) without behavioral disturbance, psychotic disturbance (delusions and hallucinations), mood disturbance, and anxiety. Record review of Resident #2's Change in Condition MDS, dated [DATE], revealed a blank BIMS, indicating severe cognitive impairment. There were no potential indicators of psychosis, verbal behavioral symptoms occurred 1 - 3 days, and other behavioral symptoms not directed toward others (e.g., physical symptoms such as hitting or scratching self, pacing, rummaging, public sexual acts, disrobing in public, throwing or smearing food or bodily waste, or verbal/vocal symptoms like screaming, disruptive sounds) occurred 1 - 3 days. Active diagnoses included: Alzheimer's Disease and dementia. Record review of Resident #2's Care Plan dated 04/02/2025 revealed: FOCUS: o The resident is potential to be physically aggressive with staff when redirected. Physically aggresive with staff during showers, dressing, adl care UPSET WHEN REDIRECTED FROM OTHER PATIENTS BED. APT TO SLEEP IN OTHER'S ROOMS. AND ON SOFA. Date Initiated: 09/09/2021 Revision on: 11/11/2024 GOALS: o The resident will not harm self or others through the review date. Date Initiated: 09/09/2021 Revision on: 12/26/2024 Target Date: 07/01/2025 INTERVENTIONS/TASKS: o Administer medications as ordered. Monitor/document for side effects and effectiveness. Date Initiated: 11/11/2024 LN RN o COMMUNICATION: provide physical and verbal cues to alleviate anxiety; give positive feedback, assist verbalization of source of agitation, assist to set goals for more pleasant behavior, encourage seeking out of staff member when agitated. Date Initiated: 09/09/2021 CNA LN RN SS o Monitor/document/report PRN any s/sx of resident posing danger to self and others. Date Initiated: 09/09/2021 CNA LN RN SS o When the resident becomes agitated: Intervene before agitation escalates; Guide away from source of distress; Engage calmly in conversation; If response is aggressive, staff to walk calmly away, and approach later. Date Initiated: 11/11/2024 CNA LN RN FOCUS: o The resident has a behavior problem r/t Vascular Dementia, Mood disorder, Delusional disorder: RP REFUSES PSCHIATRIC SERVICES. ONLY WANTS PRIMARY MD TO FOLLOW UP WITH BEHAVIORS. Bangs on exit doors Wanders into other residents rooms Rummages through other residents personal belongings Takes other residents seeing eye glasses and puts them on Removes nurses items behind nurses station Urinates in trash cans, hallway, other residents rooms Defecates in trash cans urinates in closets at times likes to eat meals on sofa with bedside table 4/9/24 combative during adl care causing skin tear. RESIDENT NOTED EATING CRAYONS DURING ACTIITY TIME. APT TO PUT ACTIVITY OBJECTS IN MOUTH 9/3/24 ALTERCATION WITH ANOTHER RESDIENT punches, scratches, kicks staff during care Date Initiated: 07/09/2021 Revision on: 11/11/2024 GOALS: o The resident will have fewer episodes by review date. Date Initiated: 07/09/2021 Revision on: 12/26/2024 Target Date: 07/01/2025 INTERVENTIONS/TASKS: o 4/9/24 Administer wound care to skin tear as ordered-patient removes dressing Date Initiated: 04/11/2024 Revision on: 04/11/2024 LN RN o 9/3/24 MEDICATON REVIEW Date Initiated: 09/04/2024 Revision on: 09/04/2024 LN RN SS o Anticipate and meet The resident's needs. Psychiatric consult 12/15/21 with medication recommendations- RP refused. Date Initiated: 07/09/2021 Revision on: 12/30/2021 CNA LN RN o Caregivers to provided opportunity for positive interaction, attention. Stop and talk with him/her as passing by. Date Initiated: 07/09/2021 CNA LN RN SS o Explain all procedures to the resident before starting and allow the resident to adjust to changes. Date Initiated: 03/17/2022 Revision on: 03/17/2022 CNA LN RN o If reasonable, discuss The resident's behavior. Explain/reinforce why behavior is inappropriate and/or unacceptable to the resident. Date Initiated: 07/09/2021 CNA LN RN SS o Intervene as necessary to protect the rights and safety of others. Approach/Speak in a calm manner. Divert attention. Remove from situation and take to alternate location as needed. Date Initiated: 07/09/2021 CNA LN RN SS o Praise any indication of The resident's progress/improvement in behavior. Date Initiated: 03/17/2022 CNA LN RN SS o Reward the resident for appropriate behavior by (OFFERINC SNACKS, ICE ACTACREAM-PER FAMILY REQUEST)- ATTEMPTED FOOD, SNACKS AND ICE CREAM. Date Initiated: 04/11/2024 Revision on: 04/11/2024 CNA LN RN SS. Record review of Resident #2's Progress Notes dated 11/11/2024 at 11:25 AM written by LVN W revealed, head to toe assessment performed. residents affected areas measured. purplish discoloration to left forearm measured at 2cm (0.787 inches) in length and 2cm (0.787 inches) in in height. purplish discoloration to left side of 52w9chin measured at 1/2 cm in height. resident denies any pain when affected areas are assessed. no skin tears or abnormal skin breakage noted. Record review of Resident #2's Progress Notes dated 11/13/2024 at 09:06 AM written by LVN P revealed LVN P assessed Resident #3 with reddened discoloration to bilateral (left and right) forearms. Record review of Resident #2's Progress Notes dated 12/17/2024 at 09:06 AM written by LVN X revealed Monitor discoloration to the left arm and to the left side of the chin. every shift. Record review of Resident #2's Progress Notes dated 01/07/2025 at 12:00 PM written by LVN J revealed CNA alerted this SN of resident having discoloration to bilateral upper extremities (left arm and right arm) and discoloration to right side of scalp. Upon assessment, red discoloration to bilateral arms noted, no skin tears to bilateral arms noted, and no swelling to bilateral arms noted. Purplish discoloration to scalp noted, approximately 2x2cm (about 0.79 inch by 0.79 inch). Record review of Resident #2's Change in Condition Note dated 02/04/2025 at 04:28 PM written by LVN J revealed Resident observed with a bump to forehead and was reported to physician. new order to monitor resident for 24 hours for any changes. Record review of Resident #2's Progress Note dated 03/10/2025 at 09:30 PM written by LVN B revealed LVN B was made aware by CNA that Resident #2 was found in supine position next to the bed. Resident #2 was assessed, and a skin tear was noted to bridge of his nose. Record review of Resident #2's Change in Condition Note dated 03/10/2025 at 09:33 PM written by LVN B revealed Type: Change of Condition Signs/Symptoms Details: unwitnessed fall, started 03/10/2025. Record review of Resident #2's Orders - Administration Note dated 03/19/2025 at 10:01 AM written by RN V revealed Monitor discoloration to the left arm and to the left side of the chin. every shift. Record review of Resident #2's Progress Note dated 03/25/2025 at 08:48 PM written by LVN C revealed S/P 1/3 Resident to Resident, Vital signs BP 124/68, pulse 67, Respiration 18, oxygen saturation 97 Room air and temperature 97.8F. Record review of Resident #2's Progress Note dated 03/25/2025 at 11:52 AM written by LVN J revealed Resident (#2) is S/P Day 2/3 of Resident to Resident. Interview on 06/18/2025 at 02:10 PM CNA Z stated if she would see a resident fall or found a resident on the floor, she would tell the nurse right away. CNA Z stated she would not move or leave the resident until the nurse said they could get them up. CNA Z stated she would stay with the resident until the nurse said it was ok to leave. CNA Z stated they try to keep the residents busy. They offer snacks, puzzles, and some watch television. CNA Z stated if there was a resident-to-resident altercation, they would try to separate residents, and they would call the nurse. She said there was a nurse in the unit at all times. CNA Z stated CNAs reported any changes to a resident immediately to the nurse. Interview on 06/25/2025 at 04:00 PM LVN X stated he had not worked at the facility for over two months. LVN X stated he could not remember the progress note he wrote on 12/17/2024 which said, Monitor discoloration to left arm and left side of chin. He said he thought it was already reported by the prior shift. Interview on 06/26/2025 at 01:14 PM LVN P stated she could not remember why she completed a Skin and Wound Assessment on Resident #2 on 03/25/2025. LVN P stated Resident #2 was not a faller. She said he paced the hall and has Alzheimer/Dementia. LVN P stated Resident #2 self-ambulated and was an assisted feeding. LVN P stated Resident #2 had unexplained bruising and they did not know why. LVN P stated for discoloration out of nowhere, it should be reported to the doctor, RP, and DON. LVN P stated for changes of a resident either a CNA reported or assessed by the nurse, the doctor would be notified, she would follow through with orders, notify family, complete a Change in Condition form, and let all the team members know what was going on including the DON. LVN P stated if a CNA told her a resident had fallen or was on the floor or if she saw a resident on the floor or a resident fell she would assess the resident, make sure they were safe, contact doctor, follow through with orders, contact family, notify DON, and put in Incident Report. LVN P stated if there was a Resident - to - Resident altercation (verbally or physically) she would immediately separate residents, assess the residents, contact doctor, make sure residents were safe, contact family, complete an Incident /accident report, monitor for 72 hours, and notify DON. Interview on 06/26/2025 at 05:33 PM the DON stated he would have to look at Resident #2's chart to know if he fell a lot because he had not been at the facility long and did not know all the residents yet. The DON stated he was not sure if Resident #2 had a history of a lot of unexplained bruising. He said all incidents are reported to the doctor (bruising, skin tears, change in condition, etc.). The DON stated all changes a CNA would report or if he would see to a resident are reported. He said if a CNA would tell him a resident had fallen or was on the floor or if he saw a resident on the floor or he had seen the resident fall, he would assess, notify doctor and RP, and follow all orders given. He said if it was safe to put the resident in bed, he would help put them in bed. He said if the fall were unwitnessed, he would get an x-ray, and report to State if needed. The DON stated if there were a Resident - to - Resident altercation (verbally or physically), first thing would be to separate them, safety first, assess, notify doctor and RP. He said if orders were given, he would follow through with the orders. Interview on 06/26/2025 at 06:42 PM the Administrator stated Resident #2 had a few falls since he had been at the facility. He said he had been at the facility since 02/03/2025. He said he was not aware of any unexplained bruising on Resident #2. He stated that no one had reported any unexplained bruising on Resident #2 to him. Record review of the facility's Documentation in Medical Record policy dated 10/24/22 revealed: Policy: Each resident's medical record shall contain an accurate representation of the actual experiences of the resident and include enough information to provide a picture of the resident's progress through complete, accurate, and doing documentation. Policy Explanation and Compliance Guidelines: 1.Licensed staff and interdisciplinary team members shall document all assessments, observations, and services provided in the resident's medical record in accordance with state law and facility policy 2.Documentation shall be completed at the time of service, but no later than the shift in which the assessment, observation, or care service occurred. 3.Principles of documentation include, but are not limited to: e. record date and time of entry